Professional Documents
Culture Documents
2 PDF
2 PDF
Uploaded by
eduar2308doOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2 PDF
2 PDF
Uploaded by
eduar2308doCopyright:
Available Formats
Fat and carbohydrate metabolism during exercise in late-onset Pompe disease
Nicolai Preisler
a,
, Pascal Laforet
b
, Karen Lindhardt Madsen
a
, Regitze Slling Hansen
a
, Zoltan Lukacs
c
,
Mette Cathrine rngreen
a
, Arnaud Lacour
d
, John Vissing
a
a
Neuromuscular Research Unit, Department of Neurology, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark
b
Centre de Rfrence de pathologie neuromusculaire Paris-Est, Groupe Hospitalier Piti-Salptrire, Assistance Publique-Hpitaux de Paris, Paris, France
c
University Medical Center of Hamburg-Eppendorf, Hamburg, Germany
d
Center for Rare Neuromuscular Diseases, University Hospital, Lille, France
a b s t r a c t a r t i c l e i n f o
Article history:
Received 1 July 2012
Received in revised form 25 August 2012
Accepted 26 August 2012
Available online 31 August 2012
Keywords:
Metabolic myopathy
Glycogen storage disease type II
Exercise
Stable isotopes
Skeletal muscle metabolism
Glycogen
Pompe disease is caused by absence of the lysosomal enzyme acid alpha-glucosidase. It is generally assumed
that intra-lysosomal hydrolysis of glycogen does not contribute to skeletal muscle energy production during
exercise. However, this hypothesis has never been tested in vivo during exercise. We examined the metabolic
response to exercise in patients with late-onset Pompe disease, in order to determine if a defect in energy
metabolism may play a role in the pathogenesis of Pompe disease. We studied six adult patients with
Pompe disease and 10 healthy subjects. The participants underwent ischemic forearm exercise testing, and
peak work capacity was determined. Fat and carbohydrate metabolism during cycle exercise was examined
with a combination of indirect calorimetry and stable isotope methodology. Finally, the effects of an IV glu-
cose infusion on heart rate, ratings of perceived exertion, and work capacity during exercise were deter-
mined. We found that peak oxidative capacity was reduced in the patients to 17.6 vs. 38.8 ml kg
1
min
1
in healthy subjects (p=0.002). There were no differences in the rate of appearance and rate of oxidation
of palmitate, or total fat and carbohydrate oxidation, between the patients and the healthy subjects. None
of the subjects improved exercise tolerance by IV glucose infusion. In conclusion, peak oxidative capacity is
reduced in Pompe disease. However, skeletal muscle fat and carbohydrate use during exercise was normal.
The results indicate that a reduced exercise capacity is caused by muscle weakness and wasting, rather
than by an impaired skeletal muscle glycogenolytic capacity. Thus, it appears that acid alpha-glucosidase
does not play a signicant role in the production of energy in skeletal muscle during exercise.
2012 Elsevier Inc. All rights reserved.
1. Introduction
Pompe disease, GSD (glycogen storage disease) type II (OMIM
#232300) is an autosomal recessively inherited disorder, caused by
mutations in the gene encoding the lysosomal enzyme acid alpha-
1,4-glucosidase (GAA; EC 3.2.1.20) [1]. GAA degrades lysosomal gly-
cogen to glucose, and low or absent activity of GAA causes glycogen
accumulation within lysosomes [2].
Clinically, Pompe disease presents as a continuum of phenotypes.
In the classic infantile onset formof the disease, presentation is within
the rst months after birth, characteristically as a oppy infant, with a
severe cardiomyopathy. Untreated, most of these children die within
the rst year of life. More commonly, Pompe disease presents later
in life, with primarily skeletal muscle dysfunction, and no cardiac in-
volvement. The variability in phenotypes and rate of progression are
due to the large genetic heterogeneity of the disease, and correlate
with residual enzyme activity [1].
Glycogen storage diseases are caused by deciencies in the specic
enzymes involved in glycogen metabolismor in the glycolytic pathway.
The GSDs that affect skeletal muscle can be divided into two groups,
based on the symptoms from skeletal muscle [3,4]. One group com-
prises the GSDs associated with exercise intolerance as the main symp-
tom. McArdle disease (myophosphorylase deciency, GSD type V) is
the most common of these. In this group of GSDs, the symptoms from
skeletal muscle are provoked by exercise, which may cause cramps,
myalgia, excessive fatigue, and even rhabdomyolysis. The other group
consists of the GSDs where skeletal muscle involvement is primarily
inthe formof a progressive skeletal muscle weakness and wasting. Clin-
ically, Pompe disease belongs to the second group. However, even
though protein metabolism and dietary interventions in combination
with exercise have been investigated in a fewpatients, fat and carbohy-
drate metabolism during exercise is unknown in Pompe disease [59].
Molecular Genetics and Metabolism 107 (2012) 462468
Abbreviations: GSD, Glycogen storage disease; GAA, Acid alpha-1,4-glucosidase;
BMI, Body mass index; VO
2peak
, peak oxidative capacity; W
peak
, peak workload; RPE,
Ratings of perceived exertion; R
a
, Rate of appearance; R
d
, Rate of disappearance;
ROX, Rate of oxidation; RER, Respiratory exchange ratio; FFA, Free fatty acids.
Statistical analysis: Statistical analysis was conducted by Nicolai Preisler, MD.
Study funding: The study was supported by the Genzyme Corporation.
Corresponding author at: Neuromuscular Research Unit 3342, Department of Neu-
rology, University of Copenhagen, Rigshospitalet, Blegdamsvej 9, DK-2100 Copenhagen,
Denmark. Fax: +45 3545 6138.
