Professional Documents
Culture Documents
Lister Ios Is
Uploaded by
Fede0Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lister Ios Is
Uploaded by
Fede0Copyright:
Available Formats
Listeriosis
Klara M. Posfay-Barbe
a,
*
, Ellen R. Wald
b
a
Department of Pediatrics, Childrens Hospital of Geneva, University Hospitals of Geneva, 6 rue Willy-Donze, 1211 Geneva 14, Switzerland
b
Department of Pediatrics, University of WisconsinMadison, School of Medicine and Public Health, 600 Highland Avenue, Box 4108, Madison, WI 53792, USA
Keywords:
Early-onset sepsis
Late-onset sepsis
Listeriosis
Neonates
Perinatal infection
s u m m a r y
Listeria monocytogenes, a small, facultative anaerobic, Gram-positive motile bacillus, is an important
cause of foodborne illness which disproportionately affects pregnant women and their newborns. Lis-
teria infects many types of animals and contaminates numerous foods including vegetables, milk,
chicken and beef. This organism has a unique proclivity to infect the fetoplacental unit with the ability to
invade cells, multiply intracellularly and be transmitted cell-to-cell. The organism possesses several
virulence factors, including internalin A and internalin B, which facilitate the direct invasion of cells. Cell-
to-cell transmission is promoted by the bacterial surface protein ActA which is regulated by a tran-
scriptional activator known as positive regulatory factor A. Both innate and adaptive immune responses
enable the host to eliminate this pathogen. Clinical manifestations of infection in the newborn fall into
the traditional categories of early- and late-onset sepsis. Therapeutic recommendations include ampi-
cillin and gentamicin for 1421 days.
2009 Elsevier Ltd. All rights reserved.
1. Microbiology
Listeria monocytogenes is a small, facultatively anaerobic, Gram-
positive, motile bacillus. It grows well in broth and on blood agar;
some species produce a narrow zone of beta-hemolysis.
1
In clinical
specimens, the organism may be Gram-variable and look like cocci,
diplococci, or diphtheroids, thereby misleading the laboratory
technician. The organism tolerates low temperatures as well as
high pH and high salt concentrations, which allow it to replicate in
soil, water, sewage, manure, animal feed, and contaminated
refrigerated foods. It can survive many months in soil and 2030
days in tap water. Although persisting on environmental surfaces,
pasteurization and most disinfecting agents eliminate Listeria.
Only four of the seven species of Listeria infect humans. Most
diseases are due to three primary serotypes: 1a, 1b and 4b. The last
is responsible for almost all outbreaks of listeriosis.
2
2. Epidemiology
Listeria spp. are distributed worldwide, but human illness is
reported most frequently in developed countries. Listeria spp. are
an important cause of zoonoses, infecting many types of animals
(domestic pets, livestock, other mammals, rodents, amphibians,
sh, and arthropods) and more than 17 avian species. In
mammals, L. monocytogenes can cause spontaneous abortions and
is the cause of circling disease, a manifestation of basilar
meningitis in which animals move incessantly in a circle. Fecal
oral transmission is the probable means by which organisms are
spread in animals. The pathogen can be transmitted directly from
animals to humans and has been documented in veterinarians,
farmers, and abattoir workers. Vertical transmission from mother
to neonate occurs transplacentally or through an infected birth
canal. Cross-infection in a neonatal unit through contact with
contaminated mineral oil used to bathe infants led to one noso-
comial outbreak.
3
Most cases of listeriosis appear to be foodborne, including those
acquired during pregnancy. Many foods can be contaminated by L.
monocytogenes, including raw vegetables, raw milk, sh, poultry,
processed chicken, and beef. Approximately 1570% of hot dogs are
reported to be contaminated with Listeria spp. Listeria spp. also are
found in the stools of w5% of healthy adults.
4
The infectious dose is
estimated to be 10
4
10
6
organisms per gram of ingested product
but may be lower in immunocompromised hosts and patients who
have diminished gastric acidity or have undergone ulcer surgery.
5
The incubation period has not been well-established, but is esti-
mated to be three weeks.
The rst clearly documented foodborne (coleslaw) outbreak
was in Nova Scotia in 1981.
5
It was associated with a case fatality
of 27%. In other sporadic outbreaks, 11% of all food samples
retrieved from the refrigerator were contaminated, and 64% of the
refrigerators of patients contained at least one contaminated food
item.
2
* Corresponding author. Tel.: 41 22 382 5462; fax: 41 22 382 5490.
E-mail address: Klara.PosfayBarbe@hcuge.ch (K.M. Posfay-Barbe).
Contents lists available at ScienceDirect
Seminars in Fetal & Neonatal Medicine
j ournal homepage: www. el sevi er. com/ l ocat e/ si ny
1744-165X/$ see front matter 2009 Elsevier Ltd. All rights reserved.
doi:10.1016/j.siny.2009.01.006
Seminars in Fetal & Neonatal Medicine 14 (2009) 228233
3. Present knowledge of transmission mechanisms
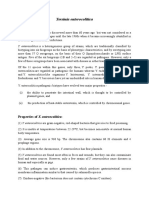
The pregnant woman ingests the bacterium, which crosses
intestinal cells into the bloodstream, passes through the placenta,
and infects the fetus (Fig. 1). While it is well-established that
placental infection always precedes fetal infection in early-onset
infection,
6
it remains unclear why there is an w20-fold increased
riskof listerial infectionduringpregnancyandwhyL. monocytogenes
targets the fetoplacental unit differently than other tissues. Immu-
nosuppression secondary to pregnancy may offer an explanation to
the rst question.
7
However, researchers have focused recently on
understanding (1) entry procedures used by L. monocytogenes to
move into host cells, (2) the placentas susceptibility to this micro-
organism, (3) cell-to-cell transmission, and the (4) immune mech-
anisms involved in infection.
810
L. monocytogenes uses a variety of
mechanisms to escape the hosts immune response to infection,
including surviving intracellularly. This factor is essential as listeria
not only survives in epithelial cells, but also inside the very cells,
such as macrophages, which should be eliminating it.
11
It is now
clear that listeriacaninfect cells bytwodifferent mechanisms: direct
invasion or cell-to-cell spread. Researchers have been working on
understanding the molecular basis of this successful strategy.
3.1. Direct invasion of cells
3.1.1. Internalin A and internalin B
L. monocytogenes invades and replicates within a wide range of
cell types, including macrophages and other antigen-presenting
cells.
11
Intracellular growth and spread to the next cells is facilitated
by a number of bacterial gene products, such as the invasion-
associated surface proteins internalin A (In1A) and internalin B
(In1B). Both invasins are necessary for listeria to enter different cell
types (for example epithelial or endothelial cells), and induce local
cytoskeletal rearrangements in the host cell, which facilitate
adherence and internalization. In1A can only mediate entry of lis-
teria into cell types expressing an In1A receptor.
