Professional Documents
Culture Documents
Case Pres Block 2
Uploaded by
Jon Adam Bermudez SamatraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Pres Block 2
Uploaded by
Jon Adam Bermudez SamatraCopyright:
Available Formats
I. OVERVIEW OF THE DISEASE Infection of a knee joint is a very serious medical condition.
A septic (infected) knee is most often caused by bacteria (such as staph or strep), but in rare instances can be caused by other microorganisms. Prompt diagnosis and treatment is essential in the native knee to avoid rapid destruction of the cartilage and bone in the knee. When diagnosed early, treatment is usually arthroscopic irrigation and debridement. However, an open debridement may be required. Despite early diagnosis and treatment, joint destruction may still occur. Late effects of joint infection (septic arthritis) may require treatment with joint replacement as long as there is no persistent infection remaining within the knee. While joint infection occasionally affects people with no known predisposing risk factors, it more commonly occurs when certain risk situations are present. Risks for the development of septic arthritis include diabetic patient, trauma such as injury or wound, bacteria/microorganism, drug use, alcoholism, kidney dialysis, malnutrition, advanced age, orthopaedic surgery Signs and Symptoms of Septic Arthritis include bone pain, swelling and redness of the skin, fatigue, general discomfort or ill feeling and drainage of pus through the skin.
II. PATIENTS PROFILE Name: Patient X Address: #52 2nd West Crame, Brgy. San Juan, San Juan City Date Admitted: May 31, 2011 Admitting Diagnosis: Septic knee, ankle, 1st MT right foot Principal Diagnosis: Septic knee, ankle, 1st MT right foot Chief Complaint: Swelling right knee, ankle and foot Principal Operation Procedure: Aspiration of knee, ankle, MT right foot III. PATIENT HISTORY Case Study: Septic Knee, Ankle, 1st MT Right Foot
History of Present Illness/Injury
Patient X is a 8 year old boy who was admitted last May 31, 2011, 3 weeks prior to consultation, patient X hit his right big toe while playing football with (+) manipulation done 3 times and (+) swelling persisted with involvement/swelling of right ankle noted and (+) fever noted.
Past Medical History
Vomited and treated
Family Medical History
Uncle (father side): (+) Explore Laparotomy due to Acute Appendicitis with Generalized Peritonitis Grandmother (mother side): (+) Hypertension with maintenance antihypertensive drugs Grandmother (father side): (+) Diabetes Mellitus Both parents: Deceased due to vehicular accident
Socioenomic History
Patient X was on his 4th grade. Both parents are deceased due to vehicular accident, there were six in the family and he was the youngest, their auntie is the one who support their needs, work as a Brgy. Health Worker with the monthly income of P3,000.
IV. ANATOMY AND PHYSIOLOGY The knee joint joins the thigh with the leg and consists of two articulations: one between thefemur and tibia, and one between the femur and patella. It is the largest joint in the human body and is very complicated. The knee is a mobile trocho-ginglymus (i.e. a pivotal hinge joint), which permits flexion and extension as well as a slight medial and lateral rotation. Since in humans the knee supports nearly the whole weight of the body, it is vulnerable to both acute injury and the development of osteoarthritis. The ankle joint is formed where the foot and the leg meet. The ankle, ortalocrural joint, is a synovial hinge joint that connects the distal ends of the tibia and fibulain the lower limb with the proximal end of the talus bone in the foot. The articulation between the tibia and the talus bears more weight than between the smaller fibula and the talus. The metatarsus or metatarsal bones are a group of five long bones in the foot located between the tarsal bones of the hind- and mid-foot and the phalanges of the toes. Lacking individual names, the metatarsal bones are numbered from the medial side (side of big toe): the first, second, third, fourth, and fifth metatarsal. The metatarsals are analogous to themetacarpal bones of the hand.
