Professional Documents
Culture Documents
Blefaritis
Uploaded by
Rully Febri AnggoroCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blefaritis
Uploaded by
Rully Febri AnggoroCopyright:
Available Formats
a r c h s o c e s p o f t a l m o l .
2 0 1 5;9 0(3):112118
ARCHIVOS DE LA SOCIEDAD
ESPAOLA DE OFTALMOLOGA
www.elsevier.es/oftalmologia
Original article
Comparative study of the efcacy of different treatment
options in patients with chronic blepharitis
a , D. Cibils a , F. Laspina a , R. Sanabria a ,
M. Arra a , M. Samudio a, , N. Farina
L. Carpinelli a , H. Mino de Kaspar b
a
b
National University of Asuncin, Asuncin, Paraguay
Ludwig-Maximilians University, Munich, Germany
a r t i c l e
i n f o
a b s t r a c t
Article history:
Objective: To compare the efcacy of 3 treatment options in patients with chronic blepharitis.
Received 4 June 2013
Methodology: An experimental, randomized, controlled study was conducted on 45 patients
Accepted 17 September 2013
(female 67%; mean age: 40.5 years) diagnosed with chronic blepharitis, in order to compare
Available online 14 April 2015
the effectiveness of three treatment options. Group 1: eyelid hygiene with neutral shampoo
three times/day; group 2: neutral shampoo eyelid hygiene plus topical metronidazole gel
Keywords:
0.75% twice/day; group 3: neutral eyelid hygiene with shampoo plus neomycin 3.5% and
Chronic blepharitis
polymyxin 10% antibiotic ointment with 0.5% dexamethasone 3 times/day. The symptoms
Demodex folliculorum
and signs were assessed by assigning scores from 0: no symptoms and/or signs; 1: mild
Metronidazole gel
symptoms and/or signs, 2: moderate symptoms and/or signs; and 3: severe symptoms and/or
Eyelid hygiene
signs.
Neutral shampoo
Results: A signicant improvement was observed in the signs and symptoms in all 3 treatment groups. While groups 1 and 2 had more improvement in all variables studied (P < .05),
Group 3 showed no clinical improvement for itching (P = .16), dry eye (P = .29), eyelashes
falling (P = .16), and erythema at the eyelid margin (P = .29).
Conclusions: Shampoo eyelid hygiene neutral and neutral shampoo combined with the use of
metronidazole gel reported better hygiene results than neutral shampoo lid with antibiotic
ointment and neomycin and polymyxin dexamethasone.
2013 Sociedad Espanola
de Oftalmologa. Published by Elsevier Espaa, S.L.U. All rights
reserved.
Estudio comparativo de la ecacia de diversas modalidades teraputicas
en pacientes con blefaritis crnica
r e s u m e n
Palabras clave:
Objetivo: Comparar la ecacia de 3 modalidades de tratamiento en pacientes con blefaritis
Blefaritis crnica
crnica.
Demodex folliculorum
Metodologa: Se realiz un estudio experimental, aleatorizado y controlado en 45 pacientes
Gel de metronidazol
(sexo femenino: 67%; edad media: 40.5 anos)
con diagnstico de blefaritis crnica para
N, Cibils D, Laspina F, Sanabria R, et al. Estudio comparativo de la ecacia de
Please cite this article as: Arra M, Samudio M, Farina
diversas modalidades teraputicas en pacientes con blefaritis crnica. Arch Soc Esp Oftalmol. 2015;90:112118.
Corresponding author.
E-mail address: microbiologia@iics.una.py (M. Samudio).
2173-5794/$ see front matter 2013 Sociedad Espanola
de Oftalmologa. Published by Elsevier Espaa, S.L.U. All rights reserved.
113
a r c h s o c e s p o f t a l m o l . 2 0 1 5;9 0(3):112118
Higiene palpebral
comparar la ecacia de 3 modalidades de tratamiento. Grupo 1: higiene palpebral con
Champ neutro
champ neutro 3 veces/da; grupo 2: higiene palpebral con champ neutro y gel tpico de
metronidazol al 0,75% 2 veces/da; grupo 3: higiene palpebral con champ neutro y pomada
antibitica de neomicina al 3,5% y polimixina al 10% con dexametasona al 0,5% 3 veces/da.
Los sntomas y signos fueron valorados asignndoles puntuaciones entre 0: sin sntomas ni
signos; 1: sntomas o signos leves; 2: sntomas o signos moderados y 3: sntomas o signos
severos.
