Professional Documents
Culture Documents
cjrt-51-69 1
cjrt-51-69 1
Uploaded by
api-3540402130 ratings0% found this document useful (0 votes)
24 views3 pagesOriginal Title
cjrt-51-69 1
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
24 views3 pagescjrt-51-69 1
cjrt-51-69 1
Uploaded by
api-354040213Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
brief communication
Innovation in respiratory therapy and the use of
three-dimensional printing for tracheostomy management
Andrew J West MAppSc RRT FCSRT1, Karen Taylor RRT2, Daniel W Rickey PhD MCCPM3,4
R espiratory therapy (RT) is a profession with a long history of
clinical applications of advanced and emerging technologies
(1,2). A cursory review of the previous two iterations of the national
relationship with the respiratory therapists of the Long Term
Ventilator Service (LTVS), Winnipeg Regional Health Authority
(Manitoba). It was natural then that this unique collaboration may
competency profile for Canadian respiratory therapists provides lead to an innovative approach to client care by applying 3D printing
insight into the rapid evolution of our professional practice (3,4). technology to RT practice.
Many changes in practice patterns were influenced, at least in part,
by technological advances. It is not, therefore, unexpected that the
rapid evolution of technologies currently being witnessed, both clin- A collaborative approach to innovative
ical and nonclinical, will invariably have an impact on RT practice. tracheostomy management
It is by adopting emerging technologies that the profession of RT will The LTVS provides RT services to long-term clients in the commun-
advance in innovative ways. ity who require support for medically complex needs. These needs
Early literature in organizational change observed that variability in frequently include tracheostomy airway management in clients who
hospital adoption of innovation could be accounted for, at least in part, may or may not also require mechanical ventilation. There are sev-
by a variability in the development of structural mechanisms that pro- eral well-known long-term effects of tracheostomy, including dys-
vide access to knowledge about change (5). Fortunately, organizational phagia, inability to phonate, tracheal granuloma and tracheomalacia
structures that support sharing of knowledge about change, including (9,10). Respiratory therapists at the LTVS use various methods of
this Journal and professional conferences, exist in RT. It is by developing customizing tracheostomy tubes to mitigate anatomical or other
a rich culture of using these venues for knowledge sharing that the therapeutic challenges, or to manage complications resulting from
innovative capital existing in RT can be fostered. long-term use of the airway itself. Routine diagnostic techniques,
We may typically believe that innovation occurs as a result of an such as bronchoscopy, broncheolar lavage, radiography and CT, have
a-ha moment. However, the knowledge-building literature suggests been used to diagnose and monitor these long-term effects.
that the majority of new ideas adopted into practice result from col- Although a cornerstone of management, these diagnostic tech-
laborative processes that develop organically over a period of time niques have occasionally proven insufficient for identifying the etiol-
(6,7). Taking a page from educational design researchers, it has been ogy of symptoms related to long-term tracheostomy use that have
theorized that professional innovation can be spurred by creating appeared clinically. This has limited the ability of the respiratory
environments where ideas can connect (8). The following example therapists to determine appropriate clinical interventions such as
illustrates how a collaborative approach, along with an environ- tracheostomy type, position and need for customization. For example,
ment supportive of knowledge sharing, became useful in addressing occasionally complicated tracheal anatomy may make airway visualiza-
a problem in RT practice through adopting three-dimensional (3D) tion highly challenging and, thus, limit the ability to determine a dif-
printing technology. ferential diagnosis in the presence of multiple long-term complications.
