Professional Documents
Culture Documents
Neonatal Complications of Premature Rupture of Membranes: Abstract
Uploaded by
Paula CyntiaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neonatal Complications of Premature Rupture of Membranes: Abstract
Uploaded by
Paula CyntiaCopyright:
Available Formats
NEONATAL COMPLICATIONS OF PREMATURE RUPTURE
OF MEMBRANES
F. Nili
*
and AA. Shams Ansari
Department of Pediatrics, Vali-e-Asr Hospital, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
Abstract- Premature rupture of membranes (PROM) is one of the most common complications of pregnancy that has a major
impact on neonatal outcomes. With respect to racial, nutritional and cultural differences between developed and developing
countries, this study was conducted to detect the prevalence of neonatal complications following PROM and the role of the
duration of rupture of membranes in producing morbidities and mortalities in these neonates in our hospital. Among 2357
pregnant women, we found 163 (6.91%) cases of premature rupture of the fetal membranes in Tehran Vali-e-Asr Hospital
during April 2001 to April 2002. Route of delivery was cesarean section in 65.6% of women. Urinary tract infection occured in
1.8%, maternal leukocytosis and fever in 20.2% and 5.5%, chorioamnionitis in 6.1%, fetal tachycardia in 1.2% and
olygohydramnios in 4.9%. Gestational age in 138 (86%) of neonates was less than 37 completed weeks. Thirty five infants
(21.47%) had respiratory distress syndrome and 33 (20.245%) had clinical sepsis. Pneumonia in 6 (3.7%) and skeletal
deformity in 7 (4.294%) were seen. Rupture of membrane of more than 24 hours duration occurred in 71 (43.6%) of the
patients. Comparison of morbidities between two groups of neonates and their mothers according to the duration of PROM
(less and more than 24 hours ) showed significant differences in NICU admission, olygohydramnios, maternal fever,
leukocytosis and chorioamnionitis rates (p<0.05). The risks of pneumonia and mortality were much higher in group with >24
hr of PROM with an odds ratio of 2.68 and 2.73, respectively. Positive blood and eye cultures were detected in 16 cases during
72 hours of age. Staphylococcus species, klebsiella, E.coli and streptococcus were the predominant organisms among positive
blood cultures. Mortality was seen in 18 (11%) of neonates because of respiratory failure, disseminated intravascular
coagulation, septic shock, and a single case of congenital toxoplasmosis. In this study, the prevalence of prematurity, sepsis and
prolonged rupture of membrane were higher than previous studies.
Acta Medica Iranica, 41(3): 175-179; 2003
Key Words: Premature rupture of membranes, Prolonged rupture of membranes, Neonatal complications.
INTRODUCTION
Premature rupture of fetal chorioamniotic
membranes by definition occurs before the onset of
labor. Premature rupture of fetal membranes (PROM)
occurs in approximately 10% of all pregnancies (1).
When this event occurs before 37 weeks of gestation,
it is deemed preterm premature rupture of membranes
(PPROM) that has been estimated to affect 3% to 4.5%
of all deliveries. The independent relationship with
perinatal complications has been illusterated by Arias
and Tomich, who have prospectively shown higher
rates of severe neonatal morbidity in pregnancies
complicated by PPROM than those caused by
idiopathic preterm labor (27% versus 15.1%, P< 0.02).
