Professional Documents
Culture Documents
Balance Deficits
Uploaded by
Maya VilCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Balance Deficits
Uploaded by
Maya VilCopyright:
Available Formats
Balance deficits One of the most common problems treated by physical therapists Are thought to be common after stroke,
e, and they have been implicated in the poor recovery of activities of daily living (ADL) and mobility and an increased risk of falls Balance - The ability to maintain the bodys center of gravity over its base of support with minimal sway or maximal steadiness - A complex process involving the reception and organization of sensory inputs and the planning and execution of movement to achieve a goal requiring upright posture - Is the set of functions which maintains mans upright during stance and locomotion by detecting and correcting displacement of the line of gravity beyond the BOS Postural control involves controlling he bodys position in space for the dual purposes of stability and orientation Postural orientation the control of relative positions of the body parts by skeletal muscles with respect to gravity and each other Postural stability the condition which all the forces acting on the body are balanced such that the center of mass (COM) is with in the stability limits or boundaries of BOS Normal anterior/posterior sway -12 degrees from most posterior-anterior position Lateral sway 16 degrees side to side Static balance BOS remains stationary and only the body center of mass (COM) moves. The balance task in this case is to maintain the COM within the BOS or the limit of stability (the maximal estimated sway angle of the COM)
Maintaining a stable antigravity position while at rest such as when standing and sitting
Automatic postural reactions maintaining balance in response to unexpected external perturbations, such as standing on a bus that suddenly accelerates forward. Dynamic balance maintaining balance when a person is moving from point A to point B, where both the BOS and COM are moving, and the COM is never kept within the BOS Is stabilizing the body when the support surface is moving or when the body is moving on a stable surface such as sit to stand transfers or walking Reactive control in response to external forces (perturbation) Proactive control in anticipation of internal forces imposed on the bodys own movements Systems model Balance controls is very complex and involves many different underlying systems Postural control results from a set of interacting systems
Musculoskeletal Joint ROM Spinal flexibility Muscle properties Biomechanical relationships among linked body segments Body schema Reactive mechanisms Anticipatory mechanisms (internal) Proactive mechanisms (external) Sensory systems Neuromuscular synergies
Neural components Motor processes (neuromuscular response synergies) Sensory processes (visual, vestibular, and somatosensory) Higher lvel integrative processes - Mapping sensation to action - Ensuring anticipatory and adaptive aspects of postural control Adaptive vs. Anticipatory Adaptive postural control - Involves modifying sensory and motor systems in response to changing task and environmental demands Anticipatory postural control - Involves preparing the sensory and motor systems for postural demands based on previous experience and learning Factors that contribute to stability Body alignment - Minimize the effect of gravitational forces, which tends to pull of Muscle tone Postural tone Standing alignment - Head balanced on level shoulders - Upper body erect, shoulders over hips - Hips in front of ankles - Feet few cm (10 cm) apart Sitting alignment - Head balanced on level shoulders - Upper body erect - Shoulders over hips - Feet and knees a few cm apart Muscle tone The force with which a muscle resists being lengthened Keeps the body from collapsing in response the pull of gravity
Postural tone Increased level of activity in antigravity muscles Activation of antigravity muscles during quiet stance Muscles that are tonically active during quiet stance: gastrocsoleus, tibialis anterior, gluteus medius, TFL, ilipsas, and erector spinae Ankle strategy Used when displacements are small Displaces COG by rotation about the ankle joint Posterior displacement of COG Anterior COG displacement Employed when ankle motion is limited, displacement is greater, when standing on unstable surface that disallows ankle strategy Preferred when perturbation is rapid and near limits of stability Post. Displacement COG backward sway, activation of paraspinals then hamstrings Ant displacement COG forward sway, activation of abdominal then quadriceps muscles Stepping strategy If displacement is large enough, a forward or backward step is used to regain postural control Sensory processes The maintenance of balance is based on an intrinsic cooperation between the Vestibular system Proprioceptive Vision - Postural control does not only depends on the integrity of the systems but also on the sensory integration with in the CNS, visual and spatial perception Visual inputs Provides information regarding:
