Professional Documents
Culture Documents
GRUPO 7 SX Turner
Uploaded by
Mariangel Suarez HenriquezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
GRUPO 7 SX Turner
Uploaded by
Mariangel Suarez HenriquezCopyright:
Available Formats
SEMINAR
Seminar
Turners syndrome
Michael B Ranke, Paul Saenger Before chromosomal analysis became available, the diagnosis of Turners syndrome was based on the characteristics independently described by Otto Ullrich and Henry Turner, such as short stature, gonadal dysgenesis, typical, visible dysmorphic stigmata, and abnormalities in organs, which present in individuals with a female phenotype. Today, Turners syndrome or Ullrich-Turners syndrome may be defined as the combination of characteristic physical features and complete or part absence of one of the X chromosomes, frequently accompanied by cell-line mosaicism. The increasing interest in Turners syndrome over the past two decades has been motivated both by the quest for a model by which the multi-faceted features of this disorder can be understood, and the endeavour to provide life-long support to the patient. New developments in research allow patients with Turners syndrome to have multidisciplinary care.
Genetics and prenatal diagnostics
Turners syndrome affects about one in 2000 liveborn females.1 In about 50% of cases, karyotype analysis of peripheral lymphocytes reveals the complete loss of one X chromosome (karyotype 45,X) whereas the remaining patients display a multitude of chromosomal abnormalities, including part absence of one X chromosome or mosaicism. In 60% of cases it is the paternal X that is lost during meiosis.2 Tissue-specific karyotyping can give divergent results. A few hypotheses have been put forward to explain the phenotypical implications of the lack of one or part of one sex chromosome: haplo-insufficiency of a gene expressed in both sex chromosomes; imprinting that leads to the expression of a gene from only one of the parents; and non-specific chromosomal effects. The wide range of somatic features in Turners syndrome indicate that a number of different X-located genes are responsible for the complete phenotype. Short stature in Turners syndrome has been associated with haplo-insufficiency of a critical chromosomal region (distal of Xp22.2), which escapes inactivation (pseudoautosomal region of X and Y), and in which the short-stature-homeobox (SHOX) gene resides (Xp22.33). The latter encodes for two isoforms of a protein (SHOXa and SHOXb), whose function is as yet unclear (putative transcription factor).3 During human embryogenesis, the SHOX gene is predominantly expressed in the limbs, particularly in the region of the elbow and knee, as well as the pharyngeal arches.4 Skeletal defects in Turners syndrome include mesomelia, micrognathia, cubitus valgus, high arched palate, short metacarpals, and Madelung deformity. SHOX defects are known to cause mesomelic short stature associated with varied phenotypical features. The heterozygous state causes Leri-Weill dyschondrosteosis, which is characterised by mesomelic short stature and Madelung deformity, whereas the homozygous type
Lancet 2001; 358: 30914
Paediatric Endocrinology Section, University Childrens Hospital, D-72076 Tuebingen, Germany (M B Ranke MD); and Department of Pediatrics, Division of Pediatric Endocrinology, Montefiore Medical Center, Albert Einstein College of Medicine of Yeshiva University, New York, USA (P Saenger MD) Correspondence to: Prof Michael B Ranke: (e-mail: mlranke@med.uni-tuebingen.de)
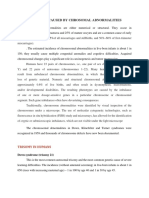
causes Langers osteodysplasia.5 Heterozygous states have, however, also been observed in idiopathic short stature, even in non-mesomelic cases.3,6 The height deficit of the affected individual is, however, about half to two-thirds of that observed in Turners syndrome. Thus, haplo-insufficiency could explain a major part of short stature in Turners syndrome, but does not entirely clarify this issue. Likewise, the variability of skeletal defects accompanying the haplo-insufficiency of SHOX could be due to other genetic or non-genetic factors. Ogata and Matsuo7 have suggested that a higher frequency of Madelung deformations in women with Leri-Weill dyschondrosteosis is caused by the effects of oestrogens, which are either absent or low in Turners syndrome. Zinn and colleagues have also suggested that there is a locus in the interval Xp11.1-p22 encoding for the gene (or genes) pertinent to stature, and have proposed that the transcription factor ZFX is the likely candidate gene (figure 1).8 To date, there are no genetic data available which would explain the soft tissue and visceral stigmata in Turners syndrome, such as lymphoedema, webbing of the neck, and congenital heart failure. It has been proposed that, in primary lymphatic hypoplasia, tissues and organs in the vicinity of the affected lymphatic system are secondarily affected.9,10 In analogy to genes affecting the skeletal and statural growth, it is inferred that a lymphogenic gene escaping X inactivation is present on the sex chromosomes. It has been suggested that genes residing in the vicinity of Xp11.3 are relevant to this issue (figure 2).10 USP9X (DFRX) is a second candidate for the Turners syndrome gonadal dysgenesis gene. DFRX (drosophila fat facets related X) is the human homologue of a fruit fly gene involved in oogenesis and eye development. DFRX escapes X inactivation and maps to Xp11.4, a region of proximal Xp which is implicated in ovarian failure. Two other candidate genes have been described on Xq: RPS4X encodes an isoform of ribosomal protein S4, which lies within a critical region for the lymphoedema-related Turners syndrome phenotype and may also relate to poor viability in utero. DIAPH2 is the second gene and is the human homologue of the drosophila diaphanous (DIA) gene. DIAPH2 is required for normal ovarian function.7,8
Diagnostic approaches
Mostthat is up to 99%11of all embryos or fetuses
THE LANCET Vol 358 July 28, 2001
309
For personal use. Only reproduce with permission from The Lancet Publishing Group.
