Professional Documents
Culture Documents
Incidence and outcome of congenital CMV in preterm and full-term neonates
Uploaded by
Minerva StanciuOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Incidence and outcome of congenital CMV in preterm and full-term neonates
Uploaded by
Minerva StanciuCopyright:
Available Formats
in vivo 18: 819-824 (2004)
Incidence and Outcome of Congenital Cytomegalovirus
Infection in Selected Groups of Preterm and Full-term
Neonates Under Intensive Care
ARANKA NAGY1, EMKE ENDREFFY1, KROLY STREITMAN1,
SNDOR PINTR1 and ROZLIA PUSZTAI2
1Department
of Paediatrics and 2Department of Medical Microbiology and Immunobiology, Faculty of Medicine,
Albert Szent-Gyrgyi Medical and Pharmaceutical Centre, University of Szeged, Hungary
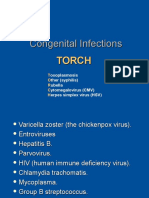
Abstract. Congenital cytomegalovirus (CMV) infection is
the leading cause of mental retardation and hearing
impairment. Examination for the presence of CMV infection
was carried out in a selected population of 70 neonates.
Urine samples were tested for CMV by means of a nested
polymerase chain reaction. CMV was detected in 6 (16.7%)
of the 36 preterm newborns and in 5 (14.7%) of the 34 fullterm newborns. One preterm neonate died and the remaining
10 newborns were followed up. Two children born at full-term
did not excrete CMV at 2 years of age and were symptomfree. Of 8 CMV-excreting children (5 preterm and 3 fullterm), 2 were symptom-free (1 preterm and 1 term).
Symptomatic CMV disease developed in 6 children (4
preterm and 2 full-term), with mental retardation (n=4),
hearing loss (n=1), strabismus (n=2) or bronchial asthma
(n=1). Screening of such neonates is important; those
identified as congenitally CMV-infected can be monitored to
correct any sequelae immediately.
Human cytomegalovirus (CMV) is one of the eight
members of the Herpesviridae family. It is a doublestranded DNA virus that is restricted to humans. Epithelial
cells, endothelial cells and fibroblasts are the major targets
of CMV infection in vivo (1). In some instances, neurones
in the brain and retina, smooth muscle cells in the
gastrointestinal tract and hepatocytes can also be infected.
In the peripheral blood, the circulating leukocytes are
susceptible to CMV. In vitro, the virus replicates well only
Correspondence to: Rozlia Pusztai, Department of Medical
Microbiology and Immunobiology, University of Szeged, H-6720
Szeged, Dm tr 10, Hungary. Tel: 36-62-546112, Fax: 36-62545113, e-mail: pusztai@comser.szote.u-szeged.hu
Key Words: Cytomegalovirus, congenital infection, preterm
neonates, full-term neonates, intensive care.
0258-851X/2004 $2.00+.40
in human fibroblasts. CMV displays many of the
characteristics of the herpesvirus family, such as the ability
to cause primary infection, then evolve into a latent state
and subsequently undergo reactivation.
CMV is the most common pathogen of intrauterine
infections, affecting an estimated 1-2% of all live births.
However, the incidence of congenital infection among
different populations is quite variable (2). Maternal primary
CMV infection occurs in approximately 0.7% to 4% and is
usually asymptomatic. Subsequent vertical transmission to
the foetus has been demonstrated at rates of 24% to 75%
(2-4). The usual clinical manifestations of congenital
infection are intrauterine growth retardation (IUGR),
microcephaly, ventriculomegaly, intracranial calcification,
chorioretinitis, hepatosplenomegaly, jaundice, petechiae,
thrombocytopenia and elevated serum transaminase levels
(5). The seriously ill babies have a mortality rate of
approximately 30% (6,7). The most common long-term
sequelae in infancy and childhood are sensorineural hearing
deficits and learning disabilities. Many infants, who appear
normal at birth, will manifest a hearing loss and other
delayed neurological complications. A progressive
sensorineural hearing loss may develop in 13-15% of
asymptomatic newborns (8).
A substantial proportion of congenital CMV infections
occur in women with preconceptional immunity (9-11). A
majority of infants with congenital CMV, who are born to
women with preconceptional immunity acquire the virus as
a result of recurrent maternal infection: reactivation of
endogenous virus or reinfection with a new strain of CMV.
A number of studies have suggested that symptoms and
permanent neurological deficits are rare in the infants of
women with preconceptional immunity (3,4). However, such
a clinical outcome may, in fact, be more common than
previously thought (12-15).
In the present study, the incidence, clinical spectrum and
outcome of congenital CMV infection were investigated
819
in vivo 18: 819-824 (2004)
among preterm and full-term newborns under intensive care
with suspected intrauterine infection. Paediatric, otologic,
ophthalmologic and neurological follow-ups were scheduled
for 1 to 4 years.
Table I. Clinical features in 11 newborn infants with congenital CMV
infection.
