Professional Documents
Culture Documents
Angelman syndrome and Rett syndrome genetic link
Uploaded by
Akmal Nugraha0 ratings0% found this document useful (0 votes)
9 views6 pagesThis document describes a study that identified mutations in the MECP2 gene in some patients clinically diagnosed with Angelman syndrome (AS) but without the typical genetic abnormalities associated with AS. The study screened 47 such patients and found MECP2 mutations in 4 females and 1 male. These patients showed features overlapping with Rett syndrome, which is caused by MECP2 mutations. The findings suggest that a subset of individuals diagnosed with AS based on clinical features alone may actually have defects in the MECP2 gene normally associated with Rett syndrome.
Original Description:
akmal
Original Title
224.full
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document describes a study that identified mutations in the MECP2 gene in some patients clinically diagnosed with Angelman syndrome (AS) but without the typical genetic abnormalities associated with AS. The study screened 47 such patients and found MECP2 mutations in 4 females and 1 male. These patients showed features overlapping with Rett syndrome, which is caused by MECP2 mutations. The findings suggest that a subset of individuals diagnosed with AS based on clinical features alone may actually have defects in the MECP2 gene normally associated with Rett syndrome.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views6 pagesAngelman syndrome and Rett syndrome genetic link
Uploaded by
Akmal NugrahaThis document describes a study that identified mutations in the MECP2 gene in some patients clinically diagnosed with Angelman syndrome (AS) but without the typical genetic abnormalities associated with AS. The study screened 47 such patients and found MECP2 mutations in 4 females and 1 male. These patients showed features overlapping with Rett syndrome, which is caused by MECP2 mutations. The findings suggest that a subset of individuals diagnosed with AS based on clinical features alone may actually have defects in the MECP2 gene normally associated with Rett syndrome.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
Original articles
Angelman syndrome phenotype associated with
mutations in MECP2, a gene encoding a methyl
CpG binding protein
Pamela Watson, Graeme Black, Simon Ramsden, Margaret Barrow, Maurice Super,
Bronwyn Kerr, Jill Clayton-Smith
Abstract
Angelman syndrome (AS) is a neurode-
velopmental disorder characterised by
severe mental retardation, absent speech,
ataxia, sociable aVect, and dysmorphic
facial features. Eighty ve percent of
patients with AS have an identiable
genetic abnormality of chromosome
15q11-13. Mutations within the X linked
MECP2 gene have been identied in
patients with Rett syndrome (RTT), a
neurodevelopmental disorder which af-
fects females almost exclusively and which
shares phenotypic overlap with AS. RTT is
usually associated with normal develop-
ment in infancy followed by loss of
acquired skills and evolution of character-
istic hand wringing movements and epi-
sodes of hyperventilation.
A panel of 25 female and 22 male patients
with a clinical diagnosis of AS and no
molecular abnormality of 15q11-13 were
screened for MECP2 mutations and these
were identied in four females and one
male. Following the diagnosis, it was pos-
sible to elicit a history of regression in
three of these patients, who by then were
showing features suggestive of Rett syn-
drome. In the remaining two subjects the
clinical phenotype was still considered to
be Angelman-like.
These ndings illustrate the phenotypic
overlap between the two conditions and
suggest that screening for MECP2 muta-
tions should be considered in AS patients
without a demonstrable molecular or
cytogenetic abnormality of 15q11-13.
Since MECP2 mutations almost always
occur de novo, their identication will
substantially aVect genetic counselling for
the families concerned.
(J Med Genet 2001;38:224228)
Keywords: Angelman syndrome; Rett syndrome;
MECP2 mutations
Angelman syndrome (AS) is a neurodevelop-
mental disorder characterised by severe mental
retardation, inability to speak, ataxia, dysmor-
phic facial features, and a seizure disorder asso-
ciated with a characteristic EEG appearance.
1 2
AVected subjects have a specic behavioural
phenotype; they are happy and sociable with a
tendency to outbursts of laughter caused by
minimal provocation. The subtle dysmorphic
features associated with AS include deep set
eyes, wide, smiling mouth, and a prominent
chin. Head circumference is usually normal at
birth but head growth decelerates during the
early years of life and 30% of subjects become
microcephalic.
3 4
Most cases of AS are sporadic,
although many familial cases have been re-
ported. A variety of diVerent genetic mecha-
nisms involving chromosome 15q11-13, a
known imprinted region, have been described in
association with AS.
5
Approximately 70% of
patients have a de novo maternal deletion of
chromosome 15q11-13, while 3% have unipa-
rental paternal disomy for chromosome 15. In a
further 5% of cases there is biparental inherit-
ance of chromosome 15, but both chromosomes
have a paternal expression pattern owing to
defective imprinting of 15q11-13. Finally,
around 5% of patients have loss of function
mutations in the UBE3A gene, a gene encoding
E6-AP, a ubiquitin protein ligase. All result in a
deciency of the E6-AP protein, which is
involved in the process of ubiquitination.
6
There
remain a group of around 15% of AS patients,
both sporadic and familial, in whom no
cytogenetic or molecular abnormality involving
chromosome 15q11-13 can be identied. There
are few data documenting the clinical character-
istics of this group of patients.
7
Our own obser-
vations suggest that patients diagnosed with AS
on clinical grounds alone have greater motor
delay, are more likely to have some speech, and
are less likely to have seizures and the character-
istic Angelman syndrome EEG changes. While
this group may have mutations aVecting UBE3A
expression which cannot be dened, there
remains the possibility that AS is heterogeneous
with other, as yet unidentied causes.
Rett syndrome (RTT) is a disorder which is
seen almost exclusively in females.
