Professional Documents
Culture Documents
420 Full
Uploaded by
ccOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
420 Full
Uploaded by
ccCopyright:
Available Formats
BRIEF REPORT
Response to Therapy Following
Retreatment of Serofast Early
Syphilis Patients With Benzathine
Penicillin
(HIV)negative patients with early syphilis remained serofast
6 months after treatment [4]. We conducted additional analyses of data from this trial to determine the serological response
of serofast patients after retreatment.
METHODS
Arlene C. Sea,1 Mark Wolff,2 Frieda Behets,1,3 Kathleen Van Damme,3
David H. Martin,4 Peter Leone,1 Linda McNeil,5 and Edward W. Hook6
1
Persistent nontreponemal titers after treatment are common
among patients with early syphilis. We retreated 82 human
immunodeciency virusnegative early syphilis participants
who were serofast at 6 months using benzathine penicillin.
Only 27% exhibited serological response after retreatment
and after an additional 6 months of follow-up.
Keywords.
response.
syphilis;
serofast;
retreatment;
serological
Early syphilologists noted that the effective treatment of early
syphilis is one of the critical medical problems of modern times
[1]. A continuing challenge to determining the response to treatment of early syphilis is exemplied by the substantial proportion of patients who fail to achieve serological cure and remain
serofast, dened as a <4-fold (2 dilution) decline in nontreponemal antibody titers at 612 months or as persistently low titers
after treatment [2, 3]. Although retreatment is recommended for
serofast patients if follow-up cannot be ensured, optimal management remains uncertain due to the paucity of data regarding
serological response to retreatment and long-term outcomes.
We report results from a randomized, controlled clinical
trial in which 21% of human immunodeciency virus
Received 10 July 2012; accepted 15 October 2012; electronically published 1 November
2012.
Correspondence: Arlene C. Sea, MD, MPH, University of North Carolina at Chapel Hill,
Division of Infectious Diseases, CB 7030, 130 Mason Farm Rd, Chapel Hill, NC 27599 (idrod@
med.unc.edu.)
Clinical Infectious Diseases 2013;56(3):42022
The Author 2012. Published by Oxford University Press on behalf of the Infectious Diseases
Society of America. All rights reserved. For Permissions, please e-mail: journals.permissions@
oup.com.
DOI: 10.1093/cid/cis918
420
CID 2013:56 (1 February)
BRIEF REPORT
Our randomized, controlled trial was conducted from June
2000 to March 2009 in North America and Madagascar
and involved HIV-negative patients 18 years with early syphilis [4, 5]. The master protocol was approved by the University
of Alabama at Birmingham (UAB) Institutional Review Board
(IRB) and by IRBs serving each study site.
Eligibility criteria, procedures for enrollment and follow-up,
and denitions for primary and secondary were previously described [4, 5]. Participants were diagnosed with early latent
(EL) syphilis based on either a nonreactive syphilis serology or
documented exposure to a sexual partner with primary or secondary syphilis within the preceding 12 months. All participants were required to have reactive rapid plasma reagin
(RPR) antibody tests at enrollment. Participants without penicillin (PCN) allergy received initial treatment with 2.4 million
units of intramuscular (IM) benzathine PCN or 2.0 g azithromycin (AZM) orally as directly observed therapy. RPR titers at
the baseline visit prior to therapy and at the 6- and 12-month
visits were performed at the UAB central laboratory according
to standards [6].
Serological cure at 6 months following therapy was dened
as either a negative RPR or 4-fold (2 dilution) decrease in
titer. Seroreversion was dened as becoming RPR negative
after therapy. Serofast status was dened as either no change
in RPR titer or a 2-fold (1 dilution) decrease or increase in
titer following initial therapy or retreatment. Per protocol, all
participants determined to be serofast at 6 months after initial
treatment with PCN or AZM were retreated with 1 dose of 2.4
million units of benzathine PCN IM at the 6-month visit.