PPROM affects 32% to 40% of preterm deliveries,
with 60% to 80% of these patients entering sponta-
Received: 25 January 2003, accepted: 16 April 2003
* Correponding Author:
F. Nili, Department of Pediatrics, Vali-e Asr Hospital, School of
Medicine, Tehran University of Medical Sciences, Tehran, Iran
Tel: +98 21 6935091-9, +98 21 6927723
Fax: +98 21 6937799
E-mail: f_nili2000@yahoo.com
neous labor within 48 hours, and the subsequent
neonatal sequelae of preterm delivery ensuing (2). The
fetal and neonatal morbidity and mortality risks are
significantly affected by severity of oligohydramnious,
duration of latency, and gestation at PROM. The
primary complication for the mother is risk of
infection. Complications of PROM for the fetus and
newborn consist of prematurity, fetal distress, cord
compression, deformation and altered pulmonary
development leading to pulmonary hypoplasia and
pulmonary hypertentsion. Infectious morbidities in
mother, fetus and newborn have been related to both
PROM and prolonged rupture of membranes. For
preterm gestations with extended duration of PROM,
the risk of clinically evident chorioamnionitis seems
greatest in the first 72 hours, and decreases with
advanced latency. Cumulative data suggest that
subclinical infection may be present before PROM and
is an etiologic factor in this complication (1). Racial
differences have been appreciated among women with
PPROM. An increased incidence has been
demonstrated specifically among black patients from
5.1% to 12.5% which is contrasted with corresponding
Neonatal complications of PROM
176
white groups of 1.5% to 2.2% (4). Socioeconomic
parameters have not been found to directly influence
the occurrence of PPROM (5).The role of smoking and
sexual activity in producing PPROM are still points of
some cotroversy. Deficiencies in vitamin C, copper,
zinc, and overall nutritional status reflected by body
mass index (BMI) have been associated with increased
rates of PPROM. There seems to be a relatively strong
association between vaginal bleeding and PPROM,
with risk ranging between two folds and seven folds
higher than control patients. Cervical parameters,
multifetal preganacy, poor obstetric history, pre-
existing medical conditions like maternal hypertension
or diabetes and genital tract infection have been
suggested to have some roles on PPROM (2). With
respect to racial, nutritional, and cultural differences
between developed and developing countries, this
study was conducted to detect the prevalence of
neonatal complications following PROM and the role
of the duration of rupture of membranes in producing
these morbidities and mortalities in neonates in our
hospital.
MATERIALS AND METHODS
All pregnant women with their babies who had the
history of rupture of membranes before labor were
entered into this study from April 2001 to April 2002.
Time of rupture of membranes from delivery, neonatal
sepsis, pneumonia, respiratory distress, NICU
admission, skeletal deformities, mortality and maternal
characteristics comprising olygohydramnios, fever,
leukocytosis, chorioamnionitis, urinary tract infections,
fetal heart rate > 160 were recorded and the data
compared in two groups ROM < 24 hrs (group 1) and
ROM> 24 hrs (group2) and using Chi -square test to
compare the two groups.
RESULTS
From 2357 pregnant women 163 (6.91%) were
complicated with PROM. Route of delivery in 107
(65.6%) women was cesarean section. Fifty eight
percent of women received antibiotic before labor and
corticosteroid were used in 87(53.4%) of cases to
induce fetal lung maturity. Gestational age in 138
(84.66%) infants was less than 37 weeks. Mean birth
weight of these infants was 2214.7 767.04 grams.
The mean time for PROM was 90.1 hours. Ninety two
(56.4%) cases had PROM < 24 hours and 71 (43.6%)
> 24 hours. 77 (47.2%) and 86 (52.8%) of cases were
female and male respectively. 32 (19.6%) of male and
23 (14.1%) of female cases had clinical sepsis (Table
1). Comparison of Neonatal intensive care unit
(NICU) admission, olygohydramnios, maternal fever ,
leukocytosis and chorioamnionitis showed significant
differences between two groups (p<0.05). Also the
difference of mortalities between two groups was
relatively significant (P= 0.053). The risks of
pneumonia, NICU admission and mortality were
higher in group 2 (odds: 2.68, 4.12, 2.73). Club foot in
7, developmental dysplasia of hip (DDH) in 2, nasal
septal deviation in 1 and skull deformity of vertex
region in 1 were the most common deformities.
Table 1. Maternal and neonatal complications in premature rupture of membranes
Complications PROM < 24 hours PROM > 24 hours Total P value Odds ratio
Number 92 (56.4%) 71 (43.6%) 163(100%)
Clinical sepsis 30 (18.4%) 25 (15.3%) 55 (33.7%) 0.741 1.123
Pneumonia 2 (1.2%) 4 (2.5%) 6 (3.7%) 0.405 2.68
RDS 31 (33.7 %) 24 (33.3) 55 (33.7%) 0.98 1.004
NICU admission 7 (4.3%) 18 (11%) 25 (15.3 %) 0.002 4.12
Olygohydramnios 1 (1.8%) 7 (9.85%) 8 (4.9%) 0.022 9.95
Mortality 7 (7.6 %) 13 (28.3) 20 ( 12.26%) 0.053 2.73
Skeletal deformity 8 (8.6%) 6 (8.45%) 14 (8.5%) 1.00 0.96
Mat. Fever 0 9 (12.67%) 9 (5.52%) 0.000 28.12
Mat. Leukocytosis 12 (13%) 21 (29.57%) 33 (20.24%) 0.011 2.8
Choriamnionitis 0 10 (14.08%) 10 (6.134%) 0.000 31.58
UTI 2 (2.2%) 1 (1.4%) 3 (1.8%) 1.00 0.64
FHR> 160 2 (1.2%) 1 (1.4%) 3 (1.8%) 1.00 0.76
Acta Medica Iranica, Vol. 41, No. 3 (2003)
177
Positive blood and eye cultures were detected in 16
(9.8%) cases during 72 hours of birth. From 9 (5.5%)
blood cultures there were 3 klebsiella, 2
Staphylococcus aureus, 2 Staphylococcus epidermidis,
1 E. Coli and 1 Streptococcus. Sepsis was detected in
48 (34.78%) and 6 (27%) of premature and term
infants, respectively. The rate of infantile sepsis was
25%, 66.66%, 36.36% and 100% in maternal
chorioamnionitis, urinary tract infection, leukocytosis
and fever respectively. Low Apgar score was detected
in 6 infants.