8
Classically, it
is characterised by normal development for the
rst 12-18 months followed by developmental
regression and loss of acquired skills, especially
J Med Genet 2001;38:224228 224
Regional Genetic
Service, St Marys
Hospital, Hathersage
Road, Manchester
M13 OJH, UK
P Watson
G Black
S Ramsden
J Clayton-Smith
University
Department of
Ophthalmology,
Manchester Royal Eye
Hospital, Manchester
M13 9WH, UK
G Black
Clinical Genetics
Service, Leicester
Royal Inrmary,
Leicester LE1 5WW,
UK
M Barrow
Department of
Paediatric Genetics,
Royal Manchester
Childrens Hospital,
Pendlebury,
Manchester M27 4HA,
UK
M Super
B Kerr
Correspondence to:
Dr Clayton-Smith,
Jcs@central.cmht.nwest.nhs.uk
Revised version received
12 January 2001
Accepted for publication
13 January 2001
www.jmedgenet.com
group.bmj.com on June 16, 2012 - Published by jmg.bmj.com Downloaded from
purposeful hand movement. Many girls develop
characteristic hand washing or hand wring-
ing stereotypies and abnormal breathing pat-
terns with periods of hyperventilation and
apnoea. Subjects with RTT are frequently
growth retarded with acquired microcephaly
and small, cold feet. Following the period of
regression, skills plateau and then there is
usually gradual deterioration with increasing
neurological impairment over many years. The
broad clinical spectrum of Rett syndrome has
been described by Wan et al
9
and includes milder
formes frustes and a severe congenital
variant where there is no period of normal
development.
10
RTT is caused by mutations in
the X linked gene MECP2.
11
This encodes
methyl CpG binding protein 2, which binds to
single CpG dinucleotides throughout the ge-
nome and interacts with a histone deacetylase
complex to mediate transcriptional repression.
In the mouse, mecp2 is highly expressed in the
brain and appears to be of importance for
embryonic cellular diVerentiation.
12
AS and RTT show phenotypic overlap, as
was pointed out by ScheVer et al
13
in 1990.
Both are associated with severe mental retarda-
tion, acquired microcephaly, ataxia, seizures,
and stereotypic hand movements. The main
distinguishing feature is the clinical history as
AS patients do not have an initial normal
period of development or a distinct period of
regression. The typical early history of
regression is not present in every RTT patient
and it can be diYcult to elicit. We investigated
the possibility that AS with no detectable
abnormality of 15q11-13 may in fact result
from a defect of MECP2.
Patients and methods
DNA extracted from lymphocytes of 47
patients with a clinical diagnosis of Angelman
syndrome but no cytogenetic or molecular
abnormality of 15q11-13 was screened for
mutations within the MECP2 gene. All of these
patients fullled the consensus diagnostic
criteria for Angelman syndrome as laid down
by Williams et al.
14
One hundred ng DNA from
each patient was amplied using the primer
pairs published by Amir et al,
11
which span
three exons and cover the coding region of the
gene. Each sample was processed through 30
cycles of amplication consisting of one minute
at 94C (denaturation), one minute at 55C
(annealing), and one minute at 72C (exten-
sion). The nal extension step was 10 minutes.
SSCP/heteroduplex analysis was performed
using equal volumes of PCR product and
formamide loading dye. Gels were run at 350 V
overnight at 4Cand silver stained according to
standard protocols. They were inspected for
abnormally migrating bands which were then
sequenced directly using the ABI Prism Dye
Terminator Cycle Sequencing kit (Perkin
Elmer, Applied Biosciences Division, War-
rington, UK). Results were compared to the
reference sequence for MECP2 (Genebank
accession No X99686.) Mutations which
created or abolished restriction sites were con-
rmed by restriction enzyme analysis of
genomic DNA using appropriate enzymes.
Products of restriction digestion were fraction-
ated by electrophoresis and the products visu-
alised under UV transillumination after ethid-
ium bromide staining.
Results
Mutations within MECP2 were identied in
four of the 25 females and one of the 22 males
screened. The clinical details of these patients
are summarised in table 1 and details of the
mutations identied are given in table 2.
Patient 1 (g 1) was a girl. There had been
concern about her general development in the
rst year of life as she was a sleepy baby and
Table 1 Clinical features of patients with MECP2 mutations
Patient 1 Patient 2 Patient 3 Patient 4 Patient 5
Sex F F F F M
Age at suspected diagnosis of AS 3 y 3 y 2 y 12 mth 3 y
Age at MECP2 testing 7 y 11 y 9 y 7 y 7 y
Age at sitting 12 mth 7 mth 3 y Unable 12 mth
Age at walking Non-ambulant Non-ambulant Non-ambulant Non-ambulant 15 mth
Microcephaly + + + +
Brachycephaly + + + + +
Prominent chin + + + + +
Truncal hypotonia + + + + +
Limb spasticity + + +
Scoliosis + + + +
Seizures + +
Abnormal EEG + + +
Ataxia +/ + +/ +/ +
Tremor + ++ + +
Titubation + + +
Hand apping + +
Repetitive hand movements + + + + +
Hand wringing +/
Severe learning disability + + + + +
History of early regression + + +
Feeding problems + + +
Drooling + + +
Bruxism + + +
Absent speech + + + + +
Hyperventilation +/ +/
Sleep disorder
Short stature +
Small, cold feet + + +
Fair hair/blue eyes +
Hirsutism + +
Angelman syndrome and MECP2 mutations 225
www.jmedgenet.com
group.bmj.com on June 16, 2012 - Published by jmg.bmj.com Downloaded from
sitting was delayed until 12 months of age. She
had febrile seizures at 6 months and meningitis
was suspected. She developed ve words of
speech but lost these during the second year of
life. Her comprehension appeared to be better
than her expressive speech. She had a small
head circumference with a at occiput and a
prominent chin. She smiled frequently. She
had a resting tremor and jerky voluntary move-
ments but no hand wringing or hyperventila-
tion. Her legs were stiV with a talipes deform-
ity of one foot.