These analyses were performed on the subset of the original
per-protocol cohort who were serofast at 6 months after initial
therapy, received retreatment, and had serological data at the
12-month visit. Proportions of participants with seroreversion,
serological cure, or serofast status after retreatment were determined at 12 months using the denitions above. Participants
who achieved serological cure after retreatment and those who
remained serofast were compared for age and baseline and 6month RPR titers using a Wilcoxon 2-sample test, and were
Downloaded from http://cid.oxfordjournals.org/ by guest on August 25, 2014
Division of Infectious Diseases, Department of Medicine, University of North
Carolina at Chapel Hill; 2EMMES Corporation, Rockville, Maryland; 3Department of
Epidemiology, University of North Carolina at Madagascar, Antananarivo;
4
Department of Medicine, Louisiana State University, New Orleans; 5FHI 360,
Research Triangle Park, North Carolina; and 6Division of Infectious Diseases,
Department of Medicine, University of Alabama at Birmingham
compared for gender, geometric mean RPR titers, initial treatment regimen, and stage using a chi-square test.
RESULTS
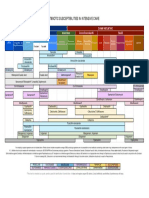
Table 1. Characteristics and Serological Outcomes of Serofast
Patients With Early Syphilis Retreated With Benzathine Penicillin
Outcome at 12 Months After
Initial Treatment (ie, 6 Months
After Retreatment)
Characteristic
Gender (n, % male)
Age (25th, 50th, and
75th percentiles)
RPR titers (25th, 50th,
and 75th percentiles)
Baseline
6 months
Seroreversion/Cure
(n = 22)
Serofast
(n = 60)
13, 59%
23, 25, 36
32, 53%
23, 30, 36
1:16, 1:32, 1:128
1:4, 1:8, 1:32*
1:16, 1:32, 1:64
1:4, 1:8, 1:16**
RPR titers (geometric
mean titer [95% CI])
Baseline
34 (19, 62)
10 (8, 14)***
26 (13, 52)
8 (6, 11)****
Primary
5, 23%
9, 15%
Secondary
Early latent
6, 27%
11, 50%
19, 32%
32, 53%
12, 55%
10, 46%
29, 48%
31, 52%
6 months
Syphilis stage (n, %)
Initial treatment (n, %)
Penicillin
Azithromycin
Abbreviations: CI, confidence interval; RPR, rapid plasma regain.
Wilcoxon 2-sample test: *P = .0004; **P = .001. T test: ***P = .0002;
****P = .0005.
DISCUSSION
Despite retreatment with 2.4 million units benzathine PCN,
73% of patients with early syphilis who failed to achieve serological cure at 6 months after initial therapy remained serofast
at 12 months. Patients with early syphilis who had higher
nontreponemal titers at baseline and at 6 months (1:32)
were more likely to exhibit serological cure after retreatment
than those with lower titers. Among the patients who were serofast at 6 months, only a small proportion exhibited seroreversion after retreatment. Our ndings illustrate the minimal
improvement in serological response among serofast patients
retreated with a single dose of PCN, especially those with
lower RPR titers (1:16) at baseline or prior to retreatment.
Assessing the biological signicance of the serofast state is
difcult; stable nontreponemal antibody titers following
therapy could represent persistent low-level infection with
Treponema pallidum, variability of host response to infection,
or possibly other confounding nontreponemal inammatory
conditions in the host. Nontreponemal tests measure immunoglobulin M (IgM) and IgG antibodies to T. pallidum and
potentially to lipoidal and cardiolipin material released from
damaged host cells during syphilis infection, which may also
result from other illnesses that can produce tissue damage [7].
Although nontreponemal antibody titers generally correlate
with syphilitic stage/disease activity [3], the implications of
high titers (eg, 1:32) vs low titers in the serofast state are
unknown. However, consistent with our previous analyses [4],
these ndings suggest that higher nontreponemal titers at
retreatment are associated with a higher probability of serological response to therapy.
Clinical management of patients who remain serofast after
treatment or retreatment for early syphilis is challenging.