DISCUSSION
Rupture of membranes before 37 weeks of
gestation accounts for 20% to 40% of PROM (3).
Prematurity is the most significant factor in the
increased perinatal morbidity and mortality associated
with PROM because delivery occurs within 7 days of
PROM in over 80% cases (4). So PROM is not an
independent risk factor for neonatal morbidity in
preterm births. Neontal morbidity is affected mainly
by prematurity itself, rather than by the occurrence of
PROM (5). 84.66% of our infants were preterm which
is more than two fold in other reported cases.
Comparing clinical sepsis, pneumonia, RDS and
mortality in two groups, there were not significant
differences relating to the time of PROM from
delivery, signifying that the time of PROM from
delivery by itself is not an indepenent risk factor for
producing neonatal morbidities. The neonatal
pulmonary consequences of PPROM include
congenital pneumonia which often is associated with
maternal chorioamnionitis and surfactant deficiency
(RDS) following preterm delivery, and pulmonary
hypoplasia and pulmonary hypertention are secondary
to interruption of fetal lung growth associated with
loss of amniotic fluid. These three conditions may
occur simultaneously in the same patient, and
presenting signs of each may overlap with other
confounding bedside diagnosis.The frequency of
pulmonary hypoplasia following midtrimester PPROM
has been reported as 0% to 24%. Kilbride et al.
identified the risk of pulmonary hypoplasia as nearly
80% with early rupture of the membranes (<25 weeks
getation) combined with duration of severe
oligohydramnios greater than 14 days (1). In our study
there was no case of pulmonary hypoplasia.
Although previous reports have suggested that
prolonged PROM might accelerate pulmonary
maturity, this effect has not consistently been
recognized. For infants with respiratory distress,
surfactant should be given as soon as possible after
birth. A recent study suggests that complicted RDS
cases, including those with superimposed asphyxia or
infection following PROM, may benefit from earlier
surfactant retreatment. In addition to RDS, severe
preterm infants are at risk for other major morbidities,
including intraventricular hemorrhage, necrotizing
enterocolitis, retinopathy of prematurity, and chronic
lung disease. Limited outcome data suggest that these
complications occur at similar rates for PROM
survivors as for infants born without PROM (1). In our
study 33.7% of infants had RDS and the statistical
difference between two groups was not significant that
may support this idea.
In PROM cases deformities are significantly related
to the duration and severity of oligohydramnios. The
reported incidence of skeletal abnormalities in PROM
series ranged from 0% to 35% (10,11). Commonly, the
newborn`s feet or hands are broad and spade-like and
may be somewhat edematous. In vertex presentation,
the skull is elongated with molding, often with potter
facies. Breech positioning, which is two to three times
more frequent following oligihydramnios in early
midtrimester, may result in marked fetal hip flexion
contractures and hyperextention of the lower
extremities with an increased risk of hip dislocation
(12). In our study 8.5% of infants had skeletal
defomities with club foot being the most common.
Incidence of documented sepsis in the neontes born to
mothers with rupture of membranes greater than 24
hours is approximately 1%. When signs and symptoms
of chorioamnionitis are present the risk of proven
sepsis increases to 3% to %5. When prolonged rupture
of membranes accompanied with prematurity, the
incidence of proven sepsis is 4-6% and in highly
suspected and proven sepsis the rate is 7- 11% (6).
Although the risk of neonatal sepsis is reduced after
intrapartum prophylaxis, a 5% to 8% risk remains (1).