Case Study: Septic Knee, Ankle, 1st MT Right Foot
Normal Abnormal
Case Study: Septic Knee, Ankle, 1st MT Right Foot
V. PATHOPHYSIOLOGY Predisposing factors: Modifiable: Compromised Immune system Invasive procedures (catheter insertion, etc.) Unsafe sex IV drug abuse Bacterial infections already present in the body Trauma Non Modifiable: Age extremes Trauma
ove
Manipulation
Tissue damage
Exposure of joints
Entrance of microorganism to synovial membrane
Growth of microorganism Infection of metatarsal (R) foot
Hematogenous spread Case Study: Septic Knee, Ankle, 1st MT Right Foot
Infection of ankle and knee (R) foot
Inflammatory response: Pain Swelling Redness Heat Loss of function
Potts Disease Risk Factor : Poor Environmental Sanitation, Living in a congested area, Trauma: Fall
MYCOBACTERIUM TUBERCLE BACILLI
Lungs
Circulation
the infection spread to the two adjacent vertebrae into the adjoining disk space
back pain, anorexia, night sweats, weight loss
Case Study: Septic Knee, Ankle, 1st MT Right Foot
mycobacterium tubercle bacilli spread into the thoracic vertebra of the spine
VI. PHYSICAL EXAMINATION
Procedure
1. Monitor Temperature 2. Monitor Pulse Rate 3. Monitor Respiration Rate 4. Monitor Apical Pulse Rate 5. Skin 6. Hair 7. Eyes 8. External Ear 9. Internal Ear 10. External Nose 11. Sinuses 12. Lips 13. Tongue 14. Gums 15. Teeth
Technique
Using thermometer Palpation Observation Auscultation Inspection Inspection Inspection Inspection Inspection Inspection Palpation Inspection Inspection Inspection Inspection
Normal Findings
35.6-37.7 C 70-100 BPM 20-28 BPM 60-100 BPM Pink, smooth, turgor present Lustrous and shiny Clear, moist surfaces, transparent cornea Non-tender auricle, tragus Free from any discharge Color same as face, smooth and symmetrical appearance Non-tender upon palpation Pink, smooth, moist Deep red with papillae Smooth, firm, pink Straight with no cavities
Actual Findings
Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal With missing upper central and lateral incisor Normal
Interpretation
Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Abnormal
Analysis
Not related to the case, the patient was at his deciduous teeth extraction
16. Neck
Inspection
17. Thyroid
Inspection/Palpation
Smooth, controlled movements, ROM flexion 45 , extension 55 , lateral abduction 40 , rotation 70 Midline, smooth, firm, non-
Normal
Normal
Normal
Case Study: Septic Knee, Ankle, 1st MT Right Foot
18. Trachea 19. Abdomen 20. Umbilicus 21. Bowel Sounds 22. Extremities 23. Nails 24. Peripheral Pulses 25. Carotid Arteries 26. Temporal Arteries 27. ROM -Cervical Spine -Elbow -Wrist
Inspection Inspection Inspection Auscultation Inspection Inspection Palpation Palpation Palpation Inspection/Observation Inspection/Observation Inspection/Observation
tender Midline position, symmetrical, landmarks identifiable Rounded or flat Sunken, centrally located 2 or 3 times/minute Fair color over the body, warm to touch Pinkish nail beds. Nail firm Bilateral pulses strong and equal Palpable, equal and strong Palpable, equal and strong Flexion/extension 45 Lateral Bending 40 Flexion 160 Extension 180 Pronation/Supination 90 Flexion/Hypertension 90 Ulnar deviation 55 Radial deviation 20 Flexion 90 Hyperextension 20 Dorsiflexion 20
Normal Normal Protrude Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Normal Limited ROM
Normal Normal Abnormal Normal Normal Normal Normal Normal Normal Normal Case Study: Septic Knee, Ankle, 1st MT Right Foot Normal Normal Normal Normal Normal Normal Normal Normal Abnormal Poor nutritional status
-Fingers -Ankles
Inspection/Observation Inspection/Observation
Plantar flexion 45
Limited ROM
Abnormal
Due to accumulation of microorganism in the area, swelling occurs thus causing pain when moving Due to accumulation of
Eversion 20
Limited ROM
Abnormal
Inversion 30
Limited ROM
Abnormal
Abduction 10
Limited ROM
Abnormal
Adduction 20
Limited ROM
Abnormal
Case Study: Septic Knee, Ankle, 1st MT Right Foot
microorganism in the area, swelling occurs thus causing pain when moving Due to accumulation of microorganism in the area, swelling occurs thus causing pain when moving Due to accumulation of microorganism in the area, swelling occurs thus causing pain when moving Due to accumulation of microorganism in the area, swelling occurs thus causing pain when moving Due to accumulation of microorganism in the area, swelling occurs thus causing pain when moving
VII. DIAGNOSTIC TEST
Test Name
Actual Findings
May 31, 2011 71 0.23 11.50 0.38 0.51 0.06 0.05 688 70 22 31 40.58 U/L 34.34 U/L August 3, 2011 CS: No growth after 72 hours of incubation GS: RBC: +++, WBC; few gram (+) cocci seen singly; No spore-forming bacilli seen August 31, 2011 92 0.28 8.80 0.21 0.64 0.08 0.07 511 82 27 33
Normal Findings
Interpretation
May 31 August 31 Low Low Normal Normal Normal High High High Normal Low
Clinical significance of this test
To provide valuable information about the blood and to some extent the bone marrow, which is the bloodforming tissue. To monitor the platelet and WBC count for patient with infection.