Treatment failure, which is usually dened as a sustained
BRIEF REPORT
CID 2013:56 (1 February)
421
Downloaded from http://cid.oxfordjournals.org/ by guest on August 25, 2014
We identied 82 HIV-negative adults with early syphilis who
were serofast at 6 months after initial treatment with benzathine PCN (n = 41) or AZM (n = 41). Their median age was
29 years (range, 1847), and most were male (55%), heterosexual (95%), and of Malagasy (88%) origin. Fourteen (17%) serofast participants had primary syphilis, 25 (31%) had
secondary syphilis, and 43 (52%) had EL syphilis. At 6
months after initial treatment, the modal RPR titer among the
82 participants was 1:16 (n = 19, 23%), with a range from 1:1
to 1:1024.
After retreatment with benzathine PCN, only 11 (13%) participants exhibited a 4-fold decline in RPR titers from their
6-month titers, and 71 (87%) remained serofast at 12 months
(P < .0001). However, when serological response was determined relative to baseline titers before initial treatment, 22
(27%) participants had achieved serological cure and 60 (73%)
were serofast (P < .0001). Of those with serological response
following retreatment, only 2 had seroreversion to a nonreactive RPR at the 12-month follow-up.
Gender, age, stage of syphilis, and initial treatment regimen
were not associated with likelihood of achieving serological
cure after retreatment (Table 1). However, there were statistically signicant differences in the baseline and 6-month RPR
titers between patients with serological cure vs serofast status.
The median baseline RPR titer among the former was 1:32
compared with the median baseline titer of 1:8 among serofast
patients (P < .01). There were similar differences in RPR titers
at the 6-month visit between groups; participants with serological cure had a higher median RPR titer prior to retreatment than did participants who remained serofast at 12
months (Table 1). Furthermore, geometric mean RPR titers
were signicantly different between patients with serological
cure vs serofast status at baseline and at 6 months (Table 1).
422
CID 2013:56 (1 February)
BRIEF REPORT
addressing the unresolved questions about the serofast state
and its management. At present, the management of individual serofast patients will continue to require clinical judgment,
consideration of nontreponemal antibody titers, underlying
medical conditions such as HIV infection, and/or the likelihood that the patient will return for subsequent serological
monitoring after treatment.
Notes
Acknowledgments. We gratefully acknowledge the following: the Sexually Transmitted Infections Clinical Trials Group Executive Committee;
the Sexually Transmitted Diseases Clinical Trials Unit Executive Committee; the Data Safety and Monitoring Board; research staff at Family Health
International, Indiana University School of Medicine, Louisiana State University, University of Alabama at Birmingham/Jefferson County Department of Health, University of North Carolina at Chapel Hill, and
University of North Carolina-Madagascar; and Jamie Winestone and Meredyth Gehrig of EMMES Corporation.
Financial support. This work was supported by the National Institute
of Allergy and Infectious Diseases through contracts N01 A1 75329 (STD
Clinical Trials Unit, Myron Cohen, MD, PI) and HHSN 26620040073C
(STI Clinical Trials Group, Edward W. Hook, III, MD, PI).
Potential Conicts of interest. P. L. has received research funding
from GlaxoSmithKline, Abbott Diagnostics, and Novartis and is a
member of the speakers bureaus for GlaxoSmithKline and Abbott
Diagnostics. E. W. H. has been a consultant for Cempra; has received research funding from Becton-Dickinson, Cepheid, Roche Molecular, Genprobe, Inc., and Cempra; and has been on the speakers bureau for BectonDickinson. All other authors report no potential conicts.
All authors have submitted the ICMJE Form for Disclosure of Potential
Conicts of Interest. Conicts that the editors consider relevant to the
content of the manuscript have been disclosed.
References
1. Moore JE. The modern treatment of syphilis. 2nd ed. Baltimore, Maryland: Charles C Thomas Books, 1941.
2. Rolfs RT, Joesoef MR, Hendershot EF, et al. A randomized trial of enhanced therapy for early syphilis in patients with and without human
immunodeciency virus infection. The Syphilis and HIV Study Group.
N Engl J Med 1997; 337:30714.
3. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2010. Morb Mort Wkly Rep 2010; 59/RR12:2630.