Documented sepsis during 72 hours of life was
detected in 5.52% of our patients and 55.8% of
women received antibiotics. Our suspected cases of
sepsis were 33.7% of whom 15.3% were located in
group 2. Sign of infection may be difficult to assess,
particularly when the newborn has been partially
treated. For preterm infants it is recommended that a
sepsis work-up and empiric antimicrobial therapy is
started shortly after birth. Depending on the antibiotic
used for maternal prophylaxis, resistant or unusual
organisms may predominate as etiologic agents for
neonatal sepsis. As always, treatment should be based
Neonatal complications of PROM
178
on local experience and upon invitro sensitivity testing
of the identified organism (1).
Table 2. Comparison of morbidities between our study
with the other`s
Our study Other`s
Incidence of PROM 6.91% 10%
Indidence of PPROM 5.85 3%-4.5%
Incidence of PPROM 84.66% 20-40%
Pulmonary hypoplasia 0% 0%-24%
RDS 33.7% 39%
Skeletal deformity 8.5% 0%-35%
Cesarean section 65.6% 59.9%
Prolonged ROM 71% 48 %
Sepsis 5.5% 3.8%
Comparison of incidence of morbidities between
our study and that of others showed that prematurity,
sepsis and cesarean section in our study were higher.
Respecting the sample size for maternal risk factors in
our study, it seems that maternal infections like urinary
tract infection and chorioamnionitis appear to be much
higher in group 2 and neonatal infection occurred more
when maternal infection exists. Because most of the
women with leukocytosis in group with PROM >24
hrs were received corticosteroid, the difference
between two groups may not be reliable. Maternal
colonization with group B stereptococcus (GBS)
without other clinical complications carries a risk of
neonatal sepsis of 0.55 to 1%, similar to the risk of
uncomplicated prolonged rupture of membranes. The
density of maternal and neonatal GBS colonization is
an infrequent quantified but potentially important
determinant of the risk of invasive disease. Light
colonization may lead to infection, when accompanied
by PROM (13). In our study gram negative organisms
and staphylococcus species were the most prevalent
agents and streptococcus species were detected in only
one case. It has been suggested that inflammatory
mediators may have a possible role in brain injury,
even in the absence of overt sepsis. Because these
inflammatory markers are elevated following PROM
and preterm labor, there remain concerns that these
obstetric complications may have long term neurologic
consequences. This hypothesis is further supported by
a recent epidemiologic study in which the risk of
spastic diplegia was found to be increased in newborns
whose delivery was complicated by PROM. Whether
intrapartum antibiotic prophylaxis can modify these
effects in PROM cases awaits further investigation (1).
With respect to our higher rate of infection and
prematurity in pregnancies complicated with PROM
and the probable risk of future neurologic sequela and
other neonatal complications, it seems investigating
about the etiologies of PROM and the type of infection
in these these pregnancies is mandatory.
REFERENCES
1. Killbride HW, Thibealt DW. Neonatal compli-
cations of preterm premature rupture of membranes,
pathophysiology and management. Clinics in
Perinatology 2001; 28: 761-785.
2. Lee T, silver H. Etiology and epidemiology of
preterm premature rupture of membranes. Clinics in
Perinatology 2001; 28:721-734.
3. Arias F, Tomich P. Etiology and outcome of low
birth weight and preterm infants. Obst Gynecol 1982;
60:277.
4. Savitz DA, Blackmore CA, Thorp JM.
Epidemiologic characteristics of preterm delivery.
Etiologic heterogeneity. Am J Obstet Gynecol 1991;
164: 467.
5. Miller HC, Jekel JF. Epidemiology of spontaneous
premature rupture of membranes : Factors in preterm
births. Yale J Biol Mede 1989; 62: 241.
6. Merenstein GB, Weisman LE. Premature rupture of
the membranes. Neonatal consequences. Semin
Perinatol 1996; 20(5): 375-380.
7. Svigos JM, Robinson JS, Vigne S. Prelabor ruture
of the membranes. In: James DK, Steer PJ, Weiner CP,
Gonik B (eds). High risk pregnancy management
options. 2th edition. W.B.Saunders. London 1999;
1015-1025.
8. Furman B, Shoham-Vardi, Bashiri A, Erez O,
Mazor M. Preterm premature rupture of membranes is
not an independent risk factor for neonatal morbidity. J
Matern Fetal Med 2001; 10(2): 107-111.