EEGshowed 2-3 Hz slowwave activity in the
temporal, central, and posterior regions and
some other non-specic features. A clinical
diagnosis of Angelman syndrome was made.
Analysis of the 15q11-13 region as described
above showed no abnormalities but analysis of
MECP2 showed a 44 base pair deletion within
exon 3 of the gene which was not present in
either parent.
Patient 2 presented to the paediatric neu-
rologist at the age of 3 years with severe devel-
opmental delay and ataxia. She had feeding
problems as an infant and had been investi-
gated for failure to thrive at 8 months. She sat
at 7 months and her parents considered that
her development had been normal up until that
time. She had never been able to crawl or walk.
She was noted to have a marked tremor with
evidence of titubation. She was microcephalic
with a at occiput and a prominent chin and
drooled frequently. She had never developed
speech or had seizures but a sleep EEG was
reported to be abnormal. A diagnosis of Angel-
man syndrome was suggested. By the age of 6
years, she had developed a scoliosis. She
continued to have tremulous movements but
she had no hand wringing stereotypies or
hyperventilation and had some purposeful
hand use. Molecular analysis of chromosome
15q11-13 was normal but analysis of MECP2
showed a C to G transition at nucleotide posi-
tion 376 causing a substitution of arginine for
proline at amino acid position 101, which lies
within the methyl binding domain of MECP2
and would therefore be likely to have an eVect
on protein function.
Patient 3 was rst seen at the age of 6 months
because of slow developmental progress; in par-
ticular she was not reaching out for toys. At that
time her head circumference was within the
normal range. When seen at the age of 3 years
she was noted to have frequent laughter with
hand apping and tongue thrusting behaviours
and occasional dgeting of her hands but no
hand wringing. Her parents had observed heavy
breathing on occasions. She was microcephalic
and had a at occiput and a prominent chin.
Progress with her motor development had been
slow. At 6 years she was sitting alone but not
mobile. There was no history of regression. She
had not had any seizures and an EEG was
reported as normal. CT scan showed a large cis-
terna magna with a small cerebellar vermis and
slightly large ventricles. A diagnosis of Angel-
man syndrome was suggested because of her
Table 2 MECP2 mutations identied in patients 15
Patient Exon Nucleotide change Mutation Mutation type Domain
1 3 44 base pair deletion 1230del44 Frameshift TRD
2 2 376 CG P101R Missense MBD
3 3 52 base pair deletion 1230del52 Frameshift TRD
4 3 497 CA Y141X Nonsense MBD
5 2 2 base pair deletion 241del2 Frameshift MBD
MBD: methyl-cytosine binding domain (85 amino acids).
TRD: transcriptional repression domain (104 amino acids).
Figure 1 (A) Patient 1 at the age of 4 years and (B) at the age of 6 years.
226 Watson, Black, Ramsden, et al
www.jmedgenet.com
group.bmj.com on June 16, 2012 - Published by jmg.bmj.com Downloaded from
happy aVect, stereotypic hand movements, and
facial features. The possibilities of Joubert
syndrome and of chromosomal mosaicism were
also considered. Analysis of 15q11-13 was
normal, but she was found to have a 52 base pair
deletion within exon 3 of MECP2.
Patient 4 was noted to have developmental
delay by the health visitor at the age of 7 months.
She was a oppy baby who was unable to sit
without support. Records showed that early in
life she was able to nger feed and transfer
objects from hand to hand. Over the next three
years, she had a decelerating head circumference
and was noted to be brachycephalic, with facial
features and a sociable disposition which were
suggestive of Angelman syndrome. There was
no denite history of developmental regression.
On review at 6 years of age, AS was thought to
be the most likely diagnosis, although she had a
normal EEG and no abnormality had been
detected within the 15q11-13 region. Analysis of
MECP2 showed a C to G transition at position
497 leading to premature termination of the
protein at amino acid position 141. This same
mutation has been reported previously in girls
with Rett syndrome.
11
Patient 5 was a boy who had been oppy as
an infant and then presented with delay in
motor development during the second year of
life. He walked at 15 months of age but needed
a lot of support and had an unusual, wide
based, stiV legged gait with marked ataxia (g
2). In addition he had a seizure disorder and an
abnormal EEG which showed an excess of
slow wave activity. His head circumference lay
between the 10th and 25th centiles but head
growth had decelerated and he was brachy-
cephalic. He drooled frequently and had some
repetitive midline hand movements but no
obvious hand wringing. Titubation and tremor
were noted. He had reduced muscle bulk in his
limbs and poor peripheral circulation with
cold, blue feet. At the age of 6, he began to
develop a scoliosis. The diagnosis of Angelman
syndrome was made based on his facial
appearance, ataxic gait, happy disposition, and
seizure disorder. No abnormality of chromo-
some 15q11-13 was identied, but analysis of
MECP2 showed that he had a 2 base pair dele-
tion at positions 241-242 within exon 2, result-
ing in a frameshift with premature termination
of the MeCP2 protein. The presence of a nor-
mal band on the SSCP gel suggested the possi-
bility of somatic mosaicism. Further details of
this analysis have been documented else-
where.
15
Parental analyses were normal.
