Professional Documents
Culture Documents
Friess Etal 2012
Uploaded by
Ernesta Aulia ROriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Friess Etal 2012
Uploaded by
Ernesta Aulia RCopyright:
Available Formats
Published online on 11 January 2012 Lab Anim, doi: 10.1258/la.2011.
011084
Short Article
Premedication with meloxicam exacerbates intracranial haemorrhage in an immature swine model of non-impact inertial head injury
S H Friess1, M Y Naim1, T J Kilbaugh1, J Ralston2 and S S Margulies2
1 Department of Anesthesiology and Critical Care Medicine, The Childrens Hospital of Philadelphia, Philadelphia, PA 19104-4399, USA; 2Department of Bioengineering, University of Pennsylvania, Philadelphia, PA 19104-6321, USA Corresponding author: S S Margulies, Department of Bioengineering, University of Pennsylvania, 240 Skirkanich Hall, 210 South 33rd Street, Philadelphia, PA 19104-6321, USA. Email: margulie@seas.upenn.edu
Abstract
Meloxicam is a cyclo-oxygenase-2 (COX-2) preferential non-steroidal anti-inammatory drug with very effective analgesic and anti-inammatory effects in swine. Previous reports in piglets have demonstrated that meloxicam also inhibits COX-1 and reduces production of thromboxane signicantly. We use preinjury analgesia in our immature swine (3 5-day-old piglets) model of brain injury using rapid head rotations without impact. In 23 consecutive subjects we found that premedication with meloxicam (n 6) produced a signicantly higher mortality rate (5/6 or 83%) than buprenorphine (n 17, 1/17 or 6%, P , 0.02). On gross neuropathological examination of the meloxicam-treated swine, we observed massive subdural and subarachnoid bleeding which were not present in buprenorphine-premedicated animals. To our knowledge there are no previous reports in swine of increased bleeding or platelet inhibition associated with meloxicam administration and further research is needed to dene mechanisms of action in piglets. We caution the use of meloxicam in swine when inhibition of platelet aggregation might adversely affect renement of experimental research protocols, such as in stroke, trauma and cardiac arrest models.
Keywords: Swine, renement, meloxicam, bleeding, brain injury
Laboratory Animals 2012: 1 3. DOI: 10.1258/la.2011.011084
Swine have become a popular laboratory animal model for biomedical research. Swine have several advantages over small animal models for modelling human disease, including physiology and organ structure and maturation. Moreover, large animals offer the opportunity to use instrumentation designed for humans. Adequate anaesthesia and analgesia during and after procedures which may produce pain or discomfort must be provided. Analgesic drugs have various pharmacodynamic effects which may vary by species and age, and can affect study outcome measures. Two common classes of medications to provide analgesia to swine are opioids and non-steroidal anti-inammatory drugs (NSAIDs). Opioid analgesics can cause central nervous system depression and decreased respiratory drive, which may be undesirable side-effects in physiological studies. NSAIDs have the advantage of providing analgesia without these unwanted physiological sideeffects. NSAIDs provide analgesia by inhibiting the activity of cyclo-oxygenase (COX). COX is an enzyme that catalyses the conversion of arachidonic acid into prostaglandin-like
molecules. There are two important isoforms: COX-1 and COX-2. COX-1 inhibition by non-preferential NSAIDs disrupts normal gastrointestinal and platelet physiology. COX-1 within platelets is responsible for the production of prostaglandin H2 which in turn is converted into thromboxane A2 (TxA2). TxA2 plays a major role in platelet aggregation and clotting. To avoid the COX-1-dependent adverse effects, COX-2 preferential inhibitors have been developed. Meloxicam (Metacam, Boehringer Ingelheim Vetmedica, Inc, Ridgeeld, CT, USA) is a COX-2 preferential NSAID which is marketed for use in humans as well as several domestic species including swine. Previous studies of meloxicam administration in swine have reported COX-1 inhibition, but adverse bleeding side-effects have not been observed.1 3 We hypothesize that meloxicam in swine may result in increased intracranial bleeding and mortality rates in our model of traumatic brain injury and adversely affect renement of experimental research protocols. We have developed an immature swine model of nonimpact inertial head injury which produces detectable
Laboratory Animals 2012: 1 3
Copyright 2012 by the Laboratory Animals Limited
................................................................................................................................................
