Professional Documents
Culture Documents
Ondan 5
Ondan 5
Uploaded by
Siva SankarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ondan 5
Ondan 5
Uploaded by
Siva SankarCopyright:
Available Formats
[Downloadedfreefromhttp://www.joacp.orgonFriday,December13,2013,IP:117.209.135.
92]||ClickheretodownloadfreeAndroidapplicationforthisjournal
J Anaesth Clin Pharmacol 2010; 26(4): 480-483
480
A Comparative Study Between Palonosetron and Granisetron to Prevent Postoperative
Nausea and Vomiting after Laparoscopic Cholecystectomy
Dhurjoti Prosad Bhattacharjee, Satrajit Dawn, Sushil Nayak, Pramod Ranjan Roy, Amita Acharya, Ramkrishna Dey
ABSTRACT
Background: Postoperative nausea and vomiting (PONV) is commonly seen after laparoscopic surgery . In this randomized
double blind prospective clinical study, we investigated and compared the efficacy of palonosetron and granisetron to
prevent postoperative nausea and vomiting after laparoscopic cholecystectomy.
Patients & Methods: Sixty female patients (18-65 yrs of age) undergoing elective laparoscopic cholecystectomy were
randomly allocated one of the two groups containing 30 patients each. Group P received palonosetron 75 g intravenously
as a bolus before induction of anaesthesia. Group G received granisetron 2.5 mg intravenously as a bolus before induction.
Results: The incidence of a complete response (no PONV, no rescue medication) during 0-3 hour in the postoperative
period was 86.6% with granisetron and 90% with palonosetron, the incidence during 3-24 hour postoperatively was 83.3%
with granisetron and 90% with palonosetron. During 24-48 hour, the incidence was 66.6% and 90% respectively (p<0.05).
The incidence of adverse effects were statistically insignificant between the groups.
Conclusion: Prophylactic therapy with palonosetron is more effective than granisetron for long term prevention of postoperative
nausea and vomiting after laparoscopic cholecystectomy.
KEYWORDS: Palonosetron, Granisetron, Postoperative Nausea and Vomiting(PONV), Laparoscopic surgery.
Post operative nausea and vomiting (PONV) are distressing
symptoms that commonly occur after laparoscopic surgery
performed under general anaesthesia1. Vomiting may cause
dehydration, electrolyte imbalance, disruption of surgical
repair and increase the perception of pain2. A number of
pharmacological agents (antihistamines, butyro-phenones,
dopamine receptor antagonists) have been tried for the
prevention and treatment of PONV but undesirable adverse
effects such as excessive sedation, hypertension, dry mouth,
dysphoria, hallucinations and extra pyramidal symptoms
have been noted 3 . 5-hydroxytryptamine type3(5HT3)
receptor antagonists are devoid of such side effects and
highly effective in prevention and treatment of PONV.
Granisetron is a highly selective and potent 5-HT3
receptor antagonist4. It acts specifically at 5-HT3 receptors
on the vagal afferent nerves of the gut. Granisetron produces
irreversible block of the 5-HT3 receptors and it may account
for the long duration of this drug5,6.
Palonosetron is a 5-HT3 receptor antagonist used for
preventing chemotherapy induced nausea and vomiting.
This unique 5-HT3 receptor antagonist has a greater binding
affinity and longer half-life than older 5-HT3 antagonists like
ondansetron. Recent receptor binding studies suggest that
palonosetron is further differentiated from other 5-HT3 by
interacting with 5-HT3 receptors in an allosteric, positively
cooperative manner at sites different from those that bind
with ondansetron and granisetron7. In addition, this sort of
receptor interaction may be associated with long lasting
effects on receptor ligand binding and functional responses
to serotonin8.
We designed this prospective randomized double blind
trial to assess and compare the antiemetic efficacy of
granisetron and palonosetron to prevent PONV in patients
undergoing laparoscopic cholecystectomy.