E-mail address: npreisler@hotmail.com (N. Preisler).
1096-7192/$ see front matter 2012 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.ymgme.2012.08.019
Contents lists available at SciVerse ScienceDirect
Molecular Genetics and Metabolism
j our nal homepage: www. el sevi er . com/ l ocat e/ ymgme
Catabolismof cytoplasmic glycogen is an essential source of fuel for
contracting muscles, and the relative proportion of energy produced
fromglycogenolysis increases with exercise intensity [10]. The impor-
tance of GAA for glucose homeostasis at rest in rats, suggests that
GAA could play a role in maintaining cellular energy homeostasis in
humans, especially when energy requirements are high, as they are
during exercise [1113]. Therefore, and impaired intra-lysosomal gly-
cogen breakdown could contribute to exercise intolerance and the
pathogenesis of skeletal muscle damage in Pompe disease.
The aim of this study was therefore to examine fat and carbohy-
drate metabolism in patients with late-onset Pompe disease during
cycle-ergometry exercise with stable isotope methodology and indi-
rect calorimetry, and anaerobic metabolism with ischemic forearm
exercise. We hypothesized that a lack of lysosomal glycogen turnover
could lead to a cytoplasmic glucose decit and energy shortage during
exercise, and that this could contribute to the pathogenesis of Pompe
disease. To further test this hypothesis, we also examined whether an
IV infusion of glucose could improve the capacity for work in patients
with Pompe disease, as it does in McArdle disease [14].
2. Methods
For a detailed description of the methods applied in this study
please refer to the Supplemental data, which is available online.
2.1. Subjects
In a casecontrol designed experimental study, six patients with
Pompe disease were included (Table 1, demographic data). Their re-
sults were compared with 10 healthy (ve men and ve women)
age-matched (37 (SD 14)years; BMI, 24.1 (SD 5.2)kg/m
2
) sedentary
healthy subjects.
Patients with enzymatic and genetically veried Pompe disease
between the ages of 18 and 65 years were included. The purpose of
the study was to determine metabolism during exercise in patients
not currently receiving enzyme replacement therapy. Therefore, treat-
ment with alglucosidase alpha (Myozyme, Genzyme Corporation,
Cambridge, MA) was paused approximately three weeks before test-
ing, in treated patients (Table 1, demographic data). A dried blood-
spot test assessed GAA activity in each individual on the rst day of
testing, to verify that GAA activity was minimal [15,16].
2.2. Exercise testing
The patients and the healthy subjects participated in all of the
tests, which were conducted on three consecutive days.
2.2.1. Ischemic forearm exercise testing (day one)
This test was performed to examine lactate and ammonia re-
sponses during anaerobic conditions, and to observe the pattern of
fatigue. A Smedley Handgrip Dynamometer (Stoelting CO., Illinois,
USA) was used. Before testing, the maximal voluntary force was de-
termined. During the ischemic forearm exercise test, the subjects
were instructed to work continuously for one minute, rhythmically
squeezing the handgrip maximally for one second, and relaxing the
next. Blood samples were obtained as shown in Fig. 1. Force was
recorded during exercise.
2.2.2. Measurements of maximal capacity for work (day one)
This test was conducted approximately one hour after the ische-
mic forearm exercise test, and was used to determine the proper
workload to be used in the tests on days two and three. The peak ox-
idative capacity (VO
2peak
), and the peak workload (W
peak
) were mea-
sured by an incremental exercise test on a cycle-ergometer (Monark
939E, Monark Exercise AB, Sweden) [17]. Pulmonary gas-exchange
was measured continuously with breath-by-breath indirect calorime-
try (Cosmed Quark b
2
, Cosmed Srl, Italy).
2.2.3. Fat and carbohydrate metabolism during exercise (day two)
This test was performed to determine fat and carbohydrate oxida-
tion during exercise. The subjects arrived in the laboratory in the
morning, after having breakfast. Catheters were inserted in arm
veins for stable isotope infusion and for blood sampling. A heating
pad was used to arterialize blood samples and was wrapped around
the arm and hand, before drawing blood samples [18]. Blood and
breath samples were collected simultaneously. After collection of
background samples, a primed, constant-rate infusion of [U-
13
C
16
]-
palmitate (primed by a NaH
13
CO
3
bolus) was delivered by a Gemini
PC2 pump (IMED, San Diego, CA, USA). Blood and breath samples
were collected at 10-min intervals, the rst sample after 100 min of
isotope infusion, and the last one after 30 min of exercise. Two hours
after the isotope infusion was started, the subjects cycled for 32 min
at a workload corresponding to approximately 70% of VO
2peak
. Heart
rate was monitored continuously during exercise, RPE (ratings of
perceived exertion) every other minute, and pulmonary gas exchange
was measured with indirect calorimetry during exercise [19]. After
32 min of exercise, workload was step-wise increased every other
minute. The subjects reached the W
peak
determined on day one after
36 min of exercise, and they were encouraged to keep on cycling for
as long as possible, continuing the step-wise increases in workload.
At time of exhaustion a nal blood sample was drawn.
2.2.4. IV glucose supplementation (day three)
The principle behind the use of stable isotopes to measure endog-
enous metabolism is to infuse minute amounts of tracers that do not
affect metabolism [20]. Hence, the stable isotope trial on day two was
used as a placebo trial for the IV glucose infusion trial. The IV glucose
trial was performed to examine if the subjects' work capacity im-
proved with an IV glucose infusion. Improvement occurs in patients
with signicant blocks in skeletal muscle carbohydrate use and
would be evidenced by a marked decrease in heart rate and RPE, or
by a higher peak workload at the end of exercise [14,21]. The subjects
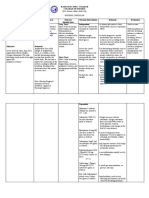
Table 1
Demographic data of the patients with Pompe disease.