4. Sea AC, Wolff M, Martin DH, et al. Predictors of serological cure and
the serofast state after treatment in HIV-negative persons with early
syphilis. Clin Infect Dis 2011; 53:10929.
5. Hook EW, Behets F, van Damm K, et al. A phase III equivalence trial
of azithromycin vs benzathine penicillin for treatment of early syphilis.
J Infect Dis 2010; 201:172935.
6. Stoner BP. Current controversies in the management of adult syphilis.
Clin Infect Dis 2007; 44:S13046.
7. Larsen SA, Pope V, Johnson RE, Kennedy EJ Jr. A manual of tests for
syphilis. Washington, DC: American Public Health Association, 1998.
Downloaded from http://cid.oxfordjournals.org/ by guest on August 25, 2014
4-fold increase in nontreponemal titers after therapy, is considered to be an indication for cerebrospinal uid (CSF) examination for T. pallidum involvement [3]. However, some
experts also recommend CSF examination for patients who do
not demonstrate serological response after treatment (4-fold
decrease in nontreponemal test titer or sustained seroreversion
occurring within 6 months of treatment) [6]. Following these
recommendations, 60 participants (13% of the 465 participants in the original study) [4] who remained serofast despite
retreatment would have been considered for lumbar puncture
to rule out neurosyphilis.
Our study provides the rst evaluation of serological outcomes following retreatment of participants with the syphilis
serofast state. However, we provided only 1 dose of benzathine
PCN for retreatment, although the recommended therapy for
patients with suspected treatment failure is 2.4 million units of
benzathine PCN weekly for 3 weeks unless neurosyphilis is
present [3]. We had a modest sample size of persons who received retreatment, and we did not conduct CSF examinations
of serofast patients at the 12-month visit. However, none of
the participants available for follow-up exhibited symptoms
suggestive of neurosyphilis during the study period. Only 23
of our participants who were serofast at 12 months returned
for additional follow-up at 18 and 24 months after initial
treatment, which limited further analysis. Long-term outcomes after retreatment require further investigation, as does
the applicability of our observations to persons with syphilis
and HIV co-infection. Another limitation of our data is the
lack of a comparison group by which to determine the expected decline in nontreponemal titers among serofast patients in
the absence of retreatment. Thus, we cannot rule out that the
seroreversion/serological cure exhibited by 24% of our participants may have been due to the natural decline in RPR titers
after initial therapy, rather than due to the additional dose of
benzathine PCN.
Prior to our study, there had been no evidence that patients
who fail to exhibit an appropriate 4-fold decline in titers
should receive additional courses of therapy for syphilis,
though this is often done in clinical practice. Our results
suggest that the incremental benet of retreating HIV-negative
serofast patients with early syphilis is marginal, considering
the 1:3 ratio of serological response to serofast state at followup despite retreatment. Further, prospectively designed studies
are needed; and our ndings provide a starting point for
You might also like
- Guidelines For The Interpretation of The Neonatal ElectrocardiogramDocument16 pagesGuidelines For The Interpretation of The Neonatal ElectrocardiogramccNo ratings yet
- Daftar Pustaka Aaakkk!!! PrintDocument2 pagesDaftar Pustaka Aaakkk!!! PrintccNo ratings yet
- 420 FullDocument43 pages420 FullccNo ratings yet
- 420 FullDocument43 pages420 FullccNo ratings yet
- 420 FullDocument3 pages420 FullccNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Integumentary System: Skin ProblemsDocument11 pagesIntegumentary System: Skin ProblemsHaru MatsubuchiNo ratings yet