PATIENTS & METHODS
The study protocol was approved by the institution ethical
committee and informed consent was obtained from every
patient. Sixty ASA III female patients, aged 18-65 years,
undergoing elective laparoscopic cholecystectomy were
randomly assigned to one of the two groups, containing
thirty patients each. Patients who had gastrointestinal
disease, were smokers, had history of motion sickness and/
or PONV, were pregnant or menstruating and those who
had taken antiemetic medication within last 24 hours were
excluded from the study.
Drs. Dhurjoti Prosad Bhattacharjee, Associate Professor, Satrajit Dawn, Assistant Professor, Sushil Nayak, Assiatant
Professor, Pramod Ranjan Roy, Second Year M.D. PGT, Amita Acharya, Associate Professor, Ramkrishna Dey, Professor
and Head, Department of Anaesthesiology, Calcutta National Medical College, Kolkata
Correspondence: Dr. Dhurjoti Prosad Bhattacharjee, E-mail: dhurjotib@yahoo.com
[Downloadedfreefromhttp://www.joacp.orgonFriday,December13,2013,IP:117.209.135.92]||ClickheretodownloadfreeAndroidapplicationforthisjournal
J Anaesth Clin Pharmacol 2010; 26(4): 480-483
Identical syringes containing study medications (2.5
ml) were prepared by the personal who were blinded to the
computer generated randomization schedule. Patients were
randomly allocated into two groups (n=30 each) to receive
one of the following regimens: palonosetron 75g in 2.5 ml
(0.9% saline was added to make the desired volume) [group
P] or granisetron 2.5 mg in 2.5 ml[group G]. The study
medication were administered immediately before the
induction of anaesthesia.
All patients were kept fasting after midnight and received
midazolam 7.5 mg orally as premedication. On the operation
table, routine monitoring (ECG, pulse oximetry, NIBP) were
started and baseline vital parameters like heart rate(HR),
blood pressure(systolic, diastolic and mean) and arterial
oxygen saturation(SpO2) were recorded. An intravenous
line was secured.
After preoxygenation for 3 minutes, induction of
anaesthesia was done by fentanyl 2g kg-1 and thiopental
5mg kg-1. Patients were intubated with appropriate size
endotracheal tube after muscle relaxation with vecuronium
bromide in a dose of 0.08mg kg-1. Anaesthesia was maintained
with 33% oxygen in nitrous oxide and sevoflurane 2%. Muscle
relaxation was maintained by intermittent bolus doses of
vecuronium bromide. The patients were mechanically
ventilated to keep EtCO2 between 35-40 mm Hg. A nasogastric
tube was inserted to make the stomach empty of air and other
contents. For laparoscopic surgical procedure, peritoneal
cavity was insufflated with carbon dioxide to keep intra
abdominal pressure <14 mmHg. At the end of surgical
procedure, residual neuromuscular block was adequately
reversed using intravenous glycopyrrolate and neostigmine
and subsequently extubated. Before tracheal extubation, the
nasogastric tube was suctioned and removed. For
postoperative analgesia, diclofenac transdermal patch was
applied on body surface. All patients were observed
postoperatively by resident doctors who were unaware of the
study drug. Patients were transferred to postanaesthesia care
unit and blood pressure, heart rate and oxygen saturation
were monitored. All episodes of PONV(nausea, retching and
vomiting) were recorded for 0-3 hour in postanaesthesia care
unit and from 3-48 hour in postoperative ward.
Nausea was defined as unpleasant sensation
associated with awareness of the urge to vomit. Retching
was defined as the laboured, spastic, rhythmic contraction
of the respiratory muscles without the expulsion of gastric
contents. Vomiting was defined as the forceful expulsion of
gastric contents from mouth. Complete response(free from
emesis) was defined as no PONV and no need for any
rescue medication. If there were two or more episodes of
PONV during first 48 hours, rescue antiemetic
(metoclopramide10 mg i.v.) was given.