Hematology
Chemistry SGOT SGPT
<37. 00 U/L <42.00 U/L No growth and free from any kind of microorganisms and/or bacteria
High Normal Abnormal (few gram (+) cocci seen singly)
Culture and Sensitivity; Gram Staining
To determine drugs effect taken by the patient thus causing cholestasis and other hepato toxicity. To identify the bacteria or fungi that normally populate in the patients wound.
Case Study: Septic Knee, Ankle, 1st MT Right Foot
Hemoglobin Mass Hematocrit Leukocyte Differential Count Lymphocytes Segmenters Monocytes Eosinophils Platelet Count Indices MCV MCH MCHC
127-183 g/L 0.37-0.54 4.5 - 10 x 10 9/L 0.20-0.40 0.50-0.70 0.00-0.07 0.00-0.05 150-400 x 10 g/L 82-92 fl 28-32 pg 32-38 %
Low Low High Normal Normal Normal Normal High Low Low Low
Chest X-ray
VIII. MEDICAL MANAGEMENT
Management
Medication
Focus
Antibiotic Therapy Anti-tuberculosis drugs NSAIDS High calorie, High protein, High calcium diet
Clinical significance of this management
To eradicate and prevent the multiplication of infectious microorganisms To eradicate the Mycobacterium tubercle bacilli To relieve the pain To regain the energy lost, to achieve normal body weight, to promote adequate calcification of the bone and bone remodelling and healing To prevent paresthesia
Nutrition
Exercise
Isometric exercise in the unaffected part
10
Case Study: Septic Knee, Ankle, 1st MT Right Foot
June 3, 2011 CS: No growth after 72 hours of incubation GS: a.) RBC: few; no microorganism seen; No spore-forming bacilli seen b.) RBC: few; WBC: rare; No microorganism seen; No spore-forming bacilli seen; No acid fast bacilli seen. -lung marking are prominent -some enlarged hilar and transbronchial lymphodes are noted -heart is not enlarged -diaphragm and sulci are intact Impression: Findings may relate to primary Kochs infection.
A normal chest x ray will show normal structures for the age and medical history of the patient.
Abnormal (some enlarged hilar and transbronchial lymphodes are noted)
To evaluate organs and structures within the chest for symptoms of disease. To determine the extent of microorganism to this part.
Blood transfusion
PRBC, FWB
PRBC: For OR (Arthrostomy) used To compensate the decrease result of CBC
IX. SURGICAL MANAGEMENT
Procedures Name
Arthrotomy and Debridement
Actual Finding
The specimen consists of several, irregular, pale red to tan-brown, soft tissue fragments with an aggregate measurement of 5x4x1.5 m and labeled as intracapsular. Received specimen in a vial containing yellow, blood tinged fluid with clots, approximately 8.0 ml in volume
Clinical significance of this procedure
To remove the patient's dead, damaged, or infected tissue to improve the healing potential of the remaining healthy tissue. To examine bone marrow, the spongy liquid part of the bone where blood cells are made.
Aspiration of right knee, ankle, and big toe
11
Case Study: Septic Knee, Ankle, 1st MT Right Foot
X. DRUG STUDY
Generic Name
Ibuprofen
Brand Name
Advil
Action
Unknown. May inhibit prostaglandin synthesis, to produce antiinflammatory, analgesic, and antipyretic effects.
Indication
Ibuprofen contains the active ingredient ibuprofen, which belongs to a group of medicines called non-steroidal anti-inflammatory drugs (NSAIDs). It works by blocking the action of a substance in the body called cyclo-oxygenase. Cyclo-oxygenase is involved in the production of various chemicals in the body, some of which are known as prostaglandins. Prostaglandins are produced in response to injury or certain diseases and would otherwise go on to cause pain, swelling and inflammation. Ibuprofen is therefore used to relieve pain and inflammation. All the medicines in this group (NSAIDs) reduce inflammation caused by the body's own immune system, and are effective pain killers. Ibuprofen can be used to relieve pain such as muscular aches and pains, period pains, headache, backache, rheumatic
Side Effects/ Adverse Reactions CNS
Headache, dizziness, nervousness, aseptic meningitis.