SEMINAR
45,X
Chromosome imbalance
Gene dosage effect
Chromosomal effect
Loss of SHOX Global non-specific developmental defects Loss of Y-growth gene Loss of lymphogenic gene Meiotic pairing failure
Short stature
Soft tissue stigmata Visceral stigmata
Skeletal stigmata
Gonadal dysgenesis
Figure 1: A schematic representation indicating the underlying factors leading to the development of 45,X Turners syndrome
Reproduced from reference 10, with permission of the authors.
with Turners syndrome are spontaneously miscarried during the first and second trimester of pregnancy. Although monosomy X is not associated with older mothers, the use of prenatal karyotype analysis (by means of chorionic villi sampling or amniocentesis) has led to the identification of an increasing number of Turners syndrome pregnancies. In addition, regular ultrasound examinations have aided the detection of nuchal cystic hygroma and non-immune hydrops during pregnancy, which are typical but not pathognomonic of Turners syndrome. If the degree of nuchal translucency exceeds the normal range in fetuses, the risk of aneuploidy is higher. Coarctation of the aorta, renal anomalies, and growth retardation are further ultrasound findings typical for Turners syndrome. In addition, several markers in maternal serum are associated with aneuploid pregnancies, including Turners syndrome, and involve increased concentrations of fetoprotein, human chorionic gonadotropin, unconjugated oestriol, and inhibin A.12 The positive or negative predictive value of biochemical markers and sonography, however, is not particularly high. The correlation between prenatal karyotyping for elucidation of data on the Turners syndrome phenotype
Phenotype Stature, skeletal anomalies Stature, gonadal failure, minor physical features Viability Gonadal failure q X p Gene (candidate) SHOX (ZFX) (USP9X) (RPS4X) (DIAPH2)
and its severity is rather weak. This is particularly true in cases with mosaicism (eg, 45,X/46,XX). There is evidence, however, supporting the view that prenatal diagnosis of Turners syndrome has led to an increase in the number of fetuses aborted electively.1316 Even if a diagnosis was established prenatally, it needs to be confirmed by postnatal karyotyping. Probing for Y chromosome material should be done in patients with Turners syndrome with evidence of virilisation, or when a marker chromosome (a sex chromosomal fragment of unknown originie, X versus Y) is reported.17 This can be achieved by DNA hybridisation, using a Y centromeric or short-arm probe, and can require probing of multiple tissues. Probing for the SRY gene may fulfil this function, but it is important to recognise that while SRY is associated with male gonadal differentiation, it does not appear to be the gene responsible for gonadoblastoma. Routine screening of all patients with Turners syndrome for SRY is not warranted. The presence of Y chromosome material can cause development of gonadoblastomathe risk of which has been estimated as more than 30%,18,19 although other studies suggest a risk of only 710%.20 Even so, gonadectomy remains the procedure of choice to exclude malignancy with absolute certainty. In cases where patients or parents decide against gonadectomy, detailed vaginal sonography, supplemented with colour doppler sonography of the gonads at regular intervals, could be sufficient to monitor some patients with Y chromosome material.
Sexual development and fertility
A consistent feature documented in Turners syndrome is the unambiguous identification with the female sex. The completion of female development may, however, be thwarted by certain factors during adolescence and in adult life; for instance, ovarian failure occurs in most patients, and up to 30% experience late, but spontaneous puberty.21 In only a fraction of these patients puberty and the menstrual cycle continue. Owing to their short stature, young and adolescent
Figure 2: Turners syndrome critical regions and (candidate) genes
Reproduced from reference 8, with permission of the authors.
310
THE LANCET Vol 358 July 28, 2001
For personal use. Only reproduce with permission from The Lancet Publishing Group.
SEMINAR
patients with Turners syndrome are likely to be overprotected by adults and possibly rejected by their peers. Growth-promoting therapy with recombinant human growth hormone is an accepted method for regulating height during childhood and adult life. Apart from their genetic growth potential, the final height of treated children chiefly depends on the dose of growth hormone, the duration of prepubertal treatment, and the timing of oestrogen substitution. Late diagnosis and insufficient doses have, in several cases, led to the postponement of oestrogen replacement, and, as a result, caused a delay in achieving feminisation. This delay in feminisation could affect the process in which the role of the mature female is learned, as primary deficits involving cognition hinder the development of appropriate social relations22,23 and interaction with the opposite sex. There is, however, insufficient empirical data both on the sexual activities of adolescents and women with Turners syndrome, and on the cause of the presumed deficits during this phase of socialisation. It is extremely rare for a patient with Turners syndrome to experience spontaneous pregnancy and delivery of healthy babies, and the few cases that have been reported include some with a 45,X constellation in peripheral leucocytes. As a rule, however, ovarian failure and infertility are major features of Turners syndrome.24 The almost uniform prospect of infertility is by far the most existential threat to patients with Turners syndrome.25 Techniques to alleviate this situation include in vitro fertilisation of donated oocytes or embryos.26 The success of such attempts depends, to a great extent, on the maturity of the uterus.27 The fact that this approach entails a higher-than-normal risk of spontaneous abortion possibly indicates that an optimum developmental window is required to ensure complete anatomical and functional uterine development. Cryopreservation of oocytes is a possibility in patients with remnant ovarian tissue whose own cells can be used at a suitable timepoint after the technical difficulties of this procedure are completely resolved. Finally, maintenance of ovarian function might be a further means of resolving infertility in Turners syndrome. It has been shown that a cascade of genes are involved in the development of the ovaries from embryonic tissue.28 We now know that ovarian failure in Turners syndrome results from premature ovarian senescence which, in most 45,X patients, ends during infancy as it progresses at a faster pace than normal. Once the mechanisms of this process are understood, it will be possible to develop therapeutic methods of maintaining ovarian function in patients with Turners syndrome.29
Growth promotion