Patient no.
(gender)
Age
(years)
BMI
(kg/m
2
)
Treatment stopped
(days) before testing
FVC (L) sitting/supine Mutation Age at onset of
weakness (years)
6 min walking
test (meters)
Plasma CK
(U l
1
)
1 () 43 33.1 18 2.00/1.30 c.-32-13T>G/c.-32-13T>G 25 240 1922
2 () 63 23.0 26 2.97/2.24 c.-32-13T>G/c.3G>A 55 603 403
3 () 44 33.0 Not treated 3.65/3.50 c.-32-13T>G/c.2481+102_2646+31del 31 448 521
4 () 55 28.6 16 1.53/0.91
a
c.-32-13T>G/c.693-1G>C 45 350 364
5 () 20 21.9 Not treated 6.39/5.69 c.-32-13T>G/c.2481+102_2646+31del 2 438 1690
6 () 56 14.8 Not treated NA/2.06 c.-32-13T>G/c.2228A>G 12 253 614
Mean 46.8 25.7 20 3.31/2.62 28 369 919
SD 15.2 7.2 5 1.91/1.75 20 166 697
Legend: = male. = female. SD = standard deviation. FVC = forced vital capacity. GAA level = acid alpha-1,4-glucosidase levels measured in leucocytes (normal range 1545)
or broblasts (normal range 75110) at time of diagnosis. CK = creatine kinase (normal valuesb200 Ul
1
).
a
Patient no. 4 was on nocturnal ventilation (started 11 months prior to study inclusion).
463 N. Preisler et al. / Molecular Genetics and Metabolism 107 (2012) 462468
served as their own control and therefore, the work protocol and the
blood sampling protocol during exercise mirrored the test on day
two. Resting samples were drawn prior to giving a 125 ml IV bolus
of a 10% glucose solution followed by a continuous infusion (infusion
rate of 300 ml/h; 10% solution). Five minutes after the bolus was
given, a blood sample was drawn and exercise was started. As on
day two, the subjects were encouraged to keep on exercising for as
long as possible.
2.3. Calculations
Oxidation rates of carbohydrate and fat were calculated using a
non-protein respiratory quotient [22]. The whole-body R
a
(rate of
appearance) and R
d
(disappearance) of palmitate, and the palmitate
ROX (rate of oxidation) at rest and during exercise were calculated
using the non-steady-state equations of Steele adapted for the use
of stable isotopes [20,23].
2.4. Main outcome measures
In the ischemic forearm exercise test, the primary outcome mea-
sures were differences in mean plasma lactate and ammonia concen-
trations after forearmexercise between patients and healthy subjects.
In the test of maximal capacity for work, the primary outcome mea-
sures were differences in the VO
2peak
and the W
peak
between the pa-
tients and the healthy subjects. The primary outcome measures in the
study of fat and carbohydrate metabolism during sub-maximal exer-
cise were differences in the mean ROX and R
a
of palmitate, and differ-
ences in mean plasma lactate concentration between patients and
controls. In the IV glucose infusion trial, the patients and the healthy
subjects served as their own controls, and the primary outcome mea-
sures were changes in mean heart rate and RPE, and differences in
W
peak
, with the IV glucose infusion.
2.5. Ethics and statistics
The study was approved by the Regional Committee on Biomedical
Research Ethics of Copenhagen (approval#: H-D-2008-100). The sub-
jects received written and oral information about the study, and
signed an informed consent form. Results are displayed as means
SD, and with 95% CI. To compare differences in means during exercise
between the patients and the healthy subjects a two-sample t-test was
applied, except for the IV glucose infusion trial, where a paired t-test
was used. A p-value of b0.05 (two-tailed testing) was considered sig-
nicant. For a detailed description of the statistics, please refer to the
online Supplement.
3. Results
The activity of alpha-glucosidase at pH 3.8 with inhibition was
signicantly diminished to 0.18 nmol/spot21 h (reference range:
>0.9 nmol/spot 21 h) indicating that not signicant enzyme activity
was present before testing in the patients.
3.1. Ischemic forearm exercise
There was a normal increase in plasma lactate and ammonia con-
centrations after ischemic forearm exercise in the patients with
Pompe disease (Fig. 1). In accordance with this, the percentage drop
in force during ischemic forearm exercise was similar in both groups
(Supplemental Table 1). The pretest maximal force production was
similar in patients and the healthy subjects (Supplemental Table 1).
This was related to the typical pattern of muscle involvement in
Pompe disease, in which proximal muscles are much more affected
than distal muscles. The results indicate an intact skeletal muscle gly-
cogenolytic capacity in the patients.
3.2. Maximal capacity for work
The VO
2peak
was signicantly lower in the patients (17.6
6.2 ml kg
1
min
1
) compared to the healthy subjects (38.8
9.5 ml kg
1
min
1
) (95% CI, 30.6 to 11.8, p=0.002), and in
line with this, the W
peak
was also lower in the patients (5847 W
vs. 17854 W in healthy subjects) (95% CI, 178 to 63, p=
0.002). A similar difference was also evident in the level of absolute
oxygen uptake (Supplemental Table 1). The RER (respiratory ex-
change ratio) was 1.170.12 (range; 0.961.29) in the patients at
time of VO
2peak
. This indicates that the reduction in peak work capac-
ity most likely was due to weakness, and not due to a block in skeletal
muscle carbohydrate use.