Nursing Considerations
-Tell patient to take with meals or milk to reduce adverse GI reactions. -Note: Drug is available at OTC. Instruct patient not to exceed 1.2 g daily, not to give to chidren younger than age 12, and not to take for extended periods ( longer than 3 days for fever or longer than 10 days for pain) without consulting presciber. -Tell patient that full therapeutic effect for arthritis may be delayed for 2 to 4 weeks. Although pain relief occurs at low dosage levels, inflammation doesnt improve at dosages less than 400 mg q.i.d. -Teach patient to watch for and report to prescriber immediately signs and symptoms of GI bleeding, including blood in vomit, urine, or stool or coffee ground vomit, and black, tarry stool. -Warn patient to avoid
CV
Peripheral edema, fluid retention, edema.
EENT GI
Tinnitus Epigastric distress, nausea, occult blood loss, peptic ulceration, diarrhea, constipation, abdominal pain, bloating, GI fullness, dyspepsia, flatulence, heartburn, decreased appetite.
GU
Acute renal failure, azotemia, cystitis, hematuria.
HEMATOLOGIC
Plonged bleeding time, anemia, neutropenia, pancytopenia, thrombocytopenia, aplastic anemia, leucopenia, agranulocystocis.
METABOLIC
12
Case Study: Septic Knee, Ankle, 1st MT Right Foot
pain, dental pain and neuralgia. It can also reduce feverishness and the symptoms of colds and flu.
Hypoglycemia, hyperkalemia.
RESPIRATORY
Bronchospasm
SKIN
Isoniazid
Niazid
-yellow skin or eyes; -dark urine; -numbness or tingling in your hands or feet; -seizures; -blurred vision; or -confusion behavior. or abnormal
13
Case Study: Septic Knee, Ankle, 1st MT Right Foot
The mechanism of action of INH is not known, but it is thought to work through its effects on lipids (fats) and DNA within the tuberculosis bacterium. It is very selective for the tuberculosis bacteria, that is, it has few if any effects on other bacteria.
INH is used to prevent active tuberculosis in persons who have an abnormal skin test for tuberculosis or in combination with other drugs for the treatment of active tuberculosis. Prophylaxis in specific patients who are tuberculin reactors (positive Mantoux test)) or who are considered to be high risk for TB.
Pruritus, rash, urticaria, stevens Johnson syndrome. -allergic reaction (difficulty breathing; closing of the throat; swelling of the lips, tongue, or face; or hives); -unusual fatigue; weakness or
-nausea, vomiting, or loss of appetite; -abdominal pain;
hazardous activities that require mental alertness until effects on CNS are known. -Advise patient to wear sunscreen to avoid hypersensitivity to sunlight. Health teachings: -Take this drug in single daily dose. -Take drug on an empty stomach, 1 hour before or 2 hours after meals. If GI distress occurs, may be taken with food. -Take this drug regularly, avoid missing doses, do not discontinue without first consulting your health care provider. -Do not drink alcohol or drink as little as possible. There is an inc. risk of heap if these two drugs are combined. -Avoid foods containing tyramine, consult a dietitian to obtain a list of foods containing tyramine or histamine. -Have periodic medical check-ups, including an eye examination and blood test, to evaluate the drug
effects. -Report for weakness, fatigue, loss of appetite, n/v, yellowing of skin or eyes, darkening of the urine, numbness or tingling in hands or feet,
14
Case Study: Septic Knee, Ankle, 1st MT Right Foot
Rifampin
Rifadin
Inhibits DNAdependent RNA polymerase activity in susceptible bacterial cells.
15
Case Study: Septic Knee, Ankle, 1st MT Right Foot
Treatment of Pulmonary TB in conjunction with at least one other effective antituberculotic. Neisseria meningitidis carriers, for asymptomatic carriers to eliminate meningococci from nasopharynx; not for treatment of meningitis. Unlabeled uses: Infections caused by Staphylococcus aureus and Staphylococcus epidermis, usually in combination therapy; gramnegative bacteremia in infancy; Legionella pneumophilia, not responsive to erythromycin; leprosy (in combination with dapsone); prophylaxis of meningitis caused by Haemophilis influenzae.