481
Data were analyzed using computer statistical software
system Graph Pad Instat Version 3.05 (Graph Pad software,
San Diego, CA) and are presented in a tabulated manner.
Comparisons between groups were performed by using the
Kruskal Wallis one way ANOVA by ranks or Fishers exact
test for small sample with a 5% risk or Mann Whitney
Wilcoxon tests when normality tests failed or Chi-square
test, as appropriate. The results were expressed in meanSD
and number(%).
RESULTS
The groups were comparable with respect to age, weight
and duration of surgery [Table 1]. The incidence of a
complete response (no PONV, no rescue medication) during
0-3 hour in the postoperative period was 86.6% with
granisetron and 90% with palonosetron, the incidence during
3-24 hour postoperatively was 83.3% with granisetron and
90% with palonosetron. During 24-48 hour, the incidence
was 66.6% and 90% respectively [Table 2]. Thus a complete
response during 24-48 hour in the postoperative period
was significantly more patients who had received
palonosetron than in those who had received granisetron
(p<0.05) [Table 2].
Table 1
Patients characteristics and duration of surgery (Mean SD)
Group G
(n=30)
Age (Years)
42.3 4.32
Weight (kg)
52.24 7.36
Duration of surgery (min) 52.72 6.62
Group P
(n=30)
P Value
43.46.46
54.42 8.22
55.828.44
0.47
0.55
0.62
Table 2
Incidence of Postoperative Nausea & Vomiting(PONV)
Postoperative
period(hr)
Granisetron
(n=30)
Palonosetron P Value
(n=30)
0-3 hr
Complete Response
Nausea
Retching
Vomiting
Rescue Drug
26(86.6%)
4(13.3%)
1(3.3%)
2(6.6%)
0
27(90%)
2(6.6%)
1(3.3%)
1(3.3%)
0
0.65
0.67
1
0.42
1
3-24 hr
Complete Response
Nausea
Retching
Vomiting
Rescue Drug
25(83.3%)
4(13.3%)
1(3.3%)
3(10%)
0
27(90%)
2(6.6%)
1(3.3%)
2(6.6%)
0
0.58
0.72
1
0.68
1
24-48 hr
Complete Response
Nausea
Retching
Vomiting
Rescue Drug
20(66.6%)
6(20%)
2(6.6%)
5(16.6%)
0
27(90%)
3(10%)
0
2(6.6%)
0
0.003
0.09
0.49
0.07
1
[Downloadedfreefromhttp://www.joacp.orgonFriday,December13,2013,IP:117.209.135.92]||ClickheretodownloadfreeAndroidapplicationforthisjournal
BHATTACHARJEE D P ET AL: PALONOSETRON AND GRANISETRON TO PREVENT PONV
The commonly observed adverse effects were
headache, dizziness and drowsiness but those were not
clinically serious or significant. The incidence of adverse
effects were statistically insignificant between the groups
[Table 3].
Table 3
Incidence of Adverse Effects
Postoperative
period (hr)
Granisetron
(n=30)
Palonosetron P Value
(n=30)
0-3 hr
Headache
Dizziness
Drowsiness
2(6.6%)
4(13.3%)
1(3.3%)
3(10%)
2(6.6%)
1(3.3%)
0.67
0.72
1
3-24 hr
Headache
Dizziness
Drowsiness
2(6.6%)
3(10%)
1(3.3%)
2(6.6%)
2(6.6%)
1(3.3%)
1
0.68
1
24-48 hr
Headache
Dizziness
Drowsiness
0
0
0
1(3.3%)
0
0
0.37
1
1
DISCUSSION
Postoperative period is associated with variable incidence
of nausea and vomiting depending on the duration of surgery,
the type of anaesthetic agents used (dose, inhalational
drugs, opioids), smoking habit etc 9 . 5-HT 3 receptor
stimulation is the primary event in the initiation of vomiting
reflex10. These receptors are situated on the nerve terminal
of the vagus nerve in the periphery and centrally on the
chemoreceptor trigger zone (CTZ) of the area postrema3.
