Professional Documents
Culture Documents
Case Report Skichooo
Uploaded by
Dana Fajardo RezanoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Report Skichooo
Uploaded by
Dana Fajardo RezanoCopyright:
Available Formats
I.
Introduction
This Case Report is about Patient Tony admitted at Mariveles Mental Hospital diagnosed of Paranoid Schizophrenia for 6 years. He is already 53 years old, born on September 20, 1960 at Pozorubio, Pangasinan. Paranoid schizophrenia is the most common type of schizophrenia in most parts of the world. The clinical picture is dominated by relatively stable, often paranoid, delusions, usually accompanied by hallucinations, particularly of the auditory variety, and perceptual disturbances. Disturbances of affect, volition, and speech, and catatonic symptoms, are not prominent.
Examples of the most common paranoid symptoms are: delusions of persecution, reference, exalted birth, special mission, bodily change, or jealousy; hallucinatory voices that threaten the patient or give commands, or auditory hallucinations without verbal form, such as whistling, humming, or laughing; hallucinations of smell or taste, or of sexual or other bodily sensations; visual hallucinations may occur but are rarely predominant. Thought disorder may be obvious in acute states, but if so it does not prevent the typical delusions or hallucinations from being described clearly. Affect is usually less blunted than in other varieties of schizophrenia, but a minor degree of incongruity is common, as are mood disturbances such as irritability, sudden anger, fearfulness, and suspicion. "Negative" symptoms such as blunting of affect and impaired volition are often present but do not dominate the clinical picture. The course of paranoid schizophrenia may be episodic, with partial or complete remissions, or chronic. In chronic cases, the florid symptoms persist over years and it is difficult to distinguish discrete episodes. The onset tends to be later than in the hebephrenic and catatonic forms. Schizophrenia affects about 24 million people worldwide. Schizophrenia is a treatable disorder, treatment being more effective in its initial stages. More than 50% of persons with schizophrenia are not receiving appropriate care. 90% of people with untreated schizophrenia are in developing countries. Care of persons with schizophrenia can be provided at community level, with active family and community involvement. (www.who.int)
II.
Nursing Assessment
Past Health History
Patient Tonys past illnesses includes only simple cases like Tonsilitis, colds, and cough. He does not have any history of Hypertension or Diabetes Mellitus. Whenever he has fever, he will take Paracetamol, and cough syrup for cough.
Present Health History
Patient Tonys first admission was on April 21, 2006 . His mental illness started when he had a fight with his co-worker in a mining company. He resigned from the company after 20 years of service, and his benefits are all gone to waste. He got himself engaged to Alcohol drinking. He was always seen talking to self, had impaired sleep, and also suspicious. He claimed that he and his family will be eaten by someone Kakainin nila ang mga anak ko. Thats the reason why he was admit ted at the Mariveles Mental Hospital. After 1 year and 4 months of confinement, he was already able to go home. But at home, he did not take his medicines telling his wife that they are fake. He drank alcohol against advice. He even suspects that his wife is not his real wife. At November 9, 2007 he was again brought to Mariveles Mental Hospital. He was again able to go home but at May 17, 2012, he was again admitted because he was triggered by the new Philippine Peso Bills being given to him as payment at their store claiming that they are fake. He kept all the new bills inside their clothes. He commanded his wife to bring out all the new Philippine Peso Bills and burn them. He told his wife that if she will not do it, he will cut her into pieces, Susunugi n mo mga yan o tatadtarin kita. Patient Tony is still at Mariveles mental Hospital, however, he is now manageable and will be home conducted after 3 months of zero visitation of his family.
III.