Resultados: En los 3 grupos de tratamiento se observ mejora signicativa de los signos
y sntomas. Mientras que los grupos 1 y 2 presentaron una mayor mejora en todas las
variables estudiadas (p < 0,05), el grupo 3 no present mejora clnica para comezn (p = 0,16),
ojo seco (p = 0,29), cada de pestanas
(p = 0,16) ni eritema en el borde palpebral (p = 0,29).
Conclusin: La higiene palpebral con champ neutro y el uso combinado de champ neutro
con gel de metronidazol reportaron mejores resultados que la higiene palpebral con champ
neutro y pomada antibitica de neomicina y polimixina con dexametasona.
de Oftalmologa. Publicado por Elsevier Espaa, S.L.U. Todos
2013 Sociedad Espanola
los derechos reservados.
Introduction
Blepharitis is a very common disease in the ophthalmological practice. It normally courses chronically with intermittent
symptom exacerbations. Generally, it is classied as acute and
chronic, the former being caused by a bacterial infection and
the latter by the involvement of the Meibomium glands.1,2
Blepharitis is commonly associated to systemic diseases
such as rosaceae and seborrheic dermatitis. Some studies
relate it to the presence of Demodex folliculorum (D. folliculorum)
which perpetuates the inammatory process at the follicular
level.36
Even though the treatment of chronic blepharitis remains
controversial, neutral shampoo cleaning has been the most
widely accepted medical therapy in our environment, followed
by the use of antibiotic ointment with 3.5% neomycin and 10%
polymixin with 0.5% dexamethasone.7,8 Said combination is
used because it has demonstrated to produce improvements
for patients with acute conditions in clinical practice, although
the presence of corticoids inhibits chronic use of said ointment
due to its potential collateral effects. The use of ointments
based exclusively on antibiotics has not demonstrated to be
effective in the treatment of chronic blepharitis as it does
not address the root cause, to which we must add the toxicity of antibiotics which could give rise to undesirable side
effects. The application of 0.75% metronidazol topical gel has
demonstrated a signicant reduction symptom as well as a
50% reduction in infestation by D. folliculorum.9,10
Apparently, metronidazole reduces the hydrogen peroxide
and hydroxyl radical levels, both powerful oxidants which can
cause tissue damage. For this reason, its effects would the
mainly anti-inammatory instead of antimicrobial.9,10 The
majority of North American and European studies recommend
the use of 2% yellow mercury oxide for treating chronic blepharitis. However, this type of treatment is not affordable for
the majority of patients in our environment due to its cost.11
The internacional workshop for the treatment of Meibomium gland dysfunctions established a clinical classication system for assessing the severity of this dysfunction
and a treatment algorithm based on the stages of this disease. For stages 1 and 2, corresponding to asymptomatic
patients or those having very slight symptoms, it was recommended to optimize the working environment, increase
consumption of omega-3, carry out palpebral hygiene with
warm pads followed by massage and expression of Meibomium gland secretions. Stages 3 and 4, corresponding to
patients with moderate and notable symptoms, the same recommendations for phase 1 and 2 apply together with the use
of lubricants, topical acytromycin, oral tetracycline derivates
and anti-inammatory therapy for dry eye.1214
The majority of chronic blepharitis treatments have
demonstrated signicant reductions in the amount of infection by the parasite. However, the only treatment which was
able to diminish the D. folliculorum count to zero is tea tree oil
(Melaleuca alternifolia), a therapeutic mode which is not available in our environment.15,16
In our country, even though chronic blepharitis is diagnosed with relative frequency, no data has been published on
the medical therapy evaluations implemented for this disease,
which increases the importance of the present report. Accordingly, the objective of this study consisted in comparing the
efcacy of 3 treatment schemes applied for chronic blepharitis: (1) palpebral hygiene with neutral shampoo; (2) palpebral
hygiene with neutral shampoo and 0.75% metronidazole topical gel; and (3) palpebral hygiene with neutral shampoo and
3.5% neomycin antibiotic ointment and 10% polymixin with
0.5% dexamethasone, as well as assessing the clinical and
microbiological characteristics of patients with chronic blepharitis and clinical improvements 2 months after beginning
treatment between the various groups of the study.
Materials and methods
A randomized, experimental design control study with
patients of both sexes over 16 years of age with chronic
blepharitis diagnostic who visited the Ophthalmology Department of the Hospital de Clnicas of the Medical Sciences
College of the National University of Asuncin. Each patient
was given a clear explanation of the objective of the study,
pointing out that the treatments did not involve any risk to
health and were already in use but had never been assessed
in our environment. It was also pointed out that lab tests
114
a r c h s o c e s p o f t a l m o l . 2 0 1 5;9 0(3):112118
would not represent additional expenses for them. After signing the informed consent, samples were taken of the patients
and sent to the microbiology laboratory. The study protocol
was approved by the Ethics Committee for Research of the
institution.