Anaesthetic agents initiate the vomiting reflex by stimulating
the central 5-HT3 receptors on the CTZ and also by releasing
serotonin from the enterochromaffin cells of the small
intestine and subsequent stimulation of 5-HT3 receptors on
vagus nerve afferent fibres3.
The incidence of PONV after laparoscopic surgery is
high(40-75%). The etiology of PONV after laparoscopic
surgery is complex and is dependent on a variety of factors
including age, obesity, a history of previous PONV, surgical
procedure, anesthetic technique, and post operative pain11.
In this study, however, both the groups were comparable
with respect to patient demographics, types and duration of
surgery and anesthesia and analgesics used postoperatively.
Therefore the difference in a complete response (no PONV,
no rescue medication) between the groups can be attributed
to the study drug.
Granisetron is effective for the treatment of emesis
induced by cancer chemotherapy12. The precise mechanism
of granisetron for the prevention of PONV remains unclear,
but it has been suggested that granisetron may act on sites
482
containing 5-HT3 receptors with demonstrated antiemetic
effects 13 . Palonosetron is a unique 5-HT 3 receptor
anatagonist approved for the prevention of chemotherapy
induced nausea and vomiting. It is a novel 5-HT3 receptor
antagonist with a greater binding affinity and longer biological
half-life than older 5-HT3 receptor antagonists7. The exact
mechanism of palonosetron in the prevention of PONV is
unknown but palonosetron may act on the area postrema
which contain a number of 5-HT3 receptors8. Therefore, the
possible mechanism of this antiemetic for preventing PONV
is similar to that of granisetron.
The effective dose of granisetron is 40-80g kg-1 for the
treatment of cancer chemotherapy induced nausea and
vomiting14. The dose of granisetron 2.5 mg (approximately
45g kg-1) selected for this study was within its effective
dose range (40-80g kg -1 ). However, the dose of
palonosetron to be used for the prevention of PONV is not
established but was extrapolated from the dose used in the
clinical trials15,16. Kovac LA and Colleagues16 demonstrated
that palonosetron 75g is the more effective dose for the
prevention of PONV after major gynecological and
laparoscopic surgery than 25g and 50g.16
Our study demonstrate that the antiemetic efficacy of
palonosetron is similar to that of granisetron for preventing
PONV during the first 24 hours (0-24 hours) after
laparoscopic surgery and that palonosetron is more effective
than granisetron for getting a complete response (no PONV,
no rescue medication) for 24-48 hours. This suggests that
palonosetron has an antiemetic effect which lasts longer
than granisetron. The exact reason for the difference in
effectiveness between granisetron and palonosetron is not
known but may be related to the half lives (granistron 8-9
hrs versus palonosetron 40 hrs) and/or the binding affinities
of 5-HT3 receptor antagonists (palonosetron interacts with
5-HT3 receptors in an allosteric, positive cooperative manner
at sites different from that bind with granisetron )7,8.
We did not include a control group receiving placebo
in our study. Aspinall and Goodman17 have suggested that
if active drugs are available, placebo controlled trials may
be unethical because PONV are very much distressing
after laparoscopic surgery17.
Adverse effects with a single therapeutic dose of
granisetron or palonosetron were not clinically serious16,18
and there were no significant differences in the incidence
of headache, dizziness and drowsiness between the groups.
Thus both palonosetron and granisetron are devoid of
clinically important side effects.
In conclusion prophylactic therapy with palonosetron is
more effective than prophylactic therapy with granisetron
for the long term prevention of PONV after laparoscopic
surgery.
[Downloadedfreefromhttp://www.joacp.orgonFriday,December13,2013,IP:117.209.135.92]||ClickheretodownloadfreeAndroidapplicationforthisjournal
J Anaesth Clin Pharmacol 2010; 26(4): 480-483
483
Author disclosures: Authors have no conflict of interest or
financial considerations.
9.