Short stature is the most consistent finding in Turners syndrome. It begins during the prenatal phase and persists after birth, thus resulting in an adult height that is 20 cm below the female average of the corresponding ethnic group.30 The availability of unlimited recombinant human growth hormone has made it possible to conduct carefully designed studies aimed at evaluating the growth response. In the Genentech Turner Study,31 a representative cohort of girls with Turners syndrome was treated with recombinant human growth hormone within the framework of a multicentre, prospective, randomised trial, with some of them receiving concurrent treatment with oxandrolone at the median age of 9 years. Of the 70 original patients, 60 (growth hormone n=17; growth hormone plus oxandrolone: n=43) have now completed therapy and, therefore, ended their participation in the trial. The investigators
also report on 25 patients with Turners syndrome who served as historical controls and who were matched with the study patients and followed to final height. The growth hormone dose was 0375 mg/kg/week (equivalent to about 10 IU/kg/week), divided into daily injections. This dose is about 2550% higher than the replacement dose in growth-hormone-deficient children. The oxandrolone dose was 00625 mg/kg/day, while oestrogen substitution began at a mean age of about 15 years. Although the control group reached an adult height of 1442 cm (SD 60), the patients receiving only growth hormone or growth hormone plus oxandrolone reached 1504 cm (55) and 1521 cm (59), respectively. The difference between the treated groups was not significant. The gain above the projected adult height averaged about 8 cm (ranging from zero to 20 cm), with growth still continuing in several patients. Although this pioneer study set the course for other groups, the controversial debate on the effectiveness of this treatment strategy continues. In several other studies,32 in which older patients were treated with lower doses of growth hormone, satisfactory improvement of height was not achieved. Analysis of these studies revealed the following factors as being predictive of the degree of height gain during growth hormone treatment: age (greatest benefit in the youngest); age at onset of puberty (not before 1314 years of age); and growth hormone dose (highest dose most beneficial).33 These assumptions were confirmed by a Dutch cooperative study in which girls at a median age of 7 years were started on recombinant human growth hormone therapy in doses of up to 14 IU/kg/week (007 mg/kg/day).34 Oestrogen substitution did not begin before the patients reached 12 years of age. Of the 65 girls in the study, 32 have now reached adult height, and only one has a final height under 150 cm. Adult height among the other patients were as follows: above 160 cm in 17 cases and above 170 cm in 5 cases. Growth promotion treatment in these patients was not marked by any major clinical or metabolic side-effects, nor was disproportional growth reported in patients.35,36 The attainment of normal height already during childhood has wide implications, not least the induction of an earlier puberty, which will certainly positively affect the psychosocial integration of patients with Turners syndrome. There was no adverse effect of growth hormone treatment on carbohydrate metabolism. HgbA1c remained in the normal range in several controlled studies. Fasting and postprandial insulin concentrations increased during therapy but returned to normal after termination of growth hormone therapy. Up to 7 years of growth hormone therapy did not affect left ventricular heart dimensions, septal thickness, or blood pressure.37
Neuropsychological and psychosocial aspects
From clinical experience it can be concluded that most patients with Turners syndrome are socially wellintegrated at all levels. Specific problems, however, have been reported. The first systematic investigations of the personality of girls and women with Turners syndrome were conducted in the 1970s.38 These studies indicated that some personality traits were common to most patients, and that these patients had a high stress tolerance, a tendency towards overcompliance, a higher degree of dependence and limitations in emotional competence.3942 Severe mental retardation was noted in patients having a small ring X chromosome that fails to undergo X inactivation43 but, on the whole, tests of intelligence showed average results for this group of
THE LANCET Vol 358 July 28, 2001
311
For personal use. Only reproduce with permission from The Lancet Publishing Group.
SEMINAR
patients. In most studies, however, it has been shown that individual patients with Turners syndrome have selective impairments in non-verbal, visual-spatial information processing, arithmetic, and the coordination of motor and visual-perceptual skills44,45 and, in addition, some degree of hyperactivity.46 The rate of psychopathological states such as depression and anorexia nervosa are slightly higher than the normal population47 while professional success tends to be below normal. As a group, patients have delayed emotional maturity, poor relations with peers, timidity, and a negative body image.48 The interpretation of some of the psychosocial characteristics has mainly been based on behavioural models. There is evidence of an interplay between short stature, delayed or absent puberty, and certain cognitive deficits, and the response of the environment (parents, teachers, peers, employers) to these characteristic Turners syndrome features. Although some of the findings are likely to reflect primary disorders in brain development and function, little evidence is available to justify an association between neurological, behavioural, emotional, and cognitive problems, with neuroanatomical/functional or genetic conditions. Neuroimaging studies using magnetic resonance imaging (MRI) and positron emission tomography4951 have demonstrated that volumetric impairment in the right parietal and occipital type processing occurs in Turners syndrome. Functional MRI studies are currently being done to elucidate the neuronal pathways associated with neurocognitive deficits.52 Results of neurogenetic research have stimulated interest and controversy: thus, the differential gene expression that is known to depend on the parental origin (genomic imprinting) is now being associated with the possibility that in Turners syndrome, genes may be differentially expressed according to the origin of the X chromosome present. It is known that, in 45,X Turners syndrome, the X chromosome is of maternal origin in about 70% of cases.53 However, Skuse and colleagues investigated 80 girls with Turners syndrome, of whom 25 had an X chromosome of paternal origin; these girls showed satisfactory social adjustment and had higher verbal and executive functional skills.40 Similar investigations of normal children54 tend to support the notion that the social communication skills of men are inferior to that of women. In an extension of these studies, the group55 investigated the relation of verbal and non-verbal memory with paternity of the X chromosome. They observed that 45,Xp girls matched controls in verbal memory, whereas this was not the case in 45,Xm. By contrast, the results of 45,Xm patients matched those of controls in visual-spatial memory tests, but the 45,Xp group did not. These studies need to be confirmed by other investigators and extended to other patient collectives. They also indicate that the interdisciplinary approach is the only way to solve complex problems such as neurological functionality and genetics.