Infant Apgar scores at
1, 5 and 10 min
pH
Materials and Methods
1
2
3
4
5
6
7
8
9
10
11
7.17
7.20
7.10
7.23
7.20
7.12
7.30
7.32
7.22
7.52
7.26
Patients. Seventy newborns aged less than 2 weeks were admitted
to the Intensive Care Unit of the Department of Paediatrics,
University of Szeged, Hungary, with suspected intrauterine
infection (gestational age 25-40 weeks, weight 750-4500 g). Virus
infection was suspected in consequence of the detection of an
abnormality such as IUGR, non-immune hydrops foetalis (NIHF),
ascites, hydrothorax, congenital malformation, sepsis, hyperbilirubinaemia, seizure or pneumonitis. Clinical information was
obtained by review of the medical records of each subject. All
neonates with proven congenital CMV infection were followed-up
by the same paediatrician, ocular specialist, otologist and
neurologist. They were examined 2 weeks after birth and once or
twice annually up to 1-4 years of age.
The control group comprised 50 infants at no risk of foetal
CMV transmission.
The present study was approved by the Human Investigation
Review Board of the University of Szeged.
Detection of CMV in urine. Urine samples were collected from the
neonates in sterile urine-collecting bags within the first 2 weeks of
life, aliquoted into Eppendorf tubes and stored at -70C until
processed. CMV DNA was extracted from 200 l of the urine
sample by using the High Pure Viral Nucleic Acid Kit (Roche
Diagnostics GmbH, Mannheim, Germany) according to the
manufacturers instructions. Briefly, cell and virus lysis was
performed by incubation of the samples in a lysis/binding buffer
with proteinase K, and poly(A) carrier RNA and CMV DNA were
selectively bound to a glass fleece by centrifugation. Residual
impurities were removed in washing steps and the bound crude
CMV DNA was eluted in 50 l of nuclease-free sterile water. The
viral DNA target sequences derived from the envelope
glycoprotein B (gB) were amplified by nested polymerase chain
reaction (nPCR). The outer primer pair consisted of
oligonucleotide 5-GGA AAC GTG TCC GTC TTT GA-3 (gB
1246) and 5-GAG TAG CAG CGT CCT GGC GA-3 (gB 1724).
The inner primer pair consisted of the sense primer 5-TGG AAC
TGG AAC GTT TGG C-3 (gB 1319) and the antisense primer 5GAA ACG CGC GGC AAT CGG-3 (gB 1604).
Amplification was carried out in a final volume of 50 l
containing 50 pmol of primers, 200 M dNTPs (each), 1.5 mM
MgCl2 and 1.25 Units of Taq DNA polymerase in 50 mM KCl, 10 mM
Tris-HCl (pH 9.0), 0.1% Triton X-100 reaction buffer. Five l
aliquots of the crude DNA preparations were added to the first
PCR, and 3 ml aliquots from the previous PCR to the second one.
The thermal cycling profile was as follows: denaturation for 5 min
at 95C, 35 cycles of amplification (95C for 30 sec, 55C for 40
sec and 72C for 60 sec) and then holding at 72C for 10 min. A
positive control with DNA isolated from the Towne strain of CMV
was included in each experiment. In both the initial and nPCR
reactions, negative controls were also included in each experiment
(buffer, nucleotides, primers, magnesium and Taq DNA
polymerase, but no template). PCR products (approximately 285 bp)
820
6/5/5
5/7/9
0/1/2
2/5/5
6/7/8
2/3/4
1/4/7
9/9/10
8/6/7
9/10/10
7/8/9
Arterial blood
PaO2 (mm Hg) O2SAT (%)
43.7
50.0
52.6
45.0
55.0
62.3
57.0
80.0
43.7
79.0
55.2
91
92
80
90
91
90
93
95
85
96
70
were detected by electrophoresis in 2% agarose gel stained with
ethidium bromide.
As the primers for amplification were selected from a region of
high peptide variability in the gB gene, the gB genotype of CMV
DNA was also determined by restriction fragment length
polymorphism (16).
Results
Seventy ill neonates were enrolled in the CMV follow-up
study: 36 preterm newborn infants and 34 term newborn
infants.
The presence of CMV DNA in the urine of the neonates
was detected by means of nPCR, and the gB genotype of the
CMV was also determined. CMV was found in the urine
samples of 11 (15.7%) of the neonates under intensive care.
Of the 11 CMV DNA samples, 10 proved to be of gB1 and
1 of gB2 genotype (case 9). During the follow-up period,
specimens for CMV detection were available from 10
patients. The gB genotype of the CMV DNA was found to
be the same as indentified after birth. Urinary excretion of
CMV was not detected in any of the 50 healthy neonates.
In 4 of the CMV-infected neonates, hypoxaemia was
detected at birth. In these cases, the Apgar scores were less
than 4 at 1 minute (Table I). The pH of the arterial blood was
below 7.2 in 3 cases. The paO2 was below 50 mm Hg in 3
cases, but the O2 therapy applied resulted in a saturation
efficiency of 89-95% (Table I). In 2 cases, hyperbilirubinaemia
was detected, and in 2 cases also thrombocytopenia (Table II).
Following clinical admission, 7 neonates, of whom 3 were
preterm (cases 1, 2 and 4) and 4 were full-term (cases 3, 5,
6 and 9), required ventilatory support for 1 to 10 days.