3.3. Fat and carbohydrate metabolism during exercise
The intensity of exercise in percent of peak heart rate (837% in
the patients, and 849% in healthy subjects) and W
peak
(6210%
in both groups) was similar. Two of the patients were only able to
cycle for 20 min, and therefore statistics was only applied to this
period of exercise. There was a similar increase in fat and carbohy-
drate oxidation during exercise in both groups, indicating an intact
use of glycogen during exercise in the patients. The average R
a
of
palmitate during exercise was 2.81.1 mol kg
1
min
1
in the pa-
tients, and 2.71.0 mol kg
1
min
1
in the healthy subjects (95%
Fig. 1. Lactate and ammonia concentrations before and after ischemic forearm exercise.
Plasma lactate (A) and ammonia concentrations (B) in six patients with Pompe disease
and 10 healthy subjects before and after one minute of ischemic forearm exercise. The
values are meanSE. The average concentration (the three samples after exercise) of
lactate and ammonia was statistically compared between the patients and the controls.
Mean plasma lactate concentration after exercise was 5.3 (SD 1.3)mmol l
1
in the pa-
tients, and 5.4 (SD 2.1)mmol l
1
in the healthy subjects (95% CI, 2.2 to 1.1, p=0.85).
Plasma ammonia (mean) increased to 66 (SD 31)mol l
1
in the patients and 73 (SD
21)mol l
1
in the healthy subjects (95% CI, 35 to 21, p=0.61) after exercise.
464 N. Preisler et al. / Molecular Genetics and Metabolism 107 (2012) 462468
CI, 1.1 to 1.3, p=0.86), and the average ROX of palmitate was 1.7
1.0 mol kg
1
min
1
in the patients, and 1.70.7 mol kg
1
min
1
in the healthy subjects (95% CI, 0.9 to 1.0, p=0.90) (Figs. 2A+B).
The plasma lactate concentration increased during exercise, and the
mean lactate concentration was insignicantly higher in the patients
(4.61.1 mmol l
1
) comparedto the level inthe groupof healthy sub-
jects (3.91.7 mmol l
1
) (95% CI, 1.0 to 2.5; p=0.36). Hence, no
derangements in skeletal muscle substrate use during sub-maximal ex-
ercise were found in the patients with Pompe disease. In line with these
ndings, the plasma glucose concentration remained stable throughout
the exercise period in both groups (4.60.3 mmol l
1
in the patients
and 4.80.5 mmol l
1
in the healthy subjects) (Fig. 3). Whole-body
carbohydrate and fat oxidation rates during exercise were similar in
the patients and the healthy subjects. Carbohydrate oxidation was
1.50.7 g min
1
and fat oxidation was 0.020.26 g min
1
in the
patients, which was slightly lower than in the healthy subjects (2.0
0.9 g min
1
and 0.160.15 g min
1
) (Fig. 2C). This was most likely
related to the lower work rate during exercise in the patients compared
to the work rate in the healthy subjects (Fig. 4). The concentration of
plasma free fatty acids (FFA), insulin, and epinephrine at rest and during
exercise was similar in both groups, as was the RER (Supplemental
Table 1).
3.4. IV glucose supplementation
One healthy subject did not complete the test on day three with the
same workload as on day two. He was only able to mirror his workload
for 20 min of exercise, and therefore only this part of his test was in-
cluded in the statistical analysis. Neither the patients nor the healthy
subjects improved their capacity for work with an IV glucose infusion.
The average heart rate during exercise was 13115 beats min
1
Fig. 2. Rate of appearance of palmitate, rate of oxidation of palmitate, and rate of oxida-
tion of carbohydrate. Rate of appearance (Ra) of palmitate (A), rate of oxidation of pal-
mitate (ROX) (B), and rate of oxidation of carbohydrate (C), during cycle-ergometer
exercise at ~70% of peak oxidative capacity in six patients with Pompe disease and 10
healthy subjects. The values are meanSE. Two patients were only able to cycle for
20 min (data point 30 min, N=4).
Fig. 3. Lactate and glucose concentrations during exercise. Plasma lactate concentra-
tion (A) and plasma glucose concentration (B) during cycle-ergometer exercise at
~70% of peak oxidative capacity in six patients with Pompe disease and 10 healthy sub-
jects. This test was used as a control for the IV glucose infusion test, and was therefore
followed by a stepwise increase in workload until exhaustion (rst increment after
32 min). The gray area above the x-axis in 3B is a visualization of the work protocol.
The values are meanSE. Two patients were only able to cycle for 20 min, and only
three reached the incremental phase of exercise. The lactate and glucose levels at
time of exhaustion have arbitrarily been displayed corresponding to 38 min of exer-
cise, even though exercise time differed in each subject.
465 N. Preisler et al. / Molecular Genetics and Metabolism 107 (2012) 462468
with the control infusion, and 13014 beats min
1
with the IV glu-
cose in the patients (95% CI, 4 to 8, p=0.52), and this was not differ-
ent from ndings in healthy subjects (1478 beats min
1
with
control infusion and 1479 beats min
1
with the IV glucose infu-
sion) (95% CI, 4 to 4, p=0.99) (Fig. 4). In line with this, there was
no change in RPE, which was 13.91.1 with the control infusion
and 13.51.1 with IV glucose infusion, in the patients (95% CI, 0.2
to 0.4, p=0.021; Wilcoxon Signed Rank Test p=0.09). RPE in the
healthy subjects with the control infusion was, 14.71.4 and 14.9
1.3 with glucose infusion (95% CI, 0.6 to 0.9, p=0.68). The IV glucose
infusion also failed to increase the W
peak
in the patients (W
peak
was
4844 W with placebo infusion and 4540 W with the IV glucose
infusion) (95% CI, 4 to 9; p=0.36). In the healthy subjects peak
workload with the control infusion was 15352 W, and 14536 W
with IV glucose (95% CI, 10 to 25, p=0.36) (Fig. 4).