REFERRENCES
1. Madej T, Simpsom K. Comparison of the use of
domperidone, droperidol and metoclopramide in the
prevention of nausea and vomiting following
gynecological surgery. Br J Anaesth 1986; 58 : 879-83
2. Jellish WS, Leonetti JP, Sawicki K, et al. Morphine/
ondansetron PCA for postoperative pain, nausea and
vomiting after skull base surgery. Otolaryngol Head
Neck Surg 2006; 135: 175-81
3. Watcha MF, White PF. Postoperative nausea and
vomiting: its etiology, treatment and prevention.
Anesthesiology 1992; 77: 162-84
4. Blower PR. The role of specific 5-HT3 receptor
antagonigm in the control of cytostatic drug-induced
emesis. Euro J Cancer 1990; 26 (suppl. 1): s8-s11
5. Newberry NR, Watkins CJ, Sprosen TS, Blackburn TP,
Grahame-Smith DG, Leslie RA. BRL 46470 potently
antagonizes neural responses activated by 5-HT 3
receptors. Neuropharmacology 1993; 32 : 729-735
6. Elliott P, Seemungal BM, Wallis DI. Antagonism of the
effects of 5-hydroxytryptamine on the rabbit isolated
vagus nerve by BRL 43694 and metoclopramide.
Naunyn-Schmiedebergs Archives of Pharmacology
1990; 341: 503-09
7. Rojas C, Stathis M, Thomas A, Massuda E, Alt J, Zhang
J, Rubenstein E, Sebastianis S, Canloreggi S, Snyder
SH, Slusher B. Palonosetron exhibits unique molecular
interactions with the 5-HT3 receptor. Anesth Analg 2008;
107: 469-78
8. Gralla R, Lichinitser M, Vander Vegt S, Sleeboom H,
Mezger J, Peschel C, Tonini G, Libianca R, Macciocchi
A, Aapro M. Palonosetron improves prevention of
chemotherapy induced nausea and vomiting following
moderately emetogenic chemotherapy: results of a
double-blind randomized phase 3 trial comparing single
doses of palonosetron with ondansetron. Ann Oncol
2003; 14: 1570-7
10.
11.
12.
13.
14.
15.
16.
17.
18.
Lerman J. Surgical and patient factors involved in
postoperative nausea and vomiting. Br J Anaesth 1992;
69: 245-325
Bunce KT, Tyers MB. The role of 5-HT in postoperative
nausea and vomiting. Br J Anaesth 1992; 69 (suppl. 1):
S60-S62
R Janknegt et al. Clinical efficacy of antiemetics following
surgery. Anaesthesia 1999; 54: 1059-68
Bermudez J, Boyle EA, Minter WD, Sanger GJ. The
antiemetic potential of the 5-hydroxytryptamine 3
receptor antagonist BR 43694. Br J Cancer 1988; 58:
644-50
Carmichel J, Cantwell BMJ, Edwards CM, et al. A
pharmacokinetic study of granisetron ( BRI 43694A), a
selective 5-HT3 receptor antagonist : correlation of
antiemetic response. Cancer Chemother Pharmacol
1989; 24: 45-9
Furue H,Oota K, Taguchi T, Niitani H. Clinical evaluation
of granisetron against nausea and vomiting induced by
anticancer drugs : optimal dose finding study. J Clin
Ther Med 1990 ; 6 : 49-61
Candiotti KA, Kovac AL, Melson TI, Clerici G, Gan TJ.