12
In1A is highly
specic for human E-cadherin, a cell surface transmembrane
protein expressed by epithelial cells.
13
E-Cadherin is transiently
exposed to the luminal surface of the intestinal villi during
remodeling of epithelial junctions, thereby offering an entry point
to L. monocytogenes in the gut.
14
E-Cadherin is also found speci-
cally in villous cytotrophoblasts, and in localized areas of the basal
plasma membrane of syncytiotrophoblasts.
15
Syncytiotrophoblasts
are directly exposed to maternal blood in the intervillous space and
are considered a form of specialized endothelium. It has been
demonstrated that In1A is required for L. monocytogenes to cross
the human materno-fetal barrier; interaction between In1A and E-
cadherin enables the bacteria to target and cross the human
materno-fetal barrier at the villous trophoblastic barrier level.
15,16
Experts believe that L. monocytogenes is advantaged by the fact that
it adheres directly (via In1A and E-cadherin) to the trophoblastic
epithelium, and invades the trophoblast layer to access the core of
placental villi,
15
thereby explaining the specic tropism of the
organism for the placenta in humans. In further support of this
concept, an interesting epidemiological study showed that 100% of
the isolates of L. monocytogenes recovered from pregnant women
expressed a functional In1A, while it was only found in 65% of
strains recovered from food.
17
However, it seems unlikely that In1A
is the only mechanism involved in the bacterial internalization into
the trophoblasts. Bakardjiev et al. showed no clinical difference (in
an animal model) in fetal infection between wild-type bacteria and
In1A-deleted mutants.
18
Recognition of E-cadherin by In1A is
species specic, explaining why wild-type mice models cannot be
used for studying E-cadherin-associated adhesion or invasion.
13
Fortunately, guinea-pig E-cadherin binds to In1A with the same
afnity as that of humans, and the guinea-pig model employed by
Bakardjiev is now often applied to explore these associations.
18
In1B is more ubiquitous than In1A but at this time does not
explain the bacteriums tropism for the placenta. However, it has
been hypothesized that In1B, which binds to another surface
protein, called c-Met-tyrosine kinase, has a role in co-operating
with In1A. In the absence of In1B, In1A invades the placental tissue
inefciently thereby decreasing the pathogenicity of L. mono-
cytogenes.
15,19
The mechanism remains unclear. In1B may also have
a role facilitating the transfer of L. monocytogenes across the blood
brain barrier, but there has been no in-vivo demonstration of this
hypothesis.
20
Listerias internalin family is growing: at least 24
members have been identied in its genome, but not all present an
anchoring signal. Research is ongoing to identify the possible
contribution of these proteins to invasion of the host cell.
10,21
3.2. Invasion and virulence
Several bacterial proteins other than the internalins have been
identied as playing a role in cellular invasion and virulence. These
were identied by comparing pathogenic listerial species with non-
pathogenic species (such as L. innocua) and by studying lysins.
3.2.1. Listeriolysin O
After internalization, listeria needs to escape fromthe vacuole to
the cytoplasm (Fig. 1). Listeriolysin O (LLO), a pore-forming protein,
9
8
7
6
4
5
3
2
1
Stomach
Gut
Enlargement
Blood
Vessel
Actin
Filament
Tail
Fig. 1. Pathogenesis of L. monocytogenes. (1) Ingestion of the bacterium. (2) Passage
through the gut into the circulation. (3) Internalization by macrophages, poly-
morphonuclear cells, and other cells. (4) L. monocytogenes in intracellular vacuoles. (5)
L. monocytogenes escapes from the phagocytic vacuole through the action of lister-
iolysin D. (6) L. monocytogenes multiplies and forms actin lament tail that enables
movement. (7) By pushing across the membrane, the bacterium forms pseudopod-like
structures. (8) The pseudopod is phagocytosed by neighboring cells. (9) The phago-
cytosed cell forms a double-membraned internalized vacuole.
K.M. Posfay-Barbe, E.R. Wald / Seminars in Fetal & Neonatal Medicine 14 (2009) 228233 229
was the rst identied virulence factor of L. monocytogenes and is
required for bacterial escape from endocytic vacuoles. LLO-defec-
tive strains are ve to 10 times less invasive than wild-type
strains.
22
LLO is required in vivo for bacterial growth in tropho-
blastic cells, and for subsequent fetal invasion.
8
It is also known as
a modulator of the innate immune response by inducing new
cytokine synthesis in different immune cells and activating
different immune-response-associated pathways, such as the NF-
kappaB pathway.
23
The mechanisms behind this activation process
are, however, still unclear.
3.3. Cell-to-cell transmission
Once in the cytoplasm, listeria multiplies rapidly, migrates to the
host cell periphery and into cell-wall protrusions, which will be
taken up and ingested by neighboring cells where a new cycle will
start again (Fig. 1). This migration to the surface of the hosts cell
depends on ActA, a bacterial surface protein.
3.3.1. ActA
ActA is a virulence factor required for cell-to-cell spread of lis-
teria. It uses components of the host cells actin cytoskeleton to
generate a comet-tail which is rich in actin, enabling bacterial
propulsion in the cytosol leading to the infection of uninfected
neighbor cells.
24
Strains lacking ActA retain the ability to grow in
the placenta although at a lower rate than wild-type strains but
are strongly curtailed in their ability to spread fromcell to cell.
8
This
was demonstrated in an animal model, in which neonatal mice
injected with an isolate of L. monocytogenes lacking ActA induced
a strong primary and secondary Th1 CD4 and CD8 T-cell response,
but were protected against death from infection with listeria.
Interestingly, motility can be conferred upon other non-motile
micro-organisms (such as L. innocua) by adding ActA.
25
3.3.2. Positive regulatory factor A
The expression of nearly all bacterial gene products that
contribute to the survival and virulence of L. monocytogenes,
including LLO and ActA, are regulated by a transcriptional activator
known as positive regulatory factor A (PrfA). Strains lacking func-
tional PrfA are not virulent. The effect of PrfA seems to be reduced
at low temperature, but increased at low pH, probably explaining
the increased virulence of strains in a warm, acidic environment
after oral ingestion.
26,27
Post-transcriptional mechanisms control-
ling PrfA expression have also been described and contribute to the
synthesis of Int1A, Int1B, and LLO.
11
In summary, it is currently believed that: In1A (especially) and
In1B play a key role in the entry of listeria into host cells; LLO
punches holes to allow the organism to multiply inside the cyto-
plasm of the host cell; ActA produces a rocket-like mechanism to
penetrate into neighboring cells; and that all these mechanisms are
co-ordinated by PrfA. New virulence factors for L. monocytogenes as
well as genes involved in virulence or stress-response are described
regularly, increasing the complexity of the bacteriums pathoge-
nicity and its regulatory mechanisms.