Patient 4, a preterm infant, died of intracranial
haemorrhage, septic uraemia and prematurity at 9 days of
age. Ten CMV-infected neonates were followed up for 5
Nagy et al: Congenital CMV Infection in Selected Groups of Neonates
Table II. Laboratory findings in 11 newborn infants with congenital CMV infection at 2 weeks of age.
Infant
Thrombocyte
number (G/l)
1
2
3
4
5
6
7
8
9
10
11
240
204
191
128
56
237
103
199
268
132
238
Bilirubin
(M)
GOT
(U/l)
Blood serum
GPT
(U/l)
CN
(mM)
Creatine
(M)
154.4
87.8
42.1
133.6
NT*
27.1
236
239
NT
102
186
22
22
NT
45
NT
NT
54
18
15
25
24
17
16
NT
57
NT
NT
17
23
13
19
20
10.9
6.6
6.7
16.6
9.9
7.8
4.4
6.0
4.9
4.8
1.8
119
55
162
207
139
45
77
118
120
98
89
* NT: not tested
GOT: glutamate-oxalate-transaminase; GPT: glutamate-pyruvate-transaminase; CN: carbamic nitrogen
months to 4 years (Table III). Mental retardation was
observed in 4 cases, of whom 2 were preterm (cases 1 and 2)
and 2 were full-term neonates (cases 3 and 5). A
sensorineural hearing loss was detected in 1 neonate (case 3),
who was also growth-retarded. Bronchial asthma developed
in 1 preterm (case 10) and strabismus in 2 preterm cases
(cases 1 and 7). Five children born preterm (cases 1, 2, 7, 10
and 11) excreted CMV at their last visit and 1 was symptomfree. In the full-term group, 3 of the 5 patients excreted virus
and 1 was symptom-free. No virus was detected in the urine
of the 2 full-term patients (cases 6 and 9) during the follow
up period. They were clinically symptom-free, but intense
mechanical ventilation was required at birth in both cases.
Ophthalmologic examination did not reveal chorioretinitis in
any of the cases. Strabismus developed in 2 preterm infants
(cases 1 and 7). The results of audiometric testing were found
to be normal in all infants except case 3.
Discussion
The prevalence of congenital CMV infection in selected
newborns under intensive care with suspected intrauterine
infection proved to be high (15.7%). The frequency of CMV
infection in the preterm newborns (16.7%) was similar to
that observed in the full-term newborns (14.7%). Santos et
al. (17) detected congenital CMV infection in 6.8% (20 out
of 292) of non-selected newborns in a neonatal intensive
care unit. In Brazil, where the rate of CMV seropositivity
among pregnant women is 95%, Yamamoto et al. (18)
observed that the frequency of congenital CMV infection in
non-selected preterm newborns (2.1%) was similar to that
in full-term newborn infants (1.8%) and to that in another
high-immunity population (19,20).
The occurrence of severe manifestations of congenital
CMV infection has been reported in preterm infants
(19,21). In our study, 1 of the 6 preterm infants (case 4),
who was born with intracranial haemorrhage, sepsis and
RDS, died at 9 days of age. Another preterm infant (case 2)
was similarly born with intracranial haemorrhage. This
infant had pneumonitis at birth, too. An association
between congenital CMV infection and intracranial
haemorrhage has been described in two previous reports
(22,23). As 1-2% of babies are born with CMV infection, it
may be important to test for CMV in infants with
intracranial haemorrhage where there is no immediately
apparent cause. Necrotizing enterocolitis (NEC) was the
only clinical finding in 1 preterm infant (case 1) at birth, and
at 12 months of age mental retardation and strabismus were
detected. The association of NEC with congenital CMV
infection is rare. During the past 20 years, 6 cases of CMVassociated NEC have been reported in infants. The last
case, in a premature infant born to a mother with recurrent
maternal CMV infection, was published recently (24). Our
CMV-associated NEC case confirms the suggestion of
others that CMV should be added to the list of pathogens
potentially responsible for NEC (24,25). However, further
studies are needed, as full-term neonates with congenital
CMV infection-associated NEC have not been identified
(26). Strabismus occurs more frequently among children
who are symptomatic at birth than among those who are
initially asymptomatic (27,28). Although additional evidence
is needed, our data suggest that the incidence of strabismus
in the preterm population may be higher than in the fullterm population. The prolonged urinary excretion of CMV
was documented in both asymptomatic and symptomatic
patients in previous studies (29-31).
821
in vivo 18: 819-824 (2004)
Table III. Clinical findings in neonatal period and outcome of congenital CMV infection in newborns under intensive care.