Health problems of adult women
Little information is available about the natural history of patients with Turners syndrome after childhood. Sybert56 has suggested that, in adulthood, they opt out of the medical milieu. Data on the mortality of Danish women have been published.14 The median survival age was 69 years for all patients with Turners syndrome, but somewhat lower (644 years) in those with the 45,X constellation. In comparison with the normal population, these statistics are below the average. In
about 50% of cases, the stated cause of death was cardiovascular disease, and in 25% of cases, diabetes mellitus developed. About 30% of patients have congenital heart failure.57,58 Bicuspid aortic valve and coarctation of the aorta are the most common defects found in patients with Turners syndrome. Aortic root dilatation, which is often associated with bicuspid aortic valve and coarctation of the aorta, poses a high risk of disease. Irrespective of any structural abnormality, adult patients tend to have high blood pressure.58 Structural defects in the aorta, combined with high blood pressure, pose a risk of aortic dissection with potentially fatal consequences. Regular cardiac examinations, including sonography of the aortic root, are therefore an essential part of adult health-care. Early, and consistent oestrogen replacement needs to be assessed, as it improves the lipid profile, and decreases aortic stiffness. In the last decade the association of aortic dissection, and Turners syndrome has been increasingly recognised, partly accounting for the excessive mortality in females with Turners syndrome. Echocardiography should be done every 5 years. Only with continued surveillance in adult life will we discover the best method of preventing aortic dilation. The reported incidence of hypothyroidism in adults with Turners syndrome is 2530%, up to 50% have thyroid antibodies, especially women with isochromosome Xp. Osteopenia and osteoporosis are common. Bone mineral density is greater in those who received growth-promoting treatment than in those who did not. Thus, growth hormone therapy in childhood could be of life-long benefit to bone health.6063 Epidemiological data indicate that the metabolic syndrome involving hypertension, dyslipidaemia, type 2 diabetes mellitus, and obesity is more frequent among adults with Turners syndrome.64 The risk of type 2 diabetes increases by a factor of 44 in Turners syndrome patients compared with the normal population. The mechanisms of development of type 2 diabetes are, however, not clear, and impaired sensitivity to insulin does not explain the disorder completely. Nonetheless, tests of annual fasting blood sugar concentrations are recommended. Adiposity accompanied by fairly low concentrations of leptin indicate a disturbance in feedback.59 Reduced physical activity could also be a factor that enhances obesity, thus increasing the risk of cardiovascular and metabolic morbidity. Guidance on nutrition and physical activity should be part of the health-care facilities. In the light of the inherent risks of developing type 2 diabetes and obesity, attempts to promote height with high doses of growth hormone in childhood need to be accompanied by careful monitoring of glucose tolerance and lipid metabolism. Raised liver enzymes, cirrhosis, and inflammatory bowel disease occur with a higher frequency in adult women with Turners syndrome.65,66 Although the frequent hearing impairment in Turners syndrome patients is not life-threatening, it cannot be neglected. The anatomical abnormalities of the middle ear dramatically increase the incidence of middle-ear infections during childhood. Timely treatment reduces the risk of developing a permanent hearing impairment. In adults, a sensorineural aural impairment has been noted in more than 50% of cases, and was predominantly seen at a frequency of 12 kHz (sensorineural dip). It is thought to be related to a defect in the outer hair cells of the lower middle coil of the cochlea. The dip is more frequent in women having a 45,X or 45,X/46,X,i(Xq) karyotype, and is known to deteriorate with age. Apart from this, age-related
312
THE LANCET Vol 358 July 28, 2001
For personal use. Only reproduce with permission from The Lancet Publishing Group.
SEMINAR
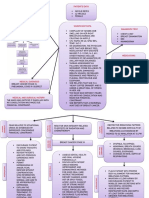
Liver function, inflammatory bowel cirrhosis
Obesity NIDDM hypertension lipids Adult Turner syndrome
Kidney and ureter structure & function Cardiac death aortic dissection
Autoimmunity hypothyroidism IDDM
Pregnancy safety
Psychology
Sensorineural deafness
Cancer Y fragments
Long term consequences of HRT Osteoporosis
Figure 3: The interrelationships of morbidity taken into account in an adult Turners syndrome clinic
Reproduced from reference 60, with permission of the authors.
deafness towards high frequencies has also been observed. The overall hearing threshold is higher in Turners syndrome at any age (about 1030 db), and hearing aids are essential devices that go a long way towards ensuring that adults with the condition are not isolated. Children and women with Turners syndrome benefit from a comprehensive health surveillance programme providing anticipatory guidance to patients and their parents. Although effective improvements in final height are now well within reach for many girls; the adult morbidity deserves new health care schemes for young adults with Turners syndrome (figure 3).60
References
1 Hsu LYF. Prenatal diagnosis of chromosomal abnormalities through amniocentesis. In: Milunsky A, ed. Genetic disorders and the fetus. Baltimore: The Johns Hopkins University Press, 1998: 179248. Mathur A, Stekol L, Schatz D, MacLaren NK, Scott ML, Lippe B. The parental origin of the single X chromosome in Turner syndrome: lack of correlation with parental age or clinical phenotype. Am J Hum Genet 1991; 48: 68286. Rao E, Weiss B, Fukami M, et al. Pseudoautosomal deletions encompassing a novel homeobox gene cause growth failure in idiopathic short stature and Turner syndrome. Nat Genet 1997; 16: 5463. Clement JM, Schiller S, Rao E, et al. The short stature homeobox gene SHOX is involved in skeletal abnormalities in Turner syndrome. Hum Mol Genet 2000; 9: 695702. Belin V, Cusin V, Viot G, et al. SHOX mutations in dyschondrosteosis (Leri-Weill syndrome). Nat Genet 1998; 19: 6769. Binder G, Schwarze CP, Ranke MB. Identification of short stature caused by SHOX defects and therapeutic effect of recombinant human growth hormone. J Clin Endocrinol Metab 2000; 85: 24549. Ogata T, Matsuo N. Sex chromosome aberrations and stature: deduction of the principal factors involved in the determination of adult height. Hum Genet 1993; 91: 55162. Zinn AR, Ross JL. Critical regions for Turner syndrome phenotypes on the X chromosome. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 1928. Vittay P, Bosze P, Gaal M, Laszlo J. Lymph vessel defects in patients with ovarian dysgenesis. Clin Genet 1980; 18: 38791. Ogata T, Muroya K, Matsuo N. Structure function relation of the X chromosome in Turner syndrome. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 918. Hook EB. Spontaneous deaths of fetuses with chromosomal abnormalities diagnosed prenatally. N Engl J Med 1978; 299: 103638. Ruiz C, Lamm F, Hart PS. Turner syndrome and multiple-marker screening. Clin Chem 1999; 45: 225961. Gravholt CH, Juul S, Naeraa RW, Hansen J. Prenatal and postnatal prevalence of Turners syndrome: a registry study. BMJ 1996; 312: 1621. Gravholt CH. Morbidity in Turner syndrome. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 28594. Goldberg JD, Porter AE, Golbus MS. Current assessment of fetal losses as a direct consequence of chorionic villus sampling.