Chronic blepharitis was dened by the presence of 3 or
more of the following characteristics. Burning feeling, foreign
body or irritation; sheathing of eyelashes, telangiectasia in the
palpebral edge, foamy secretion, slight or moderate papillary
hyperemia or hypertroa of the palpebral conjunctival or Meibomium glands. The study excluded patients with additional
acute or chronic ocular diseases (corneal, conjunctival, palpebral, lacrimal pathways), those with applied topical treatment
during the month before samples were taken or with oral
treatment involving metronidazole, isotretinoin or other medications which could interfere with the density of parasites, as
well as patients who did not return for the control examinations. The patients were recruited from the outpatient practice
of the aforementioned Ophthalmology Department and were
assigned randomly to the different groups.
Group 1: 15 patients who were treated with palpebral
hygiene with neutral shampoo 3 times a day; Group 2: 15
patients who were treated with palpebral hygiene with neutral
shampoo and topical gel 0.75% metronidazolee 2 times a day;
Group 3: 15 patients who were treated with palpebral hygiene
with neutral shampoo and 3.5% neomycin antibiotic ointment
and 10% polymixin with 0.5% dexamethasone 3 times a day.
Control visits were scheduled for day 15, 30 and 60 after establishing the treatment. In said visits, the appropriate variables
were measured.
Palpebral hygiene comprised cleaning both palpebral edges
with cotton swabs impregnated with neutral shampoo diluted
in water, followed by warm compresses and massage with
expression of the Meibomium gland points during 15 min.
A prearranged questionnaire was given to the patients
when taking the samples as well as 2 months after establishing treatment. The questionnaire included demographic
data (sex, age) and demographic data (dermatological diseases, symptoms and signs).
Due to the subjectivity involved in the assessment of symptoms and signs, a score of 0 to 3 was devised to measure
severity, considering 0 as no symptoms or signs; 1, slight
symptoms or signs; 2, moderate symptoms or signs; and
3, severe symptoms or signs. Subsequently, the score of each
variable was added up to obtain a mean value that was utilized
for the statistical analysis.
In order to determine the presence of causing agents, 6 eyelashes were removed from the eye of each individual which
exhibited more signs of chronic anterior or posterior blepharitis, alternating between the lower and upper eyelid. Said
eyelashes were placed in a recipient to which 10% potassium
hydroxide (KOH) was added for parasitologic and mycologic
analysis under microscope at 40. The palpebral edge of both
eyes was scraped with a kimura spatula to obtain samples
for bacteriological studies in 5% sheep blood agar in CO2 ;
the fungus culture was made in sabouraud agar. Isolation
and identication of germs was performed with conventional
microbiological methods.
The data were analyzed by means of the Epi-Info
2002 statistical application (CDC, Atlanta, United States).
Analytical statistics were applied for processing data, using
the KruskalWallis test for comparing mean values, taking a
value of p < 0.05 as statistically signicant.
Results
Overall, 45 subjects which fullled all the controls were
included in the study. As regards gender, the female sex (67%)
and city dwellers (69%). The mean age was of (range from
17 to 87 years). As regards personal pathological history, 7
patients (15.5%) referred dermatological history of rosaceae
(Table 1).
Of the 45 examined patients, parasitological and bacteriological isolation could be carried out in 28 (62.2%). Of these,
15 patients (54%) were positive for D. folliculorum. In turn, bacterial isolation was obtained in 26 patients (92.8%). As for
isolated bacteria, negative coagulase Staphylococcus was isolated in 21 patients (75%), Staphylococcus aureus in 3 (11%) and
Streptococcus pneumoniae in 2 (7%).
Table 2 shows the distribution of signs and symptoms
according to severity and average score. It can be seen that
the mean of the higher scores corresponded to burning (2.4),
sheathing of eyelashes (2.4), irritation (2.2), erythema or palpebral edema (2.2), hypertroa of the papilla or the Meibomium
gland (1.2), foreign body feeling (1.9), presence of scales or
crusts (1.9) and foamy secretion (1.9).
No signicant differences were found when comparing the
baseline average scores between the study groups in any of
the studied signs and symptoms (Table 3).