CNS: headache, drowsiness, fatigue, dizziness, inability to concentrate, mental confusion, generalized numbness, muscle weakness, visual disturbances. Dermatologic: Rash, pruritus, urticaria, flushing, reddish discoloration of body fluidstears, saliva, urine, sweat, sputum. GI: heartburn, distress, anorexia, vomiting gas, cramps, diaarhea, hepatitis, pancreatitis. GU: hemoglobinuria, hematuria, renal insufficiency, acute renal failure, menstrual disturbances. Hematologic: eosinophilia, thrombocytopenia, transient leucopenia, hemolytic anemia, decreased Hgb, hemolysis. Other: pain in extremities, osteomalacia, myopathy, fever, flulike symptoms.
-Teach client to take drug in a single daily dose. Take on an empty stomach, 1 hr before or 2 hrs after meals. -Inform client to take this drug regularly; avoid missing any doses; do not discontinue this drug without consulting the health care provider. -Tell client to have periodic medical checkups, including eye examinations and blood test, to evaluate the drug effects. -Inform client that he may experience the drugs side effects (especially the red colored secretion) -Instruct client to see his physician if he experience fever, chills, muscle and bone pain, excessive tiredness or weakness, loss of appetite, N/V, yellowing of eyes/skin, unusual bleeding or bruising, skin rash or itching. -Instruct client to remove contact lenses as they may discolor
Other: Mild arthralgia and myalgia have been reported frequently. Hypersensitivity reactions including rashes, urticaria, and pruritis have been reported. Fever, acne, photosensitivity, porphyria, dysuria and interstitial nephritis have been reported rarely.
16
Case Study: Septic Knee, Ankle, 1st MT Right Foot
Pyrazinamide Pyrazinamide Pyrazinamide may be bacteriostatic or bactericidal against Mycobacterium tuberculosis depending on the concentration of the drug attained at the site of infection. The mechanism of action is unknown. In vitro and in vivo the drug is active only at a slightly acidic pH.
Pyrazinamide is indicated for the initial treatment of active tubercuIosis in adults and children when combined with other antituberculous agents. (The current recommendation of the CDC for drugsusceptible disease is to use a six-month regimen for initial treatment of active tuberculosis, consisting of isoniazid, rifampin and pyrazinamide given for 2 months, followed by isoniazid and rifampin for 4 months.*4) (Patients with drug-resistant disease should be treated with regimens individualized to their situation. Pyrazinamide frequently will be an important component of such therapy.) (In patients with concomitant HIV infection, the physician should be aware of current recommendation of CDC. It is possible these patients may require a longer course of treatment.)
General: Fever, porphyria and dysuria have rarely been reported. Gastrointestinal: The principal adverse effect is a hepatic reaction (see WARNINGS). Hepatotoxicity appears to be dose related, and may appear at any time during therapy. Gl disturbances including nausea, vomiting and anorexia have also been reported. Hematologic and Lymphatic: Thrombocytopenia and sideroblastic anemia with erythroid hyperplasia, vacuolation of erythrocytes and increased serum iron concentration have occurred rarely with this drug. Adverse effects on blood clotting mechanisms have also been rarely reported.
-Take this drug in single daily dose. -Take drug on an empty stomach, 1 hour before or 2 hours after meals. If GI distress occurs, may be taken with food. -Take this drug regularly, avoid missing doses, do not discontinue without first consulting your health care provider. -Do not drink alcohol or drink as little as possible. There is an inc. risk of heap if these two drugs are combined.