The position of the head relative to the environment The orientation of the head to maintain level gaze The direction and speed of head movements because as your head moves, surrounding objects move in the opposite direction Provide a reference for vertically Visual stimuli can be used to improve a persons stability when proprioceptive or vestibular inputs are unreliable by fixating the gaze on an object
Sensitive to fast head movments (those that occur during gait or imbalance such as slips, trips, and stumbles)
Otolith organs Signal linear position and acceleration Source of information about head position with respect to gravity Respond to slow head movements (those that occur during postural sway) Sensory organization Vestibular, visual, and somatosensory inputs are normally combines seamlessly to produce our sense of orientation and movement Incoming sensory information is integrated and processed in the cerebellum, basal ganglia, and supplementary motor area Somatosensory information has the fastest processing time for rapid responses, followed by visual and vestibular inputs When sensory inputs from one system are inaccurate the CNS must suppress the inaccurate in put and slect and combine the appropriate sensory inputs from the other two systems Motor control model Individual, task, environment Causes of balance impairments Injury or diseases of the structures (e.g. eyes, inner ear, peripheral receptors, spinal cord, cerebellum, basal ganlia, cerebrum) Damage to proprioceptors Injury to or pathology of hip, knee, ankle, and back have been associated with increases postural sway and decreased balance Lesions produced by tumor, CVA, or other insults that often produced visual field losses
No Since most individuals can keep their balance when vision is occluded In addition, visual inputs are not always an accurate source of orientation information about self motion Visual system has difficulty distinguishing between object motion, referred to as exocentric motion, and self motion, referred to as egocentric motion
Somatosensory inputs... Provides the CNS with position and motion information about the body with reference to supporting surfaces Report information about the relationship of body segments to one another Receptors: muscle spindles, golgi tendon Vestibular inputs... A powerful source of information for postural control Provides the CNS with information about the position and movement of the head with respect to gravity and intertial forces Semicircular canal Sense angular acceleration of the head
Following a stroke Patients with muscle weakness and poor control lack effective anticipatory, onging, and reactive postural adjustments and therefore experience difficulty in: - Supporting the body mass over the paretic lower limb - Voluntarily moving the body mass from one lower limb to another - Responding rapidly to predicted and unpredicted threats to balance Spatiotemporal adaptations Changing the base of support Restricting movement of body mass Using hands for support Changing the base of support Wide BOS Shuffling feet with inappropriate stepping Shifting on the stronger leg Restricting movement of body mass Stiffening the body with altered segmental alignment Moving slowly Changing segmental alignment to avoid large shifts in COG - Standing reaching forward (flexing at ips instead of dorsiflexing ankles) - Standing reaching sideways (flexing trunk sidewas instead of moving body laterally at hips and feet) - Sitting reaching sideways (flexing forward instead of to the side) - In standing (not taking a step when necessary) Using the hands for support Holding on to support Grabbing Guidelines
Balance cannot be trained in isolation from the actions which must be relearned. In training walking, standing up and sitting down, reaching and manipulation... postural adjustments are also trained, since acquiring skill involves in large part the fine tuning of postural and balance control Postural adjustments are specific to each action and the conditions under which it occurs It cannot be assumed that practice of one action will transfer automatically into improved performance in another
Guidelines Progressive complexity is added by increasing the difficulty under which goals must be achieved, keeping in mind the various complex situations in which the patients will find themselves in the environment in which they live, both inside and outside their homes, and the precarious nature of balance As control over balance and confidence improves, tasks are introduced which require a stepping response, and responses to external constraints such as catching a thrown object and standing on a moving support surface Use a gait belt any time the patient practices exercises or activities that challenge or destabilize balance Stand slightly behind and to the side of the patient with one arm holding or near the gait belt and the other arm on or near the top of the shoulder (on the trunk, not the arm). Perform exercises near a railing or in parallel bars to allow patient to grab when necessary Do not perform exercises near sharp edges of equipment or objects Have on person in front and one behind when working with patients at high risk