9. Kurkinen-Raty M, Koivisto Jouoppila P. Perinatal
and neonatal outcome and late pulmonary sequelae in
infants born after preterm premature ruture of
membranes. Obstet Gynecol 1998; 92: 408-415.
Acta Medica Iranica, Vol. 41, No. 3 (2003)
179
10. Bengston JM, VanMareter LJ, Barss VA, et al.
Preganancy outcome after premature rupture of the
membranes at or before 26 weeks gestation. Obstet
Gynecol 1989; 73: 921-927.
11. Moretti M, Sibai BM. Maternal and perinatal
outcome of expectant management dilema. Am J
Obstet Gynecol 1993; 168: 503-507.
12. Killbride HW, Yeast JD, Thibealt DW. Intrapartum
and delivery room management of premature ruture of
membranes complicated by olygohydramnios. Clin
Perinat 1989; 16: 863-888.
13. Gerdes JS. Clinicopathologic approach to the
diagnosis of neonatal sepsis. Clinics in Perinatology
1991; 18(2): 361-381.
You might also like
- Neonatal Complications of Premature Rupture of Membranes: AbstractDocument5 pagesNeonatal Complications of Premature Rupture of Membranes: AbstractAris BayuNo ratings yet
- Thyroid and Pregnancy OutcomeDocument9 pagesThyroid and Pregnancy OutcomeCindy KestyNo ratings yet
- Placenta PreviaDocument5 pagesPlacenta PreviaKuro HanabusaNo ratings yet
- Prevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 WeeksDocument4 pagesPrevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 WeeksTriponiaNo ratings yet
- Adekanle Et AlDocument5 pagesAdekanle Et AlI_Ketut_Wahyu_MerthaNo ratings yet
- Neonatal Sepsis in Low Birth Weight Infants in Dr. Soetomo General HospitalDocument4 pagesNeonatal Sepsis in Low Birth Weight Infants in Dr. Soetomo General HospitalMelati Nurul UtamiNo ratings yet
- An Overview of Referral Patients With Severe Preeclampsia in Obstetric and Gynecology Department, Dr. Soetomo Hospital Surabaya in 2011 An OverviewDocument10 pagesAn Overview of Referral Patients With Severe Preeclampsia in Obstetric and Gynecology Department, Dr. Soetomo Hospital Surabaya in 2011 An OverviewAnonymous y6NmP9NHkYNo ratings yet
- A 5-Year Review of Pattern of Placenta Previa in Ilorin, NigeriaDocument6 pagesA 5-Year Review of Pattern of Placenta Previa in Ilorin, Nigeriaamalia chairunnisaNo ratings yet
- Research Article: Hindawi Biomed Research International Volume 2018, Article Id 7162478, 6 PagesDocument7 pagesResearch Article: Hindawi Biomed Research International Volume 2018, Article Id 7162478, 6 PagesKarla OrtizNo ratings yet
- Journal (Preterm Labor)Document5 pagesJournal (Preterm Labor)Zhyraine Iraj D. CaluzaNo ratings yet
- Article1380102045 - Sebastian Et AlDocument4 pagesArticle1380102045 - Sebastian Et AlAndrea RivaNo ratings yet
- Jurnal ReadingDocument4 pagesJurnal ReadingKhairunisaNo ratings yet
- Alexander 1999Document5 pagesAlexander 1999Hòa HồNo ratings yet
- Preterm Premature Rupture of Membranes: Diagnosis, Evaluation and Management StrategiesDocument6 pagesPreterm Premature Rupture of Membranes: Diagnosis, Evaluation and Management StrategiesResi Lystianto PutraNo ratings yet
- Incidence of Morbidity and Mortality in Neonate Born To Mothers With Premature Rupture of MembranesDocument7 pagesIncidence of Morbidity and Mortality in Neonate Born To Mothers With Premature Rupture of MembranesTatik HandayaniNo ratings yet
- Karakteristik Penderita Preeklamsi Dan Eklamsi Yang Dirawat Inap Di Rumah Sakit Immanuel Bandung Periode Tahun 2006 - 2008Document6 pagesKarakteristik Penderita Preeklamsi Dan Eklamsi Yang Dirawat Inap Di Rumah Sakit Immanuel Bandung Periode Tahun 2006 - 2008Radi PdNo ratings yet