Discussion
We have identied MECP2 mutations in 4/25
girls and 1/22 boys who presented initially with
a clinical diagnosis of AS. None of the subjects
concerned had a demonstrable genetic abnor-
mality of 15q11-13. The diagnosis of RTT had
been considered in cases 2 and 3, as part of the
diVerential diagnosis of AS, but RTT was not
the working diagnosis in either case at the time
of testing. On review of the clinical features of
these ve patients after identifying MECP2
mutations, four of the ve had some of the
classical phenotypic features of Rett syndrome
which had evolved over time. These were not
always typical, however, and in particular the
characteristic hand washing stereotypies and
hyperventilation were not prominent features.
All of the ve patients had the four clinical
characteristics designated consistent
(present in 100%) in the diagnostic criteria for
AS laid down by Williams et al
14
in 1995. These
are severe developmental delay, no or minimal
use of words, movement or balance disorder,
and behavioural uniqueness. In addition, all
had some of the other criteria described by
Williams et al
14
as being frequent or associ-
ated in AS and the clinical signs had been so
convincing that it had been considered reason-
able to pursue UBE3A mutation screening in
each case after methylation analysis of chromo-
some 15 had proven normal.
It is well recognised that AS and RTT have
overlapping clinical features and ScheVer et al
13
drew attention to these clinical similarities and
cautioned against making the diagnosis of AS
in a girl at an early age, especially in the
absence of the typical EEGappearance. Laan et
al
16
studied the EEGs of patients with Angel-
man syndrome and Rett syndrome at a young
age. They suggested that whereas the EEG
changes in AS are pathognomonic of this con-
dition, those seen in Rett syndrome are more
non-specic and the EEG can often be normal
in the rst few years of life. Two of our ve
patients had seizures and although three had an
abnormal EEG, none had the EEG features
Figure 2 Patient 5 at the age of 4 years. Note stiV legged
posture and small, discoloured feet.
Angelman syndrome and MECP2 mutations 227
www.jmedgenet.com
group.bmj.com on June 16, 2012 - Published by jmg.bmj.com Downloaded from
typically associated with AS. This supports the
suggestion that the EEG is a good distinguish-
ing feature. All of our patients had facial
features consistent with AS and had a happy,
sociable aVect. Episodic laughter, often noctur-
nal, has been reported as a feature of Rett syn-
drome
8
and these were frequent in the subjects
we have reported. An important diagnostic
feature in both AS and RTT is the presence of
a movement disorder. AS is characterised by
ne, tremulous movements in infancy, which
evolve into coarser, ataxic voluntary move-
ments during childhood. Hand apping and
mouthing of the hands and other objects are
also common. In contrast to Rett syndrome,
purposeful hand use is not well developed at
any stage in AS. A typical child with Rett syn-
drome will initially develop purposeful hand
use and will then lose this during the period of
regression. From that time on, repetitive hand
stereotypies such as patting, plucking clothing,
tapping, hand biting, and hand wringing begin
to appear, but these may be slow to evolve. In
those patients where the period of regression
occurs early, purposeful hand use may never
develop, and in this group especially the move-
ment disorder may be suggestive of AS in the
early stages. Looking at our ve patients retro-
spectively, prominent characteristics of the
movement disorder which were distinguishable
from that of AS were the presence of titubation
and marked tremor.
A further observation in those of the ve who
were ambulant was a habit of rocking slowly and
rhythmically from foot to foot. Facial features
were very similar to those seen in classical AS.
Three of our patients had remarkably cold, blue
feet which are not a common feature of AS.
Within any condition diagnosed on clinical
grounds, there remains an argument as to its
exact boundaries. In view of the broad clinical
variability in Rett syndrome, Hagberg
10
sug-
gested diagnostic criteria for Rett syndrome
variants to be used in girls of 10 years or over.
It is in the early years, however, that parents
usually seek a diagnosis and genetic advice
before planning further children. It is during
this period that there is most phenotypic over-
lap between the features of AS and RTT. In a
situation where AS is diagnosed on clinical
grounds alone, parents would be counselled
that recurrence risks could be as high as 50%
and that no specic prenatal test would be
available. If it could be shown that the child had
a MECP2 mutation, the recurrence risk would
be much lower in the majority of cases since
most arise de novo. Clearly it is possible to
argue that the patients described should not
now be considered to have Angelman syn-
drome. The observations nevertheless serve to
illustrate the potential clinical value of consid-
ering MECP2 screening in the young AS
patient with no 15q11-13 abnormalities, even
if the patient is a male.
The phenotypic overlap between the clinical
course of AS and RTT raises the question as to
whether the two conditions may be aetiologi-
cally related through a common pathogenesis.
MeCP2 is involved in transcriptional silenc-
ing.
17
It binds to single CpG dinucleotides
throughout the genome and with the corepres-
sor Sin3A, which binds to its transcriptional
repression domain, it recruits histone deacety-
lases. These then act to alter chromatin
conguration to prevent transcription. It has
been postulated that in the presence of a
MECP2 mutation, there may be overexpression
of downstream genes, although a study by
Xiang et al
18
did not show an increase in levels
of certain neurotransmitters within the brains
of subjects with MeCP2 mutations, which
would have supported this hypothesis. Overex-
pression of genes within the 15q11-13 region
does give rise to a specic phenotype. Several
subjects with a maternal duplication of this
region have had autistic features, ataxia,
epilepsy, learning diYculties, and subtle dys-
morphic facial features.
19 20
One hypothesis,
therefore, is that UBE3A is one of the target
genes downstream of MECP2 for which altera-
tion of expression is particularly critical.