of falling or during activities that pose a high risk of injury. Check equipment to ensure that it is operating correctly Guard patient when getting on and off equipment (such as treadmills and stationary bikes) Ensure that the floor is clean and free of debris
Trunk rotations and altered head positions alter vestibular input Stepping back/forward assists in restabilization exercises
Techniques to improve balance A variety of mode can be used to treat balance impairment Begin with weight shifts on a stable surface Gradually increase sway Increase surface challenges (mini tramp etc.) Rehabilitation balls, foam rollers, foam surfaces are often used to Provide uneven or unstable surface for exercise Sitting balance, trunk stability, and weight distribution can be trained on a chair, table, or therapeutic ball Pool is an ideal place for training balance Awareness of posture and the position of the body in space is fundamental to balance training Begin in supine or seated position Over sessions, use a variety of arm positions Unstable surfaces, single leg stances, etc Training both static posture and dynamic posture Mirrors can provide postural feedback visual feedback
Progression From simple to complex involves - BOS: advance from wide to narrow base - Posture: stable to unstable posture (sway) - Visual: closing of the eyes - COG: greater disruption to elicit hip or stepping strategy Progress to more dynamic activities, unstable surfaces, and complex movement patterns Frequency, intensity, and duration Specific techniques Bobath Normal postural activity forms necessary background for normal movement and for functional skills Flaccid stage balance exercises in sitting Stage of spasticity practice symmetrical weight bearing in standing, weight shifting, bending of knees and hips PNF techniques For stability Combination of isotonics Stabilizing reversals Rhythmic stabilization Motor relearning program Analysis of task - Individual - Task - Environment Practice of missing components - Strategy training - Impairment and strategy level Practice of whole task - Functional level
Movement - Adding movement patterns to acquired stable static postures increases balance challenge - Add ant./post. Sway to increase stability limits
Transference of learning
Static balance Vary postures Vary support surface Incorporate external loads Dynamic balance Moving support surfaces Move head, trunk, arms, legs Transitional and locomotor activities Anticipatory (feedforward) Reaching Catching Kicking Lifting Obstacle course Reactive (feedback) Standing sway Ankle strategy Hip strategy Stepping strategy Perturbations Sensory organization Reduce visual inputs Reduce somatosensory cues Sitting balance Acute stage post stroke Head and trunk movements Reaching actions To progress: Increasing distance to be reached Varying speed Reducing thigh support Increasing object weight and size to involve both upper limbs Adding an external timing constraint such as catching or bouncing a ball Standing balance Head and body movements
Reaching actions Single limb support Sideways walking Picking up objects
Paediatrics The following main aspects should be developed: Antigravity support or weight bearing on the feet Postural fixation of the head on the trunk and on the pelvis in the vertical Counterposing Control of anteroposterior weight shift of the childs COG Control of lateral sway from one foot to the other Tilt reactions in standing Saving from falling (strategies) Training should neck: Equal distribution of weight on each foot Correction of abnormal postures Building up of the childs stability by decreasing support Delay training in standing and walking if the child is not ready Weight shift leading to stepping Training lateral sway Training on different surfaces Define balance Assignment: Red kisners chapter 8: exercise for impaired balance, to enhance learning on this topic
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Guide To Physical Training ConsentDocument1 pageGuide To Physical Training ConsentMaya VilNo ratings yet
- What Is A ChristianDocument5 pagesWhat Is A ChristianMaya VilNo ratings yet
- CharacteristicsDocument1 pageCharacteristicsMaya VilNo ratings yet
- Review of Related LiteratureDocument6 pagesReview of Related LiteratureMaya Vil0% (1)
- Dear American Council of ExerciseDocument1 pageDear American Council of ExerciseMaya VilNo ratings yet
- Basic Concepts of Computer Networks and Communications: Presented By: Joss Kendrick LiquidoDocument21 pagesBasic Concepts of Computer Networks and Communications: Presented By: Joss Kendrick LiquidoMaya VilNo ratings yet
- Problem ListDocument2 pagesProblem ListMaya VilNo ratings yet
- Grading Sheet (Title Defense)Document1 pageGrading Sheet (Title Defense)Maya VilNo ratings yet
- Consent Letter Human KineticsDocument2 pagesConsent Letter Human KineticsMaya VilNo ratings yet
- Parents Consent LetterDocument1 pageParents Consent LetterMaya VilNo ratings yet
