Shock-TraumaResuscitation
Otmar Trentz, Zrich
Polytrauma
Polytrauma
Shock
Shock
Alimentation
Alimentation
Rhabdomyolysis
Rhabdomyolysis
Comp
. Syndr
. u.
Comp.
Syndr.
u. ACS
ACS
Traumatic
Traumatic brain
brain injury
injury
�Polytrauma
Syndrome of multiple injuries exceeding a
defined severity (ISS 17), with
consecutive systemic reactions which may
lead to dysfunction or failure of remote,
primarily not injured, organs or vital
systems.
Polytrauma
Surgical
Surgical systemic
systemic disease
disease
pathophysiological understanding
complete resuscitation
correct triage
negotiated titration of care
�Pathophysiology
Wound = inflammatory focus
Hypoxic zone
Dead
Tissue
Endocrine organ
Release of mediators
Systemic reaction
Cascade of defence mechanisms
Polytrauma
Systemic
Systemic reactions
reactions
Neuro-endocrine responses
Stimulation neuro-immune axis
Metabolic responses
SIRS
Shock
I/R injury
�Trauma
Systemic Inflammatory
Response Syndrome
(SIRS)
physiologic
reversible
Host defense response
Host defense failure
disease
Damage healing
Death
pathophysiologic
irreversible
Systemic Inflammatory
Response Syndrome (SIRS)
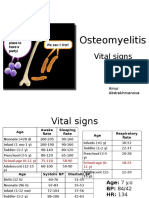
Temperature >38C or <36C
Heart beat >90/min.
Respiration >20/min. or PaCO2 <4,3 kPa or ventilated
Leukocytes >12000 cells/mm2 or <4000 cells/mm2 or
>10% juvenile Granulocytes
Society of Critical Care Medicine Consensus Conference 1992
If at least 2 of these criterias during 3 consecutive
days
Ertel W. et al., Unfallchirurg 1993
�SIRS - Definition
2 or more of the following 4 criteria:
Temperature:
>38.8C or <36.0C
Heart rate:
>90/min
Respiratory rate: >20/min or
PaCo2<32mmHg
PMNL:
>12.000/l or
<4000/l or
>10% juvenile PMNL
Hypoxia
Shock
Infection
Sepsis
SIRS Trauma
Hypotension
Burn
Injury
�Second
Second
Hit
Hit
First
First
Hit
Hit
Late
Late
MOF
MOF
vulnerable
Tissue inury
+ shock
SIRS
Recovery
Recovery
Can not resuscitate
Early
Early
MOF
MOF
Primary objectives:
Survival
Normal cognitive functions
Avoid sepsis
Best available function
�Killer
Exsanguinating hemorrhage
Tentorial herniation
Hypoxia
Sepsis
Primary survey
ATLS
Resuscitation
oxygenation, perfusion
Evaluation
vital functions?
Response ?
?
secondary survey
Life saving
surgery
Damage control
Bailout surgery
Scoring
ICU
Early total care
�Life saving surgery
1. Access to life support system
2. Decompression of cavities
3. Control of exsanguinating hemorrhage
massive hemothorax
hemoperitoneum
crushed pelvis
central amputation
�Damage control
The term Damage control is coined by
the US Navy and refers to keeping
afloat a badly damaged ship by
procedures to limit flooding, stabilize
the vessel, isolate fires and explosions
and avoid their spreading. These
measures permit damage assessment and
gain time to establish plans for
definitive salvage.
Rationale
Saving life by deferring
repair of anatomical
lesions and focussing on
restoring physiology.
�Definition
Rapid abbreviated laparotomy to
stop hemorrhage and peritoneal
soiling and staged sequential repair
after ongoing resuscitation and
recovery from hypothermia,
coagulopathy, and acidosis.
Stone HH, Strom PR, Mullins RJ.
Management of the major
coagulopathy with onset during
laparotomy.
Ann Surg 1983;197.532-535
1983
10
�Rotondo MF, Schwab CW, McGonigal
MD, Phillips,III GR, Fruchterman TM,
Kauder DR, Latenser BA, Angood PA.