When comparing symptoms and signs between the different groups at baseline and at the end of the study,
improvements were observed in all study groups for all the
variables in groups 1 and 2. In group 3, no improvement was
observed in eyelashes (p = 0.527), or in telangiectasia at the
palpebral edge (p = 0.894) (Table 4).
Table 5 compares the average posttreatment scores of
patients for each variable of the study.
Fig. 1 shows the overall scores of signs and symptoms
before and after the treatment. Even though signicant reductions were observed in the 3 groups, group 3 exhibited the
lowest improvement.
In what concerns the effects of infestation by Demodex
sp. on the efcacy of the treatment, it was not possible to
reach a conclusion due to the small number of the sample.
It was observed that patients with Demodex sp. in the group
that was administered metronidazole exhibit greater improvement than those who did not have said parasite (Fig. 2).
Discussion
Chronic blepharitis is a worldwide public health problem due
to its high prevalence, chronicity and resistance to treatment.
As described above, there are multiple treatment options for
this multifactor disease although none has demonstrated
healing capacities. Recurrence rates are very high and treatments are generally lifelong.
Shulman et al.7 concluded that the combined use of 3.5%
neomycin and 10% polymixyn with 1% dexamethasone was
more efcient than the sole use of 1% dexamethasone for
115
a r c h s o c e s p o f t a l m o l . 2 0 1 5;9 0(3):112118
Table 1 General characteristics of patients with chronic blepharitis.
Characteristics
Sex
Female
Male
Mean age (range)
Age group
1739
4059
60
Group 1
n (%)
Group 2
n (%)
10
5
45 (3087)
8
7
34 (1772)
12
3
34 (2070)
30 (66)
15 (33)
34 (1787 years)
10
3
2
11
3
1
26 (58)
14 (31)
5 (11)
5
8
2
Group 3
n (%)
Total
n (%)
Origin
Urban
Rural
Pathological antecedents
DM
Allergy
Asthma
Acne
Rosaceae
Demodex folliculorum
31 (69)
14 (31)
1
1
2
0
3
6
1
2
1
1
0
3
0
2
0
2
4
6
2 (4.4)
3 (6.7)
3 (6.7)
3 (6.7)
7 (15.6)
15/28 (54.0)
n = 45.
Group 1: palpebral hygiene with neutral shampoo 3 times/day; Group 2: palpebral hygiene with neutral shampoo and topical 0.75% metronidazole
gel 2 times/day; Group 3: palpebral hygiene with neutral shampoo and antibiotic cream comprised of 3.5% neomycin and 10% polymixin with
0.5% dexamethasone 3 times/day.
bacterial control and symptom reduction in chronic blepharitis patients, although its prolonged use could have toxic effects
on the ocular surface due to the presence of neomycin sulfate.
Demmler8 compared the use of 2% mercury oxide and lindane, which is a neutral lotion for palpebral hygiene versus the
use of combined corticoids with antibiotics, demonstrating
higher reduction of Demodex in patients who applied the neutral lotion and 2% mercury oxide. However, patients reported
difculties in the application and toxicity of the mercury
oxide, which must be applied very carefully to avoid contact with conjunctival mucosa. In turn, Junk et al.9 reported
one case of symptom improvement in a patient with chronic
blepharitis due to Demodex who was allergic to mercury oxide
and resistant to topically applied antibiotics. Barnhorst10 compared the use of palpebral hygiene and topical application
of metronidazole versus palpebral hygiene on its own, as
control group, in patients with rosaceae and chronic blepharitis, demonstrating clinical improvement in palpebral signs
and symptoms although no signicant improvements in ocular surface discomfort. No adverse effects were observed in
the treatment with metronidazole. Czepita5 found a reduction in the presence of D. folliculorum and Demodex brevis in
patients treated with 2% metronidazole versus other therapeutic modalities.
Table 2 Signs and symptoms of patients with chronic blepharitis.
Symptoms/signs
Burning
Sheathing of eyelashes
Itching
Erithema or palpebral edema
Hypertrophia of papilla or the Meibomium gland
Foreign body feeling
Presence of crusts or scale
Foamy secretion
Pruritus
Dry eye feeling
Fallen eyelashes
Telangiectasiae in the palpebral edge
Poliosis
Trichiasis
n = 45.