Further investigation of this hypothesis will
involve the study of those areas of the brain
where UBE3A is known to be expressed.
GB is a Clinician Scientist Fellowfunded by the Wellcome Trust
(reference 51390/Z). PW is funded by a grant from the Birth
Defects Foundation.
1 Angelman H. Puppet children. Dev Med Child Neurol
1965;7:681-8.
2 Boyd SG, Harden A, Patton MA. The EEG in early diagno-
sis of the Angelman (happy puppet) syndrome. Eur J Pedi-
atr 1988;147:508-13.
3 Clayton-Smith J. Clinical research on Angelman syndrome
in the UK: observations on 82 aVected individuals. Am J
Med Genet 1993;46:12-15.
4 Williams CA, Zori RT, Hendrickson J, Stalker H, Marum T,
Whidden E, Driscoll DJ. Angelman syndrome. Curr Probl
Pediatr 1995;25:216-31.
5 Jiang Y, Lev-Lehman E, Bressler J, Ting-Fen T, Beaudet
AL. Genetics of Angelman syndrome. Am J Hum Genet
1999;65:1-6.
6 Kishino T, Lalande M, WagstaV J. UBE3A/E6-AP muta-
tions cause Angelman syndrome. Nat Genet 1997;15:70-3.
7 Laan LAEM, Halley DJJ, den Boer AT, Hennekam RCM,
Renier WO, Brouwer OF. Angelman syndrome without
detectable chromosome 15q11-13 anomaly: clinical study
of familial and isolated cases. Am J Med Genet 1998;76:
262-8.
8 Clarke A. Rett syndrome. J Med Genet 1996;33:695-9.
9 Wan M, Sung Jae Lee S, Zhang X, et al. Rett syndrome and
beyond: recurrent spontaneous and familial MECP2
mutations at CpG hotspots. Am J Hum Genet 1999;65:
1520-9.
10 Hagberg B. Clinical delineation of Rett syndrome variants.
Neuropediatrics 1995;26:62.
11 Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U,
Zoghbi H. Rett syndrome is caused by mutations in
X-linked MECP2, encoding methyl-CpG- binding protein
2. Nat Genet 1999;12:205-8.
12 Tate P, Skarnes W, Bird A. The methyl-CpG binding
protein Mecp2 is essential for embryonic development in
the mouse. Nat Genet 1996;12:205-8.
13 ScheVer I, Brett EM, Wilson J, Baraitser M. Angelmans
syndrome. J Med Genet 1990;27:275-8.
14 Williams CA, Angelman H, Clayton-Smith J, et al.
Angelman syndrome: consensus for diagnostic criteria. Am
J Med Genet 1995;56:237-8.
15 Clayton-Smith J, Watson P, Ramsden S, Black GCM.
Somatic mutation in MECP2 as a cause of non-fatal
neurodevelopmental disorder in males. Lancet 2000;356:
830-2.
16 Laan LAEM, Brouwer OE, Begeer CH, Zwinderman AH,
van Dijk JG. The diagnostic value of the EEG in Angelman
syndrome and Rett syndrome at a young age. Electroen-
cephalogr Clin Neurophysiol 1998;106:404-8.
17 Nan X, Ng HH, Johnson CA, et al. Transcriptional
repression by the methyl-CpG- binding protein MeCP2
involves a histone deacetylase complex. Nature 1998;393:
386-9.
18 Xiang F, Buervenich S, Nicolao P, Bailey ME, Zhang Z,
Anvret M. Mutation screening in Rett syndrome. J Med
Genet 2000;37:250-5.
19 Browne CE, Dennis NR, Maher E, Long SL, Nicholson J,
Sillbourne J, Barber JCK. Inherited interstitial duplications
of proximal 15q: genotype-phenotype correlations. Am J
Hum Genet 1997;61:1342-52.
20 Webb T. Inv dup(15)supernumerary marker chromosomes.
J Med Genet 1994;31:585-94.
228 Watson, Black, Ramsden, et al
www.jmedgenet.com
group.bmj.com on June 16, 2012 - Published by jmg.bmj.com Downloaded from
doi: 10.1136/jmg.38.4.224
2001 38: 224-228 J Med Genet
Pamela Watson, Graeme Black, Simon Ramsden, et al.
methyl CpG binding protein
, a gene encoding a MECP2 with mutations in
Angelman syndrome phenotype associated
http://jmg.bmj.com/content/38/4/224.full.html
Updated information and services can be found at:
These include:
References
http://jmg.bmj.com/content/38/4/224.full.html#related-urls
Article cited in:
http://jmg.bmj.com/content/38/4/224.full.html#ref-list-1
This article cites 19 articles, 2 of which can be accessed free at:
service
Email alerting
box at the top right corner of the online article.