Damage control: An approach for
improved survival in exsanguinating
penetrating abdominal injury.
J Trauma 1993;35:375-383
1993
Moore EE. Staged laparotomy for the
hypothermia, acidosis, and
coagulopathy syndrome.
Am J Surg 1996;172:405-410
1996
Moore EE, Burch JM, Franciose RJ,
OffnerPJ, Biffl WL. Staged
physiologic restoration and damage
control surgery.
World J Surg 1998;22:1184-1191
1998
11
�Damage control
BailoutBailout-procedure
procedure::
Aborted termination of surgery in a
patient at imminent risk of death.
Preemptive intervention:
intervention:
Calculated early decision to
accomplish definitive correction of
injuries in staged sequential
procedures.
Indications for Damage control
control surgery
1.Physiological criteria hypothermia,
coagulopathy, acidosis.
2.Complex pattern of severe injuries
expecting major blood loss and a
prolonged reconstructive procedure in
an unstable patient.
12
�Ancillary issues indicating benefits
of Damage control:
1.Limited experience of the surgical
team in complex injuries.
2.Limited resources in a mass
casualty.
3.Fatigued and overwhelmed surgical
team.
Cave: Over -utilisation of the concept
Selecting Damage control too
careless may mean an unnecessarily
premature termination of surgery in
patients who would otherwise have
recovered from a single definitive
procedure. It would subject the
patients to risks and expenses of
multiple surgical interventions.
13
�Damage
control
Control of
Damage
done by lazy,
lingering-surgeons !
The concept of Staging is today
widely accepted and applies to
emergent and scheduled
procedures in the abdomen, pelvis,
chest, and neck as well as
extremities. The judicious surgeon
who chooses this approach must no
longer fear the whispered loss of
his surgical manhood.
14
�Stage 1 - Patient selection for
abbreviated laparotomy
Hypothermia: < 34 C
Acidosis: pH < 7.2, Serum
Lactate > 5 mmol / L
Coagulopathy
Blood Pressure < 70 mm Hg
Transfusion approaching 15 Units
Injury Severity Score > 36
Combined vascular, solid and hollow organ
injury
Inaccessible major venous injury
Anticipated need for a time consuming
procedure
Demand for operative control of other
injuries
Inability to close the abdominal incision
Desire to reassess the intraabdominal
contents
15
�Stage 2 Operative control of
haemorrhage and contamination
Haemorrhage control:
Repair or ligation for accessible
blood vessels
Inflow-occlusion by cross- clamping
or balloon-tamponade
Packing: 4 quadrants, perihepatic
packing
Intravascular shunting or stenting
Contamination control:
Ligation, suture or stapling of
bowels
Resection of damaged segments
with clips, clamps, or staples
Anastomoses and stomas have to
be deferred
16
�Temporary abdominal closure:
Towel clips
Bogota Bag (temporary silo)
Opsite-Sandwich or Vacu-Seal
Mesh closure or Ethizip
Stage 3 Physiological
restoration in the ICU
Rewarming
Correction of coagulation
Correction of acidosis
Optimisation of oxygen delivery
Monitoring and avoidance of an
Abdominal Compartment Syndrome
17
�Stage 4 Return to OR for
definitive surgery
Physiological restoration
Removal of packs and definitive repair
Persisting bleeding
Increasing intraabdominal pressure
Scheduled reoperation after repacking
and entensive gut distension due to
reperfusion
Stage 5 Reconstruction of
abdominal wall
Direct closure only without gut
distension
After fascial retraction subsequent
gradual vacuum-assisted closure
Mesh repair
In an hostile abdomen: gauze packing,
secondary granulation and skin grafting
Secondary plastic reconstruction
18
�VACVAC
-Therapy and polytraumatized patients
19
�Bailout Damage Control
Chest
Abdomen
Pelvis
Extremities
Control of Hemorrhage
Packing
Source control
Dbridement
External fixator
V.A.C.- Vacuum Sealing
20
�Workhorse -Damage control
Pelvic ring fixation
Tamponade
True pelvis
Paracolic gutters
Ethizip + second look
21
�Rationale of Packing
Main source of bleeding:
venous plexus !
