Professional Documents
Culture Documents
Acute Severe Asthma in Adults
Uploaded by
sobanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Severe Asthma in Adults
Uploaded by
sobanCopyright:
Available Formats
ADULT ASTHMA
Whats new ?
Acute severe asthma
in adults
Patients with severe asthma and adverse behavioural
and psychological factors are at particular risk of
fatal/near-fatal episodes
Colin Robertson
Intravenous magnesium sulphate has replaced
aminophylline as second-line therapy
Patient education and follow-up are essential to reduce
the frequency and severity of further episodes
Despite major improvements in the recognition of patients with
asthma and their treatment, both chronically and for acute episodes, acute severe asthma remains a life-threatening condition.
Most patients who die from asthma have a history of chronic, often
severe disease, but fatal or near-fatal events can occur in patients
who have previously exhibited only mild or moderate symptoms.
A background of poor behavioural and psychosocial features is
well recognized in these patients (Figure 1). Medical factors in
at-risk patients include:
prior severe episodes
admission to or attendance at an A&E department with asthma
during the last year
heavy use of 2-agonists
those taking three or more classes of asthma medication
those with brittle asthma.
Peaks of asthma deaths occur in the summer in younger patients
and the winter in older patients, possibly reflecting triggers of the
event. Most asthma deaths occur in the community, and in most
patients symptoms develop over hours or days rather than minutes.
The importance of patient education about asthma in general,
how to recognize the severity of symptoms and the institution of
preventive therapy cannot be over-emphasized.
Who needs referral to hospital?
Any patient with acute severe or life-threatening features should
be referred to hospital. Treatment should begin (see below) and
continue in transit to hospital. In the UK, ambulance crews can
administer oxygen and nebulized 2-agonists and institute ECG and
arterial oxygen saturation (SaO2) monitoring (pulse oximetry).
Investigations
Assessment of oxygenation and ventilation pulse oximetry is
commonly available in and out of hospital and provides a simple,
non-invasive estimate of tissue oxygen saturation. An SaO2 of 92%
or less indicates a life-threatening attack. Arterial blood analysis
is required in all patients with any life-threatening feature (Figure
2) and in any patient with SaO2 less than 92%. Normal arterial
partial pressure of carbon dioxide (PaCO2, 4.66.0 kPa) implies a
life-threatening episode. Raised PaCO2 or respiratory acidaemia is
particularly ominous.
Other investigations no individual laboratory marker at a
single point in time is useful for prognosis. A full blood count
is commonly performed, but a raised WBC count is common in
acute asthma even in the absence of infection. Urea and electrolyte
How to recognize a severe attack
Increasing symptoms of wheeze, dyspnoea, chest tightness or
coughing are common. Figure 2 lists the features of acute severe,
life-threatening and near-fatal attacks. It should be noted that
the absence of any of these features does not preclude a severe
attack. No clinical feature, individually or combined with others,
is specific for a severe event.
Measurement of peak expiratory flow (PEF) is the single most
important objective clinical measurement in the community, in
the A&E department and in hospital. PEF is best expressed as a
percentage of the patients previous best value. If this is not known,
a percentage of the predicted value is a rough guide. A PEF of less
than 50% indicates acute severe asthma; less than 33% indicates
a life-threatening situation.
Factors associated with fatal/near-fatal asthma attacks
Behavioural
Poor compliance/non-compliance with
therapy/GP or hospital reviews/hospital admission
Denial
Psychiatric
Psychosis
Depression
Major tranquillizer use
Alcohol/drug misuse
Social
Learning, work or income problems
Social isolation
Childhood abuse
Severe family or other stress
Obesity
Colin Robertson is Consultant in Emergency Medicine at the Royal
Infirmary, Edinburgh, UK. His research interests include cardiorespiratory
resuscitation, multiple trauma and pre-hospital care.
MEDICINE
69
2003 The Medicine Publishing Company Ltd
ADULT ASTHMA
fective. The drug should preferably be given in a wet nebulizer
driven by oxygen. If an oxygen source is not available, an airdriven nebulizer should be used. If a nebulizer is not available,
the 2-agonist can be given by repeatedly activating a metered-dose
inhaler via an appropriate large-volume spacer.