A randomized double-blind study to evaluate the
efficacy and safety of three different doses of palonosetron versus placebo for preventing postoperative
nausea and vomiting. Anesth Analg 2008; 107: 445-51
Kovac AL, Eberhart L, Kotarski J, Clerici G, Apfel C. A
randomized double-blind study to evaluate the efficacy
and safety of three different doses of palonosetron
versus placebo for preventing postoperative nausea
and vomiting over a 72 hour period. Anesth Analg
2008; 107: 439-44
Aspinall RL, Goodman NW. Denial of effective treatment
and poor quality of clinical information in placebo
controlled trials of ondansetron for postoperative nausea
and vomiting: a review of published trials. BMJ 1995;
311: 844-6
Yarker YE, Mactavish D. Granisetron: an update of its
therapeutic use in nausea and vomiting induced by
antineoplasmic therapy. Drugs 1994; 48: 761-93
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Post-Operative Nausea, Vomiting, and Pain - Nursing Management and EvidenceDocument11 pagesPost-Operative Nausea, Vomiting, and Pain - Nursing Management and EvidenceAdrian Castro100% (1)
- AtiDocument489 pagesAtiOanamikaela VaidaNo ratings yet
- ANACONDADocument3 pagesANACONDASiva SankarNo ratings yet
- ARDSDocument7 pagesARDSSiva SankarNo ratings yet
- My Garden Class 1Document20 pagesMy Garden Class 1Siva SankarNo ratings yet
- Perioperative Management of Acquired Hemophilia A: A Case Report and Review of LiteratureDocument3 pagesPerioperative Management of Acquired Hemophilia A: A Case Report and Review of LiteratureSiva SankarNo ratings yet
- Sedation and Anesthesia in GI Endoscopy 2008Document12 pagesSedation and Anesthesia in GI Endoscopy 2008Siva SankarNo ratings yet
- Ultrasound Guided Regional Nerve BlocksDocument32 pagesUltrasound Guided Regional Nerve BlocksSiva SankarNo ratings yet
- H, C Radiolabeled Compounds and Their Applications in Metabolism StudyDocument5 pagesH, C Radiolabeled Compounds and Their Applications in Metabolism StudySiva SankarNo ratings yet
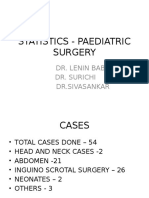
- Statistics - Paediatric SurgeryDocument9 pagesStatistics - Paediatric SurgerySiva SankarNo ratings yet
- SR-JR Leave FormDocument5 pagesSR-JR Leave FormSiva SankarNo ratings yet
- Obesity 2Document12 pagesObesity 2Siva SankarNo ratings yet
- Death SummaryDocument3 pagesDeath SummarySiva SankarNo ratings yet
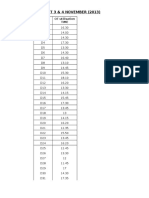
- OT 3 & 4 NOVEMBER (2013) : Date OT Utilisation TimeDocument4 pagesOT 3 & 4 NOVEMBER (2013) : Date OT Utilisation TimeSiva SankarNo ratings yet
- Thromboprophylaxis & RADocument38 pagesThromboprophylaxis & RASiva SankarNo ratings yet
- Adapted Caprini Score Protocol With Proforma Submitted To JSACDocument17 pagesAdapted Caprini Score Protocol With Proforma Submitted To JSACSiva SankarNo ratings yet
- Glycemic 2010 PDFDocument9 pagesGlycemic 2010 PDFSiva SankarNo ratings yet
- ERAS & TTSH Experience - Indonesia 2019 JakartaDocument79 pagesERAS & TTSH Experience - Indonesia 2019 JakartaFransisca Dewi KumalaNo ratings yet
- The Essential Oil of Ginger, Zingiber Officinale, and AnaesthesiaDocument9 pagesThe Essential Oil of Ginger, Zingiber Officinale, and Anaesthesiarefilda suhailiNo ratings yet
- Coba 2Document6 pagesCoba 2Bianca CaterinalisendraNo ratings yet
- Postanesthesia Care: Muhamad Chairul FadhilDocument28 pagesPostanesthesia Care: Muhamad Chairul FadhilMuhammad Chairul Fadhil100% (1)