28
4. Immunology
4.1. Innate and adaptive immune response
L. monocytogenes has been used for decades as a model
organism to study innate and adaptive immune responses against
intracellular pathogens. The innate immune response is immediate
and involves multiple cellular types, cytokines, and bactericidal
effector mechanisms. Monocytes and resident macrophages,
Kupffer cells for example, are known to ingest and destroy listeria.
Production of cytokines, such as interleukin (IL)-1, IL-6, and tumor
necrosis factor (TNF)-a are central in decreasing susceptibility to
disease by recruiting neutrophils. On the other hand, the adaptive
immune response against infection induced by L. monocytogenes
peaks about one week after infection, and is mainly a CD8
T-cell
response. This response has two main functions: the specic lysis of
infected cells and rapid production of IFN-g in response to IL-12 and
IL-18.
29
It is now hypothesized that early IFN-g production leads to
an accelerated formation of granulomas at sites of infection,
thereby walling off the infection. In mouse strains of listeria that
do not elicit an early IFN-g response, acute inammation continues
and listeria spreads between cells. Clearance of L. monocytogenes is
believed to be mediated through a Th1 immune response. IFN-g is
a crucial contributor to the Th1 response by activating macro-
phages, increasing antigen presentation via the MHC class I and II
pathways, and by inhibiting the expansion of Th2 cells.
30
A number of research groups have been focused on describing
the cells which produce IFN-g in infections caused by L. mono-
cytogenes. It seems likely that several cells, including natural killer
(NK) cells, dendritic cells during the early phase of innate immu-
nity, antigen-specic CD4 TH1 cells, and effector and memory CD8
T-cells during the later phase of adaptive immunity, produce IFN-g
during infection.
29,31
To complicate our understanding of the role of
IFN-g in listerial infection, it appears that IFN-g both promotes the
control of bacterial replication and also induces (paradoxically), the
erosion of CD8
T-cell memory during infection, thereby impairing
subsequent protective mechanisms.
32
In summary, IFN-g plays
a critical role in both innate and adaptive immune responses to L.
monocytogenes.
4.2. Toll-like receptors and autophagy
Toll-like receptor (TLR) 2 and TLR5 have been reported to
recognize L. monocytogenes.
33
TLR recognition of listerias lip-
oteichoic acid, lipoproteins, peptidoglycans and agellin leads to
the production of cytokines which in turn directly activate innate
effectors and recruit other cells.
34,35
Interestingly, however, in
a murine model in which animals lack myeloid differentiation
factor 88 (MyD88), an adaptor molecule downstream from TLRs, it
was shown that the animals are highly susceptible to infection with
listeria and that a MyD88-independent innate and adaptive
immune response exists.
36
Macro-autophagy, also referred to as autophagy, is a recently
described mechanism involved in the immune response of
mammals to micro-organisms.
37
Briey, through autophagy, an
infected cell can target an invading micro-organism and restrict its
growth by destroying it in the lysosome. It then induces an adaptive
immune response via presenting peptides on MHC Class I and II
molecules. Recent studies have shown that autophagy targets L.
monocytogenes before bacterial escape into the cytosol. However,
listeria is capable of using alternate strategies, including ActA-
dependent polymerization mentioned earlier, to avoid
destruction.
38
4.3. Specic relation to immunology of pregnant woman and child
The maternal immune system faces an important challenge
during pregnancy, i.e. to prevent rejection of the semi-allogenic
fetus and to protect itself and also the fetus from infection. Many
observations suggest that pregnancy is associated with a shift from
Th1 to Th2 cellular response and that the maternal immune system
is biased toward humoral immunity and away from cell-mediated
immunity (that could be harmful to the fetus). However, these
changes appear mostly to occur locally, as there is no strong
evidence suggesting that the maternal immune system is
K.M. Posfay-Barbe, E.R. Wald / Seminars in Fetal & Neonatal Medicine 14 (2009) 228233 230
compromised overall during pregnancy. New immunomodulating
mechanisms, not specic to L. monocytogenes, have been studied
extensively and are reviewed elsewhere.
39,40
L. monocytogenes, on
the other hand, has to develop different strategies against the
defence mechanisms of the host to survive. While some of these
defences are not specic to pregnancy, such as gastric acidity, lis-
teria has mastered manipulating the differences related to the
immaturity of the immune system of the fetus. Neonatal immunity
is reported to be Th2-biased. This avoids maternal rejection of fetal
antigens induced by Th1-type inammation that may result in
spontaneous abortion or premature delivery.
41
Furthermore, it
appears that (murine) neonates have a lower expression of
mannose-binding lectins and certain TLRs than adults.
42
These
mediators are necessary to develop Th1 immune responses and
might explainwhy neonates are highly susceptible to infectionwith
listeria. This fact has been questioned by others who believe that it
is not a decreased expression of TLRs, but instead a TLR-induced
TNF-a production which is signicantly decreased in neonates.
43
Interestingly, the same authors acknowledge that neonates are
capable of a robust IL-6 production, indicating that the intrinsic TLR
pathway is functional at birth, and suggesting an abnormal, still
unclear, TLR defect related to Th2.
L. monocytogenes can also gain access to the neonate via oral
exposure during the passage through the birth canal. Enteric anti-
microbial peptides derived from Paneth cells provide protection
from intestinal infection. However, these cells are not present
during the rst weeks of life. Recently, Me nard et al. described an
antimicrobially active form of peptide, called CRAMP (cathelin-
related antimicrobial peptide), in the epithelium of neonatal mice,
which is expressed constitutively during the rst weeks of life
only.
44
CRAMP provides signicant protection against bacterial
growth in the gut. This developmental switch in innate immune
effector expression (i.e. CRAMP being functional only while Paneth
cells are lacking) is a newly described mechanism in the early
protection against infection with listeria. Enhanced understanding
of the specicity of the immune system in neonates may lead to
novel treatment strategies in years to come.
5. Neonatal disease
Worldwide, L. monocytogenes is one of the three major causes of
meningitis in neonates. Clinical manifestations may be very similar
to those seen with group B streptococcal disease, and there is a high
fatality rate (350%). There are two forms of neonatal listeriosis.
5.1. Early onset
The mothers of affected children often have a u-like illness
a few days before delivery, which may be preterm. Listeria
bacteremia presents with an acute febrile illness, which is often
accompanied by myalgias, arthralgias, backache and headache.
Maternal illness is observed most often in the third trimester.