- Changed Indications For Cesarean Sections: Ylva Vladic Stjernholm, Karin Petersson & Eva EnerothDocument5 pagesChanged Indications For Cesarean Sections: Ylva Vladic Stjernholm, Karin Petersson & Eva EnerothSam Ath SanNo ratings yet
- Maternal and Obstetric Outcome of Women With Epilepsy 2009 SeizureDocument4 pagesMaternal and Obstetric Outcome of Women With Epilepsy 2009 Seizurebilal hadiNo ratings yet
- High Rate of Early Onset Preeclampsia in MauritiusDocument4 pagesHigh Rate of Early Onset Preeclampsia in MauritiusHarvey MatbaganNo ratings yet
- Maternal and Fetal Outcomes in Term Premature Rupture of MembraneDocument6 pagesMaternal and Fetal Outcomes in Term Premature Rupture of MembraneMuhammad Fikri RidhaNo ratings yet
- 2040 7117 1 PBDocument8 pages2040 7117 1 PBrizki ameliaNo ratings yet
- 33873-Article Text-121761-1-10-20170831Document6 pages33873-Article Text-121761-1-10-20170831AnggaNo ratings yet
- Pre Discharge Neonatal Mortality and Morbidity of Extreme Preterm InfantsDocument4 pagesPre Discharge Neonatal Mortality and Morbidity of Extreme Preterm InfantsDr. Nimesha GamhewageNo ratings yet
- Contemporary Diagnosis and Management of Preterm Premature Rupture of MembranesDocument12 pagesContemporary Diagnosis and Management of Preterm Premature Rupture of Membranesriena456No ratings yet
- Ijrm 11 385Document6 pagesIjrm 11 385Obgyn Maret 2019No ratings yet
- PT Resp OutcomesDocument6 pagesPT Resp OutcomesHarish SudarsananNo ratings yet
- Risk Factors of Persistent Pulmonary Hypertension of Newborn (PPHN) in Different GestationDocument6 pagesRisk Factors of Persistent Pulmonary Hypertension of Newborn (PPHN) in Different Gestationzionluis007No ratings yet
- Chapter 3Document32 pagesChapter 3Vaibhav JainNo ratings yet
- None 3Document7 pagesNone 3Sy Yessy ParamitaNo ratings yet
- Poryo2018 IvhDocument8 pagesPoryo2018 IvhGabriel DaneaNo ratings yet
- Patient's Profile With Hypertension in Pregnancy PatientsDocument6 pagesPatient's Profile With Hypertension in Pregnancy PatientsHendrik SuTopo LidaprajaNo ratings yet
- Dengue in Pregnancy: AbstractDocument3 pagesDengue in Pregnancy: AbstractsharenNo ratings yet
- Ileus and Intestinal Obstruction - Comparison Between Children and AdultsDocument5 pagesIleus and Intestinal Obstruction - Comparison Between Children and Adultsaliy_drNo ratings yet
- Feto-Maternal Outcomes in Hypertensive Disorders of Pregnancy in A Tertiary Care Hospital: A Retrospective StudyDocument7 pagesFeto-Maternal Outcomes in Hypertensive Disorders of Pregnancy in A Tertiary Care Hospital: A Retrospective StudyIJAR JOURNALNo ratings yet
- Objectives:: CorrespondenceDocument5 pagesObjectives:: Correspondenceraudatul jannahNo ratings yet
- Maternal Hypothyroidism During Pregnancy and The Risk of Pediatric Endocrine Morbidity in The OffspringDocument6 pagesMaternal Hypothyroidism During Pregnancy and The Risk of Pediatric Endocrine Morbidity in The OffspringlananhslssNo ratings yet
- Preterm Premature Rupture of Membranes in The Presence of Cerclage: Is The Risk For Intra-Uterine Infection and Adverse Neonatal Outcome Increased?Document6 pagesPreterm Premature Rupture of Membranes in The Presence of Cerclage: Is The Risk For Intra-Uterine Infection and Adverse Neonatal Outcome Increased?stephaniedianNo ratings yet
- Acta Obstet Gynecol Scand - 2011 - STJERNHOLM - Changed Indications For Cesarean SectionsDocument5 pagesActa Obstet Gynecol Scand - 2011 - STJERNHOLM - Changed Indications For Cesarean SectionsAli QuwarahNo ratings yet
- Acute Pyelonephritis in Pregnancy: An 18-Year Retrospective AnalysisDocument6 pagesAcute Pyelonephritis in Pregnancy: An 18-Year Retrospective AnalysisIntan Wahyu CahyaniNo ratings yet