When the initial dose of the 2-agonist does not achieve a good
result, repeat bolus nebulized doses or continuous nebulization (at
a dose of 510 mg/hour) should be given. Intravenous administration of a 2-agonist is indicated only in patients in whom nebulized
therapy cannot be used.
Ipratropium bromide nebulized ipratropium bromide, 0.5 mg,
should be added to the nebulized 2-agonist in patients suffering an
acute severe or life-threatening event, and in those who exhibit a
poor initial response to 2-agonist therapy alone. Further nebulized
doses of ipratropium bromide, 0.5 mg, can be given 46-hourly.
Corticosteroids reduce mortality and relapse rates and should
be given at the earliest possible opportunity. If the patient can
swallow, oral therapy is as effective as parenteral administration.
An initial dose of prednisolone, 4050 mg p.o., should be given.
An initial dose of hydrocortisone, 100 mg i.v., can be given to
patients who are unable to take oral treatment. Subsequently,
prednisolone, 4050 mg/day p.o., is given for at least 5 days.
(When hydrocortisone is used, the dose is 100 mg 6-hourly i.v.)
Magnesium sulphate is an adjunctive therapy in acute severe
asthma. It appears to act by blocking bronchial smooth muscle
calcium channels, inhibiting cholinergic neuromuscular transmission and stabilizing lymphocytes and mast cells. A single dose
of 1.22 g i.v. infused over 20 minutes should be considered in
life-threatening or near-fatal cases, or when a patient with acute
severe asthma has not responded well to inhaled bronchodilator
and corticosteroid therapy, after senior review. Repeated doses are
not indicated. Adverse effects of magnesium infusion, including
flushing, sweating, nausea, hypotension and muscle weakness,
are usually related to too rapid a rate of infusion.
Aminophylline intravenous aminophylline was commonly
used in the past, but does not produce additional benefit in patients
who have already received 2-agonists and corticosteroids. Adverse
affects including cardiac arrhythmias, nausea and vomiting are
more likely. As a consequence, intravenous aminophylline should
be used only under the direction of a senior, experienced clinician.
No loading dose should be used in patients who have been taking
aminophylline or theophylline orally; it is vital to measure blood
levels of aminophylline.
Other treatments bacterial infection is an uncommon precipitant of acute severe asthma, and routine or blind antibiotic
therapy is not indicated. Antibiotics may be required for patients
with pyrexia, purulent sputum or clinical/radiological evidence of
pneumonia.
Heliox (a mixture of 6080% helium and 2040% oxygen)
reduces airflow resistance because its density is lower than that
of air. It has been suggested that it may be of value in acute severe
asthma by reducing the work of breathing for sufficiently long to
allow other therapeutic modalities to take effect. This concept
is theoretically attractive but has not yet been shown to be of
unequivocal benefit.
Rehydration (oral and/or intravenous) may be required in some
patients, particularly when symptoms have been present for days
before admission. Regular estimations of plasma potassium, magnesium and phosphate (and correction when necessary) may be
Features of acute severe, life-threatening and
near-fatal asthma attacks
Acute severe asthma
Any one of the following
Peak expiratory flow 3350% best or predicted
Respiratory rate 25 per minute
Heart rate 110 per minute
Unable to complete sentences in one breath
Life-threatening asthma
Any one of the following in a patient with severe asthma
Peak expiratory flow < 33% best or predicted
SaO2 < 92%
Silent chest
Cyanosis
Poor respiratory effort
Bradycardia or other arrhythmia
Hypotension
Exhaustion
Confusion, altered consciousness or coma
PaO2 < 8 kPa
Normal PaCO2 (4.66.0 kPa)
Near-fatal asthma
Raised PaCO2 ( > 6.0 kPa) and/or patient requires mechanical
ventilation with raised inflation pressures
measurements may be useful, particularly in patients who are
already taking corticosteroids, 2-agonists or diuretics, because
hypokalaemia, hypomagnesaemia and hypophosphataemia may
be present and aggravate respiratory muscle function. Elevated
lactate levels are common, but reflect general tissue hypoxia and
are unhelpful prognostically. Chest radiography is not routinely
required, but should be undertaken in patients with suspected
pneumothorax, pneumomediastinum or pulmonary consolidation
or collapse, in life-threatening presentations, and in those who fail
to respond to treatment appropriately or require ventilation.