Neonatal death and stillbirth occur in approximately one-fth of
maternal infections. Two-thirds of the infants who survive delivery
to a woman who experiences listeriosis in pregnancy will develop
neonatal infection. The infants are believed to be infected in utero
because of the bacteremic phase of their mothers, but ascending
infections have been described. The highest concentrations of L.
monocytogenes are found in the lung and gut, suggesting that
infection also can be acquired in utero via inhalation and ingestion
of infected amniotic uid as well as via the hematogenous route.
During labor, brown-stained amniotic uid is seen and maternal
fever may be present. Serotypes 1a and 1b are most common.
The mean onset of symptoms is 1.5 days after birth. A sepsis-like
picture predominates, but other common manifestations are acute
respiratory distress, pneumonia, and more rarely, meningitis or
myocarditis. Strategies implemented to prevent group B strepto-
coccal sepsis in the newborn may have secondarily decreased the
rate of early-onset listerial infection.
Granulomatosis infantisepticum is a widely disseminated
granuloma characteristic of severe listerial disease. The lesions are
more common in the liver, skin and placenta, but also appear in the
brain, adrenal glands, spleen, kidney, lungs and gastrointestinal
tract. Aspiration of infected uid can contribute to acute respiratory
failure and hemodynamic compromise in the neonate.
5.2. Late onset
This form of neonatal listeriosis is less common than the early-
onset form, but it occurs more frequently in term infants who are
the products of uncomplicated pregnancies. The babies are healthy
at birth, and the maternal history is usually normal. The rst
manifestations of infection appear several days to weeks after birth,
with a mean onset of illness at 14.3 days after birth. The clinical
manifestation in this group is more likely to be meningitis than
sepsis, but it can be subtle, with fever, irritability, anorexia, diar-
rhea, and lethargy. Postpartum transmission is assumed to occur
either during delivery or nosocomially. Serotype 4b is most
frequent in late-onset disease.
6. Diagnosis
Listeriosis usually presents with leukocytosis, but unlike its
name, rarely with monocytosis. Isolation of Listeria spp. from
a normally sterile site denes the disease. Thirty-six hours of
incubation usually are necessary for sufcient growth for identi-
cation. The pathogen often is observed on the Gram stain of the
meconium of infected newborns. Carriage in the gastrointestinal
tracts of older children may be common but difcult to demon-
strate because the organism is fastidious and normal ora are
plentiful. Screening of rectal or vaginal cultures is not clinically
useful.
Cold enrichment is not as good as selective media to isolate the
organism from specimens containing multiple species (e.g. in food
or stools). Rapid detection tests are based on the use of either
monoclonal antibodies or nucleic acid hybridizations, but they only
identify the genus Listeria.
45
When the central nervous systemis infected, cerebrospinal uid
(CSF) is usually purulent, with leukocyte counts of 10010 000/mL
(0.110 10
9
/L). Polymorphonuclear leukocytes predominate in
70% of cases, but the severity of the inammatory response does
not correlate with the prognosis. The Gramstain of CSF is positive in
<40% of patients. Protein levels are usually elevated, and higher
values are correlated with poor prognosis. In 60% of the cases,
glucose levels in CSF are normal, unlike with other causes of
bacterial meningitis. When there is an infection of the CNS, blood
cultures are positive in 6075% of patients. Serologic test for anti-
listeriolysin O may assist in diagnosing both invasive and non-
invasive listeriosis.
46
7. Management
Four factors make therapy of listeriosis difcult: (1) The hosts
susceptibility to infection (compromised host, extreme age groups)
is linked with atypical onset of disease; (2) intracellular survival
and involvement of granulomatous tissue prevent prompt and
successful therapy, even with highly potent antibiotics; (3) diag-
nosis and treatment are delayed because of the previous two
factors; and (4) ampicillin often attains merely bacteriostatic
concentrations in vivo and is not effective intracellularly.
47
Because
K.M. Posfay-Barbe, E.R. Wald / Seminars in Fetal & Neonatal Medicine 14 (2009) 228233 231
L. monocytogenes can multiply within macrophages, several
prerequisites must be fullled to inhibit these hidden bacteria.
Antibiotics must penetrate into and distribute within host cells and
remain stable within this environment. Recommmendations are
based on data obtained from in-vitro susceptibility testing, animal
models, and clinical experience with small numbers of patients
who were compared with historic controls.
No controlled trials have established a drug of choice or duration
of therapy for listeriosis. L. monocytogenes is sensitive in vitro to
penicillin G, ampicillin, erythromycin, sulfamethoxazole, trimeth-
oprim, chloramphenicol, rifampin, tetracyclines, and aminoglyco-
sides. Bactericidal antibiotics include sulfamethoxazole,
trimethoprim, and aminoglycosides. Gentamicin and tobramycin
have been reported to have greater in-vitro activity than strepto-
mycin, kanamycin, and amikacin. Listeria always are resistant to
cephalosporins.
48
Chloramphenicol should not be used because of
unacceptable failure and relapse rates, and quinolones do not have
good in-vitro activity. Ampicillin, which is superior to penicillin,
and gentamicin have shown synergistic effects in some studies.
48
Accordingly, gentamicin with ampicillin is recommended for
treatment of listerial meningitis.
If the patient is allergic to ampicillin or gentamicin, sulfame-
thoxazole-trimethoprim is recommended because it is bactericidal
and reaches adequate levels in the serum and CSF.
48
No systematic
study has examined the duration of therapy, but the current
recommendations are 1421 days of treatment for meningitis due
to L. monocytogenes.
8. Prevention
There is no vaccine for listeria infection. Dietary recommenda-
tions for preventing foodborne listeriosis were established by the
Centers for Disease Control and Prevention (CDC) in 1992. They are
similar to those for other foodborne illnesses and include thorough
cooking of raw food from animal sources; washing of raw vegeta-
bles; avoidance of unpasteurized dairy products; keeping uncooked
meats separate from vegetables; washing hands, knives, and
cutting boards after exposure to uncooked food; and regular
cleaning and disinfection of the insides of refrigerators. Persons at
high risk for listeriosis should avoid soft cheeses, reheat (until
steaming hot) leftover and ready-to-eat foods, and avoid cold cuts if
unable to reheat them thoroughly.
The US Department of Agriculture began surveillance in 1989 for
L. monocytogenes in ready-to-eat processed meats and enforced
regulations prohibiting the sale of contaminated meats. Since then,
the number of cases of listerial infection has dropped substantially.
The CDCs Division of Foodborne, Bacterial and Mycotic Diseases
tracks the annual incidence of certain foodborne illnesses,
including listeria, in 10 states through Food Net Surveillance.
49
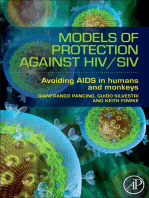
Between 1996 and 2006, the incidence of listeria declined by 36%,
although an outbreak in 2002, related to contaminated turkey
meat, resulted in 54 illnesses, eight deaths and three fetal deaths in
nine states (Fig. 2).