Infant Gestation Body weight
at
(g)
age
(weeks)
Clinical findings
in neonatal period and up to 48 months
32
1820
Prematurity, necrotizing enterocolitis
Mental retardation, Strabismus
30
1670
39
2760
25
1150
35
2800
36
3480
RDS, hypoxia, sepsis, pneumonia,
Mental retardation, hydrocephaly
intracranial haemorrhage
Intrauterine asphyxia and infection, prematurity,
Mental retardation, hearing loss
hypotonia, seizures, polytraumatization, azotaemia
RDS, sepsis, intracranial haemorrhage,
Died
polytraumatization
Intrauterine infection, microcephaly, seizures,
Mental retardation, cerebral atrophy
polytraumatization, eclampsia, perinatal cerebral lesion,
intrauterine infection, thrombocytopenia
NIHF
Symptom-free
33
2070
37
3000
Intrauterine infection and hypoxia,
thrombocytopenia
Intrauterine infection
Symptom-free
40
3300
Intrauterine hypoxia, PFC
Symptom-free
10
34
1310
RDS, icterus
Bronchial asthma
11
32
2400
Intrauterine infection, icterus
Symptom-free
RDS: respiratory distress syndrome;
* follow-up period
NIHF: non-immune hydrops foetalis;
In conclusion, our study has demonstrated that the
frequency of congenital CMV infection is high in preterm
(16.7%) and full-term (14.7%) newborn infants under
intensive care with suspected intrauterine infection. It seems
that the clinical findings and the gB genotype of CMV
detected at birth do not allow a prediction of the outcome
of congenital CMV infections. Intracranial haemorrhage and
NEC should be added to the possible sequelae of congenital
CMV infection, especially in preterm newborns. Screening
of this group of neonates for congenital CMV appears
important. Those identified as having congenital CMV
infection can be monitored to correct any sequelae
immediately. The compassionate use of ganciclovir in
newborns with life-threatening or vision-threatening
congenital CMV infection is probably justified (32).
Acknowledgements
This study was supported by the Hungarian Scientific Research
Fund (grant OTKA-T26442/1998), the Research Fund of the
Hungarian Ministry of Education (grant FKFP 113/2000), and
ICON-H3 Ltd.
822
Strabismus, anaemia, chronic bronchitis
CMV excretion
(months)*
+
(12)
+
(5)
+
(48)
+
(9)
(36)
+
(36)
+
(24)
(24)
+
(36)
+
(36)
PFC: persistent foetal circulation.
We thank Mrs. Ildik Wellinger and Mrs. Csilla Szab for their
excellent technical assistance.
References
1 Stagno S. Cytomegalovirus: In: Infectious Diseases of the Fetus
and Newborn Infant. (Remington JS, Klein JO eds.)
Philadelphia Saunders WB, 2001 pp 389-424.
2 Griffiths PD, Baboonian D: A prospective study of primary
cytomegalovirus infection during pregnancy: Final report. Br J
Obstet Gynecol 91: 307-315, 1984.
3 Stagno S, Pass RF, Cloud G et al: Primary cytomegalovirus
infection in pregnancy. Incidence, transmission to fetus, and
clinical outcome. JAMA 256: 1904-1910, 1986.
4 Alford CA, Stagno S, Pass RF and Britt WJ: Congenital and
perinatal cytomegalovirus infections. Rev Infect Dis 12: 745-753,
1990.
5 Brown HL and Abernaty MP: Cytomegalovirus infection. Semin
Perinatol 22: 260-266, 1998.
6 Hagay ZJ, Biran G, Or-Noy A et al: Congenital cytomegalovirus
infection: A long-standing problem still seeking a solution. Am
J Obstet Gynecol 174: 241-245, 1996.
7 Morris DJ. Prevention of congenital cytomegalovirus disease. J
Infec Dis 161: 149, 1990.
Nagy et al: Congenital CMV Infection in Selected Groups of Neonates
8 Williamson WD, Demmler GJ, Percy AK et al: Progressive
hearing loss in infants with asymptomatic congenital
cytomegalovirus infection. Pediatrics 90: 862-866, 1992.
9 Stagno S, Pass RF, Dworsky ME and Alford CA: Maternal
cytomegalovirus infection and perinatal transmission. Clin
Obster Gynecol 25: 563-576, 1982.
10 Schopfer K, Lauber E and Kerch U: Congenital
cytomegalovirus infection in newborn infants of mothers
infected before pregnancy. Arch Dis Child 53: 536-539, 1978.
11 Bello C and Whittle H: Cytomegalovirus infection in Gambian
mothers and their babies. J Clin Pathol 44: 366-369, 1991.
12 Morris DJ, Sims D, Chiswick M, Das VK and Newton VE:
Symptomatic congenital cytomegalovirus infection after maternal
recurrent infection. Pediatr Infect Dis J 13: 61-64, 1994.
13 Benhushan A, Brzezinski A, Ben-David A and Nadjari M: Early
recurrent CMV infection with severe outcome to the fetus. Acta
Obstet Gynecol Scand 77: 694-698, 1998.
14 Durand C, Spagnolo G and Sagot P: Severe fetal cytomegalic
inclusion disease after documented maternal reactivation of
cytomegalovirus infection during pregnancy. Prenatal Diagn 20:
333-336, 2000.
15 Inoue T, Matsumura N, Fukuoka M, Sagawa N and Fujii S:
Severe congenital cytomegalovirus infection with fetal hydrops
in a cytomegalovirus-seropositive healthy woman. Eur J Obstet
Gynecol Reprod Biol 95: 184-186, 2001.
16 Chou S and Dennison KM: Analysis of interstrain variation in
cytomegalovirus glycoprotein B sequences encoding neutralizationrelated epitopes. J Infect Dis 163: 1229-1234, 1991.
17 Santos DVV, Souza MMR, Goncalves SHL et al: Congenital
cytomegalovirus infection in a neonatal intensive care unit in
Brazil evaluated by PCR and association with perinatal aspect.