Management
Patients should be seen and treated immediately in a highdependency or resuscitation area of the A&E department or receiving unit. ECG, SaO2 and non-invasive blood pressure recordings are the minimum monitoring requirements.
Oxygen therapy hypoxaemia is almost invariably present in
patients with acute severe asthma. All patients should be given
oxygen at a high inspired concentration, using a mask that can
deliver an FiO2 of 4060%. The aim is to maintain SaO2 above 92%.
Nebulizers should be oxygen-driven whenever possible. Concerns
that hypercapnoea may be induced by high-flow oxygen, as may
occur in some patients with chronic obstructive pulmonary disease
(COPD), are unfounded. Hypercapnoea in the context of acute
severe asthma indicates a near-fatal event and mandates immediate involvement of senior specialist/anaesthetic staff.
2-agonists are first-line agents and should be given immediately. Salbutamol, 5 mg, and terbutaline, 10 mg, are equally ef-
MEDICINE
70
2003 The Medicine Publishing Company Ltd
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
required, because both 2-agonists and corticosteroid therapy can
cause or exacerbate hypokalaemia.
Senior/ICU assistance should be sought immediately in every
patient with features of life-threatening asthma (Figure 2). Tracheal
intubation is clearly required in patients with cardiac arrest, apnoea
or loss of consciousness. Otherwise, the decision to intubate and
institute positive-pressure ventilation in an asthmatic patient
requires senior specialist expertise.
While preparations are being made for emergency intubation,
the patient should be given 100% oxygen by an anaesthetic mask.
Data on the optimal induction agent are limited, but ketamine (a
parenteral anaesthetic agent) and inhalational anaesthetics (e.g.
isoflurane, halothane, ether) have been used and have bronchodilating properties. Their use requires specialist expertise, because
they have vasodilating and myocardial depressant actions and
may sensitize the myocardium to catecholamines. The potential
for induction of life-threatening arrhythmias and/or hypotension
is high.
Following intubation, use of a benzodiazapine is indicated to
ensure sedation, with neuromuscular blockade to improve pulmonary compliance and aid ventilation. A ventilation strategy of
controlled hypoventilation (permissive hypercapnoea) with high
FiO2 is commonly used. Often, only a short period of ventilation and ICU care is required, because most patients respond
rapidly to these and previously started treatments. However,
positive-pressure ventilation in patients with asthma has specific
problems including hypotension, barotrauma (pneumothorax
and pneumomediastinum) and nosocomial infection. The most
common cause of severe hypotension in a ventilated asthmatic
patient is auto-positive end-expiratory pressure secondary to air
trapping. This can be corrected by stopping ventilation for a brief
period (< 60 seconds) while observing the patients oxygen
status, then restarting at a ventilation rate of 810 per minute.
Discharge and follow-up before discharge, check that the
patients inhaler technique is adequate, that all medications (inhalers, corticosteroid, antibiotics) have been altered appropriately,
and that he or she has and understands a PEF record chart and
symptom-based asthma plan. The GP must be informed directly
whenever a patient with asthma has needed A&E or hospital treatment following an exacerbation. The patient should be reviewed
by an asthma liaison nurse or GP within 48 hours of discharge,
and in a specialist hospital clinic after about 1 month.
COPD: causes and pathology
William MacNee
Chronic obstructive pulmonary disease (COPD) is a general term
encompassing several previously used clinical labels such as
chronic bronchitis and emphysema, chronic obstructive airways
disease and chronic obstructive lung disease. COPD is defined
by the Global Initiative for Obstructive Lung Disease (GOLD) as
a disease state characterised by airflow limitation that is not fully
reversible. The airflow limitation is usually both progressive and
associated with an abnormal inflammatory response of the lungs
to noxious particles or gases.