- POST OP BrunnerDocument7 pagesPOST OP Brunnerjamie carpioNo ratings yet
- Anesthesia and Sedation Outside ofDocument9 pagesAnesthesia and Sedation Outside ofPutriRahayuMoidadyNo ratings yet
- Peter S.A. Glass MD - Ambulatory Anesthesia, An Issue of Anesthesiology Clinics (The Clinics - Surgery) - Saunders (2010) PDFDocument204 pagesPeter S.A. Glass MD - Ambulatory Anesthesia, An Issue of Anesthesiology Clinics (The Clinics - Surgery) - Saunders (2010) PDFdannybest2009No ratings yet
- Adjuvant Local Anestesi PNBDocument23 pagesAdjuvant Local Anestesi PNBBangkit PrimayudhaNo ratings yet
- DwefgnmjDocument8 pagesDwefgnmjfabian arassiNo ratings yet
- Day Care AnesthesiaDocument68 pagesDay Care AnesthesiaSri Sruthi PichikaNo ratings yet
- Pediatric Anesthesia - 2021 - Luo - Effects of Erector Spinae Plane Block On Postoperative Pain in Children UndergoingDocument10 pagesPediatric Anesthesia - 2021 - Luo - Effects of Erector Spinae Plane Block On Postoperative Pain in Children UndergoingPablo Lukacs CarmonaNo ratings yet
- Enhanced Recovery After SurgeryDocument47 pagesEnhanced Recovery After SurgeryPeri HidayatNo ratings yet
- Anesthetics and Anesthesiology: Effect of Opioid-Free Anaesthesia On Perioperative Period: A ReviewDocument11 pagesAnesthetics and Anesthesiology: Effect of Opioid-Free Anaesthesia On Perioperative Period: A Reviewveranisa suciaNo ratings yet
- Alexanders Care of The Patient in Surgery 16th Edition Rothrock Test BankDocument11 pagesAlexanders Care of The Patient in Surgery 16th Edition Rothrock Test Banklilykeva56r100% (34)
- Anaesthesia For Major Urological SurgeryDocument23 pagesAnaesthesia For Major Urological SurgeryDianita P Ñáñez VaronaNo ratings yet
- Annex Pil DHCPDocument11 pagesAnnex Pil DHCPAbdelrahman MohamedNo ratings yet
- Postoperative Complications of Spine SurgeryDocument42 pagesPostoperative Complications of Spine Surgerydonira73No ratings yet
- Standardized Nursing Terminology AssignmentDocument6 pagesStandardized Nursing Terminology Assignmentapi-3284480220% (1)
- Ambulatory Urology and Urogynaecology, 2021Document286 pagesAmbulatory Urology and Urogynaecology, 2021Desmosedici GrenadierNo ratings yet
- Nursing Journal PACUDocument11 pagesNursing Journal PACUJet BautistaNo ratings yet
- Longo 2017Document7 pagesLongo 2017Azza SintaNo ratings yet
- Aid To Multiple Choice Questions in Surgery - 230304 - 020620Document164 pagesAid To Multiple Choice Questions in Surgery - 230304 - 020620K.M.S. ChathunikaNo ratings yet
- Day SurgeryDocument350 pagesDay SurgeryMohamed Fawzy100% (1)
- Anesthetic Management and Deep Sedation After Emergence From General Anesthesia - A Retrospective Cohort StudyDocument10 pagesAnesthetic Management and Deep Sedation After Emergence From General Anesthesia - A Retrospective Cohort Studygwhqvmqks5No ratings yet
- Nausea in AdultsDocument13 pagesNausea in AdultsSadaf N. HudaNo ratings yet
- Perioperative Fasting: A Time To Relook: Guest EditorialDocument2 pagesPerioperative Fasting: A Time To Relook: Guest EditorialIbraim CervantesNo ratings yet
- Anesthesia For Day Care Dental ProceduresDocument20 pagesAnesthesia For Day Care Dental Proceduresramanrajesh83No ratings yet
- Adult PONV and PDNV Process by ASCDocument2 pagesAdult PONV and PDNV Process by ASCHundalHarmanNo ratings yet