The patient and his illness
Synthesis of the Disease Definition of the Disease
Paranoid schizophrenia is a subtype of schizophrenia in which the patient has delusions (false beliefs) that a person or some individuals are plotting against them or members of their family. The majority of people with paranoid schizophrenia, as with most schizophrenia subtypes may also have auditory hallucinations - they hear things that are not real. They may also have delusions of personal grandeur - a false belief that they are much greater and more powerful and influential than they really are. An individual with paranoid schizophrenia may spend a disproportionate amount of time thinking up ways of protecting themselves from their persecutors. Typically, a person with paranoid schizophrenia has fewer problems with memory, dulled emotions and concentration compared to those with other subtypes; which allows them to think and function more successfully. Even so, paranoid schizophrenia is a chronic (long-term, lifelong) condition which may eventually lead to complications, including suicidal thoughts and behavior
Signs and Symptoms
The patient will have relatively stable, frequently paranoid delusions, which are usually accompanied by auditory hallucinations (hearing things that are not there) and perceptual disturbances. Some schizophrenia symptoms are not prominent, such as disturbances of volition, affect, speech and catatonia.
Auditory hallucinations - hearing voices that are not there (they don't exist). Visual hallucinations are possible, but rare. Delusions - beliefs that are not real; false personal beliefs that are not subject to reason or contradictory evidence. The patient may firmly believe something, even though there is incontrovertible evidence that it is false. An example may be a belief that a neighbor is plotting to kill or poison the patient. Anxiety - a patient with paranoid schizophrenia will usually suffer from periods of high anxiety. Anger - this emotional state may range from mild irritation, which most healthy individuals sometimes have, to fury and rage. Anger may raise heart rate, blood pressure and levels of adrenaline and noradrenaline.
Detachment - the patient may sometimes be physically or emotionally; reserved and remote (aloofness) Aggression and violence - aggression may reach levels in which violent outbursts occur. Quarrels Condescension - sometimes the patient may seem patronizing; perhaps they may feel they know stuff other people don't and subsequently assume such a manner. Suicidal thoughts and behavior - these may be noticeable by people around the individual, with statements such as "I wish I were dead", I am going to kill myself", or "I wish I had never been born". The patient may go further and obtain the means to kill himself/herself, such as getting a weapon or accumulating pills.
Other warning signs may be:
o o o o o o o o
Becoming socially withdrawn Mood swings - however, mood disorders and problems with thinking are less common in this type of schizophrenia Being obsessed with death, dying or violence Feeling trapped or desperate Increased consumption of drugs (including illegal ones) and alcohol Changing eating or sleeping patterns Starting to get their affairs in order and giving away belongings Saying goodbye to people in a specific way (as if they are never going to see them again) While some patients may have clear suicidal behaviors and thoughts (obvious to others), others may be more secretive. The warning signs might be subtle, and sometimes not noticeable at all.
Patients with paranoid schizophrenia are more likely to be affected by positive symptoms, such as delusions and auditory hallucinations, and less by problems with mood, cognition (thinking, concentration, attention), compared to other types of schizophrenia.
Health promotion and preventive aspects
Paranoid schizophrenia is an illness that lasts all the way through the individual's life it is a chronic condition. Patients with paranoid schizophrenia require treatment on a permanent basis; even when symptoms seem to have receded - a tempting time for schizophrenia patients to say they are fine and need no more help. Treatment is basically the same for all forms of schizophrenia; there are variations depending on the severity and types of symptoms, the health of the patient, his/her age, as well as some other factors. Treatment options include drugs (medications), psychotherapy, hospitalization (or partial hospitalization), ECT (electroconvulsive therapy), and vocational skills training.
Medications: Atypical antipsychotics (2nd generation antipsychotics) - a group of antipsychotic drugs used for the treatment of psychiatric conditions. Atypicals differ from typical antipsychotics in that they do not tend to cause extrapyramidal symptoms (EPS). EPS include parkinsoniantype movements, rigidity and tremor. Side effects may include:
Weight gain Diabetes Elevated blood cholesterol levels Typical antipsychotics (1st generation antipsychotics) - even though they are as effective in treating the same symptoms as atypical antipsychotics are, patients have a much higher risk of experiencing extrapyramidal symptoms (EPS), including involuntary movements of the face, tremor and parkinsonian-type movements. The generic versions of these drugs are much cheaper than atypical antipsychotics. Other drugs (medications) - individuals with schizophrenia are susceptible other mental health problems, such as depression. The doctor may prescribe an antidepressant, an anti-anxiety drug, or a mood-stabilizing medication. Hospitalization - when symptoms are severe the patient may need to be hospitalized. A hospital setting may be safer, where proper nutrition may be provided, and the patient may get better sleep and receive help with hygiene. Sometimes partial hospitalization is also possible. Psychotherapy - for patients with paranoid schizophrenia, medications are the key part of treatment; however, psychotherapy is also important.