Receive free email alerts when new articles cite this article. Sign up in the
Collections
Topic
(530 articles) Epidemiology
(314 articles) Clinical diagnostic tests
(46 articles) Movement disorders (other than Parkinsons)
Articles on similar topics can be found in the following collections
Notes
http://group.bmj.com/group/rights-licensing/permissions
To request permissions go to:
http://journals.bmj.com/cgi/reprintform
To order reprints go to:
http://group.bmj.com/subscribe/
To subscribe to BMJ go to:
group.bmj.com on June 16, 2012 - Published by jmg.bmj.com Downloaded from
You might also like
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- Marinesco-Sjo Gren Syndrome - 2013Document5 pagesMarinesco-Sjo Gren Syndrome - 2013Irfan RazaNo ratings yet
- Epilepsia EpicongressDocument245 pagesEpilepsia EpicongressВасилий КоптеловNo ratings yet
- Morphometry of WS On ASDocument6 pagesMorphometry of WS On ASAdrien DuthéNo ratings yet
- Novel p53 Splicing Site Mutation in Li-Fraumeni-like Syndrome With OsteosarcomaDocument5 pagesNovel p53 Splicing Site Mutation in Li-Fraumeni-like Syndrome With OsteosarcomaMissy MishaNo ratings yet
- (1479683X - European Journal of Endocrinology) Parental Genomic Imprinting in EndocrinopathiesDocument9 pages(1479683X - European Journal of Endocrinology) Parental Genomic Imprinting in EndocrinopathiesRavia SharmaNo ratings yet
- 23 - 224Praktis-Strategi Terapi Cairan Pada DehidrasiDocument8 pages23 - 224Praktis-Strategi Terapi Cairan Pada DehidrasiRahmat AbbasNo ratings yet
- Batten Disease: Features To Facilitate Early Diagnosis: Scientific ReportDocument6 pagesBatten Disease: Features To Facilitate Early Diagnosis: Scientific ReportMaferNo ratings yet
- Biopolym - Cell 2018 34 5 361 enDocument6 pagesBiopolym - Cell 2018 34 5 361 enАнна ШаповаловаNo ratings yet
- Biopolym - Cell 2018 34 5 361 enDocument6 pagesBiopolym - Cell 2018 34 5 361 enАнна ШаповаловаNo ratings yet
- Methylation, Cytogenetic and Fish Tests in The Molecular Diagnosis of Prader-Willi and Angelman SyndromesDocument12 pagesMethylation, Cytogenetic and Fish Tests in The Molecular Diagnosis of Prader-Willi and Angelman SyndromesNayara MacedoNo ratings yet
- 10 1038@nature07261Document7 pages10 1038@nature07261ANo ratings yet
- Fragile X Syndrome Due to a Rare Missense MutationDocument5 pagesFragile X Syndrome Due to a Rare Missense MutationhanzelNo ratings yet
- Fragile X Syndrome (Martin-Bell Syndrome)Document6 pagesFragile X Syndrome (Martin-Bell Syndrome)yudhi kurniawanNo ratings yet
- Gim 200269 ADocument5 pagesGim 200269 AfakeempireNo ratings yet
- Genodermatosis MCQsDocument152 pagesGenodermatosis MCQsDr.Tawheed88% (8)
- AngelmanDocument12 pagesAngelmanapi-295680726No ratings yet
- Full TextDocument4 pagesFull TextladybieibiNo ratings yet
- (03241750 - Acta Medica Bulgarica) Molecular-Genetic Diagnostics of Angelman Syndrome - The Bulgarian ExperienceDocument8 pages(03241750 - Acta Medica Bulgarica) Molecular-Genetic Diagnostics of Angelman Syndrome - The Bulgarian ExperienceTeodorNo ratings yet
- Recurrent 7q11.23 Deletions Identified in Patients with Neurodevelopmental DisordersDocument9 pagesRecurrent 7q11.23 Deletions Identified in Patients with Neurodevelopmental DisordersEAPNo ratings yet
- Clinical Features and Gene Mutational Spectrum of CDKL5-related Diseases in A Cohort of Chinese PatientsDocument7 pagesClinical Features and Gene Mutational Spectrum of CDKL5-related Diseases in A Cohort of Chinese PatientsGaly Crt FlzNo ratings yet
- A TESIS GalvanDocument28 pagesA TESIS GalvanSaul PsiqNo ratings yet
- 439 2007 Article 362Document6 pages439 2007 Article 362Zinik EşanuNo ratings yet
- MLPA Dummy ReportDocument3 pagesMLPA Dummy ReportAakash verma100% (1)
- 2.3kb FOXG1 gene deletion detected by array CGHDocument1 page2.3kb FOXG1 gene deletion detected by array CGHdvNo ratings yet
- Journal of Child Neurology 2Document7 pagesJournal of Child Neurology 2NEUROLAB ESCALÓNNo ratings yet
- Patogenesis IMNDocument23 pagesPatogenesis IMNshiloinNo ratings yet
- Menkes Kinky Hair Disease (Menkes Syndrome) - A Case ReportDocument5 pagesMenkes Kinky Hair Disease (Menkes Syndrome) - A Case ReportTannov SiregarNo ratings yet
- ng00229 PDFDocument3 pagesng00229 PDFPaijo SusenoNo ratings yet
- Role For Hedgehog Signaling in Cranial-Suture Development and ObesityDocument9 pagesRole For Hedgehog Signaling in Cranial-Suture Development and ObesityDanny Alvarez FocacciNo ratings yet
- Prion (CJD), Lahiru Perera, 23416785Document6 pagesPrion (CJD), Lahiru Perera, 23416785Lahiru PereraNo ratings yet
