Professional Documents
Culture Documents
Symptomatology
Uploaded by
Roxanne Ganayo ClaverOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Symptomatology
Uploaded by
Roxanne Ganayo ClaverCopyright:
Available Formats
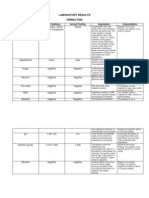
SYMPTOMATOLOGY CLINICAL MANIFESTATIONS 1. Dizziness Dizziness is a common occurrence before or after stroke.
It is particularly common with brainstem ACTUAL FINDINGS IMPLICATIONS
stroke. Decreased blood flow in the back of the brain, vertebrobasilar insufficiency the blood vessels leading to the called
brain from the heart may be blocked (known as
atherosclerosis) causes (Swenson, 2008) 2. Speech problems Problems were a with common
which dizziness.
speech early
symptom of a stroke. This was usually due to
weakness of the muscles
that are crucial for speech production on one side of the face. (Health Talk,
2014) 3. Confusion Confusion is a common problem before or after a stroke. When different
areas of the brain are damaged, the pathways
that control thoughts and behaviors can become
jumbled. Stroke confusion is different for everyone, depending on where in the brain place. the It stroke can from takes range difficulty
anywhere
understanding speech to a lack of judgment about serious safety issues.
(Jacques, 2010) 4. Blurred or double vision Visual problems are more common in people who
have
suffered
stroke
affecting the right side of their brain. The damage the stroke does in the brain impacts the visual
pathways of the eye which can result in visual field loss, blurry vision, double vision and moving images. When stroke affects the areas of the brain that processes the information we see, it can cause 'visual neglect' (lack of awareness to one half of the body or space) difficulties as with well as
judging
depth and movement. In a few cases, visual problems caused by stroke can
improve on their own with time. (RNIB, 2012) 5. Sudden severe The other major site of
headache
trouble, the basilar artery, is formed at the base of the skull from the vertebral arteries, which run up
along the spine and join at the back of the head. When stroke or TIAs occur here, both hemispheres of the brain may be affected so that symptoms occur on both sides of the body such as a sudden severe headache. (Simon, 2008) 6. Sudden loss of coordination or problems with balance Loss of coordination on one side of the body. While your limb may be strong, you may not have the coordination something to you do were
before, such as hold a spoon or button a clasp. In rare cases a body part may develop abnormal,
spontaneous movements. (Pressman, 2012) 7. Sudden numbness and weakness Numbness typically occurs on one side of the body, opposite the side of the brain affected by the
stroke. (Caplan, 2007)
ETIOLOGY PREDISPOSING FACTORS CLINICAL MANIFESTATIONS 1. Vices (Alcohol, smoke) Smoking doubles the risk for stroke when compared to a nonsmoker. It reduces the amount of oxygen in the blood, causing the ACTUAL FINDINGS IMPLICATIONS
heart to work harder and allowing blood clots to form more easily. Smoking also increases the amount of build-up in the arteries, which may block the flow
of
blood
to
the
brain,
causing a stroke. Drinking three or more alcoholic beverages a day may raise the risk for spontaneous intracerebral hemorrhage
at a much younger age than typical, researchers found. (National Stroke
Association, 2003) 2. Age For each decade of life after age 55, the chance of having a stroke more than doubles. (American Heart Association, 2006) 3. Diet A poor diet is a major risk factor for a stroke. High-fat foods can lead to the buildup of fatty plaques in your arteries and being
overweight can lead to high blood pressure (NHS Choices, 2012)
4. Sex
Stroke incidence rates are 1.25 times greater in men, but because women tend to live longer than men, more women than men die of stroke each year. ( American Association, 2003) Heart
5. Heredity
The chance of stroke is greater in people who have a family history of stroke. (American Association, 2004) Heart
PRECIPITATING FACTORS CLINICAL MANIFESTATIONS 1. Hypertension The most important ACTUAL FINDINGS IMPLICATIONS
controllable risk factor for stroke (brain attack) is
controlling pressure higher).