Rev Inst Med Trop S Paulo 42: 129-132, 2000.
18 Yamamoto AY, Mussi-Pinhata MM, Pinto PCG, Figueiredo
LTM and Jorge SM: Congenital cytomegalovirus infection in
preterm and full-term newborn infants from a population with a
high seroprevalance rate. Pediatr Infect Dis J 20: 188-192, 2001.
19 Stagno S, Dworsky ME, Torres J, Mesa T and Hirsch T:
Prevalence and importance of congenital cytomegalovirus infection
in three different populations. J Pediatr 101: 897-900, 1982.
20 Pannuti CS, Vilas-Boas LS, Angelo MJO, Carvalho RPS and
Segre CM: Congenital cytomegalovirus infection: occurrence in
two socioeconomically distinct populations of a developing
country. Rev Inst Med Trop S Paulo 27: 105-107, 1985.
21 Perlman JM and Argyle C: Lethal cytomegalovirus infection in
preterm infants: clinical, radiological, and neuropathological
findings. Ann Neurol 31: 64-68, 1992.
22 Berkovich AJ and Lindan CE: Congenital cytomegalovirus
infection of the brain: imaging analysis and embryologic
consideration. Am J Neuroradiol 15: 703-715, 1994.
23 McDonald JM, Raghuveer TS and DAlessandro MP: Can
congenital CMV infection lead to intracranial hemorrhage? J
Perinatol 21: 402-404, 2001.
24 Gaytant MA, Ingrid G, Rours JG, Steegers EAP, Galama JMD
and Semmerkrot BA: Congenital cytomegalovirus infection
after recurrent infection: case reports and review of the
literature. Eur J Pediatr 162: 248-253, 2003.
25 Reyes C, Pereira S, Warden MJ and Sills J: Cytomegalovirus
enteritis in a premature infant. J Pediatr Surg 32: 1545-1547,
1997.
26 Scy Ng: Necrotizing enterocolitis in the full-term neonate. J
Pediatr Child Health 37: 1-4, 2001.
27 Anderson KS, Amos CS, Boppana S and Pass R: Ocular
abnormalities in congenital cytomegalovirus infection. J Am
Optom Assoc 67: 273-278, 1996.
28 Coats DK, Demmler GJ, Paysse EA, Du LT and Libby C:
Ophthalmologic findings in children with congenital
cytomegalovirus infection. J AAPOS 4: 110-116, 2000.
29 Saigal S, Lunyc O, Larke RPB and Chernesky MA: The
outcome in children with congenital cytomegalovirus infection.
Am J Dis Child 136: 896-901, 1982.
30 Pass RF, Stagno S, Britt WJ and Alford CA: Specific cellmediated immunity and the natural history of congenital
infection with cytomegalovirus. J Infect Dis 148: 953-961, 1983.
31 Noyola DE, Demmler GJ, Williamson WD et al:
Cytomegalovirus urinary excretion and long term outcome in
children with congenital cytomegalovirus infection. Pediatr
Infect Dis J 19: 505-510, 2000.
32 Management of cytomegalovirus infection in the pregnant
women and neonate. In: Pass R, Weber T, Whitley R. eds.
Herpesvirus Infections in Pregnancy. IHMF Managements
Strategies in Herpes monographs. 2001 pp 55-66. Available at
http://www/ihmf.org/monography/m_09.pdf.
Received July 30, 2004
Accepted October 20, 2004
823
You might also like
- Case Report: Severe Congenital Toxoplasmosis: A Case Report and Strain CharacterizationDocument4 pagesCase Report: Severe Congenital Toxoplasmosis: A Case Report and Strain CharacterizationNamanamanaNo ratings yet
- PCR IT RatioDocument5 pagesPCR IT RatioAgus WijayaNo ratings yet
- TORCH InfectionsDocument37 pagesTORCH InfectionsEylin Halim Rahardjo100% (1)
- Evidence 3) Congenital Infection Causes Neurologic and Hematologic Damage andDocument5 pagesEvidence 3) Congenital Infection Causes Neurologic and Hematologic Damage andandamar0290No ratings yet
- AbstractDocument1 pageAbstractRadwa AlkadyNo ratings yet
- Jurnal HibridisasiDocument12 pagesJurnal HibridisasiNurfanida Natasya mNo ratings yet
- Congenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasDocument3 pagesCongenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasMinerva StanciuNo ratings yet
- HPV E6E7 mRNA 1173 PatientDocument9 pagesHPV E6E7 mRNA 1173 PatienthippopotamasNo ratings yet
- 040 27736am101214 311 314Document4 pages040 27736am101214 311 314Finka InaraeNo ratings yet
- Art 3A10.1007 2Fs00405 009 0988 6Document6 pagesArt 3A10.1007 2Fs00405 009 0988 6mfhfhfNo ratings yet
- MEDRXIV 2021 267417v1 SigalDocument9 pagesMEDRXIV 2021 267417v1 SigalAme DNo ratings yet
- MEDRXIV 2021 267417v1 SigalDocument9 pagesMEDRXIV 2021 267417v1 Sigalenota15No ratings yet
- Ijpedi2021 1544553Document6 pagesIjpedi2021 1544553Naresh ReddyNo ratings yet