Laboratory Animals
neurobehavioural decits and in this communication we report our experience using two different analgesia plans; an opioid based (buprenorphine) compared with a COX-2 preferential NSAID (meloxicam).4 Of note, all protocols were approved by the Institute of Animal Care and Use Committee of the University of Pennsylvania. Under general anaesthesia (isourane 2 4%), 3 5-day-old farm piglets heads (n 23) were secured to a padded bite plate. Then using the HYGE pneumatic actuator, piglets experienced head rotations in the axial direction (160 200 rad/s).5,6 Rotational velocity was measured by an angular rate sensor (ATA Inc, Albuquerque, NM, USA) attached to the linkage of the sidearm. After the head rotation, animals were monitored for return of pinch reex and extubated and survived for several days for neurobehavioural outcome studies. Return of pinch reex usually occured on average 6 7 min after the head rotation, and animals were able to appropriately ambulate, vocalize and feed within 2 h of injury before being returned to general husbandry care.4,7 Neurobehavioural decits in visualbased problem-solving and open-eld behaviour were observed in injured animals compared with sham animals on post injury days 1 and 4 but resolved by post injury day 11.4 On neuropathological examination, we typically observed diffuse axonal injury (b-amyloid precursor protein immunohistochemistry), as well as scattered amounts of subarachnoid and subdural haemorrhage. Historically, we had previously premedicated animals with buprenorphine 0.02 mg/kg intramuscularly prior to injury with a low mortality rate (5 10%), but with the concerns of possible central nervous depression and alteration in physiology and respiratory drive, a switch was made to the NSAID, meloxicam. Six animals were premedicated with meloxicam 0.2 mg/kg intramuscularly, and we observed a mortality rate of 83% within 24 h following head rotation (Table 1). Meloxicam premedication was then discontinued in favour of buprenorphine for the next 17 consecutive subjects with a return to our expected mortality rate (1/17, 6%), despite no reduction in angular velocity of the head (Table 1). Gross neuropathological evaluation of the meloxicam-treated animals revealed massive subdural and subarachnoid bleeding with mass effect, whereas buprenorphine-treated animals had thin subdural and subarachnoid haemorrhage accumulations in the sulci. Due to the high early mortality rate of the meloxicam-treated group, we were unable to perfusion x the brains and compare axonal injury assessed by immunohistochemistry between the two groups. Meloxicam is marketed as a preferential COX-2 inhibitor. Human studies have demonstrated that meloxicam does inhibit TxA2 formation but not to signicant levels that alter in vivo platelet function or clotting
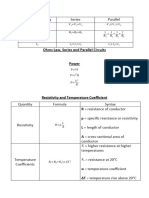
Table 1 Mortality and angular velocity of meloxicam and buprenorphine-treated piglets Meloxicam Mortality (%) Angular velocity (rad/s)
times.8 However, NSAID selectivity of COX isoform inhibition can be species dependent.9 Fosse et al.3 performed pharmacokinetic and pharmacodynamic studies of meloxicam in 2 3-week-old farm piglets. A carrageenan-sponge model of acute inammation was used to evaluate the effects of meloxicam. Animals received meloxicam 0.4 mg/ kg intravenously or saline vehicle. Exudate levels of prostaglandin E2 were measured as an indirect indicator of COX-2 activity and serum levels of thromboxane B2 (TxB2) as an indicator of COX-1 activity. Profound inhibition of TxB2 was observed for at least 8 h after administration of meloxicam, indicating strong inhibition of COX-1 in piglets.3 In another study, 2-month-old swine were challenged with endotoxin and randomized to treatment with meloxicam or placebo. TxB2 levels were found to be markedly reduced in meloxicam-treated animals compared with placebo.10 Unfortunately, no coagulation prole or platelet aggregation studies were performed in either study to determine if decreased TxB2 levels resulted in alterations in bleeding times or platelet aggregation. Our swine model may be more sensitive to smaller changes in platelet aggregation associated with COX-1 inhibition, due to the known clinical association of traumatic brain injury with coagulopathy.11 Our experience with meloxicam in our head injury model would corroborate the strong COX-1 inhibition by meloxicam in immature swine previously reported.3,10 Unlike the buprenorphine-premedicated animals, most of the meloxicam-treated piglets developed lethal massive intracranial haemorrhage after experiencing non-impact head rotation. We speculate that the unexpected lethal intracranial haemorrhage was the result of meloxicam inhibition of COX-1, resulting in decreased TxA2 levels, and reduction in platelet aggregation. Although meloxicam appears to have higher selectivity for COX-2 inhibition, its COX-1 selectivity is not trivial.3 We caution the use of meloxicam in swine when inhibition of platelet aggregation might adversely affect renement of experimental research protocols, such as in stroke, trauma and cardiac arrest models. Further research is needed to dene meloxicams effects in swine on bleeding and platelet aggregation.