Plasma glucose and insulin concentrations rose with IV glucose in-
fusion in both groups, and this lead to a suppression of circulating
FFAs. Carbohydrate oxidation rates tended to be higher with the IV
glucose infusion, and in accordance with this fat oxidation rates
tended to be lower. In line with a proportionate increase in carbohy-
drate use, the lactate concentration tended to rise slightly above the
levels observed during control infusion, in both groups (Fig. 3 and
Supplemental Table 2). Rest and peak plasma epinephrine concentra-
tions were lower in both groups with the IV glucose infusion (Supple-
mental Table 2).
4. Conclusion
We challenged metabolism with anaerobic and aerobic exercises
in six patients with late-onset Pompe disease. The major ndings of
this study were: 1) plasma lactate levels increased 4-fold with ische-
mic forearm exercise in patients. 2) Peak exercise capacity was
reduced in the patients. 3) Skeletal muscle substrate metabolism dur-
ing sub-maximal exercise, measured with stable isotopes and indirect
calorimetry, was comparable to ndings in healthy subjects. 4) Plas-
ma lactate levels increased signicantly and to the same extent as in
healthy subjects during aerobic exercise in the patients. 5) The pa-
tients did not improve exercise tolerance with an IV glucose infusion.
In summary, our data indicate that the skeletal muscle glycogenolytic
capacity is intact during exercise in patients with Pompe disease, de-
spite an impaired lysosomal glycogenolytic capacity. Thus, exercise
intolerance in Pompe disease is likely structurally rather than meta-
bolically related, and a consequence of the skeletal muscle weakness
and wasting in this myopathy.
The exact pathogenesis underlying the skeletal muscle dysfunc-
tion in Pompe disease remains unknown. One hypothesis is that the
massive accumulation of glycogen within skeletal muscle bers, dis-
rupts the transmission of force, and thus causes skeletal muscle
weakness [24,25]. Another proposed mechanism is that lysosomal
rupture or other autophagic events leads to leakage of proteases
and potentially other toxic elements into the cytoplasm, causing cel-
lular damage [26]. Finally, it has been proposed that GAA plays a role
in intermediary metabolism, and that local cellular energy deciency
is the cause of skeletal muscle pathology [27]. Our results support
that the cause of skeletal muscle damage is either a consequence of
structural or toxic damage, as we found no impairment of skeletal
muscle substrate metabolism, even though metabolism was chal-
lenged with moderate- to high-intensity exercise tests. This is in con-
trast to the ndings in other glycogen storage diseases, in which the
specic metabolic block causes a decrease in the glycolytic ux, and
hence a reduced capacity to generate energy [14,28].
Ischemic forearm exercise specically challenges the glycogeno-
lytic and the glycolytic capacity of skeletal muscle. A signicant
block in either of the pathways, will cause a blunted increase in plas-
ma lactate concentration, together with an excessive increase in plas-
ma ammonia, and a steep drop in force production [29]. Neither was
observed in our patients, in contrast to ndings in metabolic myopa-
thies, with a signicantly reduced capacity for skeletal muscle glyco-
gen breakdown [30,31].
We expected the patients to have a lower maximal oxidative ca-
pacity compared to the group of healthy subjects, as all of our patients
had some degree of muscle weakness and atrophy of the muscles
involved in cycling. Nevertheless, this is the rst study, to our knowl-
edge, in which the peak oxidative capacity has been quantied direct-
ly with indirect calorimetry in more than one Pompe patient [32]. The
data on substrate metabolism during exercise suggest that the re-
duced oxidative capacity in Pompe disease is a consequence of a re-
duced muscle mass, and not a consequence of a reduced capacity
for cellular respiration (secondary to a reduction in glycogenolysis).
This is in line with the results in mice lacking GAA activity, where a
normal skeletal muscle oxidative capacity was observed [25]. Even
though we did not measure the muscle mass, the degree of atrophy
was clinically evident. The patients in this study reported muscular
fatigue as the reason for terminating exercise. Three of our patients
had a reduced forced vital capacity, and diaphragmatic weakness
may have been a contributing factor to the fatigue and low VO
2peak
.
In late-onset Pompe disease, cardiac involvement is rare, but cardiac
involvement could contribute to exercise intolerance. A thorough car-
diac evaluation should always be conducted before a peak exercise
test. The patients in this study were all evaluated with echocardiogra-
phy before testing, and they all had normal ejection fractions and
structurally normal hearts.
A reduced rate of glycogen breakdown during exercise would be
expected to cause a compensatory increase in FFA oxidation. This
has been observed in McArdle disease [33]. In this study, the oxida-
tion rates of palmitate and carbohydrates, and the R
a
of palmitate in
the patients were similar to the rates measured in the healthy sub-
jects, and hence we found no signs of a compromised substrate
metabolism during exercise. Plasma lactate concentrations increased
signicantly during exercise in both groups, and were even nominally
higher in the patients. This was probably caused by a higher relative
intensity of exercise in the patients. Two of the patients were very
weak and could only complete 20 min of cycling. Therefore, these
patients were probably exercising at a higher relative intensity, as
Fig. 4. Heart rate and workload during exercise with and without IV glucose. Heart rate
and workload, with and without IV glucose infusion, in six patients with Pompe disease
and 10 healthy subjects. HR = heart rate. The values are meanSE. The subjects exer-
cise for 32 min at a workload corresponding to ~70 of peak oxidative capacity. This
phase was followed by a step-wise increase in workload until exhaustion. The stable
isotope infusion trial was used as a control trial, and the work protocol of that trial
was mirrored in the IV glucose infusion trial. An improvement in work capacity
would be evident as a signicantly decreased heart rate, or a higher peak work load
while on the glucose infusion. Only the part of the test where the workload of the pla-
cebo trial was mirrored in the IV glucose infusion test is included. Two patients only
exercised for 20 min, and one control only exercised for 20 min with the glucose
infusion.