Few population-based prevalence surveys of COPD have
been published. Data based on physician diagnosis from the UK
General Practice Research Database indicate a prevalence in 1997
of 1.7% in men and 1.4% in women. The prevalence of COPD in
men reached a plateau in the mid-1990s, but continues to increase
in women. In the UK, about 30,000 deaths/year are caused by
COPD; this accounts for about 6% of all male and 4% of all
female deaths. The annual NHS workload for COPD exceeds that
of asthma. About 25% of all medical admissions are as a result
of respiratory diseases, and more than 50% of these are cases of
COPD. In general practice, annual consultation rates for COPD
increase with age from 417/10,000 population in 4564-year-olds
to 1032/10,000 population in 7584-year-olds.
Risk factors
Exposure to tobacco smoke cigarette smoking is the most
important risk factor for COPD. In general, the greater the exposure
to tobacco, the greater the risk, though there is wide variation in
susceptibility (Figure 1). The commonly cited statement that only
1020% of smokers appear to be susceptible and develop clinically
significant COPD is probably an underestimate, because COPD is
under-diagnosed.
Passive exposure to cigarette smoke may also contribute to
respiratory symptoms and to COPD. Smoking during pregnancy
may increase the risk of COPD by affecting fetal lung growth.
Recurrent bronchopulmonary infections the British hypothesis suggests that persistent airflow obstruction may be the end
result of damage caused by repeated bronchopulmonary infections.
A history of severe childhood infections has been associated with
reduced lung function and increased respiratory symptoms in
FURTHER READING
British Thoracic Society, Scottish Intercollegiate Guidelines Network.
British guideline on asthma management: a national clinical
guideline. Thorax 2003; 58: (Suppl. 1): i194.
(Essential reading for all clinicians involved in the care of asthma
patients.)
Cates C J, Rowe B H, Bara A. Holding chambers vs nebulisers for
beta-agonist treatment of acute severe asthma. The Cochrane Library
2001; 3.
Parameswaran K, Belda J, Rowe B H. Addition of intravenous
aminophylline to beta2 agonists in adults with acute asthma.
The Cochrane Library 2001; 3.
Rowe B H, Bretzlaff J A, Bourdon C et al. Magnesium sulphate for treating
exacerbations of acute asthma in the emergency department.
The Cochrane Library 2001; 2.
MEDICINE
William MacNee is Professor of Respiratory and Environmental Medicine
at the University of Edinburgh Medical School, Edinburgh, UK,
Consultant Physician and Patient Services Director in Lothian University
NHS Trust, an MRC Research Fellow in Edinburgh, and MRC Travelling
Fellow to the University of British Columbia, Vancouver, Canada.