- The School of Allied Health Sciences ofDocument1 pageThe School of Allied Health Sciences ofMaya VilNo ratings yet
- Clinical Case Study GonadsDocument18 pagesClinical Case Study GonadsMaya VilNo ratings yet
- Guide To Physical Training ConsentDocument1 pageGuide To Physical Training ConsentMaya VilNo ratings yet
- Research Exercise Prescription and Youth Resistance GuidelinesDocument5 pagesResearch Exercise Prescription and Youth Resistance GuidelinesMaya VilNo ratings yet
- Sermon On The Ten Virgins - Parable of The Ten VirginsDocument4 pagesSermon On The Ten Virgins - Parable of The Ten VirginsMaya VilNo ratings yet
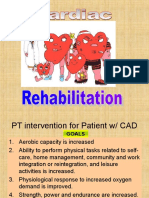
- Cardiac RehabilitationDocument87 pagesCardiac RehabilitationMaya Vil100% (2)
- Special Tests-ListDocument3 pagesSpecial Tests-ListMaya VilNo ratings yet
- Exercise in SMA - Methods 2014Document12 pagesExercise in SMA - Methods 2014Maya VilNo ratings yet
- The Physiology of Sports Injuries and Repair ProcessesDocument44 pagesThe Physiology of Sports Injuries and Repair ProcessesMaya VilNo ratings yet
- Principles and Techniques of Tendon RepairDocument5 pagesPrinciples and Techniques of Tendon RepairMaya VilNo ratings yet
- Presented By: Myra Leslie S. ViloriaDocument10 pagesPresented By: Myra Leslie S. ViloriaMaya VilNo ratings yet
- Berg Balance Scale: By: Myra Leslie S. ViloriaDocument5 pagesBerg Balance Scale: By: Myra Leslie S. ViloriaMaya VilNo ratings yet
- Below Knee Orthosis PrescriptionDocument18 pagesBelow Knee Orthosis PrescriptionMaya VilNo ratings yet
- Postpartum Physical TherapyDocument10 pagesPostpartum Physical TherapyMaya VilNo ratings yet
- Report in Law1Document18 pagesReport in Law1Maya VilNo ratings yet
- MyopathiesDocument127 pagesMyopathiesMaya VilNo ratings yet
- Bilateral OsteoarthritisDocument58 pagesBilateral OsteoarthritisMaya VilNo ratings yet
- Adrenal Cortex Case StudyDocument21 pagesAdrenal Cortex Case StudyMaya Vil0% (1)
- LMN NeuroDocument48 pagesLMN NeuroMaya VilNo ratings yet
- GeriatricDocument18 pagesGeriatricMaya VilNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Detrimental Effects of Orthodontic Treatment1Document12 pagesDetrimental Effects of Orthodontic Treatment1abhay_narayane3456100% (1)
- Syndrome Acute Lung InjuryDocument7 pagesSyndrome Acute Lung InjuryJiezl Abellano AfinidadNo ratings yet
- 2N3903-2N3904 MotorolaDocument8 pages2N3903-2N3904 MotorolaLaAngelitaOropezaNo ratings yet
- JAAOS Preoperative - Peripheral - Nerve - Blocks - in Trauma. (22088)Document7 pagesJAAOS Preoperative - Peripheral - Nerve - Blocks - in Trauma. (22088)Ben QuigleyNo ratings yet
- Biomechanics LectureDocument2 pagesBiomechanics LectureOmar OsamaNo ratings yet
- Atls Trauma ThermalDocument36 pagesAtls Trauma ThermalsheisamarinkaNo ratings yet
- English EssayDocument3 pagesEnglish EssayMerlyn JeejoNo ratings yet
- Carte de Abstracte Cimsc 2017 1Document135 pagesCarte de Abstracte Cimsc 2017 1Remus BobârnacNo ratings yet
- Morton's NeuromaDocument8 pagesMorton's Neuromagreencrystal81No ratings yet
- 4 - Hydro Jetting and Sludge RemovalDocument18 pages4 - Hydro Jetting and Sludge RemovalPerwez21100% (2)
- Osteogenesis ImperfectaDocument25 pagesOsteogenesis ImperfectaNavya Sruthi MandapatiNo ratings yet
- X1 Air Install ManualDocument18 pagesX1 Air Install ManualNeil CzsNo ratings yet
- ch06 Lecture PPT ADocument93 pagesch06 Lecture PPT ALeona Rabe100% (3)
- The Cold Truth The Role of Cryotherapy in The Treatment of Injury and Recovery From ExerciseDocument19 pagesThe Cold Truth The Role of Cryotherapy in The Treatment of Injury and Recovery From ExerciseJacob FreemanNo ratings yet
- 19 Tibial NerveDocument38 pages19 Tibial Nerverodrigocorcino899959No ratings yet
- 1.wall of ThoraxDocument14 pages1.wall of ThoraxChandru ANo ratings yet
- Chapter 14 - Renal and Urinary ProblemsDocument8 pagesChapter 14 - Renal and Urinary ProblemscariNo ratings yet
- Orthopedic AssessmentDocument4 pagesOrthopedic Assessmentkrissh20No ratings yet
- Magnamax Operation ManualDocument73 pagesMagnamax Operation ManualMuhammed Imran Khalid100% (3)
- Your First Uke Lesson - Three Little Birds Chord ChartDocument2 pagesYour First Uke Lesson - Three Little Birds Chord CharttinaNo ratings yet
- Surgery McqsDocument43 pagesSurgery McqsDara Harish100% (4)
- Sonography of The Knee Joint PDFDocument8 pagesSonography of The Knee Joint PDFChavdarNo ratings yet
- Case Study 7 8 and 9Document32 pagesCase Study 7 8 and 9Lyca Ledesma JamonNo ratings yet
- Sorensen2 PDFDocument24 pagesSorensen2 PDFAnirban RoyNo ratings yet
- Rnbe-16-0312-Nae High Output Sell SheetDocument2 pagesRnbe-16-0312-Nae High Output Sell SheetYacine Tarik AizelNo ratings yet
- Bandaging NotesDocument5 pagesBandaging NotesadiNo ratings yet
- US Marine Corps Daily 16 ProgramDocument12 pagesUS Marine Corps Daily 16 ProgramHip Hop 1919No ratings yet
- C1, C2 InjuriesDocument58 pagesC1, C2 InjuriesVishad NaidooNo ratings yet
- Fracturi de Coloana Cervicala, Toracala Si LombaraDocument770 pagesFracturi de Coloana Cervicala, Toracala Si Lombaracomir2002100% (3)
- Tames Hi GiriDocument3 pagesTames Hi GiriDarko тралала0% (1)