- Acute Pyelonephritis in PregnancyDocument7 pagesAcute Pyelonephritis in PregnancyKvmLlyNo ratings yet
- Articulo 5Document6 pagesArticulo 5Monica ReyesNo ratings yet
- Association Between Polymorphisms in CXCR2 Gene and PreeclampsiaDocument8 pagesAssociation Between Polymorphisms in CXCR2 Gene and PreeclampsiaalyneNo ratings yet
- Correlation of Myometrial Thickness and The Latency Interval of Women With Preterm Premature Rupture of The MembranesDocument6 pagesCorrelation of Myometrial Thickness and The Latency Interval of Women With Preterm Premature Rupture of The MembranesstephaniedianNo ratings yet
- 140 140 1 PBDocument4 pages140 140 1 PBMina LelymanNo ratings yet
- 04 Shehla20Noor 20PREVALANCE20OF20PRROM20AND20ITS20OUTCOMEDocument5 pages04 Shehla20Noor 20PREVALANCE20OF20PRROM20AND20ITS20OUTCOMEMirachel AugustNo ratings yet
- Short-Term Outcomes and Mortality of Late Preterm Infants: Cahide Bulut, Tuğba Gürsoy, Fahri OvalıDocument6 pagesShort-Term Outcomes and Mortality of Late Preterm Infants: Cahide Bulut, Tuğba Gürsoy, Fahri OvalızulfikarNo ratings yet
- KPD 2Document9 pagesKPD 2Muh AqwilNo ratings yet
- Prognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisDocument6 pagesPrognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisWulan CerankNo ratings yet
- Al Riyami-2020-Respiratory Distress Syndrome IDocument6 pagesAl Riyami-2020-Respiratory Distress Syndrome IHidayatt NurulNo ratings yet
- Alteration of The Amniotic Fluid and Neonatal Outcome 2004Document5 pagesAlteration of The Amniotic Fluid and Neonatal Outcome 2004Sergio CuervoNo ratings yet
- Kim 2006 Neonatal Outcome After Preterm Delivery in HELLPDocument6 pagesKim 2006 Neonatal Outcome After Preterm Delivery in HELLPMeta ParamitaNo ratings yet
- Clinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenDocument4 pagesClinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenNurul Huda KowitaNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument7 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologySuis MionooNo ratings yet
- Placental Abruption in Term and Preterm.8 PDFDocument8 pagesPlacental Abruption in Term and Preterm.8 PDFMuhammad Riza FahlawiNo ratings yet
- Less Is More Modern NeonatologyDocument11 pagesLess Is More Modern NeonatologyEN BUNo ratings yet
- 77754571Document7 pages77754571stephaniedianNo ratings yet
- Sayar, 2011Document6 pagesSayar, 2011Cristina CarpioNo ratings yet
- Obstetrical Outcomes in Women With ChorioamnionitisDocument6 pagesObstetrical Outcomes in Women With ChorioamnionitisCentral Asian StudiesNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)From EverandComplementary and Alternative Medical Lab Testing Part 1: EENT (Eyes, Ears, Nose and Throat)No ratings yet
- Fast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeFrom EverandFast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeNo ratings yet
- Hi V StrategyDocument1 pageHi V StrategyPaula CyntiaNo ratings yet
- 71 142 1 PBDocument5 pages71 142 1 PBYuliana PurnamasariNo ratings yet
- Predicting rRNA-, RNA-, and DNA-binding Proteins From Primary Structure With Support Vector MachinesDocument10 pagesPredicting rRNA-, RNA-, and DNA-binding Proteins From Primary Structure With Support Vector MachinesPaula CyntiaNo ratings yet
- 175131Document28 pages175131Paula CyntiaNo ratings yet
- Ijtld 1471 - 2Document7 pagesIjtld 1471 - 2Paula CyntiaNo ratings yet
- 92 104 April Vol - 30 No - 2 2010 - 2Document13 pages92 104 April Vol - 30 No - 2 2010 - 2Paula CyntiaNo ratings yet