71
2003 The Medicine Publishing Company Ltd
You might also like
- Acute Exacerbation of Copd & Status AsthmaticusDocument59 pagesAcute Exacerbation of Copd & Status AsthmaticusSaras SinghNo ratings yet
- Jurnal Fadhila AsthmaDocument32 pagesJurnal Fadhila AsthmaJannah Miftahul JannahNo ratings yet
- Acute Asthma Bts 2011 QRCDocument2 pagesAcute Asthma Bts 2011 QRCJustin AuchwitzNo ratings yet
- Mksap PulmonaryDocument77 pagesMksap PulmonaryAna Roman100% (4)
- Asthma & COPDDocument9 pagesAsthma & COPDRobert L G MabongaNo ratings yet
- Managing Acute Asthma EpisodesDocument6 pagesManaging Acute Asthma EpisodesMariana UngurNo ratings yet
- Acute Severe Asthma (Status Asthmaticus)Document20 pagesAcute Severe Asthma (Status Asthmaticus)blok etikakedokteranNo ratings yet
- Journal Reading STATUS ASMATIKUS-Rezky Amalia Basir 70700120013Document15 pagesJournal Reading STATUS ASMATIKUS-Rezky Amalia Basir 70700120013Rezky amalia basirNo ratings yet
- Assessment and Management OF Acute Severe AsthmaDocument43 pagesAssessment and Management OF Acute Severe Asthmadentist40No ratings yet
- Critical Care Management of Acute Severe AsthmaDocument53 pagesCritical Care Management of Acute Severe AsthmaYohana SepthiyaNo ratings yet
- Management of Acute Severe Asthma in PediatricsDocument53 pagesManagement of Acute Severe Asthma in PediatricsAmit AnandNo ratings yet
- I Am Sharing 'Case Study NCM 118' With YouDocument6 pagesI Am Sharing 'Case Study NCM 118' With YouQusai BassamNo ratings yet
- Management of Worsening Asthma Aand Exacerbation (Edit)Document32 pagesManagement of Worsening Asthma Aand Exacerbation (Edit)fenty nisaNo ratings yet
- 01-Obstractihe Pulmonary Diseases (Asthma) PDFDocument50 pages01-Obstractihe Pulmonary Diseases (Asthma) PDFsima.koye2005No ratings yet
- Management of Overdose of Aspirin, Paracetamol, Opioid, BenzodiazepineDocument19 pagesManagement of Overdose of Aspirin, Paracetamol, Opioid, BenzodiazepineRawan AlmutairiNo ratings yet
- Asthm Seminar 1Document38 pagesAsthm Seminar 1Sol Gat ChupataNo ratings yet
- Gold and Gina Guideline For Copd and AsthmaDocument56 pagesGold and Gina Guideline For Copd and AsthmaSomnath Das GuptaNo ratings yet
- Noninvasive Respiratory TherapiesDocument2 pagesNoninvasive Respiratory TherapiesFerreze AnnNo ratings yet
- center3rdMedicineSummary202620Practice20FilesPractice20Files2-20pulmonology PDFDocument33 pagescenter3rdMedicineSummary202620Practice20FilesPractice20Files2-20pulmonology PDFLaiba FatimaNo ratings yet
- Status AsthamaticusDocument40 pagesStatus AsthamaticusNazia ShamimNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD)Document12 pagesChronic Obstructive Pulmonary Disease (COPD)Marwan M.100% (1)
- Clinical Pharmacy Lectures on Asthma ManagementDocument66 pagesClinical Pharmacy Lectures on Asthma Managementgurrya786No ratings yet
- Status Asthmaticus!!!!!! PDFDocument13 pagesStatus Asthmaticus!!!!!! PDFKassandra Mildred GutierrezNo ratings yet
- ACUTE ASTHMA ATTACK EMERGENCY TREATMENTDocument31 pagesACUTE ASTHMA ATTACK EMERGENCY TREATMENTMuneeb YounisNo ratings yet
- Acute Severe Asthma Talk 2Document63 pagesAcute Severe Asthma Talk 2AdeyemoNo ratings yet
- Asthma Clinical Care GuidelinesDocument17 pagesAsthma Clinical Care GuidelinesWalaa MoustafaNo ratings yet
- Copd in Primary CareDocument27 pagesCopd in Primary CarerobyalfNo ratings yet