49
References
1. Swaminathan B, Hayes PS, Przybyszewski VA, Plikaytis BD. Evaluation of
enrichment and plating media for isolating Listeria monocytogenes. J Assoc Off
Anal Chem 1988;71:6648.
2. Pinner RW, Schuchat A, Swaminathan B, et al. Role of foods in sporadic liste-
riosis. II. Microbiologic and epidemiologic investigation. The Listeria Study
Group. J Am Med Assoc 1992;267:204650.
3. Schuchat A, Lizano C, Broome CV, Swaminathan B, Kim C, Winn I. Outbreak of
neonatal listeriosis associated with mineral oil. Pediatr Infect Dis J 1991;10:
1839.
4. Schlech III WF. Foodborne listeriosis. Clin Infect Dis 2000;31:7705.
5. Schlech III WF. Listeria gastroenteritis old syndrome, new pathogen. N Engl J
Med 1997;336:1302.
6. Kaur S, Malik SV, Vaidya VM, Barbuddhe SB. Listeria monocytogenes in spon-
taneous abortions in humans and its detection by multiplex PCR. J Appl
Microbiol 2007;103:188996.
7. Redline RW, Lu CY. Specic defects in the anti-listerial immune response in
discrete regions of the murine uterus and placenta account for susceptibility to
infection. J Immunol 1988;140:394755.
8. Le Monnier A, Autret N, Join-Lambert OF, et al. ActA is required for crossing of
the fetoplacental barrier by Listeria monocytogenes. Infect Immun 2007;75:
9507.
9. DOrazio SE, Troese MJ, Starnbach MN. Cytosolic localization of Listeria mono-
cytogenes triggers an early IFN-gamma response by CD8 T cells that correlates
with innate resistance to infection. J Immunol 2006;177:714654.
10. Seveau S, Pizarro-Cerda J, Cossart P. Molecular mechanisms exploited by Lis-
teria monocytogenes during host cell invasion. Microbes Infect 2007;9:116775.
11. Gray MJ, Freitag NE, Boor KJ. How the bacterial pathogen Listeria monocytogenes
mediates the switch from environmental Dr. Jekyll to pathogenic Mr. Hyde.
Infect Immun 2006;74:250512.
12. Hamon M, Bierne H, Cossart P. Listeria monocytogenes: a multifaceted model.
Nat Rev Microbiol 2006;4:42334.
13. Lecuit M, Dramsi S, Gottardi C, Fedor-Chaiken M, Gumbiner B, Cossart P.
A single amino acid in E-cadherin responsible for host specicity
towards the human pathogen Listeria monocytogenes. EMBO J
1999;18:395663.
14. Pentecost M, Otto G, Theriot JA, Amieva MR. Listeria monocytogenes invades the
epithelial junctions at sites of cell extrusion. PLoS Pathog 2006;2:e3.
15. Lecuit M, Nelson DM, Smith SD, et al. Targeting and crossing of the human
maternofetal barrier by Listeria monocytogenes: role of internalin interaction
with trophoblast E-cadherin. Proc Natl Acad Sci USA 2004;101:61527.
16. Bonazzi M, Veiga E, Cerda JP, Cossart P. Successive post-translational modi-
cations of E-cadherin are required for InlA-mediated internalisation of Listeria
monocytogenes. Cell Microbiol 2008; 10: 220822.
17. Jacquet C, Doumith M, Gordon JI, Martin PM, Cossart P, Lecuit M. A molecular
marker for evaluating the pathogenic potential of foodborne Listeria mono-
cytogenes. J Infect Dis 2004;189:2094100.
18. Bakardjiev AI, Stacy BA, Fisher SJ, Portnoy DA. Listeriosis in the pregnant guinea
pig: a model of vertical transmission. Infect Immun 2004;72:48997.
19. Shen Y, Naujokas M, Park M, Ireton K. InIB-dependent internalization of Listeria
is mediated by the Met receptor tyrosine kinase. Cell 2000;103:50110.
2.0
1.0
0.5
0.4
1996-
1998
1999 2000 2001 2002 2003
Year
R
e
l
a
t
i
v
e
r
a
t
e
(
l
o
g
s
c
a
l
e
)
2004 2005 2006 2007
0.9
0.8
0.7
0.6
Fig. 2. Relative rates of laboratory-conrmed infections with listeria compared with
19961998 rates, by year (Foodborne Diseases Active Surveillance Network, USA,
19962007).
Research directions
To understand better how this quiet saprophyte
becomes a deadly agent.
To determine the infectious dose of listeria and to dene
the extent of human illness by searching for listeria in
outbreaks of febrile gastroenteritis where no other
pathogens are identied.
To identify new bacterial and host effectors.
To examine interaction and activation processes
between bacteria and host, especially in vulnerable
populations, such as neonates.
K.M. Posfay-Barbe, E.R. Wald / Seminars in Fetal & Neonatal Medicine 14 (2009) 228233 232
20. Greiffenberg L, Goebel W, Kim KS, et al. Interaction of Listeria monocytogenes
with human brain microvascular endothelial cells: InlB-dependent invasion,
long-term intracellular growth, and spread from macrophages to endothelial
cells. Infect Immun 1998;66:52607.
21. Sabet C, Lecuit M, Cabanes D, Cossart P, Bierne H. LPXTG protein InlJ, a newly
identied internalin involved in Listeria monocytogenes virulence. Infect Immun
2005;73:691222.
22. Dramsi S, Cossart P. Listeriolysin O-mediated calcium inux potentiates entry of
Listeria monocytogenes into the human Hep-2 epithelial cell line. Infect Immun
2003;71:36148.
23. Park JM, Ng VH, Maeda S, Rest RF, KarinM. AnthrolysinOandother gram-positive
cytolysins are toll-like receptor 4 agonists. J Exp Med 2004;200:164755.
24. Portnoy DA, Auerbuch V, Glomski IJ. The cell biology of Listeria monocytogenes
infection: the intersection of bacterial pathogenesis and cell-mediated immu-
nity. J Cell Biol 2002;158:40914.
25. Kocks C, Marchand JB, Gouin E, et al. The unrelated surface proteins ActA of
Listeria monocytogenes and IcsA of Shigella exneri are sufcient to confer actin-
based motility on Listeria innocua and Escherichia coli respectively. Mol Micro-
biol 1995;18:41323.
26. Johansson J, Mandin P, Renzoni A, Chiaruttini C, Springer M, Cossart P. An RNA
thermosensor controls expression of virulence genes in Listeria mono-
cytogenes. Cell 2002;110:55161.