Stable pelvic ring:
Abutment for tamponade !
Packing pelvis and paracolic gutters
Abdominal wall remains open
Monitoring ACS
22
�Trauma
Abdomen 204
penetr.
71
blunt
133
Pelvis
Abdomen
+ Pelvis
Isolated /
Packing
Multiple
ACS
Survival
39/32
21/112
17 %
16 %
3%
5%
90 %
76 %
63
7/56
19 %
6%
80 %
44
0/44
25 %
9%
57 %
Ertel et al.: Crit Care Med 28: 1747, 2000
DC Injured Limbs
Dbridement, Fasciotomies
External fixator
Temporary intraluminal vascular shunts
Epigard, Vacuum-Sealing
23
�Safe conditions: Early total care
Stable hemodynamics
No need for vasoactive/
inotropic stimulation
No hypoxemia, no hypercapnia
Lactate < 2 mmol/L
Normal coagulation
Normothermia
Urinary output > 1 mL/kg/hour
Physiological status Surgical intervention Timing
Response to
resuscitation:
Life saving surgery
?
"Damage control"
Early total care
Hyper-inflammation
"Window of
opportunity"
"Second look", only!
Scheduled definitive
surgery
Immunosuppression
No surgery!
Recovery
Secondary reconstructive
surgery
Day 1
Day 2-3
Day 5-10
Week 3
24
�Shock
Definition
Reduced tissue perfusion leading to
generalized cellular hypoxia with a
persistent discrepancy between
delivery and consumption of oxygen.
25
�Oxygen delivery
Intracellular ATP
Cell dysfunction
Cell death
reversible
irreversible
Trauma specific forms
Hemorrhagic shock
Cardiogenic shock
Spinal shock
Hemorrhagic shock and tissue injury
Traumatic-Hemorrhagic
Traumatic-Hemorrhagic shock
shock
26
�Pathophysiological
alterations
Loss of fluid
Pump failure
Decreased vascular
resistance
Hemorrhagic shock
Symptoms
Symptoms
Tachycardia
Late symptoms in
young patients !!
Hypotension
Central venous pressure
Hemoglobin
Not occurring in early
posttraumatic period !!
27
�TraumaticHemorrhagic shock
Blood
Blood loss
loss
<10%
complete compensation
10% - 25%
cardiac output
>25%
arterial blood pressure
Trauma-Cardiogenic
shock
Tension pneumothorax
Myocardial contusion
Cardiac tamponade
Vena caval obstruction
28
�Cardiogenic shock
Symptoms
Symptoms
Hypotension
Tachycardia
Arrhythmia
Central venous pressure
Paradoxic pulse
Spinal shock
Symptoms
Symptoms
Hypotension
Pulse normal or decreased
Pulse feels strong
Skin dry and warm
29
�Emergency treatment
Correction of oxygen availability
Fluid
Fluid replacement
replacement
Ventilation
Ventilation therapy
therapy
Vasoconstrictive
Vasoconstrictive and
and
cardiotropic
cardiotropic agents
agents
O2av = CO x O 2sat. x Hbconc. x 1.34
(mL/min) (mL/min) (%)
(g%)
1000 = 5.250 x 95
x 15
x 1.34
300 = 3.500 x 64
x 10
x 1.34
Oxygen debt !
Nunn JF, FreemanJ. Anaesthesia 1964;19:206
30
�Alimentation
31
�Disease Process
Change in
Metabolic
Activity (%)
100
50
50% Burn
20% Burn,
Infection,
Multiple Trauma
Long Bone Fracture
Normal
Postoperative
Flow phase
The body tries
to maximize gluconeogenesis
from all available sources !