- Diagnosis of Congenital Toxoplasmosis by Polymerase Chain Reaction On Neonatal Peripheral BloodDocument3 pagesDiagnosis of Congenital Toxoplasmosis by Polymerase Chain Reaction On Neonatal Peripheral BloodRika FitriaNo ratings yet
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- Lau2015 PDFDocument11 pagesLau2015 PDFAntoniaNo ratings yet
- EBV Virus Causing Infectious MononucleosisDocument21 pagesEBV Virus Causing Infectious MononucleosiskamalNo ratings yet
- Dr. Vona 12Document5 pagesDr. Vona 12Agustiawan ImronNo ratings yet
- Serological Evidence of Merkel Cell Polyomavirus Primary Infections in ChildhoodDocument5 pagesSerological Evidence of Merkel Cell Polyomavirus Primary Infections in ChildhoodzahidNo ratings yet
- Acta Paediatrica - 2020 - Lüsebrink - Retrospectively diagnosing congenital cytomegalovirus infections in symptomaticDocument6 pagesActa Paediatrica - 2020 - Lüsebrink - Retrospectively diagnosing congenital cytomegalovirus infections in symptomaticdossantoselaine212No ratings yet
- Diagnostic VirologyDocument46 pagesDiagnostic VirologySarah DadoNo ratings yet
- Aids With CMVDocument8 pagesAids With CMVIchunx MelissaNo ratings yet
- 2 - Adult Meningitis in A Setting of High HIV and TB Prevalence - Findings From 4961 Suspected Cases 2010 (Modelo para o Trabalho)Document6 pages2 - Adult Meningitis in A Setting of High HIV and TB Prevalence - Findings From 4961 Suspected Cases 2010 (Modelo para o Trabalho)SERGIO LOBATO FRANÇANo ratings yet
- Detection of Toxoplasma Gondii by PCR and Quantitative PCR With High Specificty and Lower Limit of DetectionDocument7 pagesDetection of Toxoplasma Gondii by PCR and Quantitative PCR With High Specificty and Lower Limit of DetectionSholatya FurqonieNo ratings yet
- ToxoplasmosisDocument16 pagesToxoplasmosisNur MasrurohNo ratings yet
- tmp88D2 TMPDocument5 pagestmp88D2 TMPFrontiersNo ratings yet
- Newborn Screening For Congenital Infectious DiseasesDocument5 pagesNewborn Screening For Congenital Infectious DiseasesMinerva StanciuNo ratings yet
- CLL and ERs Manuscript.Document15 pagesCLL and ERs Manuscript.Nadeem khanNo ratings yet
- B The PigDocument16 pagesB The PigMaria SerlyantiNo ratings yet
- Assessment of The FilmArray Multiplex PCR System and Asso 2020 Infection PRDocument6 pagesAssessment of The FilmArray Multiplex PCR System and Asso 2020 Infection PRjwfqcw74mfNo ratings yet
- Evidence of Human Papillomavirus in The Placenta: BriefreportDocument3 pagesEvidence of Human Papillomavirus in The Placenta: Briefreportursula_ursulaNo ratings yet
- Suleiman 1Document8 pagesSuleiman 1elsa_imamNo ratings yet
- MikesDocument34 pagesMikesBesong MichaelNo ratings yet
- Zauli 2013Document6 pagesZauli 2013Денис КрахоткинNo ratings yet
- 10096_2015_Article_2481Document8 pages10096_2015_Article_2481Frank Barreiro SanchezNo ratings yet
- Lower Vitamin D Levels Are Associated With Increased Risk of Early-Onset Neonatal Sepsis in Term InfantsDocument7 pagesLower Vitamin D Levels Are Associated With Increased Risk of Early-Onset Neonatal Sepsis in Term InfantsMohamed Abo SeifNo ratings yet
- Detecting Genital Herpes by Real-Time PCRDocument5 pagesDetecting Genital Herpes by Real-Time PCRAron RonalNo ratings yet
- Evaluation of PCV, Cd4 T Cell Counts, ESR and WBC Counts in Malaria Infected Symptomatic HIV (Stage 11) Male HIV/ Aids Subjects On Antiretroviral Therapy (Art) in Nnewi, South Eastern NigeriaDocument5 pagesEvaluation of PCV, Cd4 T Cell Counts, ESR and WBC Counts in Malaria Infected Symptomatic HIV (Stage 11) Male HIV/ Aids Subjects On Antiretroviral Therapy (Art) in Nnewi, South Eastern NigeriaIOSR Journal of PharmacyNo ratings yet
- Laboratory Diagnosis of CMV Infection: A ReviewDocument6 pagesLaboratory Diagnosis of CMV Infection: A ReviewAchmad ArrizalNo ratings yet
- 1 BavejaDocument9 pages1 BavejaIJAMNo ratings yet
- Carraro 2013 RSBMTV 46 N 2 P 161Document5 pagesCarraro 2013 RSBMTV 46 N 2 P 161Emerson CarraroNo ratings yet
- Pathcare May-Aug PDFDocument6 pagesPathcare May-Aug PDFdenosciNo ratings yet
- Interferon Gamma Production in The Course of Mycobacterium Tuberculosis InfectionDocument9 pagesInterferon Gamma Production in The Course of Mycobacterium Tuberculosis InfectionAndia ReshiNo ratings yet