high (140/90 High
blood or blood
pressure blood
can vessels
damage (called
arteries) that supply blood to the brain. According to the CDC, reducing the
systolic (or top number) blood pressure by 12 to 13 points can decrease the risk for a stroke by 37%. (John Hopkins Medical
Health Library, 2009) 2. Diabetes Mellitus Diabetes is controllable,
but having it increases the risk for stroke. People with diabetes have 2 to 4 times the risk of having a stroke than someone without
diabetes. Blood pressure for people with diabetes should be 130/80 or less to reduce the risk of stroke. (John Hopkins Medical
Health Library, 2008)
3. Heart diseases
Heart
disease
is
the
second most important risk factor for stroke, and the major cause of death
among survivors of stroke. Heart disease and stroke have many of the same risk factors. (John Hopkins Medical 2008) 4. Cardiac structural abnormalities Damaged heart valves can cause damage, chronic which heart can Health Library,
ultimately increase the risk of developing stroke. This is known as valvular heart disease. New evidence
shows that heart structure abnormalities including
patent foramen ovale and atrial septal defect may possibly increase risk for embolic stroke. (John
Hopkins
Medical
Health
Library, 2012) 5. Atherosclerosis Stroke secondary to
atherosclerosis about 2 out of
affects 1,000
people, or approximately 50% of all those who have strokes. Atherosclerosis (hardening of the arteries) sticky, occurs fatty
when
substances called plaque buildup in the inner lining of the arteries. The plaque may slowly block or narrow an artery or trigger a clot (thrombus). Clots can lead to stroke. (John Hopkins Medical 2008) Health Library,
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Chater 5 The Role of ProbabilityDocument11 pagesChater 5 The Role of ProbabilityShruti Mangal100% (6)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- FDARDocument2 pagesFDARRoxanne Ganayo ClaverNo ratings yet
- Personality PowerpointDocument49 pagesPersonality Powerpointapi-240281479No ratings yet
- Peplau's Theory of Interpersonal Relations: An Alternate Factor Structure For Patient Experience Data?Document9 pagesPeplau's Theory of Interpersonal Relations: An Alternate Factor Structure For Patient Experience Data?Rila LuaduNo ratings yet
- Jay Allen Marc J. SabandalDocument3 pagesJay Allen Marc J. SabandalRoxanne Ganayo ClaverNo ratings yet
- CV MaelDocument1 pageCV MaelRoxanne Ganayo ClaverNo ratings yet
- Tila INFANT Kung MaglaroDocument4 pagesTila INFANT Kung MaglaroRoxanne Ganayo ClaverNo ratings yet
- Monday Tuesday Wednesday Thursday Friday Saturday SundayDocument12 pagesMonday Tuesday Wednesday Thursday Friday Saturday SundayRoxanne Ganayo ClaverNo ratings yet
- Final CsDocument92 pagesFinal CsRoxanne Ganayo ClaverNo ratings yet
- 10.) Head Nurse Structured ProgramDocument4 pages10.) Head Nurse Structured ProgramRoxanne Ganayo ClaverNo ratings yet
- Joanne G. Ediong: Owner, RO Abella BrokerageDocument1 pageJoanne G. Ediong: Owner, RO Abella BrokerageRoxanne Ganayo ClaverNo ratings yet
- The Social Support and Self-Image of The Students of Tagum Doctors College IncDocument4 pagesThe Social Support and Self-Image of The Students of Tagum Doctors College IncRoxanne Ganayo ClaverNo ratings yet
- Ncp-Ineffective Breathing PatternDocument4 pagesNcp-Ineffective Breathing PatternRoxanne Ganayo Claver100% (1)
- Ms. Kenji Casul: Head, HRDDocument1 pageMs. Kenji Casul: Head, HRDRoxanne Ganayo ClaverNo ratings yet
- Will, End-Oflife Of: Kron L - Nllons. IivingDocument12 pagesWill, End-Oflife Of: Kron L - Nllons. IivingRoxanne Ganayo ClaverNo ratings yet
- ) With A Reading Capability of 780 NM Wavelength (Infrared and Red Edge) Semiconductor Laser, 1200 Kib/s (1×) - While USB Has A Capability of UpDocument1 page) With A Reading Capability of 780 NM Wavelength (Infrared and Red Edge) Semiconductor Laser, 1200 Kib/s (1×) - While USB Has A Capability of UpRoxanne Ganayo ClaverNo ratings yet
- Nursing Care Plan #3 DAT E& Shif T Assessment Nursing Diagnosis Need S Planning Intervention Rationale EvaluationDocument2 pagesNursing Care Plan #3 DAT E& Shif T Assessment Nursing Diagnosis Need S Planning Intervention Rationale EvaluationRoxanne Ganayo ClaverNo ratings yet