None
0
1
0
0
4
0
4
1
8
9
8
22
42
34
32
Slight
1
5
12
7
8
4
9
15
5
7
11
9
2
5
7
Moderate
2
12
18
23
19
18
18
16
17
20
19
8
1
6
5
Severe
3
Average score
27
15
15
14
23
14
13
15
9
7
6
0
0
1
2.4
2.4
2.2
2.2
2.1
1.9
1.9
1.9
1.6
1.6
1.0
0.1
0.1
0.1
116
a r c h s o c e s p o f t a l m o l . 2 0 1 5;9 0(3):112118
Table 3 Inter-group comparison of the baseline average scores on symptoms and signs of patients with chronic
blepharitis.
Symptoms/signs
Group 2
n = 15
Group 1
n = 15
Burning
Sheathing of eyelashes
Itching
Palpebral erythema or edema
Hypertrophia of the papilla or the Meibomium gland
Foreign body feeling
Presence of crusts or scale
Foamy secretion
Pruritus
Dry eye feeling
Fallen eyelashes
Telangiectasiae in the palpebral edge
Poliosis
Trichiasis
2.2
2.5
2.2
2.2
2.0
2.1
1.9
1.8
1.6
1.5
1.1
0.1
0.5
0.2
Group 3
n = 15
2.4
2.4
2.1
1.9
2.1
1.8
1.9
1.8
1.8
1.5
0.8
0.1
0.5
0.5
2.7
2.3
2.2
2.5
2.1
1.9
1.9
2.0
1.4
1.6
1.0
0.1
0.5
0.5
0.2
0.7
0.9
0.7
0.9
0.6
1.0
0.8
0.5
1.0
0.7
1.0
1.0
0.5
Group 1: palpebral hygiene with neutral shampoo 3 times/day; Group 2: palpebral hygiene with neutral shampoo and topical 0.75% metronidazole gel 2 times/day; Group 3: palpebral hygiene with neutral shampoo and 3.5% neomycin antibiotic ointment and 10% polymixin with 0.5%
dexamethasone 3 times/day.
p: KruskalWallis test.
In the present experimental study, signicant improvements were observed in the studied variables when comparing
baseline and the results of treatment after 2 months in the
3 groups of the study, matching several published studies58
in what concerns efcacy of each administered treatment. As
for the most effective treatment, it is concluded that treatments with nutrition pool 3 times a day and with nutrition
pool and 0.75% metronidazole topical gel twice a day one
of the treatments which exhibited the best improvement of
assessed symptoms and signs, similar to the results reported
by Czepita5 and Barnhorst,10 nding statistically signicant
values (p < 0.05) for all the studied variables. The treatment
with neutral shampoo and antibiotic ointment with 3.5%
neomycin and 10% polymyxin with 0.5% dexamethasone 3
times a day exhibited signicant improvements in the studied
variables with the exception eyelashes loss and telangiectasia
in the palpebral edge. These differences could be mainly due to
higher patient compliance with simpler treatments as cleaning with neutral shampoo or the use of ointments with lesser
frequency against metronidazole gel with antibiotics and corticoids ointment, as well as the higher toxicity and side effects
associated to the latter.
Even though corticoids exhibit higher anti-inammatory
effect than that reported for metronidazole, these only act in
Table 4 Inter-group comparison of the average scores on symptoms and signs of patients with chronic blepharitis
before and after treatment.
Symptoms/signs
Burning
Sheathing of eyelashes
Itching
Palpebral erythema or edema
Hypertrophia of the papilla or the Meibomium gland
Foreign body feeling
Presence of crusts or scale
Foamy secretion
Pruritus
Dry eye feeling
Fallen eyelashes
Telangiectasiae in palpebral edge
Poliosis
Trichiasis
Group 1
Pre
Post
2.2
2.5
2.2
2.2
2.0
2.1
1.9
1.8
1.6
1.5
1.1
0.1
0.5
0.2
0.3
0.3
0.5
0.6
0.6
0.3
0.7
0.5
0.2
0.4
0.6
0.0
0.4
0.1
Group 2
p
Pre
Post
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
0.0003
0.0234
0.0234
0.0234
2.4
2.4
2.1
1.9
2.1
1.8
1.9
1.8
1.8
1.5
0.8
0.1
0.5
0.5
0.7
0.9
0.5
0.9
0.6
0.5
0.5
0.5
0.2
0.7
0.3
0.1
0.2
0.2
Group 3
p
Pre
Post
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
0.0354
<0.0001
<0.0001
2.7
2.3
2.2
2.5
2.1
1.9
1.9
2.0
1.4
1.6
1.0
0.1
0.5
0.5
1.5
1.4
0.9
1.1
1.5
1.3
1.3
1.4
0.8
0.9
0.6
0.1
0.2
0.2
p
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
<0.0001
0.527
0.894
<0.0001
<0.0001
Group 1: palpebral hygiene with neutral shampoo 3 times/day; Group 2: palpebral hygiene with neutral shampoo and topical 0.75% metronidazole gel 2 times/day; Group 3: palpebral hygiene with neutral shampoo and 3.5% neomycin antibiotic ointment and 10% polymixin 0.5% with
dexamethasone 3 times/day.