- Clinical Characteristics of 19 Neonates Born To Mothers With COVID-19Document6 pagesClinical Characteristics of 19 Neonates Born To Mothers With COVID-19anhiramdhaniNo ratings yet
- Esc Pointers On The Diagnosis and Administration of Acute Pulmonary EmbolismDocument3 pagesEsc Pointers On The Diagnosis and Administration of Acute Pulmonary EmbolismgwaniegdnrNo ratings yet
- Pelagia Research Library: Available Online atDocument4 pagesPelagia Research Library: Available Online atRabecca TobingNo ratings yet
- PapilomaDocument6 pagesPapilomaapi-3710742No ratings yet
- Congenital Viral InfectionsDocument43 pagesCongenital Viral Infectionsannie1970100% (1)
- Background: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSDocument6 pagesBackground: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSSav GaNo ratings yet
- 0036 4665 Rimtsp 55 03 148Document1 page0036 4665 Rimtsp 55 03 148don yenNo ratings yet
- Dxto de Infecciones en El SNCDocument17 pagesDxto de Infecciones en El SNCcarlos ballestasNo ratings yet
- NLR - Neonatal SepsisDocument6 pagesNLR - Neonatal SepsisGlen LazarusNo ratings yet
- Role of Hematologic Scoring System in Early Diagnosis of Neonatal SepticemiaDocument6 pagesRole of Hematologic Scoring System in Early Diagnosis of Neonatal SepticemiarantiadrianiNo ratings yet
- Jurnal 2Document12 pagesJurnal 2zingioNo ratings yet
- CMV Primer Non PrimerDocument3 pagesCMV Primer Non PrimerNi Wayan Ana PsNo ratings yet
- MAKALAH Keputusasan-1Document7 pagesMAKALAH Keputusasan-1ARINANo ratings yet
- HPV Detection Using Primers MY09/MY11 and GP5+/GP6+ in Patients With Cytologic And/or Colposcopic ChangesDocument6 pagesHPV Detection Using Primers MY09/MY11 and GP5+/GP6+ in Patients With Cytologic And/or Colposcopic ChangesLorena BlancoNo ratings yet
- Klebsiella Pneumoniae ThesisDocument6 pagesKlebsiella Pneumoniae Thesisaprillaceyjackson100% (1)
- 77754571Document7 pages77754571stephaniedianNo ratings yet
- Complications of Infectious Mononucleosis in Children: PediatricsDocument10 pagesComplications of Infectious Mononucleosis in Children: PediatricsOrhan ErNo ratings yet
- Tutorial - DMDocument52 pagesTutorial - DMMinerva StanciuNo ratings yet
- Administrare Diazepam RectalDocument1 pageAdministrare Diazepam RectalMinerva StanciuNo ratings yet
- 12 - CHEER Predicting PreDM CVD Risk Obese TeensDocument61 pages12 - CHEER Predicting PreDM CVD Risk Obese TeensMinerva StanciuNo ratings yet
- CongenitalDocument25 pagesCongenitalSUTHANNo ratings yet
- Kapil Sethi - Paroxysmal Dyskinesias Newest-NO VIDEOSDocument43 pagesKapil Sethi - Paroxysmal Dyskinesias Newest-NO VIDEOSMinerva StanciuNo ratings yet
- 17 173583Document15 pages17 173583Minerva StanciuNo ratings yet
- Strategic Multiannual Programme 2014 2020Document63 pagesStrategic Multiannual Programme 2014 2020Minerva StanciuNo ratings yet
- Early Metabolic ImprintingDocument14 pagesEarly Metabolic ImprintingMinerva StanciuNo ratings yet
- 18 Garweg PDFDocument40 pages18 Garweg PDFMinerva StanciuNo ratings yet
- 1congenital Infections - DRSQDocument21 pages1congenital Infections - DRSQMinerva StanciuNo ratings yet
- Congenital Cytomegalovirus Infection: Description of VirusDocument6 pagesCongenital Cytomegalovirus Infection: Description of VirusMinerva StanciuNo ratings yet
- 19en V68n1a2Document13 pages19en V68n1a2Minerva StanciuNo ratings yet
- Role of Hcps in The Prevention of Obesity: Dr. Abdul JabbarDocument73 pagesRole of Hcps in The Prevention of Obesity: Dr. Abdul JabbarMinerva StanciuNo ratings yet
- Congenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasDocument3 pagesCongenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasMinerva StanciuNo ratings yet
- 22britt William FINALDocument15 pages22britt William FINALMinerva StanciuNo ratings yet
- Congenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasDocument3 pagesCongenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasMinerva StanciuNo ratings yet
- 15MonicaLahra PerinatalInfectionDocument40 pages15MonicaLahra PerinatalInfectionMinerva StanciuNo ratings yet
- 17 173583Document15 pages17 173583Minerva StanciuNo ratings yet