466 N. Preisler et al. / Molecular Genetics and Metabolism 107 (2012) 462468
they would be expected to exercise longer at the intended intensity
(i.e. 70% of VO
2peak
). Overall, the lactate levels in both groups
corresponded well with the intensity of exercise, and the high lactate
levels observed in the patients, support a high and non-restricted gly-
cogenolytic ux during exercise.
Increasing blood glucose levels before exercise has a dramatic and
positive effect on the exercise capacity in McArdle disease [14,21].
Even though plasma glucose levels were doubled by the IV glucose in-
fusion, we did not observe any improvements in exercise capacity in
our patients. This further supports the theory of a preserved capacity
of skeletal muscle glycogen catabolism during exercise, and that a
compensatory increase in glucose uptake during exercise is not nec-
essary to fuel glycolysis in Pompe disease during exercise.
Currently, exercise training in Pompe disease has received much
attention, because the effect of enzyme replacement therapy on skel-
etal muscle function in late-onset Pompe disease is small. However,
a combination of exercise and enzyme replacement therapy may
improve skeletal function in Pompe disease, even more than enzyme
replacement therapy alone, due to better delivery of the recombinant
enzyme to the muscle. This is supported by recently published re-
sults in a study combining strength and aerobic exercise in Pompe
patients [34]. The oxidative capacity in our patients was reduced to
~18 ml kg
1
min
1
(range; 1325 ml kg
1
min
1
). This is as se-
vere reduction, which may have detrimental effects on general health,
as a low physical tness level is associated with an increase in all-
cause mortality [35]. Regular aerobic exercise could potentially im-
prove oxidative capacity in patients with Pompe disease, but caution
is warranted before exercise is recommended on a regular basis. The
type, intensity, and volume of exercise that may be tolerated are cur-
rently unknown for patients with Pompe disease.
Even though stable isotopes and indirect calorimetry are powerful
tools to examine human substrate metabolismin vivo during exercise,
the methods applied are limited to a whole-body evaluation, and it is
possible that abnormalities in glycogen metabolismmay exist at a cel-
lular sub-compartment level, which we cannot detect. Nevertheless,
the results of this study showthat Pompe disease differs metabolically
from most other glycogen storage diseases, in which a partial or a
complete block in carbohydrate metabolism causes exercise intoler-
ance [14,28]. Pompe disease is a metabolic myopathy and a glycogen
storage disease, which clinically and in phenotype rather mimics the
muscular dystrophies. This study also indicates that the pathogenesis
of Pompe disease may be structural rather than metabolic, and exer-
cise intolerance is a consequence of skeletal muscle weakness.
Disclosure
This study was supported by the Genzyme Corporation. NP, PL and
JV report having received research support, honoraria, and travel
funding from the Genzyme Corporation. PL and JV are members of
the Genzyme Pompe Disease Advisory Board. JV works as a consultant
for Lundbeck Pharmaceutical Company and Cardoz AB. KLM, RSH, ZL,
MC and AL report no disclosures.
Acknowledgments
The authors thank D. Goralska-Olsen, N. Pluszek and C. Caillaud
for their technical support, and M. Kronborg Have for coordinating
patients/investigator travels and accommodation.
Appendix A. Supplementary data
Supplementary data to this article can be found online at http://
dx.doi.org/10.1016/j.ymgme.2012.08.019.
References
[1] A.T. van der Ploeg, A.J. Reuser, Pompe's disease, Lancet 372 (2008) 13421353.
[2] H.G. Hers, Alpha-glucosidase deciency in generalized glycogen storage disease
(Pompe's disease), Biochem. J. 86 (1963) 1116.
[3] P. Laforet, D.A. Weinstein, P.A. Smit, The glycogen storage diseases and related
disorders, in: J.M. Saudubray, G. van den Berghe, J.H. Walter (Eds.), Inborn Meta-
bolic Diseases, 5th ed., Springer, 2012, pp. 115139.
[4] S. DiMauro, A.P. Hays, S. Tsujino, Metabolic disorders affecting muscle, in: A.G. Engel,
C. Franzini-Armstrong (Eds.), Myology, 3rd ed., McGraw-Hill, 2004, pp. 15351558.
[5] G.W. Padberg, A.R. Wintzen, M.A. Giesberts, P.J. Sterk, A.J. Molenaar, J. Hermans,
Effects of a high-protein diet in acid maltase deciency, J. Neurol. Sci. 90 (1989)
111117.
[6] O.A. Bodamer, D. Halliday, J.V. Leonard, The effects of l-alanine supplementation
in late-onset glycogen storage disease type II, Neurology 55 (2000) 710712.
[7] O.A. Bodamer, J.V. Leonard, D. Halliday, Dietary treatment in late-onset acid malt-
ase deciency, Eur. J. Pediatr. 156 (Suppl. 1) (1997) S39S42.
[8] A.E. Slonim, L. Bulone, T. Goldberg, J. Minikes, E. Slonim, J. Galanko, F. Martiniuk,
Modication of the natural history of adult-onset acid maltase deciency by nu-
trition and exercise therapy, Muscle Nerve 35 (2007) 7077.