- McKinnis Bone Marrow Transplantation Hunter Syndrome The Journal of PediatricsDocument17 pagesMcKinnis Bone Marrow Transplantation Hunter Syndrome The Journal of PediatricsBoNo ratings yet
- 2008 Elsea EurJHumGenetDocument10 pages2008 Elsea EurJHumGenetEAPNo ratings yet
- NPM1 Gene Deletions in MDS Patients with 5q- Deletion and Complex KaryotypeDocument2 pagesNPM1 Gene Deletions in MDS Patients with 5q- Deletion and Complex KaryotypeglodovichiNo ratings yet
- 61-1-13sd RettDocument11 pages61-1-13sd RettCarolina GuzmánNo ratings yet
- A Novel RLIM/RNF12 Variant Disrupts Protein Stability and Function To Cause Severe Tonne-Kalscheuer SyndromeDocument9 pagesA Novel RLIM/RNF12 Variant Disrupts Protein Stability and Function To Cause Severe Tonne-Kalscheuer SyndromeMohamad SoveyziNo ratings yet
- De Novo Mutations in YWHAG Cause Early Onset EpilepsyDocument11 pagesDe Novo Mutations in YWHAG Cause Early Onset EpilepsyGiselle Costa Daniel HonoratoNo ratings yet
- EJE-Cuny2013Document9 pagesEJE-Cuny2013W Antonio Muñoz ChNo ratings yet
- Nascimento Et Al. - 2012 - Adrenoleukodystrophy A Forgotten Diagnosis in Children With Primary Addison' S DiseaseDocument5 pagesNascimento Et Al. - 2012 - Adrenoleukodystrophy A Forgotten Diagnosis in Children With Primary Addison' S DiseaseflashjetNo ratings yet
- CHAP NO4 Results (Abbas) Rewritten FileDocument12 pagesCHAP NO4 Results (Abbas) Rewritten FileRahid KhanNo ratings yet
- Spinal Muscular Atrophy 2023Document21 pagesSpinal Muscular Atrophy 2023Arbey Aponte PuertoNo ratings yet
- Mutations in Mitochondr Ial GenesDocument6 pagesMutations in Mitochondr Ial Geneslynden matbaganNo ratings yet
- FRAGILE X SYNDROME: CLINICAL FEATURES AND MOLECULAR BASISDocument65 pagesFRAGILE X SYNDROME: CLINICAL FEATURES AND MOLECULAR BASISFlory ZapantaNo ratings yet
- La Epigenética y Los Estudios en Gemelos en El Campo de La PsiquiatríaDocument9 pagesLa Epigenética y Los Estudios en Gemelos en El Campo de La PsiquiatríaHerb MedrNo ratings yet
- Pyruvate Kinase Deficiency and Malaria: Brief ReportDocument6 pagesPyruvate Kinase Deficiency and Malaria: Brief ReportErlangga Perwira NegaraNo ratings yet
- AP1S2 Is Mutated in Xlinked DandyWalker Malformation With Intellectual Disability Basal Ganglia Disease and Seizures Pettigrew Syndrome - 2014Document6 pagesAP1S2 Is Mutated in Xlinked DandyWalker Malformation With Intellectual Disability Basal Ganglia Disease and Seizures Pettigrew Syndrome - 2014Jose Rafael Villafan BernalNo ratings yet
- Book JewsDocument230 pagesBook JewsFred Duarte CaldeiraNo ratings yet
- Reyes - Unit 2 (Part 2)Document4 pagesReyes - Unit 2 (Part 2)Justine Ericca ReyesNo ratings yet
- Genotype-Phenotype Studies in Three Families PQBP1Document9 pagesGenotype-Phenotype Studies in Three Families PQBP1Mosabbira RahmanNo ratings yet
- Genetic Mutations BTCIDocument59 pagesGenetic Mutations BTCIDharti Adhia100% (1)
- Ocular Features of Marfan Syndrome: Gordana Stanković-Babić, Milena Vujanović, Jasmina Đorđević-Jocić, Sonja CekićDocument4 pagesOcular Features of Marfan Syndrome: Gordana Stanković-Babić, Milena Vujanović, Jasmina Đorđević-Jocić, Sonja CekićmongiiiNo ratings yet
- Progressive Increase of The Mutated Mitochondria1 DNA Fraction in Kearns-Sayre SyndromeDocument6 pagesProgressive Increase of The Mutated Mitochondria1 DNA Fraction in Kearns-Sayre SyndromeGréta BotyánszkiNo ratings yet
- 05 Molecular Genetics of The EpilepsiesDocument15 pages05 Molecular Genetics of The EpilepsiesvenkatesannagarajanNo ratings yet
- Microscopy Res Technique - 2001 - Southwood - Molecular pathways of oligodendrocyte apoptosis revealed by mutations inDocument9 pagesMicroscopy Res Technique - 2001 - Southwood - Molecular pathways of oligodendrocyte apoptosis revealed by mutations inAnglia LopesNo ratings yet
- Detect 80% of AS Cases with Methylation AnalysisDocument5 pagesDetect 80% of AS Cases with Methylation AnalysisBeatriz AzevedoNo ratings yet
- 2008 - MarshallDocument12 pages2008 - MarshallCarlosNo ratings yet
- Genetic and Neurodevelopmental Spectrum of SYNGAP1-associated Intellectual Disability and EpilepsyDocument12 pagesGenetic and Neurodevelopmental Spectrum of SYNGAP1-associated Intellectual Disability and EpilepsySaya OtonashiNo ratings yet
- Winawer Et Al-2018-Annals of NeurologyDocument14 pagesWinawer Et Al-2018-Annals of NeurologyAndoingNo ratings yet
- Neuroendocrine Tumors: Surgical Evaluation and ManagementFrom EverandNeuroendocrine Tumors: Surgical Evaluation and ManagementJordan M. CloydNo ratings yet
- ContentServer AspDocument12 pagesContentServer AspAkmal NugrahaNo ratings yet
- ContentServer AspDocument12 pagesContentServer AspAkmal NugrahaNo ratings yet
- Idr 7 323Document7 pagesIdr 7 323Akmal NugrahaNo ratings yet