Vitamin B complex
Surbex, Vicon-C, ZBec
A coenzyme that stimulate metabolic function and is needed for cell replication, hematopoiesis, and nucleoprotein and myelin synthesis
This product is a combination of B vitamins used to treat or prevent vitamin deficiency due to poor diet, certain illnesses, alcoholism, or during pregnancy. Vitamins are important building blocks of the body and help keep you in good health. B vitamins include thiamine, riboflavin, niacin/niacinamide, vitamin B6, vitamin B12, folic acid, and pantothenic acid
17
Case Study: Septic Knee, Ankle, 1st MT Right Foot
CV: Peripheral vascular thrombosis, heart failure. GI: transient diarrhea. Respi: pulmonary edema. Skin: it ching, transitory exanthema, urticaria. Other: anaphylaxis, anaphylactoid reactions with parenteral administration , pain or burning at injection site
BEFORE: ~ Determine reticulocyte count, hct, Vit.B12, iron, folate levels before beginning therapy. ~ Obtain a sensitivity test history before administration ~ Avoid I.V. administration bec. faster systemic elimination will reduce effectiveness of vitamin. DURING: ~ Dont give large doses of vitaminB12 routinely; drug is lost through excretion. ~ Dont mix parenteral preparation in same syringe with other drugs. AFTER: ~ Protect Vit.B12 from light. Dont refrigerate or freeze. ~ Monitor patient for hypokalemia for first 48 hours, as anemia correct itself. Give potassium supplements, as needed
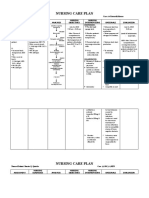
XI. NURSING CARE PLAN Assessment Subjective: Kaya ko po umupo pero di ko po kayang tumayo at lumakad Objective: Limited range of motion Limited ability to perform gross or fine motor skills Postural instability Diagnosis Impaired physical mobility related to decreased muscle strength or control as manifested by limited range of motion; limited ability to perform fine motor skills and postural instability. Planning Short term: After 4 hours of rendering nursing intervention the patient will be able to; Improve limited range of motion. Improve postural instability. Intervention Establish rapport to the patient. Assess patients condition. Determine diagnosis that contributes to immobility Assist patient to perform range of motion exercises Use assistive devices ( crutches, walkers, overhead trapeze) Provide patient with ample time to perform mobility-related tasks. Encourage the support of significant others. Rationale To gain trust and active participatio n. To be aware of the patients condition and feeling. To obtain baseline data. To prevent muscle contracture . To promote independen t movement and support. Evaluation After 4 hours of rendering nursing intervention the patient will now be able to improved range of motion and postural instability.
The patient will be able to; Maintain maximum physical mobility. Perform physical activity independently or with assisted devices.
Vital signs taken as follows: Temp: 36.9C PR: 78 BPM RR: 21 BPM Apical: 70 BPM
18
Case Study: Septic Knee, Ankle, 1st MT Right Foot
Long term:
To promote optimum level of functioning
Allow them to assist with range of motion exercises and positioning if desired. Evaluation Short term: Patient gained weight of 1 kilogram from 20.4kg to 21.4 kg. Long term: Clients condition of electrolytes and blood counts are within normal and demonstrate a Case Study: Septic Knee, Ankle, 1st MT Right Foot
Assessment Subjective: Puro cup noodles lang ang kinakain niya. As verbalized by the patients relative. Objective:
Diagnosis Risk for Imbalance Nutrition Less than body Requirements related to decrease absorption of nutrients as evidenced by poor skin turgor and weight loss.
Planning Short term: Patient will gain weight at least 1 kilogram for the next 2 weeks. Long term: Client will exhibit no signs or symptoms of malnutrition by
Intervention Establish rapport to the patient. Assess the patients weight. Determine the patients nutritional history. Determine the
Rationale To gain trust and active participation. To obtain baseline data. To assess the usual food that he eats even before he became ill. Psychological
19
Poor skin turgor Age: 8 y/o Height: 33inches Weight: 20.4 kg
time of discharge from treatment.
patients attitude towards eating. Encourage to eat nutritious foods( High protein, high calorie & high calcium diet). Ensure that client receives small, frequent feedings. Maintain adequate hydration, increase fluid intake. Administer vitamin and mineral supplements, as ordered by physician.
factor towards eating may affect appetite and to know his eating habits. To achieve normal body weight and calcification of bone. Large amount of foods may be intolerable, to the client. To prevent dehydration & maintain hydration status. This will help as an additional to the nutritional status of the client.
steady weight gain.
Collaborative: Consult dietitian for further
Dietitians have a greater understanding of the nutritional
20
Case Study: Septic Knee, Ankle, 1st MT Right Foot
assessment and recommendati ons regarding food preferences and nutritional support
value of foods and may be helpful in assessing specific ethnic or cultural foods.