27. Ferreira A, Sue D, OByrne CP, Boor KJ. Role of Listeria monocytogenes sigma(B) in
survival of lethal acidic conditions and in the acquired acid tolerance response.
Appl Environ Microbiol 2003;69:26928.
28. Chaturongakul S, Raengpradub S, Wiedmann M, Boor KJ. Modulation of stress
and virulence in Listeria monocytogenes. Trends Microbiol 2008;16:38896.
29. Berg RE, Crossley E, Murray S, Forman J. Memory CD8 T cells provide innate
immune protection against Listeria monocytogenes in the absence of cognate
antigen. J Exp Med 2003;198:158393.
30. Pamer EG. Immune responses to Listeria monocytogenes. Nat Rev Immunol
2004;4:81223.
31. Plitas G, Chaudhry UI, Kingham TP, Raab JR, DeMatteo RP. NK dendritic cells are
innate immune responders to Listeria monocytogenes infection. J Immunol
2007;178:44116.
32. Dudani R, Murali-Krishna K, Krishnan L, Sad S. IFN-gamma induces the erosion
of preexisting CD8 T cell memory during infection with a heterologous intra-
cellular bacterium. J Immunol 2008;181:17009.
33. Torres D, Barrier M, Bihl F, et al. Toll-like receptor 2 is required for optimal
control of Listeria monocytogenes infection. Infect Immun 2004;72:21319.
34. Hayashi F, Smith KD, Ozinsky A, et al. The innate immune response to bacterial
agellin is mediated by Toll-like receptor 5. Nature 2001;410:1099103.
35. Machata S, Tchatalbachev S, Mohamed W, Jansch L, Hain T, Chakraborty T.
Lipoproteins of Listeria monocytogenes are critical for virulence and TLR2-
mediated immune activation. J Immunol 2008;181:202835.
36. Way SS, Kollmann TR, Hajjar AM, Wilson CB. Cutting edge: protective cell-
mediated immunity to Listeria monocytogenes in the absence of myeloid
differentiation factor 88. J Immunol 2003;171:5337.
37. Kirkegaard K, Taylor MP, Jackson WT. Cellular autophagy: surrender, avoidance
and subversion by microorganisms. Nat Rev Microbiol 2004;2:30114.
38. BirminghamCL, Canadien V, Gouin E, et al. Listeria monocytogenes evades killing
by autophagy during colonization of host cells. Autophagy 2007;3:44251.
39. Poole JA, Claman HN. Immunology of pregnancy. Implications for the mother.
Clin Rev Allergy Immunol 2004;26:16170.
40. Seavey MM, Mosmann TR. Immunoregulation of fetal and anti-paternal
immune responses. Immunol Res 2008;40:97113.
41. Adkins B, Leclerc C, Marshall-Clarke S. Neonatal adaptive immunity comes of
age. Nat Rev Immunol 2004;4:55364.
42. Byun HJ, Jung WW, Lee JB, et al. An evaluation of the neonatal immune system
using a listeria infection model. Neonatology 2007;92:8390.
43. Levy O, Coughlin M, Cronstein BN, Ry RM, Desai A, Wessels M. The adenosine
system selectively inhibits TLR-mediated TNF-a production in the human
newborn. J Immunol 2006;144:195666.
44. Menard S, Forster V, Lotz M, et al. Developmental switch of intestinal antimi-
crobial peptide expression. J Exp Med 2008;205:18393.
45. Sontakke S, Farber JM. The use of PCR ribotyping for typing strains of Listeria
spp. Eur J Epidemiol 1995;11:66573.
46. Dalton CB, Austin CC, Sobel J, et al. An outbreak of gastroenteritis and fever due
to Listeria monocytogenes in milk. N Engl J Med 1997;336:1005.
47. Marget W, Seeliger HP. Listeria monocytogenes infections therapeutic possi-
bilities and problems. Infection 1988;16:S1757.
48. Espaze EP, Reynaud AE. Antibiotic susceptibilities of Listeria: in vitro studies.
Infection 1988;16:S1604.
49. Anonymous. Preliminary foodnet data on the incidence of infection with
pathogens transmitted commonly through food 10 states, 2007. MMWR Morb
Mortal Wkly Rep 2008;57:36670.
K.M. Posfay-Barbe, E.R. Wald / Seminars in Fetal & Neonatal Medicine 14 (2009) 228233 233
You might also like
- Female Urinary Tract Infections in Clinical PracticeFrom EverandFemale Urinary Tract Infections in Clinical PracticeBob YangNo ratings yet
- UNP-0064-archivekontoliosiss 2 PDFDocument2 pagesUNP-0064-archivekontoliosiss 2 PDFfarah rachmahNo ratings yet
- Jurnal Patogenesis AmoebiasisDocument12 pagesJurnal Patogenesis AmoebiasisAngga NuralamNo ratings yet
- Enterobacter SakazakiiDocument7 pagesEnterobacter SakazakiiRadwan AjoNo ratings yet
- Amebiasis: Review ArticleDocument9 pagesAmebiasis: Review ArticleJouffrey Itaar MadridistaNo ratings yet
- Shigella Infections in Children: New Insights: Shai Ashkenazi, MD, MSCDocument7 pagesShigella Infections in Children: New Insights: Shai Ashkenazi, MD, MSCmerrycardinaNo ratings yet
- Listeria Monocytogenes ThesisDocument4 pagesListeria Monocytogenes Thesisjennymancinibuffalo100% (1)
- Congenital Toxoplasmosis: A Review: Marissa Martinez Hampton, MSNDocument5 pagesCongenital Toxoplasmosis: A Review: Marissa Martinez Hampton, MSNayuwulandariNo ratings yet
- Listeria Monocytogenes (Listeriosis) 2-12-2015Document11 pagesListeria Monocytogenes (Listeriosis) 2-12-2015MohamedNo ratings yet
- Kongenital ToksoplasmosisDocument6 pagesKongenital Toksoplasmosisrini9384No ratings yet
- Canine Brucellosis Old Foe and Reemerging ScourgeDocument17 pagesCanine Brucellosis Old Foe and Reemerging ScourgeMargarita CCNo ratings yet
- Parasitic Diseases OMSDocument13 pagesParasitic Diseases OMSlacmftcNo ratings yet
- ListeriaDocument10 pagesListeriasajad abasNo ratings yet
- Salmonella, The Host and Disease: A Brief ReviewDocument8 pagesSalmonella, The Host and Disease: A Brief ReviewPedro Albán MNo ratings yet
- Key Infections in The PlacentaDocument14 pagesKey Infections in The PlacentaLauraGonzalezNo ratings yet