- Idr 7 323Document7 pagesIdr 7 323Akmal NugrahaNo ratings yet
- ContentServer AspDocument12 pagesContentServer AspAkmal NugrahaNo ratings yet
- Idr 7 323Document7 pagesIdr 7 323Akmal NugrahaNo ratings yet
- RefraksiDocument53 pagesRefraksigilaliNo ratings yet
- RefraksiDocument53 pagesRefraksigilaliNo ratings yet
- CERAMAHDocument2 pagesCERAMAHAkmal NugrahaNo ratings yet
- 02 - Physical ExaminationDocument69 pages02 - Physical Examinationkrizia_arifinNo ratings yet
- CERAMAHDocument2 pagesCERAMAHAkmal NugrahaNo ratings yet
- CERAMAHDocument2 pagesCERAMAHAkmal NugrahaNo ratings yet
- Chromatin RemodellingDocument234 pagesChromatin Remodellingplastioid4079No ratings yet
- Aberrant Astrocyte Protein Secretion Contributes To Altered Neuronal Development in Multiple Models of Neurodevelopmental DisordersDocument36 pagesAberrant Astrocyte Protein Secretion Contributes To Altered Neuronal Development in Multiple Models of Neurodevelopmental DisordersLeon PalomeraNo ratings yet
- Combinepdf 7Document129 pagesCombinepdf 7Joe JosephNo ratings yet
- HMB200 Lecture 10 ASD Genetics 2020-21Document56 pagesHMB200 Lecture 10 ASD Genetics 2020-21bluetooth opencvNo ratings yet
- Evaluation of the Child with Global Developmental Delay: Diagnostic Yield of Metabolic and Genetic InvestigationsDocument61 pagesEvaluation of the Child with Global Developmental Delay: Diagnostic Yield of Metabolic and Genetic InvestigationsAnsilNo ratings yet
- FDAapproves Daybuethefirsttreatmentfor RettsyndromeDocument8 pagesFDAapproves Daybuethefirsttreatmentfor RettsyndromeNeethu Anna StephenNo ratings yet
- Rett Syndrome A Neurological Disorder With MetabolDocument17 pagesRett Syndrome A Neurological Disorder With MetabolTiara PuspaNo ratings yet
- Avexis Investor PresentationDocument20 pagesAvexis Investor PresentationmedtechyNo ratings yet
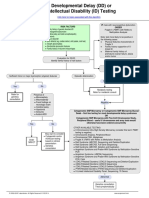
- Developmental Delay (DD) or Intellectual Disability (ID) Testing AlgorithmDocument1 pageDevelopmental Delay (DD) or Intellectual Disability (ID) Testing AlgorithmNeo Mervyn Monaheng100% (1)
- Autism Spectrum DisordersDocument9 pagesAutism Spectrum DisordersClaudia Verónica Revilla PazNo ratings yet
- Prenatal ScreningDocument44 pagesPrenatal ScreningHoopmen tampubolonNo ratings yet
- Science:, 792 (2003) Robin D. Rogers and Kenneth R. SeddonDocument3 pagesScience:, 792 (2003) Robin D. Rogers and Kenneth R. SeddonJohnSmithNo ratings yet
- Rett SyndromeDocument13 pagesRett SyndromeAileish Kate Lanuevo JaudianNo ratings yet
- Thesis TitlesDocument25 pagesThesis TitlesMicah Dianne DizonNo ratings yet
- Rett Syndrome 1Document19 pagesRett Syndrome 1api-545157726No ratings yet
- PHD Credit Seminar 2 Punjab Agricultural University, LudhianaDocument141 pagesPHD Credit Seminar 2 Punjab Agricultural University, LudhianaSUSHANT DHARNo ratings yet
- What Is Rett Syndrome?Document4 pagesWhat Is Rett Syndrome?Jon_NamikazeNo ratings yet
- Rett SyndromeDocument55 pagesRett SyndromeSnezana MihajlovicNo ratings yet
- Intellectual Disability in Children - Evaluation For A Cause - UpToDateDocument30 pagesIntellectual Disability in Children - Evaluation For A Cause - UpToDatecapt_zoe100% (1)
- THE Ironies of Human Mind: A Case of Rett SyndromeDocument5 pagesTHE Ironies of Human Mind: A Case of Rett Syndromeaprillia kusuma putriNo ratings yet
- Athens 2010 IALP - PROCEEDINGS PDFDocument882 pagesAthens 2010 IALP - PROCEEDINGS PDFYelly Andriani Barlian100% (1)
- Neural and Synaptic Defects in Autism SPDocument287 pagesNeural and Synaptic Defects in Autism SPGabriel NeiraNo ratings yet
- The Role of Neuroglia in AutismDocument30 pagesThe Role of Neuroglia in AutismWesley M.SantosNo ratings yet
- Autism A Neuroepigenetic DisorderDocument13 pagesAutism A Neuroepigenetic DisorderMelania TonelloNo ratings yet
- Antipurinergic Therapy For Autism-An In-Depth Review.Document15 pagesAntipurinergic Therapy For Autism-An In-Depth Review.Miguel Romero100% (1)
- Abstracts From ESMED Congress 2021Document197 pagesAbstracts From ESMED Congress 2021European Society of Medicine (ESMED)100% (2)
- Pediatric Neurology - Lawson Peter N. (SRG)Document200 pagesPediatric Neurology - Lawson Peter N. (SRG)Hriday DeNo ratings yet
- Genetic Causes of Syndromic and Non-Syndromic Autism PDFDocument9 pagesGenetic Causes of Syndromic and Non-Syndromic Autism PDFRaisa CoppolaNo ratings yet
- Retraso Global Del DesarrolloDocument18 pagesRetraso Global Del Desarrolloenypaola19No ratings yet
- GABAA receptor downregulation in autism brain regionsDocument7 pagesGABAA receptor downregulation in autism brain regionsaini qurrotullainNo ratings yet