Social and vocational skills training - this may help the patient live independently; a vital part of recovery for the patient. The therapist can help the patient learn good hygiene, prepare nutritional meals, and have better communication. There may be help in finding work, housing and joining self-help groups. Compliance (adherence) - compliance or adherence in medicine means following the therapy regime (the treatment plan). Unfortunately, lack of compliance is a major problem for patients with schizophrenia. Patients can go off their medication for long periods during their lives, at enormous personal costs to themselves and often to those around them as well. As a significant percentage of individuals go off their medication within the first 12 months of treatment, a life-long regimen of both drug and psychological/support therapies are important for treatment to be effective and long-lasting. ECT (electroconvulsive therapy) - in this procedure an electric current is sent through the brain to produce controlled seizures (convulsion). It may be used on patients with severe symptoms or depression who either have not responded to other treatments or cannot take antidepressants. It is also sometimes used for patients at high risk of suicide. Experts believe that ECT triggers a massive neurochemical release in the brain, caused by the controlled seizure. Side effects may include short-term memory loss (usually resolves rapidly). It is important that the doctor explain clearly the pros and cons of ECT to the patient and/or guardian or family member.
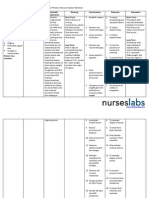
Cues S> O> impaired Judgement
Nursing Diagnosis Disturbed Thought Processes related to Inability to trust as evidenced by suspiciousness
Scientific explanation
Goal/Planning After proper Nurse-patient interaction, the patient will demonstrate decreased anxiety level.
Intervention Greet the client and introduce self. Be sincere and honest when communicating with the client. Avoid vague or evasive remarks
Rationale To develop trust
Evaluation After proper Nurse-patient interaction, the patient demonstrated decreased anxiety level.
Distractibility
Hypervigilance
Delusional clients are extremely sensitive about others andcan recognize insincerity. Evasive comments or hesitationreinforces mistrust or delusions.
Be consistent in setting expectations, enforcing rules,and so forth.
Clear, consistent limits provide a secure structure for the client.
Do not make promises that cannot be kept.
Broken promises reinforce the clients mistrust of others.
Interact with the client on the basis of real things; do notdwell on the delusional material
Interacting about reality is healthy for the client
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Melvin D. Fabra: Objective - Aspiring To Obtain A Position As A Call Center Representative in A DynamicDocument2 pagesMelvin D. Fabra: Objective - Aspiring To Obtain A Position As A Call Center Representative in A DynamicDana Fajardo RezanoNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- CA 2 Nres Exam & Answers 2014Document5 pagesCA 2 Nres Exam & Answers 2014Dana Fajardo RezanoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Diagnostic and Laboratory ProcedureDocument4 pagesDiagnostic and Laboratory ProcedureDana Fajardo RezanoNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Fluid Volume Excess CRFDocument3 pagesFluid Volume Excess CRFDana Fajardo RezanoNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- General Physical AssessmentDocument2 pagesGeneral Physical AssessmentDana Fajardo RezanoNo ratings yet
- Benign Prostatic HyperplasiaDocument18 pagesBenign Prostatic HyperplasiaDana Fajardo Rezano0% (1)