- Yersinia EnterocoliticaDocument9 pagesYersinia EnterocoliticaVALENTINA JOCABED OROZCO VARGASNo ratings yet
- Correspondence: Broad-And Narrow-Spectrum Antibiotics: A Different ApproachDocument2 pagesCorrespondence: Broad-And Narrow-Spectrum Antibiotics: A Different ApproachJulio Andro ArtamulandikaNo ratings yet
- The Reoviridae Family: by Luka, Mela IluDocument49 pagesThe Reoviridae Family: by Luka, Mela IluMela LukaNo ratings yet
- Assessing Gut Microbiota Perturbations During The Early Phase of Infectious Diarrhea in Vietnamese ChildrenDocument18 pagesAssessing Gut Microbiota Perturbations During The Early Phase of Infectious Diarrhea in Vietnamese ChildrenKavyarani RathodNo ratings yet
- Intestinal HelminthsDocument4 pagesIntestinal HelminthssivaNo ratings yet
- Poirel 2018Document27 pagesPoirel 2018Leidy GarciaNo ratings yet
- Human Trophoblasts Confer Resistance To Viruses ImDocument8 pagesHuman Trophoblasts Confer Resistance To Viruses Imonline videoNo ratings yet
- Yersinia EnterocoliticaDocument10 pagesYersinia EnterocoliticaShaheen AlamNo ratings yet
- Uma Revisão Sobre Leptospitose BovinaDocument9 pagesUma Revisão Sobre Leptospitose BovinaDiovana MachadoNo ratings yet
- Rudolph PediatricDocument9 pagesRudolph PediatricMuhammad RezaNo ratings yet
- Infectious Causes of Embryonic and Fetal MortalityDocument16 pagesInfectious Causes of Embryonic and Fetal MortalityFlaviu Tabaran0% (1)
- Diarrhea in Neonatal RuminantsDocument8 pagesDiarrhea in Neonatal Ruminantsbarbybackup2No ratings yet
- Safety Aspects of Probiotic ProductsDocument4 pagesSafety Aspects of Probiotic ProductsSrinivas PingaliNo ratings yet
- Volume: 04 Issue: 06 - Nov-Dec 2023Document8 pagesVolume: 04 Issue: 06 - Nov-Dec 2023Central Asian StudiesNo ratings yet
- Fimmu 04 00507 PDFDocument20 pagesFimmu 04 00507 PDFSilma FarrahaNo ratings yet
- Ijerph 15 00617Document19 pagesIjerph 15 00617arieftamaNo ratings yet
- Gram-Negative Rods Related To AnimalDocument35 pagesGram-Negative Rods Related To AnimalAsa Mutia SNo ratings yet
- Systemic Infections From GiDocument10 pagesSystemic Infections From GiJake MillerNo ratings yet
- Balantidium Coli: Rare Urinary Pathogen or Fecal Contaminant in Urine? Case Study and ReviewDocument3 pagesBalantidium Coli: Rare Urinary Pathogen or Fecal Contaminant in Urine? Case Study and Reviewnabil saktiNo ratings yet
- Listeria Mono OIEDocument17 pagesListeria Mono OIEAjay PathakNo ratings yet
- Lawsonia Intracellularis - Revisiting The Disease Ecology and Control of This Fastidious Pathogen in PigsDocument11 pagesLawsonia Intracellularis - Revisiting The Disease Ecology and Control of This Fastidious Pathogen in PigsVo Thanh ThinNo ratings yet
- Clinical Forum: Bovine Leptospirosis: Sheila RusbridgeDocument7 pagesClinical Forum: Bovine Leptospirosis: Sheila RusbridgePaulo CarvalhoNo ratings yet
- J. Biol. Chem.-2019-Coelho-1202-17 PDFDocument17 pagesJ. Biol. Chem.-2019-Coelho-1202-17 PDFJoel Torres VillenaNo ratings yet
- B1 CellDocument22 pagesB1 CellPierfelice CutrufelliNo ratings yet
- Introduction To Medical MicrobiologyDocument9 pagesIntroduction To Medical MicrobiologyIsba Shadai Estrada GarciaNo ratings yet
- Ascaris LumbricoidesDocument33 pagesAscaris LumbricoidesRosi Gustina100% (5)
- Helmintos NematodosDocument12 pagesHelmintos NematodosHANNIANo ratings yet
- Toxo PregnancyDocument15 pagesToxo PregnancyYossy CatarinaNo ratings yet
- BiflacDocument17 pagesBiflacMohamed SafwanNo ratings yet
- INTESTINO FELIZ, ANIMAL SALUDABLE EsDocument22 pagesINTESTINO FELIZ, ANIMAL SALUDABLE EsurielNo ratings yet
- Ascaris LumbricoidesDocument33 pagesAscaris LumbricoidesBio SciencesNo ratings yet
- Rotavirus: Structure & Composition PathogenesisDocument4 pagesRotavirus: Structure & Composition PathogenesisyusrinastitiNo ratings yet
- Eosinophils Protect Nematode Parasite Larvae by Regulating Local ImmunityDocument20 pagesEosinophils Protect Nematode Parasite Larvae by Regulating Local ImmunityLeonardo DonatiNo ratings yet
- (WIDMER E A) Flesh of Swine (Ministry, 1988-05)Document3 pages(WIDMER E A) Flesh of Swine (Ministry, 1988-05)Nicolas MarieNo ratings yet
- Salmonella Bacteria, While The Infectious Dose For Conventional Animals Is Near 10Document6 pagesSalmonella Bacteria, While The Infectious Dose For Conventional Animals Is Near 10Mudit MisraNo ratings yet
- Lec 3 Host-Parasite RelationshipDocument23 pagesLec 3 Host-Parasite RelationshiphazelNo ratings yet
- PHD Thesis SalmonellaDocument4 pagesPHD Thesis Salmonellafqzaoxjef100% (2)
- Infectious Diseases of The Female Genital TractDocument1,111 pagesInfectious Diseases of The Female Genital TractJohn Ntokos100% (2)
- Factsheet Toxoplasmosis enDocument2 pagesFactsheet Toxoplasmosis enSunil YadavNo ratings yet
- Pyometrainsmallanimals: Ragnvi HagmanDocument23 pagesPyometrainsmallanimals: Ragnvi HagmansalomonNo ratings yet
- Models of Protection Against HIV/SIV: Models of Protection Against HIV/SIVFrom EverandModels of Protection Against HIV/SIV: Models of Protection Against HIV/SIVGianfranco PancinoNo ratings yet
- 2011 - Spuriously Raised Serum Creatinine Associated With An Excipient Present in An Intravenous Dexamethasone FormulationDocument4 pages2011 - Spuriously Raised Serum Creatinine Associated With An Excipient Present in An Intravenous Dexamethasone FormulationFede0No ratings yet
- Severing Ha Us 1987Document4 pagesSevering Ha Us 1987Fede0No ratings yet