9 10
11
12 13
14
15
Am J Med Genet 1990; 35: 17477. 16 Kulkarni R, Hawkins J, Bradford WP. Prenatal diagnosis of 45,X/46,XX mosaicism in the fetus. Should the pregnancy be terminated? Prenat Diagn 1989; 9: 43941. 17 Zinn AR, Page DC. Turner syndrome and the Y chromosome. In: Hibi I, Takano K, eds. Basic and clinical approach to Turner syndrome, Amsterdam: Elsevier Science Publishers BV, 1993: 4956. 18 Manuel M, Katayama PK, Jones-HW J. The age of occurrence of gonadal tumors in intersex patients with a Y chromosome. Am J Obstet Gynecol 1976; 124: 293300. 19 Verp MS, Simpson JL. Abnormal sexual differentiation and neoplasia. Cancer Genet Cytogenet 1987; 25: 191218. 20 Gravholt CH, Fedder J, Naeraa RW, Muller J. Occurrence of gonadoblastoma in females with Turner syndrome and Y chromosome material: a population study. J Clin Endocrinol Metab 2000; 85: 31993202. 21 Pasquino AM, Pucarelli I, Segni M. Spontaneous puberty in Turner syndrome. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 23138. 22 Sonis W, Levine-Ross J, Blue J. Hyperactivity and Turner syndrome. San Francisco: American Academy of Child Psychiatry, 1983. 23 Williams JK. School-aged children with Turners syndrome. J Pediatr Nurs 1992; 7: 1419. 24 Tarani L, Lampariello S, Raguso G, et al. Pregnancy in patients with Turners syndrome: six new cases and review of literature. Gynecol Endocrinol 1998; 12: 8387. 25 Sylven L, Magnusson C, Hagenfeldt K, von Schoultz B. Life with Turners syndrome - a psychosocial report from 22 middle-aged women. Acta Endocrinol Copenh 1993; 129: 18894. 26 Hovatta O, Foudila T, Sderstrm-Anttila V. Assisted reproductive techniques in Turner syndrome. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 24753. 27 Baird DT, Webb R, Campbell BK, Harkness LM, Gosden RG. Long-term ovarian function in sheep after ovariectomy and transplantation of autografts stored at -196 C. Endocrinol 1999; 140: 46271. 28 Heikkil M, Peltoketo H, Vainio S. Genetic regulation of female development: lessons from Wnt-4. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 2941. 29 Tilly JL, Morita Y, Maravei DV, Matikainen T, Perez GI. Genetic control of apoptosis in oocytes. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 43. 30 Ranke MB, Grauer ML. Adult height in Turner syndrome: results of a multinational survey 1993. Horm Res 1994; 42: 9094. 31 Rosenfeld RG, Hintz RL, Johanson AJ, et al. Three-year results of a randomized prospective trial of methionyl human growth hormone and oxandrolone in Turner syndrome. J Pediatr 1988; 113: 393400. 32 Donaldson MDC. Growth hormone therapy in Turner syndrome Current uncertainties and future strategies. Horm Res 1997; 48 (suppl 5): 3544. 33 Ranke MB, Price DA, Maes M, Albertsson-Wikland K, Lindberg A. Factors influencing final height in Turner syndrome following GH treatment: results of the Kabi International Growth Study (KIGS). In: Albertsson-Wikland K, Ranke MB, eds. Turner Syndrome in a Life-Span Perspective, Amsterdam: Elsevier Science BV, 1995: 16168. 34 Sas TCJ, Keizer SS, Stijnen T, et al. Normalization of height in girls with Turner syndrome after long-term growth hormone treatment: results of a randomized dose-response trial. J Clin Endocrinol Metab 1999; 84: 460712. 35 Sas T, de Muinck Keizer-Schrama S, Aanstoot HJ, Stijnen T, Drop S. Carbohydrate metabolism during growth hormone treatment and after discontinuation of growth hormone treatment in girls with Turner syndrome treated with once or twice daily growth hormone injections. Clin Endocrinol 2000; 52: 74147. 36 Sas T, de Muinck Keizer-Schrama SMPF, Gerver WJ, Drop S. Body proportions in girls with Turner syndrome (TS) after long-term growth hormone (GH) treatment (Rx). Horm Res 1999; 51 (suppl 2): 58. 37 Saenger P. Turners syndrome. N Engl J Med 1996; 355: 174954. 38 Money J, Mittenthal S. Lack of personality pathology in Turners syndrome: relation to cytogenetics, hormones and physique. Behav Genet 1970; 1: 4356. 39 Stabler B. Effects of growth hormone deficiency on psychological functioning and quality of life. In: Ranke MB, Wilton P, eds. Growth Hormone Therapy in KIGS: 10 Years Experience, J & J ed. Heidelberg-Leipzig: Johann Ambrosius Barth Verlag, 1999: 36570. 40 Skuse DH, James RS, Bishop DVM, et al. Evidence from Turners syndrome of an imprinted X-linked locus affecting cognitive
THE LANCET Vol 358 July 28, 2001
313
For personal use. Only reproduce with permission from The Lancet Publishing Group.