21
Case Study: Septic Knee, Ankle, 1st MT Right Foot
You might also like
- FUNDAMENTALS 1-3 Comprehensive ExamDocument14 pagesFUNDAMENTALS 1-3 Comprehensive ExamJon Adam Bermudez SamatraNo ratings yet
- Introduction To Nursing PharmacologyDocument5 pagesIntroduction To Nursing PharmacologyJon Adam Bermudez SamatraNo ratings yet
- EthicsDocument7 pagesEthicsJon Adam Bermudez SamatraNo ratings yet
- Shuttlecockwas Played in China, Japan, India and Greece. This Is ADocument1 pageShuttlecockwas Played in China, Japan, India and Greece. This Is AKath CampomanesNo ratings yet
- Akapulko or Acapulco in English Is A Shrub Found Throughout The PhilippinesDocument6 pagesAkapulko or Acapulco in English Is A Shrub Found Throughout The PhilippinesJon Adam Bermudez SamatraNo ratings yet
- Raynauds DiseaseDocument20 pagesRaynauds DiseaseJon Adam Bermudez SamatraNo ratings yet
- Pharma ReportDocument1 pagePharma ReportJon Adam Bermudez SamatraNo ratings yet
- PreventionDocument1 pagePreventionJon Adam Bermudez SamatraNo ratings yet
- Profession Adjustment PhilnursingstudentDocument13 pagesProfession Adjustment PhilnursingstudentJon Adam Bermudez SamatraNo ratings yet
- Profession Adjustment PhilnursingstudentDocument13 pagesProfession Adjustment PhilnursingstudentJon Adam Bermudez SamatraNo ratings yet
- Common Medical TermsDocument10 pagesCommon Medical TermsJon Adam Bermudez SamatraNo ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Intervention Rationale EvaluationDocument1 pageAssessment Nursing Diagnosis Scientific Explanation Planning Intervention Rationale EvaluationJon Adam Bermudez SamatraNo ratings yet
- Cinderella story set in palaceDocument1 pageCinderella story set in palaceRio Juliver SipahutarNo ratings yet
- Babasahin (Pedia)Document44 pagesBabasahin (Pedia)Jon Adam Bermudez SamatraNo ratings yet
- NCP - Disturbed Sleeping PatternDocument2 pagesNCP - Disturbed Sleeping Patternjsthr89% (27)
- A CaseStudy of CesareanDeliveryDocument4 pagesA CaseStudy of CesareanDeliveryJon Adam Bermudez SamatraNo ratings yet
- CNS: GI: Assessment & Drug Effects: Generic Name Brand Name Indications Action Side Effects Nursing ResponsibilitiesDocument4 pagesCNS: GI: Assessment & Drug Effects: Generic Name Brand Name Indications Action Side Effects Nursing ResponsibilitiesJon Adam Bermudez SamatraNo ratings yet
- NCPDocument2 pagesNCPJon Adam Bermudez SamatraNo ratings yet
- NuDocument8 pagesNuJon Adam Bermudez SamatraNo ratings yet
- Assessment Procedure Methods Actual Findings Normal Status Interpretati On SkinDocument8 pagesAssessment Procedure Methods Actual Findings Normal Status Interpretati On SkinJon Adam Bermudez SamatraNo ratings yet
- A CaseStudy of CesareanDeliveryDocument4 pagesA CaseStudy of CesareanDeliveryJon Adam Bermudez SamatraNo ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Intervention Rationale EvaluationDocument1 pageAssessment Nursing Diagnosis Scientific Explanation Planning Intervention Rationale EvaluationJon Adam Bermudez SamatraNo ratings yet
- Drug Guide: Generic, Class, Action, Uses, Risks & Nursing CareDocument2 pagesDrug Guide: Generic, Class, Action, Uses, Risks & Nursing CareJon Adam Bermudez SamatraNo ratings yet
- Nursing InformaticsDocument11 pagesNursing InformaticsJon Adam Bermudez SamatraNo ratings yet
- HemodialysisDocument4 pagesHemodialysisJon Adam Bermudez SamatraNo ratings yet
- Generic Name Brand Name Indications Action Side Effects Nursing ResponsibilitiesDocument1 pageGeneric Name Brand Name Indications Action Side Effects Nursing ResponsibilitiesJon Adam Bermudez SamatraNo ratings yet
- Chapter III RizalDocument12 pagesChapter III RizalJon Adam Bermudez SamatraNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- PMLS MidtermsDocument3 pagesPMLS MidtermslhalaineiluisNo ratings yet