ACKNOWLEDGEMENTS
This work was supported by National Institutes of Health K08-NS064051 (SHF); Thrasher Research Foundation New Investigator Award (MYN); and National Institutes of Health R01 NS39679 (SSM).
REFERENCES 1 Reyes L, Tinworth KD, Li KM, Yau DF, Waters KA. Observer-blinded comparison of two nonopioid analgesics for postoperative pain in piglets. Pharmacol Biochem Behav 2002;73:521 8 2 Busch U, Schmid J, Heinzel G, et al. Pharmacokinetics of meloxicam in animals and the relevance to humans. Drug Metab Dispos 1998;26:576 84 3 Fosse TK, Haga HA, Hormazabal V, Haugejorden G, Horsberg TE, Ranheim B. Pharmacokinetics and pharmacodynamics of meloxicam in piglets. J Vet Pharmacol Ther 2008;31:246 52 4 Friess SH, Ichord RN, Owens K, et al. Neurobehavioral functional decits following closed head injury in the neonatal pig. Exp Neurol 2007;204:234 43
Buprenorphine 1/17 (6%) 194.3 + 6.9
5/6 (83%) 187.2 + 6.7
P , 0.02 by chi-square test, P 0.06 by Students t-test
................................................................................................................................................
Friess et al. Meloxicam exacerbates intracranial haemorrhage in swine
5 Raghupathi R, Margulies SS. Traumatic axonal injury after closed head injury in the neonatal pig. J Neurotrauma 2002;19:843 53 6 Raghupathi R, Mehr MF, Helfaer MA, Margulies SS. Traumatic axonal injury is exacerbated following repetitive closed head injury in the neonatal pig. J Neurotrauma 2004;21:307 16 7 Naim MY, Friess S, Smith C, et al. Folic acid enhances early functional recovery in a piglet model of pediatric head injury. Dev Neurosci 2010;32:466 79 8 Rinder HM, Tracey JB, Souhrada M, Wang C, Gagnier RP, Wood CC. Effects of meloxicam on platelet function in healthy adults: a randomized, double-blind, placebo-controlled trial. J Clin Pharmacol 2002;42:881 6
9 Brideau C, Van Staden C, Chan CC. In vitro effects of cyclooxygenase inhibitors in whole blood of horses, dogs, and cats. Am J Vet Res 2001;62:1755 60 10 Friton GM, Schmidt H, Schrodl W. Clinical and anti-inammatory effects of treating endotoxin-challenged pigs with meloxicam. Vet Rec 2006;159:552 7 11 Halpern CH, Reilly PM, Turtz AR, Stein SC. Traumatic coagulopathy: the effect of brain injury. J Neurotrauma 2008;25:997 1001
(Accepted 20 November 2011)
You might also like
- WHO. Hearing Aids GuidelineDocument38 pagesWHO. Hearing Aids GuidelineErnesta Aulia RNo ratings yet
- Acces Economic. The ECONOMIC IMPACT and COST of Hearing Loss in AustraliaDocument97 pagesAcces Economic. The ECONOMIC IMPACT and COST of Hearing Loss in AustraliaErnesta Aulia RNo ratings yet
- SSNHLDocument14 pagesSSNHLErnesta Aulia RNo ratings yet
- Pathophysiology of The Ear - HansenDocument16 pagesPathophysiology of The Ear - HansennavhospihNo ratings yet
- Michelle Meyer, BS, Karie Vander Werf, DVM, Beth Davis, DVM, PHD, Dacvim, Butch Kukanich, DVM, PHD, DacvcpDocument1 pageMichelle Meyer, BS, Karie Vander Werf, DVM, Beth Davis, DVM, PHD, Dacvim, Butch Kukanich, DVM, PHD, DacvcpErnesta Aulia RNo ratings yet
- Con 018086Document41 pagesCon 018086Juan GabrielNo ratings yet
- NICE Guidelines PDFDocument37 pagesNICE Guidelines PDFKahubbi Fatimah Wa'aliyNo ratings yet
- S 022 LBLDocument13 pagesS 022 LBLErnesta Aulia RNo ratings yet
- Lancet Neurology 2010 KumarDocument14 pagesLancet Neurology 2010 KumarErnesta Aulia RNo ratings yet