- Assessment A. Biographical DataDocument5 pagesAssessment A. Biographical DataRoxanne Ganayo ClaverNo ratings yet
- Generic Name: Co-Amoxiclav Brand Name: Augmentin Classification: Dosage: 625 MGDocument6 pagesGeneric Name: Co-Amoxiclav Brand Name: Augmentin Classification: Dosage: 625 MGRoxanne Ganayo ClaverNo ratings yet
- NCP Intra FinalDocument7 pagesNCP Intra FinalRoxanne Ganayo ClaverNo ratings yet
- Laboratory ResultsDocument4 pagesLaboratory ResultsRoxanne Ganayo ClaverNo ratings yet
- Aluminium: Aluminium (Or Aluminum) Is A Chemical Element in The Boron Group With Symbol Al and Atomic Number 13. ItDocument2 pagesAluminium: Aluminium (Or Aluminum) Is A Chemical Element in The Boron Group With Symbol Al and Atomic Number 13. ItRoxanne Ganayo ClaverNo ratings yet
- Deborah Bartz, M.D. Massachusetts Reprimand On ProfileDocument2 pagesDeborah Bartz, M.D. Massachusetts Reprimand On ProfileAnonymous 8m05a5No ratings yet
- Psyche ReviewerDocument13 pagesPsyche ReviewerKem100% (1)
- Ebp Presentation 1Document21 pagesEbp Presentation 1api-340248301No ratings yet
- Aquilion ONE GENESIS Edition Transforming CTDocument40 pagesAquilion ONE GENESIS Edition Transforming CTSemeeeJuniorNo ratings yet
- Guidelines of An Effective Interview and Ethico-Legal ConsiderationsDocument37 pagesGuidelines of An Effective Interview and Ethico-Legal ConsiderationsSherinne Jane CariazoNo ratings yet
- Anxiety Dissorder PDFDocument273 pagesAnxiety Dissorder PDFdnaNo ratings yet
- PRC Form (Minor Operation)Document1 pagePRC Form (Minor Operation)mawelNo ratings yet
- Atropine Drug StudyDocument3 pagesAtropine Drug StudyMaej83% (6)
- Imran Ahmad Sajid-Medical Social Work in Lady Reading Hospital, Peshawar, PakistanDocument52 pagesImran Ahmad Sajid-Medical Social Work in Lady Reading Hospital, Peshawar, PakistanimranahmadsajidNo ratings yet
- Jurnal Rujukan KuesionerDocument10 pagesJurnal Rujukan KuesionerMiss BerlyantiNo ratings yet
- Hands On: The Approach To The Patient Presenting With Multiple Joint PainDocument12 pagesHands On: The Approach To The Patient Presenting With Multiple Joint PainMithun CbNo ratings yet
- Aus Endod J April 2012-31-35 PDFDocument5 pagesAus Endod J April 2012-31-35 PDFlupusebastianNo ratings yet
- Surgery Department: Emergency Case ReportsDocument46 pagesSurgery Department: Emergency Case ReportsMohamad ZulfikarNo ratings yet
- Survival of The Sickest Presentation 1Document21 pagesSurvival of The Sickest Presentation 1api-296981910No ratings yet
- Empyema CPGDocument8 pagesEmpyema CPGLe Vu AnhNo ratings yet
- Hematology - Oncology GlossaryDocument18 pagesHematology - Oncology GlossaryFran CescaNo ratings yet
- Insomnia and Vivid Dreaming in Chinese Medical Thinking: by Heiner FruehaufDocument5 pagesInsomnia and Vivid Dreaming in Chinese Medical Thinking: by Heiner FruehaufRomi BrenerNo ratings yet
- Indirect Patient Duty oDocument5 pagesIndirect Patient Duty oJiansong ChangNo ratings yet
- Janumet PM eDocument62 pagesJanumet PM eRaffi DerderianNo ratings yet
- Treatment of Hyperthyroidism by Traditional Medicine TherapiesDocument3 pagesTreatment of Hyperthyroidism by Traditional Medicine TherapiesPirasan Traditional Medicine CenterNo ratings yet
- Retinopathy of PrematurityDocument15 pagesRetinopathy of Prematuritymarissa ulkhairNo ratings yet
- Ewout JasperDocument400 pagesEwout JasperJohnny AtmanNo ratings yet
- First Aid Pharmacology AntimicrobialsDocument23 pagesFirst Aid Pharmacology AntimicrobialsLaura Lopez RocaNo ratings yet
- Chapter 19Document16 pagesChapter 19missy23pap100% (1)
- Therapy in TuberculosisDocument4 pagesTherapy in TuberculosisSamir SkejicNo ratings yet
- Prevention of Needle Stick and Sharp Injuries During Clinical Training Among Undergraduate Nursing Students: Effect of Educational ProgramDocument14 pagesPrevention of Needle Stick and Sharp Injuries During Clinical Training Among Undergraduate Nursing Students: Effect of Educational ProgramIOSRjournalNo ratings yet
- Esr Check ListDocument8 pagesEsr Check ListMona Ismail AlsomaliNo ratings yet