- Tuberculosis: krisbantas/EPM/s1 1Document33 pagesTuberculosis: krisbantas/EPM/s1 1Yoerdy Agusmal SaputraNo ratings yet
- Revised Guidelines For HIV Counseling, Testing, ReferralDocument110 pagesRevised Guidelines For HIV Counseling, Testing, ReferralDarrel Allan MandiasNo ratings yet
- PMLS 2 LaboratoryDocument11 pagesPMLS 2 LaboratoryJanna EchavezNo ratings yet
- JUNE, 2017: Instructions To CandidateDocument11 pagesJUNE, 2017: Instructions To Candidatekalasa roydNo ratings yet
- CRAFT Symposium Program - SMDocument65 pagesCRAFT Symposium Program - SMU of T MedicineNo ratings yet
- NSTP ReviewerDocument18 pagesNSTP ReviewerKrystel TullaoNo ratings yet
- Puerperial PyrexiaDocument4 pagesPuerperial Pyrexiakutra3000No ratings yet
- Schistosoma Japonicum: Schistosoma Japonicum or The Oriental Blood Fluke Causes Schistosomiasis Japonica. It IsDocument7 pagesSchistosoma Japonicum: Schistosoma Japonicum or The Oriental Blood Fluke Causes Schistosomiasis Japonica. It IsPau SorianoNo ratings yet
- T - 1437039951caipang 9Document15 pagesT - 1437039951caipang 9Doge WoweNo ratings yet
- Covid19 Preventive Measures in The WorkplaceDocument8 pagesCovid19 Preventive Measures in The WorkplaceAnthony Sanglay, Jr.No ratings yet
- Occupational Hazards Part 1Document94 pagesOccupational Hazards Part 1Eshan VermaNo ratings yet
- 08 January Dawn Editorials+opinions With Urdu TranslationDocument21 pages08 January Dawn Editorials+opinions With Urdu TranslationAgha Khan DurraniNo ratings yet
- Allergic Rhinitis and Its Impact On AsthmaDocument188 pagesAllergic Rhinitis and Its Impact On AsthmaSergioNo ratings yet
- Tugas Critical Appraisal - DR - AfifurrahmanDocument5 pagesTugas Critical Appraisal - DR - AfifurrahmanAfifurrahman RizalNo ratings yet
- Microbiology and Parasitology (Finals) : Khrizlynne Soberano BSN 1-Stem BDocument3 pagesMicrobiology and Parasitology (Finals) : Khrizlynne Soberano BSN 1-Stem BNicoleVillamorNo ratings yet
- 18 Amazing Health Benefits of Honey and CinnamonDocument6 pages18 Amazing Health Benefits of Honey and CinnamonHabib MohammedNo ratings yet
- Second Thoughts About Viruses Vaccines and The HIV Part 2 Robert.O.YoungDocument5 pagesSecond Thoughts About Viruses Vaccines and The HIV Part 2 Robert.O.YoungDavidNo ratings yet
- Mekanisme Penyakit InfeksiDocument35 pagesMekanisme Penyakit InfeksiNur FaidahNo ratings yet
- Global Health InitiativesDocument31 pagesGlobal Health InitiativesDaisy Joy SalanNo ratings yet
- Awareness of Carabao Raisers On The Incidence of Parasitic Liver FlukeDocument29 pagesAwareness of Carabao Raisers On The Incidence of Parasitic Liver FlukeArvin Manalo100% (1)
- ACC166 Slides 3Document4 pagesACC166 Slides 3URANG CHITONo ratings yet
- Nursing Care Plan-Mam LazoDocument7 pagesNursing Care Plan-Mam LazoGayLah MomblancoNo ratings yet
- Adaptive Architecture and The Prevention of InfectDocument8 pagesAdaptive Architecture and The Prevention of InfectsummiNo ratings yet
- Infection Control in Burns PatietnsDocument41 pagesInfection Control in Burns Patietnstummalapalli venkateswara raoNo ratings yet
- MSF Field Research Causes of false positive HIV rapid diagnostic test resultsDocument35 pagesMSF Field Research Causes of false positive HIV rapid diagnostic test resultsSavioPereira1234No ratings yet
- Ramaphosa Speech - Coronavirus LockdownDocument13 pagesRamaphosa Speech - Coronavirus LockdownBusinessTech100% (2)
- Eponyms SyndromesDocument23 pagesEponyms Syndromestekennn021No ratings yet
- Cancer Pain ManagementDocument8 pagesCancer Pain ManagementMaryjoy Gabriellee De La Cruz100% (1)
- Source of Infections 1. Endogenous SourceDocument6 pagesSource of Infections 1. Endogenous SourceDeepu VijayaBhanuNo ratings yet