[9] A.M. Umpleby, P.S. Trend, D. Chubb, J.V. Conaglen, C.D. Williams, R. Hesp, I.N.
Scobie, C.M. Wiles, G. Spencer, P.H. Sonksen, The effect of a high protein diet on
leucine and alanine turnover in acid maltase deciency, J. Neurol. Neurosurg. Psy-
chiatry 52 (1989) 954961.
[10] L.J. van Loon, P.L. Greenhaff, D. Constantin-Teodosiu, W.H. Saris, A.J. Wagenmakers,
The effects of increasing exercise intensity on muscle fuel utilisation in humans,
J. Physiol. 536 (2001) 295304.
[11] W.D. McArdle, F.I. Katch, V.L. Katch, Human energy expenditure during rest and
physical activity, in: W.D. McArdle, F.I. Katch, V.L. Katch (Eds.), Exercise Physiology:
Energy, Nutrition, and Human Performance, 6th ed., Lippincott Williams & Wilkins,
2007, pp. 195208.
[12] P.C. Calder, R. Geddes, Rat skeletal muscle lysosomes contain glycogen, Int. J.
Biochem. 21 (1989) 561567.
[13] O.B. Kotoulas, S.A. Kalamidas, D.J. Kondomerkos, Glycogen autophagy in glucose
homeostasis, Pathol. Res. Pract. 202 (2006) 631638.
[14] R.G. Haller, J. Vissing, Spontaneous second wind and glucose-induced second
second wind in McArdle disease: oxidative mechanisms, Arch. Neurol. 59
(2002) 13951402.
[15] N.A. Chamoles, G. Niizawa, M. Blanco, D. Gaggioli, C. Casentini, Glycogen storage
disease type II: enzymatic screening in dried blood spots on lter paper, Clin.
Chim. Acta 347 (2004) 97102.
[16] Z. Lukacs, C.P. Nieves, E. Mengel, R. Hartung, M. Beck, M. Deschauer, A. Keil, R. Santer,
Diagnostic efcacy of the uorometric determination of enzyme activity for Pompe
disease from dried blood specimens compared with lymphocytes-possibility for
newborn screening, J. Inherit. Metab. Dis. 33 (2010) 4350.
[17] J.R. Day, H.B. Rossiter, E.M. Coats, A. Skasick, B.J. Whipp, The maximally attainable
VO
2
during exercise in humans: the peak vs. maximum issue, J. Appl. Physiol. 95
(2003) 19011907.
[18] N.N. Abumrad, D. Rabin, M.P. Diamond, W.W. Lacy, Use of a heated supercial
hand vein as an alternative site for the measurement of amino acid concentra-
tions and for the study of glucose and alanine kinetics in man, Metabolism 30
(1981) 936940.
[19] G. Borg, Perceived exertion as an indicator of somatic stress, Scand. J. Rehabil.
Med. 2 (1970) 9298.
[20] R.R. Wolfe, D.L. Chinkes, Isotope Tracers in Metabolic Research, John Wiley &
Sons, Inc., Hoboken, New Jersey, 2005.
[21] J. Vissing, R.G. Haller, The effect of oral sucrose on exercise tolerance in patients
with McArdle's disease, N. Engl. J. Med. 349 (2003) 25032509.
[22] F. Peronnet, D. Massicotte, Table of nonprotein respiratory quotient: an update,
Can. J. Sport Sci. 16 (1991) 2329.
[23] R. Steele, Inuences of glucose loading and of injected insulin on hepatic glucose
output, Ann. N. Y. Acad. Sci. 82 (1959) 420430.
[24] S. Xu, M. Galperin, G. Melvin, R. Horowits, N. Raben, P. Plotz, L. Yu, Impaired orga-
nization and function of myolaments in single muscle bers from a mouse
model of Pompe disease, J. Appl. Physiol. 108 (2010) 13831388.
[25] R.P. Hesselink, M. Gorselink, G. Schaart, A.J. Wagenmakers, J. Kamphoven, A.J.
Reuser, G.J. van der Vusse, M.R. Drost, Impaired performance of skeletal muscle
in alpha-glucosidase knockout mice, Muscle Nerve 25 (2002) 873883.
[26] J.L. Grifn, Infantile acid maltase deciency. I. Muscle ber destruction after lyso-
somal rupture, Virchows Arch. B Cell Pathol. Incl. Mol. Pathol. 45 (1984) 2336.
[27] T. Fukuda, L. Ewan, M. Bauer, R.J. Mattaliano, K. Zaal, E. Ralston, P.H. Plotz, N.
Raben, Dysfunction of endocytic and autophagic pathways in a lysosomal storage
disease, Ann. Neurol. 59 (2006) 700708.
[28] S.F. Lewis, S. Vora, R.G. Haller, Abnormal oxidative metabolism and O
2
transport
in muscle phosphofructokinase deciency, J. Appl. Physiol. 70 (1991) 391398.
[29] R.G. Haller, J. Vissing, Functional evaluation of metabolic myopathies, in: A.G. Engel,
C. Franzini-Armstrong (Eds.), Myology, 3rd ed., McGraw-Hill, 2004, pp. 665679.
[30] P. Kazemi-Esfarjani, E. Skomorowska, T.D. Jensen, R.G. Haller, J. Vissing, A
nonischemic forearm exercise test for McArdle disease, Ann. Neurol. 52 (2002)
153159.
[31] I. Mineo, N. Kono, T. Shimizu, N. Hara, Y. Yamada, S. Sumi, K. Nonaka, S. Tarui, Ex-
cess purine degradation in exercising muscles of patients with glycogen storage
disease types V and VII, J. Clin. Invest. 76 (1985) 556560.