- TYPHIDOT IgG - IgM - ICTDocument1 pageTYPHIDOT IgG - IgM - ICTAlveera Zafar100% (1)
- Scale For Ranking Health Conditions and Problems According To PrioritiesDocument9 pagesScale For Ranking Health Conditions and Problems According To Prioritiescnvfiguracion100% (1)
- 2017 WHO TRS 1004 Biological StandardizationDocument616 pages2017 WHO TRS 1004 Biological StandardizationMohamad IsmailNo ratings yet
- Chikungunya VirusDocument13 pagesChikungunya VirusiuliualbescuNo ratings yet
- Randy C Ploetz - Diseases of Tropical Fruit Crops-CABI (2003) - 58-94Document37 pagesRandy C Ploetz - Diseases of Tropical Fruit Crops-CABI (2003) - 58-94Kres DahanaNo ratings yet
- Bacteriology - Semifinals - Neisseria and MoraxellaDocument10 pagesBacteriology - Semifinals - Neisseria and MoraxellaUshuaia Ira Marie L. GallaronNo ratings yet
- Module 3Document3 pagesModule 3Leah LlobellNo ratings yet
- VirologyDocument129 pagesVirologyAmoako KingsleyNo ratings yet
- Emerging & Reemerging InfectionsDocument18 pagesEmerging & Reemerging InfectionsBiManda Rizki NurhidayatNo ratings yet
- MMWR HiB PDFDocument20 pagesMMWR HiB PDFworksheetbookNo ratings yet
- Introduction To VirusesDocument64 pagesIntroduction To Virusesyudith novidaNo ratings yet
- Biocontrol Science and TechnologyDocument22 pagesBiocontrol Science and TechnologyDaniFierroNo ratings yet
- Standard Operating Procedures For Blood Bank Processes in PakistanDocument204 pagesStandard Operating Procedures For Blood Bank Processes in PakistanMohamed Elmasry100% (4)
- TRS 910 Annex2-WHO Revision of The WHO Recommendations For The Production and Control of IPVDocument28 pagesTRS 910 Annex2-WHO Revision of The WHO Recommendations For The Production and Control of IPVaprilmm419No ratings yet
- Specimen Collection and ProcessingDocument19 pagesSpecimen Collection and ProcessingFirman Setiawan Moehan100% (2)
- Infectious Disease Questions 1Document36 pagesInfectious Disease Questions 1Jelly BeansNo ratings yet
- ENGERIX B LeafletDocument50 pagesENGERIX B LeafletEllaNo ratings yet
- Community Guide To Good Practice For Hygiene and The Application of The HACCP Principles in The Production of Natural Sausage CasingsDocument53 pagesCommunity Guide To Good Practice For Hygiene and The Application of The HACCP Principles in The Production of Natural Sausage CasingsEmanuele BelleiNo ratings yet
- Micro Ch4 Physical ControlDocument95 pagesMicro Ch4 Physical ControlBernadette Joyce PascualNo ratings yet
- Community Health Nursing II NotesDocument11 pagesCommunity Health Nursing II NotesMarjorie UmipigNo ratings yet
- Ophthalmology PDFDocument28 pagesOphthalmology PDFKukuh Rizwido PrasetyoNo ratings yet
- Laboratory Exercise No. 6 Identification and Classification of Crop Pest Based On Morphological Traits and Damage Characteristics WorksheetDocument5 pagesLaboratory Exercise No. 6 Identification and Classification of Crop Pest Based On Morphological Traits and Damage Characteristics WorksheetmmabejarNo ratings yet
- Antibiotic Susceptibilities in Intensive Care: Gram Positive Gram NegativeDocument1 pageAntibiotic Susceptibilities in Intensive Care: Gram Positive Gram NegativeFaisal Reza AdiebNo ratings yet
- Palmoplantar PustulosisDocument6 pagesPalmoplantar PustulosisputraimanullahNo ratings yet
- CD Post Test 100 AprilDocument11 pagesCD Post Test 100 AprilMei JoyNo ratings yet
- Infectious Disease in An Era of GlobalDocument13 pagesInfectious Disease in An Era of Globalsebastian herreraNo ratings yet
- Grade - 5 3RD Quarter ExaminationDocument7 pagesGrade - 5 3RD Quarter ExaminationStephanie Shane ArellanoNo ratings yet
- Can I Take Neozep Without EatingDocument1 pageCan I Take Neozep Without EatingEij AnnNo ratings yet
- Cannabis Based Pesticides 2018Document13 pagesCannabis Based Pesticides 2018richard.schumacherNo ratings yet