- 2012 - Prediction of The Hematocrit of Dried Blood Spots Via Potassium Measurement On A Routine Clinical Chemistry AnalyzerDocument14 pages2012 - Prediction of The Hematocrit of Dried Blood Spots Via Potassium Measurement On A Routine Clinical Chemistry AnalyzerFede0No ratings yet
- Interpretation of Arterial Blood Gas: Review ArticleDocument8 pagesInterpretation of Arterial Blood Gas: Review ArticleFede0No ratings yet
- Severinghaus 1986Document16 pagesSeveringhaus 1986Fede0No ratings yet
- Severing Ha Us 1985Document13 pagesSevering Ha Us 1985Fede0No ratings yet
- Severinghaus 1986Document14 pagesSeveringhaus 1986Fede0No ratings yet
- 2005 - Estimate of Biological Variation of Laboratory Analytes Based On The Third National Health and Nutrition Examination SurveyDocument3 pages2005 - Estimate of Biological Variation of Laboratory Analytes Based On The Third National Health and Nutrition Examination SurveyFede0No ratings yet
- Shaw 2014Document7 pagesShaw 2014Fede0No ratings yet
- Ball Och 2008sdfDocument8 pagesBall Och 2008sdfFede0No ratings yet
- Stubblefield 2012Document8 pagesStubblefield 2012Fede0No ratings yet
- BMJ h6138 FullDocument10 pagesBMJ h6138 FullFede0No ratings yet
- Sevenet Et Al-2017-International Journal of Laboratory HematologyDocument8 pagesSevenet Et Al-2017-International Journal of Laboratory HematologyFede0No ratings yet
- Mechanism of Interference by Hemoglobin in The Determination of Total Bilirubin. II. Method of Jendrassik-GrofDocument4 pagesMechanism of Interference by Hemoglobin in The Determination of Total Bilirubin. II. Method of Jendrassik-GrofFede0No ratings yet
- 2009 - Reference Intervals The Way ForwardDocument11 pages2009 - Reference Intervals The Way ForwardFede0No ratings yet
- Boyd 2015Document8 pagesBoyd 2015Fede0No ratings yet
- 77: Hyperphenylalaninemia: Phenylalanine Hydroxylase DeficiencyDocument114 pages77: Hyperphenylalaninemia: Phenylalanine Hydroxylase DeficiencyFede0No ratings yet
- Biological Variation Database Structure and Criteria Used For Generation and UpdateDocument7 pagesBiological Variation Database Structure and Criteria Used For Generation and UpdateFede0No ratings yet
- Arzideh 2009Document15 pagesArzideh 2009Fede0No ratings yet
- Ar ExportsDocument1 pageAr ExportsRais AlamNo ratings yet
- Manual OccultismDocument390 pagesManual OccultismJikker Gigi Phatbeatzz Barrow100% (11)
- 510 1453 1 PB Tiang ReklameDocument6 pages510 1453 1 PB Tiang ReklameGunaedy UtomoNo ratings yet
- Module 5: Safety and Health at Work: Participant's HandbookDocument24 pagesModule 5: Safety and Health at Work: Participant's HandbookChristian Surio RamosNo ratings yet
- Yehuda Berg Satan PDFDocument77 pagesYehuda Berg Satan PDFOswaldo Archundia100% (7)
- Eureka Forbes ReportDocument75 pagesEureka Forbes ReportUjjval Jain0% (1)
- MFI 2 - Unit 3 - SB - L+SDocument10 pagesMFI 2 - Unit 3 - SB - L+SHoan HoàngNo ratings yet
- WPP Jak Campus - Defect All Level - 18042023Document15 pagesWPP Jak Campus - Defect All Level - 18042023bbm FebriNo ratings yet
- Miltel - Case Study, Steven Age, UKDocument2 pagesMiltel - Case Study, Steven Age, UKAnit SahuNo ratings yet
- Module IiDocument5 pagesModule IiFahmi PrayogiNo ratings yet
- Safety Data Sheet: Section 1. Identification Jotun Essence Easy CleanDocument11 pagesSafety Data Sheet: Section 1. Identification Jotun Essence Easy CleanHồng PhongNo ratings yet
- UNDP NP Dhangadhi SWM TOR FinalDocument4 pagesUNDP NP Dhangadhi SWM TOR FinalNirmal K.c.No ratings yet
- Anil Singh Rathore: Career HighlightsDocument4 pagesAnil Singh Rathore: Career HighlightsHRD CORP CONSULTANCYNo ratings yet
- SSMTT-27 E1 PDFDocument8 pagesSSMTT-27 E1 PDFblackNo ratings yet
- BSN Curriculum 2012Document1 pageBSN Curriculum 2012Joana Bless PereyNo ratings yet
- Drainage BasinsDocument4 pagesDrainage BasinsDannySP10100% (1)
- Agricultural Machinery in PakistanDocument19 pagesAgricultural Machinery in PakistanBadar NiaziNo ratings yet
- (WWW - Asianovel.com) - Quan Zhi Gao Shou Chapter 051 - Chapter 100Document310 pages(WWW - Asianovel.com) - Quan Zhi Gao Shou Chapter 051 - Chapter 100Exile0105No ratings yet
- Paper 2 Phy 2019-2023Document466 pagesPaper 2 Phy 2019-2023Rocco IbhNo ratings yet
- Welding Inspection Technology: Module 7 - Visual Inspection WorkshopDocument20 pagesWelding Inspection Technology: Module 7 - Visual Inspection Workshoprex valenciaNo ratings yet
- Suez Canal ReportDocument5 pagesSuez Canal ReportAnonymous Pc6LwfCNo ratings yet
- The DSG DQ200 LifespanDocument1 pageThe DSG DQ200 Lifespanqt99qzyhrbNo ratings yet
- Appetizer Summative TestDocument36 pagesAppetizer Summative TestArgelynPadolinaPedernalNo ratings yet
- Identifying - Explaining Brake System FunctionsDocument39 pagesIdentifying - Explaining Brake System FunctionsJestoni100% (1)
- TSBDocument3 pagesTSBnoe dela vegaNo ratings yet
- The Art of Logical ThinkingDocument210 pagesThe Art of Logical ThinkingAndyAyam100% (1)
- Saberon StratMan2Document3 pagesSaberon StratMan2paredesladyheart18No ratings yet
- Action, Desire and Subjectivity in Prabhakara MimamsaDocument28 pagesAction, Desire and Subjectivity in Prabhakara Mimamsasiddy_777No ratings yet
- Industrial Training Report (Kapar Power Plant)Document40 pagesIndustrial Training Report (Kapar Power Plant)Hakeemi Baseri100% (2)
- EclipseDocument6 pagesEclipsetoncipNo ratings yet