[32] H.R. Mundy, J.E. Williams, A.J. Cousins, P.J. Lee, The effect of L-alanine therapy in a
patient with adult onset glycogen storage disease type II, J. Inherit. Metab. Dis. 29
(2006) 226229.
467 N. Preisler et al. / Molecular Genetics and Metabolism 107 (2012) 462468
[33] M.C. Orngreen, T.D. Jeppesen, S.T. Andersen, T. Taivassalo, S. Hauerslev, N.
Preisler, R.G. Haller, H.G. van, J. Vissing, Fat metabolism during exercise in pa-
tients with McArdle disease, Neurology 72 (2009) 718724.
[34] G. Terzis, F. Dimopoulos, G.K. Papadimas, C. Papadopoulos, K. Spengos, I. Fatouros,
S.A. Kavouras, P. Manta, Effect of aerobic and resistance exercise training on
late-onset Pompe disease patients receiving enzyme replacement therapy, Mol.
Genet. Metab. 104 (2011) 279283.
[35] S.N. Blair, H.W. Kohl III, C.E. Barlow, R.S. Paffenbarger Jr., L.W. Gibbons, C.A.
Macera, Changes in physical tness and all-cause mortality. A prospective study
of healthy and unhealthy men, JAMA 273 (1995) 10931098.
468 N. Preisler et al. / Molecular Genetics and Metabolism 107 (2012) 462468
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Savage Gamma World (SWADE)Document61 pagesSavage Gamma World (SWADE)Bob Johnston100% (5)
- The Little Enema Book For Those On The Gerson Therapy PDFDocument18 pagesThe Little Enema Book For Those On The Gerson Therapy PDFLeonardo Velez De VillaNo ratings yet
- Unit 9 Genetic Engineering PowerpointDocument49 pagesUnit 9 Genetic Engineering Powerpointapi-235160519No ratings yet
- ImpDocument36 pagesImptejas100% (1)
- Basic Urban Design Principles PDFDocument73 pagesBasic Urban Design Principles PDFSumit yadav0% (1)
- Profile of MT MalindangDocument62 pagesProfile of MT MalindangDanz Alanna100% (1)
- NCP Anaphylactic ShockDocument6 pagesNCP Anaphylactic ShockKirstin del CarmenNo ratings yet
- 3rd Grade Desert Habitat LessonDocument5 pages3rd Grade Desert Habitat Lessonapi-283433684No ratings yet
- The Human Body As The PrimaryDocument51 pagesThe Human Body As The PrimaryCleiton XavierNo ratings yet
- Animal ClassificationDocument15 pagesAnimal Classificationchc5258No ratings yet
- DELSUDocument27 pagesDELSUSegunOladejoNo ratings yet
- MATH5PICSDocument4 pagesMATH5PICSLinden Dexter DaligconNo ratings yet
- Aktivasi Sel T LimfositDocument36 pagesAktivasi Sel T LimfositKatou Jeffrey ShigehitoNo ratings yet
- My Favorit Animal Is A ButterflyDocument2 pagesMy Favorit Animal Is A ButterflyAnnisa Luthfi ZakiyaNo ratings yet
- Bapp Babs Eleuthero 01172022 v1Document13 pagesBapp Babs Eleuthero 01172022 v1Donald R. NelsonNo ratings yet
- TimeTableJanJune2020 PDFDocument160 pagesTimeTableJanJune2020 PDFritik dwivediNo ratings yet
- Organic Chemistry Option II: Chemical BiologyDocument57 pagesOrganic Chemistry Option II: Chemical BiologyAhmad RizqiNo ratings yet
- Behind The Zhan Zhuang TrainingDocument13 pagesBehind The Zhan Zhuang TrainingLupe PalomeroNo ratings yet
- Scitech Final Exam ReviewerDocument2 pagesScitech Final Exam ReviewerhannieyuhNo ratings yet
- Handbook of Phytochemical Constituent GRAS Herbs and Other Economic Plants Herbal Reference Library Second Edition DukeDocument54 pagesHandbook of Phytochemical Constituent GRAS Herbs and Other Economic Plants Herbal Reference Library Second Edition Dukecatherine.fontenot978100% (10)
- Updated NCM 107 Lecture Week 7Document27 pagesUpdated NCM 107 Lecture Week 7Quencee CalaycayNo ratings yet
- BoichemistryDocument20 pagesBoichemistrynishwa RajpootNo ratings yet
- Isolation of Bacteria Into Pure Culture: Learning ObjectivesDocument6 pagesIsolation of Bacteria Into Pure Culture: Learning ObjectivesLiv LeysonNo ratings yet
- ch06 Ecology TestbankDocument6 pagesch06 Ecology Testbankhalabisarah100% (1)
- ScienceShore JanDocument93 pagesScienceShore JanZaara BarriosNo ratings yet
- Question Chapter 3 Nerve Fibers and Peripheral InnervationDocument20 pagesQuestion Chapter 3 Nerve Fibers and Peripheral InnervationTrang BuiNo ratings yet
- Hematology NotesDocument3 pagesHematology NotesFarisa Jane BanggoNo ratings yet
- Assure Lesson Plan MosaicDocument4 pagesAssure Lesson Plan Mosaicdaveeelya0% (1)
- PhysioEx Exercise 1 Activity 3Document3 pagesPhysioEx Exercise 1 Activity 3Paulina AguirreNo ratings yet
- Cell Cycle Formal ObservationDocument4 pagesCell Cycle Formal Observationapi-261437868No ratings yet