Paired t test for comparing pre- and post-treatment.
117
a r c h s o c e s p o f t a l m o l . 2 0 1 5;9 0(3):112118
Table 5 Inter-group comparison of the average scores on symptoms and signs of patients with chronic blepharitis
2 months after treatment.
Symptoms/signs
Group 2
n = 15
Group 1
n = 15
Burning
Sheathing of eyelashes
Itching
Palpebral erythema or edema
Hypertrophia of the papilla or the Meibomium gland
Foreign body feeling
Presence of crusts or scale
Foamy secretion
Pruritus
Dry eye feeling
Fallen eyelashes
Telangiectasiae in the palpebral edge
Poliosis
Trichiasis
0.3
0.3
0.5
0.6
0.6
0.3
0.7
0.5
0.2
0.4
0.6
0.0
0.4
0.1
p*
Group 3
n = 15
0.7
0.9
0.5
0.9
0.6
0.5
0.5
0.5
0.2
0.7
0.3
0.1
0.2
0.2
1.5
1.4
0.9
1.1
1.5
1.3
1.3
1.4
0.8
0.9
0.6
0.1
0.2
0.2
<0.001
<0.001
0.161
0.296
<0.001
<0.001
0.002
0.002
<0.001
0.295
0.169
0.350
0.808
0.350
Group 1: palpebral hygiene with neutral shampoo 3 times/day; Group 2: palpebral hygiene with neutral shampoo and topical 0.75% metronidazol gel 2 times/day; Group 3: palpebral hygiene with neutral shampoo and 3.5% neomycin antibiotic cream and 10% polymixin with 0.5%
dexamethasone 3 times/day.
KruskalWallis test.
case of extreme inammation and chronic use gives rise to
adverse effects which are damaging at the ocular level and
the palpebral surface. This diminishes its efcacy for continued use, as observed in the present study. Considering that
blepharitis is a chronic and benign disease, corticoids should
be used only for severe inammation and for complications
associated to blepharitis, such as marginal ulcers and in the
phlyctenules.
The number of patients per group was limited because the
study was carried out in a public hospital visited by patients
with lower resources who do not always return for controls
and for the necessary follow-up for inclusion in the study. In
30
Total score
20
Treatment
10
Pre
Post
0
No. = 15
15
15
15
15
15
Study group
Fig. 1 Comparison of the overall signs and symptoms
score between the groups of the study and within the
group, pre- and postreatment. Group 1: palpebral hygiene
with neutral shampoo 3 times/day; Group 2: palpebral
hygiene with neutral shampoo and topical gel 0.75%
metronidazole 2 times/day; Group 3: palpebral hygiene with
neutral shampoo and antibiotic cream comprised of 3.5%
neomycin and 10% polymixin with 0.5% dexamethasone 3
times/day.
Difference between pre and post treatment
40
30
20
10
Demodex
Absence
Presence
10
No. = 3
Study group
Fig. 2 Comparison of the difference before and after
treatment of the overall signs and symptoms scores
between the groups of the study, classied by infestation
with Demodex sp. Group 1: palpebral hygiene with neutral
shampoo 3 times/day; Group 2: palpebral hygiene with
neutral shampoo and topical 0.75% metronidazole gel 2
times/day; Group 3: palpebral hygiene with neutral
shampoo and antibiotic cream comprised of 3.5% neomycin
and 10% polymixin with 0.5% dexamethasone 3 times/day.
118
a r c h s o c e s p o f t a l m o l . 2 0 1 5;9 0(3):112118
addition, it was not possible to assess signs and symptoms as
double-blind due to logistic limitations. These shortcomings
must be taken into account as they restrict the scope of the
study. Even so, the latter paves the way for implementing
the use of metronidazole as alternative treatment for patients
with chronic blepharitis.
The international literature recommends the use of 2%
mercury yellow oxide, topical azithromycin and green tea
oil for treating chronic blepharitis. However, these therapy
modes are not available in our environment. The present study
demonstrates that, even though the 3 therapy modes provide
clinical improvements in symptoms and signs of patients with
chronic blepharitis, palpebral hygiene with neutral shampoo
and the combined use of neutral shampoo with metronidazole
gel are the therapeutic options available in our environment
that demonstrated the best results.