- 92 104 April Vol - 30 No - 2 2010 - 2Document13 pages92 104 April Vol - 30 No - 2 2010 - 2Paula CyntiaNo ratings yet
- 92 104 April Vol - 30 No - 2 2010 - 2Document13 pages92 104 April Vol - 30 No - 2 2010 - 2Paula CyntiaNo ratings yet
- MemantineDocument7 pagesMemantineroboNo ratings yet
- Mix It Up and SqueezeDocument3 pagesMix It Up and Squeezeapi-233757247100% (1)
- Antidepression ReikiDocument6 pagesAntidepression ReikiDoc Lyman88% (8)
- Curriculum Vitae: Dr. Avinash K. Jangde - . - ., - . (A)Document5 pagesCurriculum Vitae: Dr. Avinash K. Jangde - . - ., - . (A)Mohammad TariqNo ratings yet
- Msds Aplus 110 Semen AcianDocument5 pagesMsds Aplus 110 Semen AcianWidia YpnNo ratings yet
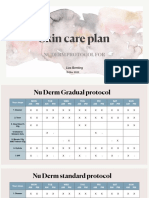
- Skin Care Plan: Nu Derm Protocol ForDocument7 pagesSkin Care Plan: Nu Derm Protocol ForsheilaNo ratings yet
- Outbreak Investigation Part 1 PDFDocument4 pagesOutbreak Investigation Part 1 PDFashythegreat93No ratings yet
- Trust Me, Im A (Junior) Doctor (Pemberton, Max (Pemberton, Max) )Document234 pagesTrust Me, Im A (Junior) Doctor (Pemberton, Max (Pemberton, Max) )Rakshith BalajiNo ratings yet
- AP Research PresentationDocument26 pagesAP Research PresentationCameron SherryNo ratings yet
- Visual NeglectDocument2 pagesVisual NeglectPierre A. RodulfoNo ratings yet
- Spring Meadows Hospital VsDocument10 pagesSpring Meadows Hospital VsManoj Kumar MNo ratings yet
- Bishara, R. - Qualification Versus ValidationDocument4 pagesBishara, R. - Qualification Versus ValidationLuis Gustavo PachecoNo ratings yet
- 11th Grade Before Band Aids TextDocument1 page11th Grade Before Band Aids Textعبدالرحمن باجسيرNo ratings yet
- Sodium Chloride (Rock Salt) MSDS: Section 1: Chemical Product and Company IdentificationDocument6 pagesSodium Chloride (Rock Salt) MSDS: Section 1: Chemical Product and Company IdentificationMohamed MaghawryNo ratings yet
- Impression Making in Complete DentureDocument128 pagesImpression Making in Complete DentureBharanijaNo ratings yet
- Article - CVD Cardiac Arrest - Bls AclsDocument2 pagesArticle - CVD Cardiac Arrest - Bls AclsAkhosh SomarajanNo ratings yet
- TheTranssexualEmpire JaniceRaymondDocument254 pagesTheTranssexualEmpire JaniceRaymondCaroline Jamhour60% (5)
- Daftar Pustaka NewDocument2 pagesDaftar Pustaka NewRini LianingsihNo ratings yet
- Tetracycline, Doxycycline, minocycline-Tetracyclines-InfenctionsDocument1 pageTetracycline, Doxycycline, minocycline-Tetracyclines-InfenctionsNatalia SpencerNo ratings yet
- Pebc Evaluating Exam Sample QuestionDocument50 pagesPebc Evaluating Exam Sample QuestionZain zanzoonNo ratings yet
- Parenteral NutritionDocument8 pagesParenteral NutritionivanNo ratings yet
- 04-09-12 EditionDocument28 pages04-09-12 EditionSan Mateo Daily JournalNo ratings yet
- 2023 Aaha Senior Care Guidelines For Dogs and CatsDocument21 pages2023 Aaha Senior Care Guidelines For Dogs and CatsisvpNo ratings yet
- Aseptic MeningitisDocument24 pagesAseptic Meningitisidno1008100% (1)
- Item Balance Per Unit RPTDocument60 pagesItem Balance Per Unit RPTYogie 1290No ratings yet
- Turpentine Oil Poisoning MedlinePlus Medical EncyclopediaDocument4 pagesTurpentine Oil Poisoning MedlinePlus Medical Encyclopediapiemar10No ratings yet
- Disease Deficient Enzyme Cardinal Clinical Features Glycogen Structure Von Gierke'sDocument84 pagesDisease Deficient Enzyme Cardinal Clinical Features Glycogen Structure Von Gierke'sclubstar100% (4)
- DentistDocument3 pagesDentistuhurtuyNo ratings yet
- Cassida Fluid GL 220-SdsDocument5 pagesCassida Fluid GL 220-SdsFajar EkoNo ratings yet
- Love Pain e Book PDFDocument14 pagesLove Pain e Book PDFTina AnesNo ratings yet