- Status Asthmaticus PDFDocument13 pagesStatus Asthmaticus PDFAtchiim Aif100% (1)
- CC Junsay Nicole Xyza T. Learning Interaction FormDocument10 pagesCC Junsay Nicole Xyza T. Learning Interaction FormNicole Xyza JunsayNo ratings yet
- Deteriorating PatientDocument39 pagesDeteriorating PatientDoc EddyNo ratings yet
- Aspiration SyndromesDocument16 pagesAspiration SyndromesAswathy RCNo ratings yet
- COPD CaseDocument5 pagesCOPD Caseshilanhiwa211No ratings yet
- Acute Severe AsthmaDocument61 pagesAcute Severe AsthmadrmsaqibNo ratings yet
- Common Pediatric Emergencies - A2Document46 pagesCommon Pediatric Emergencies - A2Ahmad JustNo ratings yet
- Prescribing Oxygen Therapy GuidelineDocument26 pagesPrescribing Oxygen Therapy Guidelinedanasli7607245No ratings yet
- COPD Treatment and Acute Exacerbation ManagementDocument22 pagesCOPD Treatment and Acute Exacerbation Managementsarwat86% (7)
- AsthmaDocument100 pagesAsthmaRoselle Louise L. PublicoNo ratings yet
- 19 Respiratory Renal and Hepatic Disease and AnaesthesiaDocument0 pages19 Respiratory Renal and Hepatic Disease and AnaesthesiajuniorebindaNo ratings yet
- 5-Diabetic and Respiratory DrugDocument24 pages5-Diabetic and Respiratory DrugAkmalia HardiniNo ratings yet
- Approach Considerations: Respiratory Acidosis Treatment & ManagementDocument8 pagesApproach Considerations: Respiratory Acidosis Treatment & Managementprince1500No ratings yet
- Triage - ARDS (Autosaved)Document35 pagesTriage - ARDS (Autosaved)Farhana Fefe Amani FeFeNo ratings yet
- Essential guide to intubation decisions and techniquesDocument6 pagesEssential guide to intubation decisions and techniquesWinnieChin LeeNo ratings yet
- Management of Poisoning and Drug Overdose - 2 PDFDocument24 pagesManagement of Poisoning and Drug Overdose - 2 PDFramadanNo ratings yet
- Asthma Lecture 2022Document32 pagesAsthma Lecture 2022grim reaperNo ratings yet
- Mnagment of Asthma in Adults and PediatricsDocument2 pagesMnagment of Asthma in Adults and Pediatricsmukhtar abddiNo ratings yet
- COPD Management and PrognosisDocument21 pagesCOPD Management and PrognosisMudrekaNo ratings yet
- Adrenaline Dosing and Effects in Cardiac ArrestDocument55 pagesAdrenaline Dosing and Effects in Cardiac ArrestinnyNo ratings yet
- Mnagment of Asthma in Adults and PediatricsDocument2 pagesMnagment of Asthma in Adults and Pediatricsmukhtar abddiNo ratings yet
- Brigham 2019 MCQsDocument13 pagesBrigham 2019 MCQsfarex100% (1)
- Clinical Toxicology: Management of A PoisonedpatientDocument57 pagesClinical Toxicology: Management of A Poisonedpatientnica velanoNo ratings yet
- Management of COPD2Document55 pagesManagement of COPD2frankozed1No ratings yet
- Pediatric Community Acquired PneumoniaDocument50 pagesPediatric Community Acquired PneumoniaggalicinaoNo ratings yet
- Assessing Patients For Oxygen Therapy: Figure. I May Be Jus..Document4 pagesAssessing Patients For Oxygen Therapy: Figure. I May Be Jus..Angeline Monilla Pante100% (1)
- Reversible Airflow ObstructionDocument2 pagesReversible Airflow Obstruction85robertNo ratings yet
- Respiratory Medicine 1 50Document33 pagesRespiratory Medicine 1 50Ahmed Kh. Abu WardaNo ratings yet
- COPD ExacerbationDocument2 pagesCOPD ExacerbationjusthoangNo ratings yet
- Management of Life Threatening Asthma. Severe Asthma Series. CHEST 2022Document10 pagesManagement of Life Threatening Asthma. Severe Asthma Series. CHEST 2022carla jazmin cortes rodriguezNo ratings yet