Funding
Financial support: Hannelore-Georg Zimmermann Foundation, Munich, Germany.
Conict of interest
No conict of interest has been declared by the authors.
references
1. Kanski JJ. Oftalmologa clnica. 5th ed. Madrid: Elsevier
S.A.; 2004.
Espana,
2. Bentez del Castillo JM, Daz-Valle D, Vico Ruiz E, Bentez del
Castillo J, Bentez JM. Blefaritis. In: Bentez del Castillo JM,
Durn de la Colina JA, Rodrguez Ares MT, editors. Supercie
ocular. Madrid: Sociedad Espanola
de Oftalmologa; 2004. p.
6576.
3. Norn MS. Incidence of Demodex folliculorum on skin of lids
and nose. Acta Ophthalmol (Cph). 1982;60:57583.
4. Corredor-Osorio R, Nava Castaneda
A, Tovilla Canales JL,
Tovilla y Pomar JL, Munoz
Salas S. Blefaritis por Demodex
folliculorum. Rev Fac Med UNAM. 2000;43:1259.
5. Czepita D, Kuzna-Grygiel
W, Czepita M, Grobelny A. Demodex
folliculorum and Demodex brevis as a cause of chronic marginal
blepharitis. Ann Acad Med Stetin. 2007;53:637, discussion
67.
6. Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in
blepharitis. Curr Opin Allergy Clin Immunol. 2010;10:
50510.
7. Shulman DG, Sargent JB, Stewart RH, Mester U. Comparative
evaluation of the short-term bactericidal potential of a
steroid-antibiotic combination versus steroid in the
treatment of chronic bacterial blepharitis and conjunctivitis.
Eur J Ophthalmol. 1996;6:3617.
8. Demmler M, de Kaspar HM, Mhring C, Klauss V. Blepharitis.
Demodex folliculorum, associated pathogen spectrum and
specic therapy. Ophthalmologe. 1997;94:1916.
9. Junk AK, Lukacs A, Kampik A. Topical administration of
metronidazole gel as an effective therapy alternative in
chronic Demodex blepharitis: a case report. Klin Monatsbl
Augenheilkd. 1998;213:4850.
10. Barnhorst DA Jr, Foster JA, Chern KC, Meisler DM. The efcacy
of topical metronidazole in the treatment of ocular rosacea.
Ophthalmology. 1996;103:18803.
11. Rodrguez AE, Ferrer C, Ali JL. Chronic blepharitis and
Demodex. Arch Soc Esp Oftalmol. 2005;80. Madrid.
12. Geerling G, Tauber J, Baudouin C, Goto E, Matsumoto Y,
OBrien T, et al. The international workshop on Meibomian
gland dysfunction report of the subcommittee on
management and treatment of meibomian gland
dysfunction. Invest Ophthalmol Vis Sci. 2011;52:
205064.
13. Asbell PA, Stapleton FJ, Wickstrm K, Akpek EK, Aragona P,
Dana R, et al. The international workshop on meibomian
gland dysfunction: report of the clinical trials subcommittee.
Invest Ophthalmol Vis Sci. 2011;52:206585.
14. Nelson JD, Shimazaki J, Benitez-del-Castillo JM, Craig JP,
McCulley JP, Den S, et al. The international workshop on
meibomian gland dysfunction: report of the denition and
classication subcommittee. Invest Ophthalmol Vis Sci.
2011;52:19307.
15. Gao YY, di Pascuale MA, Li W, Baradaran-Rai A, Elizondo A,
Kuo CL, et al. In vitro and in vivo killing of ocular Demodex
by tea tree oil. Br J Ophthalmol. 2005;89:146873.
16. Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular
surface discomfort and Demodex: effect of tea tree oil eyelid
scrub in Demodex blepharitis. J Korean Med Sci.
