Brain MRI Sequences
08/21/2015
1. Sequences
a. Dominant weighting
b. Modifiers
2. T1 and T2-weighted
a. Two fundamental anatomic sequences
b. T1 TR short and TE short (repetition time, echo time)
c. T2 TR long and TE long
d. Best way to differentiate is the relationship between gray matter
and white matter
i. T1 gray matter is gray (hypointense) and white matter is
white (hyperintense)
1. Hyperintense on T1: blood product, fat, proteinaceous
material and contrast enhancement
ii. T2 gray matter is white and white matter is gray
3. Proton-density
a. Intermediate sequence characterized by long TR but short TE
b. Makes white matter lesions easier to identify than on T2 and T1
c. Not used as much anymore because it has been superseded by
FLAIR
�i. However, this is used still in other parts of the body
(particularly MSK)
4. C+
a. Gadolinium-enhanced
b. Administer contrast and then perform T1-weighted sequences
c. E.g. in a thalamic primary brain tumor
i. Hemorrhagic change intrinsically high signal in T1
ii. Another component of it demonstrates contrast-enhancement
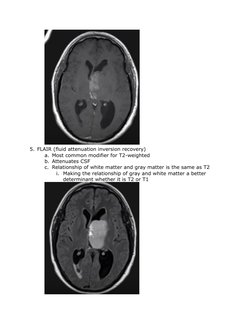
�5. FLAIR (fluid attenuation inversion recovery)
a. Most common modifier for T2-weighted
b. Attenuates CSF
c. Relationship of white matter and gray matter is the same as T2
i. Making the relationship of gray and white matter a better
determinant whether it is T2 or T1
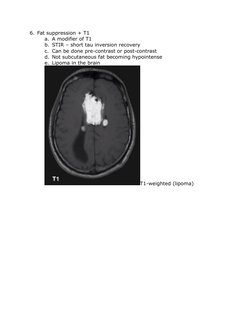
�6. Fat suppression + T1
a. A modifier of T1
b. STIR short tau inversion recovery
c. Can be done pre-contrast or post-contrast
d. Not subcutaneous fat becoming hypointense
e. Lipoma in the brain
T1-weighted (lipoma)
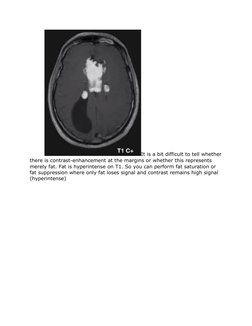
�It is a bit difficult to tell whether
there is contrast-enhancement at the margins or whether this represents
merely fat. Fat is hyperintense on T1. So you can perform fat saturation or
fat suppression where only fat loses signal and contrast remains high signal
(hyperintense)
�You can see at the
margins that theres only very minimal contrast enhancement with the bulk
of the tumor completely attenuating out. Note that it is the subcutaneous fat
that becomes dark and the scalp remaining bright post contrast
Note: fat-saturated post-contrast T1 sequences are routine in most
parts of the body because of the presence of significant amounts of fat. This
is not the case in the brain where fat is an abnormal substance. And as such
for purely parenchymal lesions fat saturation is not usually performed. The
exception to this is intracranial masses that are involving the skull or skull
base where an extracranial extension is being sought. So the most common
situation for this to be performed is in base of skull meningiomas or CPA
masses where potential for extracranial spread is present
7. Fat suppression + T2
a. Performed as part of a gradient echo sequence where the intention
is not particularly to suppress fat, but to make it more susceptible
to paramagnetic effects
�b. In the orbits, or base of the skulls, to examine structures that are
otherwise closely related to fat
i. Common in the case of orbits where the extraocular muscles
and optic nerve are surrounded by fat and that examining for
abnormal signal within either of those structures is much more
easily performed with fat attenuation
c. For intracranial imaging, also important in looking for CSF leak
�8. Susceptibility weighted (SWI)
a. Represent a number of different sequences that share the
propensity to have signal loss due to paramagnetic or diamagnetic
effects
b. Calcium or blood product will result in dark or black signal
c. Exquisitely sensitive to very small amounts of such materials
d. Photo below: familial autosomal dominant multiple cavernoma
syndrome
i. If you look at the T1 or T2 sequences, these abnormalities
would be much smaller
ii. The phenomenon is called blooming: signal loss extends
beyond the anatomical confines of the lesion due to the fact
that paramagnetic or diamagnetic materials distort the
magnetic field locally beyond their margins
e. SWI at higher field strengths are particularly sensitive
�f. Susceptibility sensitive sequences gradient echo imaging
g. May deserve their own column but placed under T2-weighted
because many of these are T2* weighted
9. Diffusion weighted imaging
�a. Encompass DWI (or isotropic imaging) and ADC; can include
diffusion tensor imaging
b. DWI
i. Dirty sequence made up of both diffusion information and T2
information
ii. Examining DWI alone can lead you to erroneously interpret
high signal as representing true abnormal restricted diffusion
when in fact what you are seeing is so called T2 shine-through
10.
Apparent Diffusion Coefficient
a.
�11.
Diffusion tensor
a. Allows for tractography
b. Research based or operative planning
�12.
Flow sensitive sequences
a. MR angiography
i. Usually without intravenous contrast and relies on blood
bringing with it signal
ii. Usually shown as MIPs
1. Because there is little background for the vessels to be
localized against, it can be difficult to know exactly
where one is on a single image
iii. Photo: young patient with vein of Galen malformation
�b. MR
i.
ii.
iii.
venography
Can use phase contrast or similar to MR angiography
For dural venous sinuses or cerebral veins
Photo: dural venous thrombosis (posterior part of the superior
sagittal sinus)
c. CSF flow studies
�i. Same principles as phase contrast venography can be used to
look at the pulsatile flow of CSF in cisterns and aqueduct as
shown in photo
ii. Can be useful to exclude aqueduct stenosis or hyperdynamic
flow of normal pressure hydrocephalus needs to be evaluated
13.
Miscellaneous
a. MR spectroscopy
i. Performed routinely as part of brain tumor or mass work up
�b. Functional MRI
i. Image during memory or verbal tasks
c. MR Perfusion
i. Routine in assessment of tumors and neurodegenerative
conditions
�14.
Summary table