- JMDocument45 pagesJMDana Fajardo RezanoNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Does Moore Succeed in Refuting IdealismDocument5 pagesDoes Moore Succeed in Refuting IdealismharryNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Criteria 5 Points 4 Points 3 Points 2 Points 1 Point Total PointsDocument2 pagesCriteria 5 Points 4 Points 3 Points 2 Points 1 Point Total PointsReyno D. Paca-anasNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Counter-Example NLPDocument8 pagesCounter-Example NLPRafaelBluskyNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- BD9897FS Ic DetailsDocument5 pagesBD9897FS Ic DetailsSundaram LakshmananNo ratings yet
- Contoh Pidato Bahasa Inggris Dan Terjemahannya Untuk SMPDocument15 pagesContoh Pidato Bahasa Inggris Dan Terjemahannya Untuk SMPAli Husein SiregarNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Iyengar S., Leuschke G.J., Leykin A. - Twenty-Four Hours of Local Cohomology (2007)Document298 pagesIyengar S., Leuschke G.J., Leykin A. - Twenty-Four Hours of Local Cohomology (2007)wojtekch100% (1)
- An Improved Version of The Skin Chapter of Kent RepertoryDocument6 pagesAn Improved Version of The Skin Chapter of Kent RepertoryHomoeopathic PulseNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- ESC Cardiomyopathy ClassificationDocument7 pagesESC Cardiomyopathy Classificationvalerius83No ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Rainfall Runoff ModellingDocument23 pagesRainfall Runoff ModellingmansikakaniNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Functions of Ecgc and Exim BankDocument12 pagesFunctions of Ecgc and Exim BankbhumishahNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Mis 2023Document62 pagesMis 2023Ana Mae MunsayacNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Sample File: A of TheDocument6 pagesSample File: A of TheMegan KennedyNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 211 N. Bacalso Avenue, Cebu City: Competencies in Elderly CareDocument2 pages211 N. Bacalso Avenue, Cebu City: Competencies in Elderly CareScsit College of NursingNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Impact of Video Gaming To The Academic Performance of The Psychology Students in San Beda UniversityDocument5 pagesThe Impact of Video Gaming To The Academic Performance of The Psychology Students in San Beda UniversityMarky Laury GameplaysNo ratings yet
- Thailand Day 2Document51 pagesThailand Day 2Edsel BuletinNo ratings yet
- SWOT ANALYSIS - TitleDocument9 pagesSWOT ANALYSIS - TitleAlexis John Altona BetitaNo ratings yet
- ArticlesOfConfederation Constitution 3.0Document6 pagesArticlesOfConfederation Constitution 3.0ChristinaNo ratings yet
- Histology Solution AvnDocument11 pagesHistology Solution AvnDrdo rawNo ratings yet
- Eapp Module 1Document6 pagesEapp Module 1Benson CornejaNo ratings yet
- Endogenic Processes (Erosion and Deposition) : Group 3Document12 pagesEndogenic Processes (Erosion and Deposition) : Group 3Ralph Lawrence C. PagaranNo ratings yet
- Modbus Manual TD80 PDFDocument34 pagesModbus Manual TD80 PDFAmar ChavanNo ratings yet
- MATH 7S eIIaDocument8 pagesMATH 7S eIIaELLA MAE DUBLASNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Bad SenarioDocument19 pagesBad SenarioHussain ElboshyNo ratings yet
- A Portrayal of Gender and A Description of Gender Roles in SelectDocument429 pagesA Portrayal of Gender and A Description of Gender Roles in SelectPtah El100% (1)
- Network Scanning TechniquesDocument17 pagesNetwork Scanning TechniquesjangdiniNo ratings yet
- 10 Chapter 3Document29 pages10 Chapter 3felefel100% (1)
- San Beda Alabang School of Law: Syllabus inDocument3 pagesSan Beda Alabang School of Law: Syllabus inLucia DielNo ratings yet
- Occ ST 1Document3 pagesOcc ST 1Rona Marie BulaongNo ratings yet
- Secant Method - Derivation: A. Bracketing MethodsDocument5 pagesSecant Method - Derivation: A. Bracketing MethodsStephen Dela CruzNo ratings yet
- PDF Certificacion 3dsmaxDocument2 pagesPDF Certificacion 3dsmaxAriel Carrasco AlmanzaNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)