2012;27:15749.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Emergency Care Algorithms 2019 PDFDocument75 pagesEmergency Care Algorithms 2019 PDFsiraj ammed75% (4)
- Nursing Process of PneumoniaDocument5 pagesNursing Process of Pneumoniatin2x061275% (8)
- Chapter 1 - INTRODUCTION TO ANATOMY AND PHYSIOLOGY PDFDocument121 pagesChapter 1 - INTRODUCTION TO ANATOMY AND PHYSIOLOGY PDFKorina Marawis67% (3)
- Sari Gunawan, Skm. Msi: Admen UKPDocument1 pageSari Gunawan, Skm. Msi: Admen UKPRully Febri AnggoroNo ratings yet
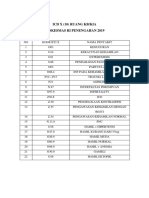
- Icd X (10) Ruang Kb/Kia Puskesmas Ri Penengahan 2019Document1 pageIcd X (10) Ruang Kb/Kia Puskesmas Ri Penengahan 2019Rully Febri AnggoroNo ratings yet
- Ketorolac vs. TramadolDocument5 pagesKetorolac vs. TramadolRully Febri AnggoroNo ratings yet
- Efficacy Comparison of Cetirizine and Loratadine ForDocument4 pagesEfficacy Comparison of Cetirizine and Loratadine ForRully Febri AnggoroNo ratings yet
- Soal Bahasa Inggris 2aDocument19 pagesSoal Bahasa Inggris 2aMegaaNo ratings yet
- The Central Nervous SystemDocument7 pagesThe Central Nervous Systemjoeywap29No ratings yet
- Evaluation of Surgical Glove Integrity and Factors Associated With Glove DefectDocument4 pagesEvaluation of Surgical Glove Integrity and Factors Associated With Glove DefectAdel AdielaNo ratings yet
- Applications of Biological Anthropology To Human Affairs - C. G. Nicholas Mascie-... (2005, PDFDocument263 pagesApplications of Biological Anthropology To Human Affairs - C. G. Nicholas Mascie-... (2005, PDFkenNo ratings yet
- Cane Sugar PDFDocument633 pagesCane Sugar PDFbernie_bph50% (2)
- Oxoid 2012-13Document84 pagesOxoid 2012-13Athar AbbasNo ratings yet
- Prolapsed Intervertebral Disc: By: Diksha Solanki Bot 4 YearDocument37 pagesProlapsed Intervertebral Disc: By: Diksha Solanki Bot 4 YearISIC IRS100% (1)
- Liver Function Tests: Steve Bradley Chief Medical Resident, HMC Inpatient ServicesDocument24 pagesLiver Function Tests: Steve Bradley Chief Medical Resident, HMC Inpatient ServicesRAHUL GANGWARNo ratings yet
- HomeostasisDocument2 pagesHomeostasisAnn Calindo EstafiaNo ratings yet
- Drink Water On Empty StomachDocument4 pagesDrink Water On Empty StomachbabuNo ratings yet
- First Semester QuizDocument14 pagesFirst Semester Quiz11521166No ratings yet
- AIIMS 2015 Solved PaperDocument436 pagesAIIMS 2015 Solved PaperSurya TejaNo ratings yet
- Ancient Cures, Charms, and Usages of IrelandDocument282 pagesAncient Cures, Charms, and Usages of IrelandIan ThomsonNo ratings yet
- 3 - Physical Examination of UrineDocument6 pages3 - Physical Examination of UrineKunware TropaNo ratings yet
- CBSE Class 7 Science MCQs-Respiration in OrganismsDocument2 pagesCBSE Class 7 Science MCQs-Respiration in Organismssiba padhy100% (3)
- Ho Lester OlllDocument6 pagesHo Lester OlllVlad VladNo ratings yet
- Medical Rehabilitation in Compression FractureDocument32 pagesMedical Rehabilitation in Compression FracturegloriaNo ratings yet
- 2021-05-15 New ScientistDocument62 pages2021-05-15 New ScientistAgenor Phillips100% (1)
- B.inggris Report TextDocument3 pagesB.inggris Report TextSeryx DoankNo ratings yet
- Actinomycetes - Ranjana BhatiDocument22 pagesActinomycetes - Ranjana BhatiShaivya BajpayeeNo ratings yet
- ICU MSC Logbook-FinalDocument101 pagesICU MSC Logbook-FinalCwali MohamedNo ratings yet
- Homescience f1-f4Document300 pagesHomescience f1-f4elizabethk1981No ratings yet
- Aedes Egypti ADocument10 pagesAedes Egypti AOswin YohsaNo ratings yet
- Remodelling of Nola PenderDocument5 pagesRemodelling of Nola PenderDon Chiaw ManongdoNo ratings yet
- Final RM Mini ProjectDocument33 pagesFinal RM Mini ProjectRahul ChaudharyNo ratings yet
- Rds CaseDocument42 pagesRds Casegebby puspitaNo ratings yet
- Case Presentation OngDocument12 pagesCase Presentation OngRaja Azman Raja AhmadNo ratings yet