SEMINAR
function. Nature 1997; 387: 70508. 41 McCauley E, Ito J, Kay T. Psychosocial functioning in girls with Turners syndrome and short stature: social skills, behavior problems, and self-concept. J Am Acad Child Psychiatry 1986; 25: 10512. 42 Haverkamp F, Keuker T, Kaiser G, Noeker M, Zerres KRC. Social cognition in relation to different visuospatial cognitive styles in Ullrich-Turner syndrome: evidence for a selective deficit in social context dependent visual integration. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 97103. 43 El-Abd S, Patton MA, Turk J, Hoey H, Howlin P. Social, communicational, and behavioral deficits associated with ring X Turner syndrome. Amer J Med Genet 1999; 88: 51016. 44 Downey J, Ehrhardt AA, Gruen R, Bell JJ, Morishima A. Psychopathology and social functioning in women with Turner syndrome. J Nerv Ment Dis 1989; 177: 191201. 45 Romans SM, Stefanatos G, Roeltgen DP, Kushner H, Ross JL. Transition to young adulthood in Ullrich-Turner syndrome: neurodevelopmental changes. Am J Med Genet 1998; 79: 14047. 46 McCauley E, Kay T, Ito J, Treder R. The Turner syndrome: cognitive deficits, affective discrimination, and behavior problems. Child Dev 1987; 58: 46473. 47 Rovet JF. School outcome in Turner syndrome. In: Stabler B, Underwood LE, eds. Growth, stature, and adaptation: behavioral, social and cognitive aspects of growth delay, Chapel Hill: University of North Carolina at Chapel Hill, 1994: 16580. 48 McCauley E, Ross JL, Kushner H, Cutler G. Self-esteem and behavior in girls with Turner syndrome. J Dev Behav Pediatr 1995; 16: 8288. 49 Clark C, Klonoff H, Hayden M. Regional cerebral glucose metabolism in Turner syndrome. Can J Neurol Sci 1990; 17: 14044. 50 Reiss AL, Mazzocco MM, Greenlaw R, Freund LS, Ross JL. Neurodevelopmental effects of X monosomy: a volumetric imaging study. Ann Neurol 1995; 38: 73138. 51 Murphy DG, Mentis MJ, Pietrini P, et al. A PET study of Turners syndrome: effects of sex steroids and the X chromosome on brain. Biol Psychiatry 1997; 41: 28598. 52 Haberecht M, Menon V, Warsofsky I, et al. Neurocognitive function in Turner syndrome: a review of neuroimaging and behavioural studies. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 7984. 53 Jacobs P, Dalton P, James R, et al. Turner syndrome: a cytogenetic
and molecular study. Ann Hum Genet 1997; 61 (Part 6): 47183. 54 Scourfield J, Martin N, Lewis G, McGuffin P. Heritability of social cognitive skills in children and adolescents. Br J Psychiatry 1999; 175: 55964. 55 Bishop DVM, Canning E, Elgar K, Morris E, Jacobs PA, Skuse DH. Distinctive patterns of memory function in subgroups of females with Turner syndrome: evidence for imprinted loci on the X-chromosome affecting neurodevelopment. Neuropsychol 2000; 38: 71221. 56 Sybert VP. Cardiovascular malformations and complications in Turner syndrome. Pediatr 1998; 101: 11117. 57 Lin AE. Management of cardiac problems. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 11523. 58 Mazzanti L, Prandstraller D, Picchio FM, Cacciari E, and the Italian Study Group for Turner Syndrome (ISGTS). Italian Turner syndrome study: cardiac function and complications. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 12536. 59 Gravholt CH, Naeraa RW, Nyholm B, et al. Glucose metabolism, lipid metabolism, and cardiovascular risk factors in adult Turners syndrome: the impact of sex hormone replacement. Diab Care 1998; 21: 106270. 60 Conway GS, Elsheik M, Cadge B, Ostberg J. Adult Turner followupthe Middlesex experience. In: Saenger P, Pasquino AM, eds. Optimizing health care for Turner patients in the 21st century, Elsevier, 2000: 295306. 61 Garden AS, Diver MJ, Fraser WD. Undiagnosed morbidity in adult women with Turners syndrome. Clin Endocrinol 1996; 45: 58993. 62 de Kerdanet M, Lucas J, Lemee F, Lecornu M. Turners syndrome with X-isochromosome and Hashimotos thyroiditis. Clin Endocrinol Oxf 1994; 41: 67376. 63 Radetti G, Mazzanti L, Paganini C, et al. Frequency, clinical and laboratory features of thyroiditis in girls with Turners syndrome.The Italian Study Group for Turners Syndrome. Acta Paediatr 1995; 84: 90912. 64 Gravholt CH, Juul S, Naeraa RW, Hansen J. Morbidity in Turner Syndrome. J Clin Epidemiol 1998; 51: 14758. 65 Albareda MM, Gallego A, Enriquez J, Rodriguez JL, Webb SM. Biochemical liver abnormalities in Turners syndrome. Eur J Gastroenterol Hepatol 1999; 11: 103739. 66 Salerno M, Di-Maio S, Gasparini N, Rizzo M, Ferri P, Vajro P. Liver abnormalities in Turner syndrome. Eur J Pediatr 1999; 158: 61823.
314
THE LANCET Vol 358 July 28, 2001
For personal use. Only reproduce with permission from The Lancet Publishing Group.
You might also like
- Clinical Manifestations and Diagnosis of Turner Syndrome PDFDocument50 pagesClinical Manifestations and Diagnosis of Turner Syndrome PDFcesar chiangNo ratings yet
- Isochromosome Paper-CorrectionDocument6 pagesIsochromosome Paper-CorrectionponnambalamNo ratings yet
- Jurnal 5Document14 pagesJurnal 5mellvinNo ratings yet
- Hum. Reprod. Update 2002 Laml 483 91Document9 pagesHum. Reprod. Update 2002 Laml 483 91Amit GoelNo ratings yet
- Turner Syndrome: Update On Biology and Management Across The Life SpanDocument8 pagesTurner Syndrome: Update On Biology and Management Across The Life SpanKarla JuárezNo ratings yet
- Fragile X Syndrome (Martin-Bell Syndrome)Document6 pagesFragile X Syndrome (Martin-Bell Syndrome)yudhi kurniawanNo ratings yet