- Special Circumstances Guidelines ALSDocument19 pagesSpecial Circumstances Guidelines ALSHamzaMasoodNo ratings yet
- Recovery Room Care: BY Rajeev KumarDocument50 pagesRecovery Room Care: BY Rajeev Kumarramanrajesh83No ratings yet
- Palliative CareDocument4 pagesPalliative CaresobanNo ratings yet
- The Immunocompromised Patient Primary ImmunodeficienciesDocument2 pagesThe Immunocompromised Patient Primary ImmunodeficienciessobanNo ratings yet
- Malnutrition and InfectionDocument3 pagesMalnutrition and InfectionsobanNo ratings yet
- Adolescent NutritionDocument1 pageAdolescent NutritionsobanNo ratings yet
- Urinary Tract ObstructionDocument3 pagesUrinary Tract ObstructionsobanNo ratings yet
- Medicolegal Issues and STIsDocument3 pagesMedicolegal Issues and STIssobanNo ratings yet
- Antineoplastic SDocument20 pagesAntineoplastic SsobanNo ratings yet
- Rome III Diagnostic Criteria FGIDsDocument14 pagesRome III Diagnostic Criteria FGIDsPutu Reza Sandhya PratamaNo ratings yet
- Gastroenterology and AnaemiaDocument5 pagesGastroenterology and Anaemiasoban100% (1)
- Antiphospholipid SyndromeDocument4 pagesAntiphospholipid SyndromesobanNo ratings yet
- Vulval PainDocument3 pagesVulval PainsobanNo ratings yet
- Acr Omega LyDocument3 pagesAcr Omega LysobanNo ratings yet
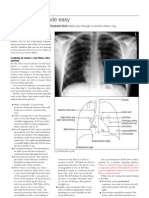
- Cara Membaca Foto Thoraks Yang BaikDocument2 pagesCara Membaca Foto Thoraks Yang BaikIdi Nagan RayaNo ratings yet
- Autonomic & NeuromuscularDocument20 pagesAutonomic & Neuromuscularzeina32No ratings yet
- Case Scenarios Nutrition Growth and DevelopmentDocument4 pagesCase Scenarios Nutrition Growth and DevelopmentsobanNo ratings yet
- The Wheezing InfantDocument4 pagesThe Wheezing InfantsobanNo ratings yet
- Non Epileptic Causes of Loss of ConsciousnessDocument3 pagesNon Epileptic Causes of Loss of ConsciousnesssobanNo ratings yet
- Analgesic & AntimigraineDocument12 pagesAnalgesic & AntimigraineChin ChanNo ratings yet
- What's New in Respiratory DisordersDocument4 pagesWhat's New in Respiratory DisorderssobanNo ratings yet
- Disorders of PubertyDocument2 pagesDisorders of PubertysobanNo ratings yet
- The Management of Acute Renal FailureDocument4 pagesThe Management of Acute Renal Failuresoban100% (1)
- Drugs That Damage The LiverDocument5 pagesDrugs That Damage The LiversobanNo ratings yet
- Neuro DegenerativeDocument11 pagesNeuro DegenerativesobanNo ratings yet
- Haemo Chroma To SisDocument4 pagesHaemo Chroma To SissobanNo ratings yet
- Neuro DegenerativeDocument11 pagesNeuro DegenerativesobanNo ratings yet
- Renal Disease and PregnancyDocument4 pagesRenal Disease and PregnancysobanNo ratings yet
- What Is DiabetesDocument2 pagesWhat Is DiabetessobanNo ratings yet
- Contraception: What's New in ..Document4 pagesContraception: What's New in ..sobanNo ratings yet
- AppendixC NutrientChartDocument5 pagesAppendixC NutrientChartArianne Nicole LabitoriaNo ratings yet
- Whats New in Asthma and COPDDocument3 pagesWhats New in Asthma and COPDsobanNo ratings yet
- ARIA guidelines improve care for allergic rhinitis and asthmaDocument14 pagesARIA guidelines improve care for allergic rhinitis and asthmazeegerzNo ratings yet
- Asthma: Done by Group 4 (Abdrahman, Kalad, Sultan) Dr. Mohammad Tarique EmamDocument13 pagesAsthma: Done by Group 4 (Abdrahman, Kalad, Sultan) Dr. Mohammad Tarique EmamSO SNo ratings yet