32
�Glucose the
sole source for energy
PMNL
RBC
Renal medulla
Bone marrow
RES
Neurons
Acute Nonstress Fasting Metabolism
Free Fatty
Acids
Fat
Fat
Source
Source
Triglyceride
Ketosis
Ketosis
Liver
Liver
Ketone
Bodies
Nonpreferred
Nonpreferred
Glucose
Glucose
Users
Users
(eg.
(eg. kidney,
kidney,
heart,
heart,
muscle
muscle
Glycogen
Glycogen
Glycerol
Lean
Lean Body
Body
Mass
Mass
Amino
Amino Acid
Acid
Stores
Stores
Amino
Acids
GluconeoGluconeogenesis
genesis
Urinary
Nitrogen
Lactate
Lactate
Glucose
Preferred
Preferred
Glucose
Glucose
Users
Users
(eg.
(eg. Brain,
Brain,
RBC)
RBC)
33
�Muscle catabolism
Aminoacids:
substrate for gluconeogenesis
in the liver
Byproduct urea:
increased level of urinary urea
nitrogen
Early enteral nutrition
Gut access distal to the pylorus
Gastric suction tube
Transpyloric feeding tube
(Gastroscopic guidance)
34
�Rhabdomyolysis
Rhabdomyolysis
Metabolic disturbances
acute renal failure (ARF)
35
�Muscle injury
Trauma-mechanical/thermal
I/R-injury
Crush
Seizure
Drug abuse
Malignant hyperthermia
Symptoms
Cramping pain
Progressive weakness
(calves / lower back)
Discoloration of urine
36
�Release
Purines (uric acid)
Sulfur-containing protein+hydrogen
(anion gap acidosis)
Creatine (creatinine+BUN)
Myglobine
Release
Aldolase
LDH
sGOT
Creatine-Kinase (CK)
CK-MB (7%)
37
�Myoglobine
Not highly protein bound
Filtered at the glomeruli
50 g/L color visible in water
>100 mg/L color visible in urine
Serum concentrations >>>25 mg/L
>25 mg/L hemolysis
Plugging of renal tubuli
Low urine flow
Acidosis
Sludge or urate crystals and
ferrihemate (pH < 5.6)
Myoglobine converted to
ferrihemate
toxic and precipitation
38
�Muscle cell lysis
Influx:
Efflux:
sodium + calcium
fluid
potassium + phosphate
Electrolyte
Electrolyte ++ fluid
fluid shifts
shifts
Severe
Severe hypovolemia
hypovolemia
Rhabdomyolysis
>>>ARF in 30 %
Hypovolemia
Free oxygen radicals
Plugging of renal rubuli
39
�Therapy
Fluid resuscitation
Bicarbonate
(urine pH 8.0, serum pH 7.45)
Mannitol 25 g / every 6 hrs.
Furosemid 40 - 200 mg
CVVH (pump)
Compartment
Compartment Syndrome
Syndrome
and
and
Abdominal
Abdominal Compartment
Compartment
Syndrome
Syndrome
40
�Compartment Syndrome
Raised pressure
Within a closed space
Causing damage to its
contents
Due to decreased capillary
blood flow
Precondition
Ischemia-Reperfusion-Injury
Posttraumatic edema
Low MAP
41
�Clinical Diagnosis
Unrelenting pain
Swollen, tense compartment
Painful muscle stretch
Sensory deficit
Muscle weakness
BUT:
BUT: Palpable
Palpable pulses
pulses !!
CPP = MAP - ICP
Critical Treshhold:
CPP <30 mmHg (4 kPa)
ICP >30-40 mmHg (5.3 kPa)
42
�I
S
C
H
M
E
I
A
ATP
Edema
Microvascular
Injury
ATP-break-down
Xanthine
Dehydrogenase
OH-.
Fe2+
Conversion
Hypoxanthine
Xanthine
Xanthine
Oxidase
H2O2
O2-.
O2
Uric Acid
REPERFUSION
Trauma
Ischemia
Histamine
C3a / C5a
X.D.
Reperfusion
Hypoxanthine
Xanthine
O2
Xanthine Oxidase
Uric
Acid
O2.OH-.