- Y Chromosome in Turner Syndrome: Review of The Literature: Cromossomo Y Na Síndrome de Turner: Revisão Da LiteraturaDocument6 pagesY Chromosome in Turner Syndrome: Review of The Literature: Cromossomo Y Na Síndrome de Turner: Revisão Da Literaturakirki pNo ratings yet
- Laboratory Guideline For Turner Syndrome.Document4 pagesLaboratory Guideline For Turner Syndrome.lguerreroNo ratings yet
- S7. Turner SyndromeDocument5 pagesS7. Turner SyndromeAxSlzrNo ratings yet
- Chromosome Imbalance As A Driver of Sex Disparity in DiseaseDocument12 pagesChromosome Imbalance As A Driver of Sex Disparity in DiseaseFirmanNo ratings yet
- Epidemiology, Endocrinology and Metabolism in Turner SyndromeDocument31 pagesEpidemiology, Endocrinology and Metabolism in Turner SyndromeRaihandi PutraNo ratings yet
- Fragile X Syndrome: Understanding the Most Common Cause of Inherited Mental RetardationDocument4 pagesFragile X Syndrome: Understanding the Most Common Cause of Inherited Mental RetardationChristin Natalia KalembangNo ratings yet
- Mechanisms and lifelong management of Turner syndromeDocument15 pagesMechanisms and lifelong management of Turner syndromekirki pNo ratings yet
- Molecular Biology of Turner's Syndrome-Archive of Disease in ChildhoodDocument2 pagesMolecular Biology of Turner's Syndrome-Archive of Disease in ChildhoodNinaNo ratings yet
- Autosomal Deletion SyndromesDocument50 pagesAutosomal Deletion SyndromesZainab Jamal SiddiquiNo ratings yet
- Fragile X syndrome: causes, diagnosis, mechanisms, and therapeuticsDocument9 pagesFragile X syndrome: causes, diagnosis, mechanisms, and therapeuticshanzelNo ratings yet
- Turner Syndrome: Update The Paradigm of Diagnosis, Clinical Care and Consequences of Y Cell LinesDocument10 pagesTurner Syndrome: Update The Paradigm of Diagnosis, Clinical Care and Consequences of Y Cell LinesBastiaanNo ratings yet
- 2 - Fragile X SyndromeDocument4 pages2 - Fragile X Syndromechenelyn_15No ratings yet
- Hir SprungDocument7 pagesHir SprungNajwaNo ratings yet
- Disorders of Gonadal and Sexual Development: BESHG Postgraduate Course in Human GeneticsDocument43 pagesDisorders of Gonadal and Sexual Development: BESHG Postgraduate Course in Human GeneticsDarmawan HariyantoNo ratings yet
- Swyer Syndrome 5 7 14Document20 pagesSwyer Syndrome 5 7 14ireneaureliaNo ratings yet
- Turner Syndrome Research PaperDocument7 pagesTurner Syndrome Research Paperapi-316370647100% (1)
- Sindrome de TurnerDocument13 pagesSindrome de TurnerVALENTINA CORNELLNo ratings yet
- Burégio-Frota Et Al 2010Document5 pagesBurégio-Frota Et Al 2010dida_bispoNo ratings yet
- Bookshelf NBK425926Document21 pagesBookshelf NBK425926Xime AlegríaNo ratings yet
- Genetic Causes of Teratozoospermia Highlighted in Human Reproduction StudyDocument31 pagesGenetic Causes of Teratozoospermia Highlighted in Human Reproduction StudyAdhe Cakra Mandala PutraNo ratings yet
- TS Diagnostic and Management For ClinicianDocument10 pagesTS Diagnostic and Management For ClinicianILham SyahNo ratings yet
- Diapositiva 1: Título Turner: Clinical CharacteristicsDocument7 pagesDiapositiva 1: Título Turner: Clinical CharacteristicselmancuernoNo ratings yet
- NIH Public Access: Author ManuscriptDocument13 pagesNIH Public Access: Author ManuscriptBastiaanNo ratings yet
- XX Gonadal Dysgenesis Is A Type of Female Hypogonadism inDocument4 pagesXX Gonadal Dysgenesis Is A Type of Female Hypogonadism inSisayNo ratings yet
- Nelson 2007 Parte 9 y 10 Gen MetabDocument177 pagesNelson 2007 Parte 9 y 10 Gen MetabLupis Meza IglesiasNo ratings yet
- Actualización en El Manejo Del Síndrome de Turner en Niñas y Adolescentes. Revisión de La Literatura e Incorporación de Recomendaciones de Las Nuevas Guías ClínicasDocument8 pagesActualización en El Manejo Del Síndrome de Turner en Niñas y Adolescentes. Revisión de La Literatura e Incorporación de Recomendaciones de Las Nuevas Guías ClínicasLopez Alvarado JheisonNo ratings yet
- Presidency School Mangalore: Chromosomal DisordersDocument28 pagesPresidency School Mangalore: Chromosomal DisordersAiman SyedNo ratings yet
- Intersex or Disorders of Sexual DevelopmentDocument19 pagesIntersex or Disorders of Sexual DevelopmentHUSAMNo ratings yet
- Prenatal Evaluation of Short FemursDocument15 pagesPrenatal Evaluation of Short FemursadicrisNo ratings yet
- Arumugam Et Al-Clinical Anatomy 2Document10 pagesArumugam Et Al-Clinical Anatomy 2Kavitha RajaNo ratings yet
- A Novel RLIM/RNF12 Variant Disrupts Protein Stability and Function To Cause Severe Tonne-Kalscheuer SyndromeDocument9 pagesA Novel RLIM/RNF12 Variant Disrupts Protein Stability and Function To Cause Severe Tonne-Kalscheuer SyndromeMohamad SoveyziNo ratings yet
- 2010.a Review of Trisomy X (47,XXX)Document9 pages2010.a Review of Trisomy X (47,XXX)rpina.genNo ratings yet
- 2023.Understanding the Genetics of Human InfertilityDocument6 pages2023.Understanding the Genetics of Human Infertilityrpina.genNo ratings yet
- 3 - Genetics Lec.3 (Gross Structural Anomalies of Chromosoms)Document27 pages3 - Genetics Lec.3 (Gross Structural Anomalies of Chromosoms)Ammar AlnajjarNo ratings yet
- KAL1 Mutations Are Not A Common Cause of Idiopathic Hypogonadotrophic Hypogonadism in HumansDocument6 pagesKAL1 Mutations Are Not A Common Cause of Idiopathic Hypogonadotrophic Hypogonadism in Humansndre_bocchaanNo ratings yet
- Fragile X Syndrome GuideDocument8 pagesFragile X Syndrome GuideFianirazhaPrimesaNo ratings yet
- Sindrome de NoonamDocument19 pagesSindrome de NoonamLicMarinaGarayNo ratings yet