- NosebleedsDocument9 pagesNosebleedsErnesta Aulia RNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- An Appraisal of The Literature On Centric Relation. Part II: ReviewDocument11 pagesAn Appraisal of The Literature On Centric Relation. Part II: ReviewManjulika TysgiNo ratings yet
- Under Pass Wing Wall (4.1m)Document12 pagesUnder Pass Wing Wall (4.1m)Naveed NazNo ratings yet
- Calabano Clinical Bacteriology Exercise 1Document5 pagesCalabano Clinical Bacteriology Exercise 1MarkJasperCalabanoNo ratings yet
- Tech Manual 1396 Rev. B: 3.06/4.06" 15,000 Psi ES BOPDocument39 pagesTech Manual 1396 Rev. B: 3.06/4.06" 15,000 Psi ES BOPEl Mundo De Yosed100% (1)
- EET - Formulas - Christmas TermDocument3 pagesEET - Formulas - Christmas TermJMDNo ratings yet
- CADS Revit Scia Engineer Link Best PracticesDocument32 pagesCADS Revit Scia Engineer Link Best PracticestrevorNo ratings yet
- Zetor Crystal 150 170 Tractor Operator Manual PDFDocument234 pagesZetor Crystal 150 170 Tractor Operator Manual PDFAntonNo ratings yet
- Flash Memoir RevisedDocument3 pagesFlash Memoir Revisedapi-511179803No ratings yet
- Diesel Rotary UPS Configurations V1 - 00 - Jan2008Document10 pagesDiesel Rotary UPS Configurations V1 - 00 - Jan2008Karim SenhajiNo ratings yet
- Genie Z45/22Document58 pagesGenie Z45/22jonny david martinez perezNo ratings yet
- Dinacharya HandbookDocument5 pagesDinacharya Handbookvera sirakovaNo ratings yet
- Color Codes and Irregular MarkingDocument354 pagesColor Codes and Irregular MarkingOscarGonzalezNo ratings yet
- VAM Must Sumitomo 1209 PDFDocument4 pagesVAM Must Sumitomo 1209 PDFnwohapeterNo ratings yet
- Electric Bike Monitoring and Controlling System Based On Internet of ThingsDocument8 pagesElectric Bike Monitoring and Controlling System Based On Internet of ThingsEarl PhamtonhiveNo ratings yet
- Streamline SWR (S) - Rev - 00-04-2019 PDFDocument2 pagesStreamline SWR (S) - Rev - 00-04-2019 PDFarjun 11No ratings yet
- Ays 082914 3331 PDFDocument18 pagesAys 082914 3331 PDFFabian R. GoldmanNo ratings yet
- Chemistry NotesDocument11 pagesChemistry Notesraifaisal9267% (12)
- Varaah KavachDocument7 pagesVaraah KavachBalagei Nagarajan100% (1)
- Advanced Steel Structure Concepts: 2 MonthsDocument4 pagesAdvanced Steel Structure Concepts: 2 MonthsAnkit SoniNo ratings yet
- Soal Bahasa Inggris X - XiDocument6 pagesSoal Bahasa Inggris X - XiBydowie IqbalNo ratings yet
- Class 28: Outline: Hour 1: Displacement Current Maxwell's Equations Hour 2: Electromagnetic WavesDocument33 pagesClass 28: Outline: Hour 1: Displacement Current Maxwell's Equations Hour 2: Electromagnetic Wavesakirank1No ratings yet
- Daphne Alpha Cleaner Series: Lubricant Product InformationDocument2 pagesDaphne Alpha Cleaner Series: Lubricant Product InformationChart ChNo ratings yet
- Chemistry Mid Term Exam 2014Document8 pagesChemistry Mid Term Exam 2014Adham TamerNo ratings yet
- Kiss Forex How To Trade Ichimoku PDFDocument72 pagesKiss Forex How To Trade Ichimoku PDFSastryassociates Chartered100% (3)
- Karan AsDocument3 pagesKaran AsHariNo ratings yet
- In Truth To Mollusca According To New Studies by J RutherfordDocument4 pagesIn Truth To Mollusca According To New Studies by J RutherfordbalaiNo ratings yet
- Recetario TransistoresDocument23 pagesRecetario TransistoresTitán SotoNo ratings yet
- Working at Heights GuidelineDocument15 pagesWorking at Heights Guidelinechanks498No ratings yet
- CAT25256 EEPROM Serial 256-Kb SPI: DescriptionDocument22 pagesCAT25256 EEPROM Serial 256-Kb SPI: DescriptionPolinho DonacimentoNo ratings yet
- Leta-Leta CaveDocument5 pagesLeta-Leta CaveToniNo ratings yet