Microvascular
Injury
43
�Abdominal cavity own compartment !!
Intraabdominal increase of volume
Intraabdominal pressure
Risk factors for ACS
2 or more criteria:
Combined abdominal and pelvic
trauma
severe hemorrhagic shock
Abdominal packing
Primary abdominal closure
44
�Pathophysiology of increased
abdominal pressure
Cardiopulmonary:
Thoracic pressure
Venous reflow
Preload
Systemic afterload
Cardiac output
Cardiac index
Diagnosis of ACS
Ventilation pressure >35mbar and
Horowitz-quotient
(PaO2/FIO2 )
>20kPa
Urinary output <30ml / hr
Clinically tense abdomen
Bladder pressure >25 mmHg
improvement after decompression
45
�Therapy
Decompression !
Ethizip
Secondary abdominal closure
Summary
Abdominal
Abdominal Compartment
Compartment Syndrome
Syndrome after
after
severe
severe abdominal
abdominal and
and pelvic
pelvic trauma:
trauma:
Incidence: 4.4 %
After tamponade: 8%
Organ failure: spleen 100%,
hemodynamics: 86%
Therapy: emergency decompression
Complications: intestinal ischemia
46
�Conclusion
Monitoring of bladder pressure
Monitoring of organ functions
Secondary abdominal closure after
emergency laparotomy with
tamponade
Traumatic brain injury
47
�Severe brain injury
Avoid secondary brain damage
Hypotension
Hypotension // hypoxemia
hypoxemia
Evacuation
Evacuation of
of intracerebral
intracerebral hemmorrhage
hemmorrhage
Early
Early fracture
fracture fixation
fixation
Fracture reconstruction: Window of opportunity
Chesnut et al. (1993): Traumatic
Coma Database
Secondary Insults
5-4
2-1
307
64
17
Early
30
40
47
Late
117
20
66
Early and late
39
15
77
No hypotension
SBP <90 mmHg
GOS %
48
�Brain injury with multiple trauma
1.
Control of shocking hemorrhage
Oxygenation
2.
CNS assessment
Evacuation of EDH / SDH
ICP / pti O2 monitoring
Brain protection
3.
Fixation of major fractures for unrestricted IC
Damage control
Reduction of afferent input
Stress
Stress
Fear
Fear
Pain
Pain
Endotoxin
Endotoxin
Temperature
Temperature
Cortex
Cortex
Hypothalamus
Hypothalamus
Pituitary
Pituitary
Blood
Blood volume
volume
Fluid
shifts
Fluid shifts
Hypoxemia
Hypoxemia
Hypercapnia
Hypercapnia
Acidosis
Acidosis
Receptors
Receptors
Brain
Brain stem
stem
Autonomic
Autonomic
centers
centers
Tissue
Tissue injury
injury
49
�ICP - therapy
CBV
BWC
CSF
steal
Therapy ICP > 15 mm Hg
No hemorrhage to evacuate
Normoventilation
Maintenance of CPP (CPP=MAP-ICP)
Optimization of sedation and relaxation
Drainage of liquor
Mannitol
Hyperventilation
Pentothal (Barbiturate)
50
�Klassifikation SHT
Wach
Somnolent
Sopors
Komats
Symptomatik
1)
1) Psychopathologisches
Psychopathologisches Syndrom
Syndrom
Vigilanzstrung
Somnolenz
Sopor
Bewusstlosigkeit (Koma)
akustisch weckbar
Abwehr auf Schmerz
unerweckbar
cave: Abwehr auf Sz
kann erhalten sein
Orientierungsstrung
Gedchtnisstrung
Durchgangssyndrom
51
�Symptomatik
2)
2) Neurologische
Neurologische Ausflle
Ausflle
Pupillenstrung (Weite und Lichtreaktion)
Reflexstatus
Motorik
Sensibilitt
Muskeltonus
Symptomatik
3)
3) Vegetatives
Vegetatives Syndrom
Syndrom
Schwindel
Brechreiz
Kreislaufinstabilitt
Strung der Wrmeregulation
52