- Ocular Pathology in Congenital Infections: Swiss Eye Institute and University of Bern, SwitzerlandDocument40 pagesOcular Pathology in Congenital Infections: Swiss Eye Institute and University of Bern, SwitzerlandMinerva StanciuNo ratings yet
- 12 Child Neurol 2015 Urger 9 20Document12 pages12 Child Neurol 2015 Urger 9 20Minerva StanciuNo ratings yet
- TGF-b1 Genotype in Pediatric Migraine PatientsDocument5 pagesTGF-b1 Genotype in Pediatric Migraine PatientsMinerva StanciuNo ratings yet
- Congenital Cytomegalovirus Infection: Description of VirusDocument6 pagesCongenital Cytomegalovirus Infection: Description of VirusMinerva StanciuNo ratings yet
- 214 FullDocument8 pages214 FullMinerva StanciuNo ratings yet
- 15MonicaLahra PerinatalInfectionDocument40 pages15MonicaLahra PerinatalInfectionMinerva StanciuNo ratings yet
- Corticosteroid Use in Duchenne Muscular Dystrophy Increased Over TimeDocument6 pagesCorticosteroid Use in Duchenne Muscular Dystrophy Increased Over TimeMinerva StanciuNo ratings yet
- Other Congenital and Perinatal InfectionsDocument3 pagesOther Congenital and Perinatal InfectionsRabi SyedNo ratings yet
- 13Lec-Approach To Neonates With Suspected Congenital InfectionsDocument56 pages13Lec-Approach To Neonates With Suspected Congenital InfectionsMinerva Stanciu100% (1)
- 11pediatrics in Review 2011 Del Pizzo 537 42Document8 pages11pediatrics in Review 2011 Del Pizzo 537 42Minerva StanciuNo ratings yet
- ICPC-2 - EnglishDocument2 pagesICPC-2 - EnglishEddieNo ratings yet
- Kelainan Kongenital GenetikDocument39 pagesKelainan Kongenital GenetikvictorNo ratings yet
- Course 1 Prefixation and SuffixationDocument6 pagesCourse 1 Prefixation and SuffixationSárközi TiborNo ratings yet
- Annotated BibliographyDocument13 pagesAnnotated BibliographyAkailah MasonNo ratings yet
- Genetic Control of Cell Function and InheritanceDocument7 pagesGenetic Control of Cell Function and InheritanceSADAVEJO100% (1)
- Diagnosis in Orthodontics: Key to Effective TreatmentDocument13 pagesDiagnosis in Orthodontics: Key to Effective TreatmentMargarita Lopez MartinezNo ratings yet
- NEONATAL MALARIA New OneDocument41 pagesNEONATAL MALARIA New Onemufracaca60% (5)
- AntepartalDocument27 pagesAntepartalaliehso100% (1)
- The Infant of A Diabetic MotherDocument19 pagesThe Infant of A Diabetic MotherapolismarNo ratings yet
- Pneumocystis Pneumonia Causes, Symptoms, Diagnosis & PreventionDocument16 pagesPneumocystis Pneumonia Causes, Symptoms, Diagnosis & PreventionMaría Luisa MantillaNo ratings yet
- Apert SyndromeDocument9 pagesApert SyndromeRiyan BudianorNo ratings yet
- Genetic DiseasesDocument43 pagesGenetic DiseasesAisha BirdNo ratings yet
- whd2016 Brochure en 2Document16 pageswhd2016 Brochure en 2api-311125682No ratings yet
- TORCH in PregnancyDocument63 pagesTORCH in PregnancySaRah AmiThia SaRi BuLanNo ratings yet
- Truncus ArteriosusDocument9 pagesTruncus ArteriosusAkang KurniawanNo ratings yet
- OB Nursing Bullets PNLEDocument25 pagesOB Nursing Bullets PNLEACNo ratings yet
- Hiperc YpDocument5 pagesHiperc YpRandall BarahonaNo ratings yet
- Star Smiley 2007Document343 pagesStar Smiley 2007David Ajibade100% (1)
- Arthrogryposis Multiplex Congenita-Dr S P DasDocument7 pagesArthrogryposis Multiplex Congenita-Dr S P DasSheel GuptaNo ratings yet
- Colonic Atresia PDFDocument2 pagesColonic Atresia PDFCraigNo ratings yet
- Public Health - Resume of Shah BookDocument54 pagesPublic Health - Resume of Shah BookKami Dhillon83% (6)
- Prenatal care guideDocument31 pagesPrenatal care guideNoraNo ratings yet
- Congenital Corneal DisordersDocument101 pagesCongenital Corneal Disorderseyemd_in_training100% (1)
- Dengue Infection During Pregnancy andDocument7 pagesDengue Infection During Pregnancy andAlia SalviraNo ratings yet
- 1 Perspectives of Pediatric NursingDocument57 pages1 Perspectives of Pediatric NursingBluebloodboyNo ratings yet
- HemoDynamics and CardiologyDocument452 pagesHemoDynamics and CardiologyYuliawati Haruna100% (1)
- Biological BeginningsDocument24 pagesBiological BeginningsRabia DastiNo ratings yet
- Final SLE4 ThedDocument95 pagesFinal SLE4 Thednavi_khiNo ratings yet
- RubelaDocument11 pagesRubelaMuhammad YusriNo ratings yet
- Poilcy Guidelines & Help ManualDocument32 pagesPoilcy Guidelines & Help ManualHarshad PaigudeNo ratings yet