- Leaflet Bricanyl TurbohalerDocument7 pagesLeaflet Bricanyl TurbohalerKrisna SyammaNo ratings yet
- FoPE MAPEH 7Document3 pagesFoPE MAPEH 7Charleen Anne ValdezNo ratings yet
- TOEFL EssaysDocument12 pagesTOEFL EssaysYamFerreira100% (1)
- Peak Flow MeterDocument3 pagesPeak Flow MeterNicole PramonoNo ratings yet
- Test Bank For Human Diseases 3rd Edition NeighborsDocument24 pagesTest Bank For Human Diseases 3rd Edition NeighborsBarbaraHernandezimgf100% (44)
- Aafa 2021 Asthma Capitals ReportDocument41 pagesAafa 2021 Asthma Capitals ReportWXYZ-TV Channel 7 DetroitNo ratings yet
- Journal On Respiratory Disorders in PregnancyDocument7 pagesJournal On Respiratory Disorders in PregnancyallyssaNo ratings yet
- Pulmonary and Respiratory Nursing Assessment GuideDocument48 pagesPulmonary and Respiratory Nursing Assessment GuideEmjay JapitanaNo ratings yet
- Smart Asthma InhalerDocument4 pagesSmart Asthma Inhalerchirag suresh chiruNo ratings yet
- Reviews: Lung Function Testing Assessment by Impulse Oscillometry in Chronic Lung DiseaseDocument7 pagesReviews: Lung Function Testing Assessment by Impulse Oscillometry in Chronic Lung DiseaseCristiana LibuNo ratings yet
- (13384139 - Acta Medica Martiniana) Bronchial Asthma - Current Trends in TreatmentDocument9 pages(13384139 - Acta Medica Martiniana) Bronchial Asthma - Current Trends in TreatmentteuuuuNo ratings yet
- Trisodium Phosphate Data-SheetDocument4 pagesTrisodium Phosphate Data-Sheetgauravalok85No ratings yet
- JCM 08 01283 v2Document44 pagesJCM 08 01283 v2Ambika SuwalNo ratings yet
- Newborn Tachypnea GuideDocument14 pagesNewborn Tachypnea GuideMarielaTessyGonzalesParedesNo ratings yet
- NoseDocument7 pagesNoseJoshua BrownNo ratings yet
- A Comparative Study of Two Nebulizers in The Emergency Department Breath-Actuated Nebulizer and Handheld NebulizerDocument7 pagesA Comparative Study of Two Nebulizers in The Emergency Department Breath-Actuated Nebulizer and Handheld Nebulizerfachrudin arNo ratings yet
- التدريب الصيفي محلولهDocument129 pagesالتدريب الصيفي محلولهMohamed MosawiNo ratings yet
- Benefits of TulsiDocument13 pagesBenefits of TulsiBIKRAM KUMAR BEHERANo ratings yet
- Key Changes Gold 2023 2Document16 pagesKey Changes Gold 2023 2Muhammad Nur Ardhi LahabuNo ratings yet
- WP Contentuploads202305GINA 2023 Full Report 2023 WMS PDFDocument246 pagesWP Contentuploads202305GINA 2023 Full Report 2023 WMS PDFJaquelin GarciaNo ratings yet
- Bronchial AsthmaDocument16 pagesBronchial AsthmaSHAIK SHABEENA100% (1)
- Mexican Asthma Guidelines GUIMA 2017Document131 pagesMexican Asthma Guidelines GUIMA 2017Merk100% (1)
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocument21 pagesWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDeniNo ratings yet
- เฉลยข้อสอบ MCQ R2ครั้งที่2Document362 pagesเฉลยข้อสอบ MCQ R2ครั้งที่2Kareem Sukwihan100% (2)
- Cough Management: A Practical ApproachDocument13 pagesCough Management: A Practical ApproachJonathan OverianNo ratings yet
- WLP - Q4 - Music 10 - Week 4Document8 pagesWLP - Q4 - Music 10 - Week 4Gladys GutierrezNo ratings yet
- Randomised Comparison of Intravenous Magnesium Sulphate, Terbutaline and Aminophylline For Children With Acute Severe AsthmaDocument7 pagesRandomised Comparison of Intravenous Magnesium Sulphate, Terbutaline and Aminophylline For Children With Acute Severe AsthmaRosi NadilahNo ratings yet