- TURNER SyndromeDocument4 pagesTURNER SyndromeAmina RajahNo ratings yet
- RT Xy 3 TXT 7 Cs VP TPVW WGV X3 MDocument4 pagesRT Xy 3 TXT 7 Cs VP TPVW WGV X3 MFlavia ChNo ratings yet
- Genes, Environment and Inheritance_MG 4Document30 pagesGenes, Environment and Inheritance_MG 4snowrose2609No ratings yet
- Turner SyndromeDocument4 pagesTurner SyndromeRajat BhatnagarNo ratings yet
- Chromosomal Aberration Causes Genetic DisordersDocument4 pagesChromosomal Aberration Causes Genetic DisordersSyed Shah HussainNo ratings yet
- Reyes - Unit 2 (Part 2)Document4 pagesReyes - Unit 2 (Part 2)Justine Ericca ReyesNo ratings yet
- Turner PDFDocument12 pagesTurner PDFGuadalupeNo ratings yet
- Down Syndrome-Recent Progress and Future ProspectsDocument9 pagesDown Syndrome-Recent Progress and Future ProspectsRuxandra CretuNo ratings yet
- Current Concepts in Disorders of Sexual Development 2013Document10 pagesCurrent Concepts in Disorders of Sexual Development 2013sheyla alegreNo ratings yet
- Triple X Syndrome With A Rare Finding: Cleft Palate: Case ReportDocument3 pagesTriple X Syndrome With A Rare Finding: Cleft Palate: Case ReportDewi JayantiNo ratings yet
- Cui 2018Document6 pagesCui 2018Naman KhalidNo ratings yet
- Treacher Collins Syndrome: Clinical CharacteristicsDocument21 pagesTreacher Collins Syndrome: Clinical Characteristicschristian roblesNo ratings yet
- Pre-Reading Genetics DisordersDocument10 pagesPre-Reading Genetics DisordersMya Phone MohNo ratings yet
- Cornelia, OminDocument11 pagesCornelia, OminVictor Hugo Guapi NauñayNo ratings yet
- Chromosomal Disorders SimpleDocument8 pagesChromosomal Disorders SimpleSadia KanwalNo ratings yet
- Duplication at Xq13.3-q21.1 With Syndromic Intellectual Disability, A Probable Role For The ATRX GeneDocument6 pagesDuplication at Xq13.3-q21.1 With Syndromic Intellectual Disability, A Probable Role For The ATRX GeneEyyup UctepeNo ratings yet
- CaseFiles FamilyMed Notes 5Document150 pagesCaseFiles FamilyMed Notes 5vesv86% (7)
- Gliomas Linea Media 1Document9 pagesGliomas Linea Media 1JOHN LOPERANo ratings yet
- Widal TestDocument8 pagesWidal Testhamadadodo7No ratings yet
- Tribology in Total Hip and Knee Arthroplasty PDFDocument216 pagesTribology in Total Hip and Knee Arthroplasty PDFNoel Alonso Calleros HernandezNo ratings yet
- Analysis of Quantitative Studies - EditedDocument7 pagesAnalysis of Quantitative Studies - EditedViotry ChepkwonyNo ratings yet
- Tracheostomy SuctioningDocument59 pagesTracheostomy SuctioningMaan LapitanNo ratings yet
- Multiple SclerosisDocument6 pagesMultiple SclerosisRonnel Alvin Antonio AdrianoNo ratings yet
- Intravenous InfusionDocument35 pagesIntravenous InfusionDael GerongNo ratings yet
- A Comparative Clinical Study To Evaluate The Efficacy of Koshataki Ksharasutra in The Management of Bhagandara With Special Reference To Fistula in AnoDocument7 pagesA Comparative Clinical Study To Evaluate The Efficacy of Koshataki Ksharasutra in The Management of Bhagandara With Special Reference To Fistula in AnoEditor IJTSRDNo ratings yet
- Epidemics and PandemicsDocument36 pagesEpidemics and PandemicsRusu CristianaNo ratings yet
- Care Plan - Ineffective MobilityDocument10 pagesCare Plan - Ineffective MobilityAshley ToppNo ratings yet
- Music and Therapy Bun2Document17 pagesMusic and Therapy Bun2PanteaAlisaNo ratings yet
- Medical Device Risk Classification GuidanceDocument36 pagesMedical Device Risk Classification GuidanceGina ArcNo ratings yet
- New Report in The Treatment of Breast Cancer MastectDocument2 pagesNew Report in The Treatment of Breast Cancer MastectGil LedermanNo ratings yet
- Spray and Stretch TechDocument2 pagesSpray and Stretch TechrahulphysioNo ratings yet
- Induction Agents For Rapid Sequence Intubation in Adults For Emergency Medicine and Critical Care - UpToDateDocument27 pagesInduction Agents For Rapid Sequence Intubation in Adults For Emergency Medicine and Critical Care - UpToDateignacia.conejerosNo ratings yet
- Anestesi RecordDocument1 pageAnestesi RecordWelmi Sulfatri IshakNo ratings yet
- Wound Dressing Checklist SKL 112 FINAL EDITDocument5 pagesWound Dressing Checklist SKL 112 FINAL EDITCamille GuintoNo ratings yet
- Ayushman Bharat YojanaDocument28 pagesAyushman Bharat YojanaParth VasaveNo ratings yet
- Distal Tibial Fractures Intramedullary NailingDocument8 pagesDistal Tibial Fractures Intramedullary NailingasdaadNo ratings yet
- Health Problem Addressed: Umdns GMDNDocument1 pageHealth Problem Addressed: Umdns GMDNHaerul ImamNo ratings yet
- Breast Cancer Concept MapDocument2 pagesBreast Cancer Concept MapMaria Cristina100% (1)
- Malaria in ChildrenDocument19 pagesMalaria in ChildrenAngel Ellene MarcialNo ratings yet
- Translate These Into Communicative EnglishDocument2 pagesTranslate These Into Communicative Englishjuwita lestariNo ratings yet
- Confidentiality and JusticeDocument3 pagesConfidentiality and JusticeRaseff Tesorero50% (2)
- Resume Sample For Xray TechDocument7 pagesResume Sample For Xray Techpfbhkvekg100% (1)
- The Common ColdDocument3 pagesThe Common ColdLalan ArdyanNo ratings yet
- Tepid SpongingDocument3 pagesTepid SpongingNrs Sani Sule MashiNo ratings yet
- Recognising Seriously Ill ChildrenDocument12 pagesRecognising Seriously Ill ChildrenNurul Aulia AbdullahNo ratings yet
- Pediatricians' Letter To LCS Superintendent Rocky HannaDocument2 pagesPediatricians' Letter To LCS Superintendent Rocky HannaWCTV Digital TeamNo ratings yet