One approach that has been used to give a detailed and informative
Adopting 3D printing technology understanding of the etiology of client symptoms has been the use of 3D
Additive manufacturing, more commonly known as 3D printing, has printing technology to reproduce the results of high-resolution CT scan-
been used in the clinical sciences for planning complex surgeries and ning. The genesis of the idea to use 3D printing technology in cases such
designing custom implants. The introduction of low-cost consumer- as these came as a result of collaborative review and a shared desire to
grade 3D printers enables this technology to be used for more routine design a solution for these clinical concerns. The existing relationship
procedures, although its application in RT has not been widely pub- between the respiratory therapists of the LTVS and personnel in the
lished. These 3D printers deposit 0.1 mm- to 0.3 mm-thick layers of hot Medical Devices Department at CancerCare Manitoba served as an
acrylonitrile butadiene styrene or polylactic acid plastic. The resulting important environmental factor, which facilitated the connection of
model (3D printout) is slowly built up layer by layer. An important fea- ideas. Encouraging professionals to connect ideas and expertise with
ture of 3D printers is that they can produce complex objects. In addi- those of colleagues and others in this manner brought individuals
tion, there are several software packages that import medical magnetic together and supported a sense of collective cognitive responsibility
resonance or computed tomography (CT) images and enable the cre- (11). Through sharing in the responsibility for knowledge creation,
ation of models suitable for printing. both the individual goals of the respiratory therapist and the patient,
The use of medical imaging and 3D printing had previously been as well as the collective goals of the organization were achieved in an
used for radiation therapy applications at CancerCare Manitoba. innovative way. As a result, 3D printing was used as a means of assessing
Additionally, the institutions medical devices department regularly modi- airway abnormalities and symptomology not explained by traditional
fies tracheostomy tubes and, thus, has developed a strong collaborative diagnostic and assessment techniques.
1Collegeof Rehabilitation Sciences, University of Manitoba; 2Long Term Ventilator Service, Winnipeg Regional Health Authority; 3Division of
Medical Physics, CancerCare Manitoba; 4Departments of Radiology, and Physics & Astronomy, University of Manitoba, Winnipeg, Manitoba
Correspondence: Mr Andrew J West, College of Rehabilitation Sciences, University of Manitoba, R106-771 McDermot Avenue, Winnipeg,
Manitoba R3E 0T6. Telephone 204-789-3897, fax 204-789-3927, e-mail westa@cc.umanitoba.ca
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://
creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is
properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact support@pulsus.com
Can J Respir Ther Vol 51 No 3 Summer 2015 69
West et al
Figure 1) Image acquired using high-resolution computed tomography
showing a tracheal cross-section. Visible are the tracheal lumen (A) and
tracheostomy tube (B) in situ. The contour (in cyan) was used to create a Figure 3) Computer rendering of a stereolithography (stl) file developed
stereolithography (stl) file from high-resolution computed tomography scan, from which a negative
model of the tracheal lumen could be created using a three-dimensional
printer. A Extensive anatomical abnormality
Figure 4) Photograph of three-dimensional printed positive model of the air-
way. This model corresponds to the stereolithography data shown in Figure 2.
The model is approximately 11.5 cm 3.8 cm 7 cm. A Tracheal lumen.
B Tracheal lumen and stoma
Figure 2) Computer rendering of a stereolithography (stl) file developed
from a high-resolution computed tomography scan, from which a positive
model of the airway could be created using a three-dimensional printer. determine the most appropriate airway specification relative to the
A Tracheal lumen. B Tracheal lumen and stoma anatomical limitations and other complications. Figures 4, 5 and 6
demonstrate three different models of the trachea that were printed
using the 3D printer. These models provided a profound visual aid in
Innovation design challenges understanding the unexpectedly extensive anatomical abnormality of
In this example, a client underwent a high-resolution CT scan. The this symptomatic client. An additional strength of 3D printing is that
resulting images were then imported into 3D modelling software (3D the models may be sliced in any plane before printing, and producing
Doctor V5, Able Software Corp, USA) in which the trachea was out- additional copies is simple.
lined. Although parts of this task were automated, several hours of Although 3D printing technology holds much potential for use in
manual work by the medical devices personnel was necessary. A sig- RT and in tracheostomy management, one notable limitation of this
nificant challenge is that because a trachea tube was in place during approach is the lengthy process of outlining the trachea on the CT
the CT scan, it was subsequently necessary to remove it from each images. Although this step is partially automated, the presence of the
image manually (Figure 1). The resulting outline of the trachea was trachea tube in the images complicates the process considerably.
then exported as a stereolithography (stl) file from which tracheal
models were printed using a consumer-grade fused-deposition printer Conclusion
(Solidoodle 3, Solidoodle LLC, USA and MakerGear M2, MakerGear The use of 3D printing technology to enhance clinical evaluation of
LLC, USA) (Figures 2 and 3). Printing the tracheal models was rela- clients with long-term tracheostomy provides an example of how
tively straightforward as either a positive that was a copy of the patient innovative ideas lead to practical solutions using new technologies.
anatomy, or as a negative that revealed the lumen of the trachea. The adoption of 3D printing in RT practice has not previously been
The 3D printed model of the tracheal lumen simplified observation reported in the literature. As is the case in many innovation-generating
of its complex shape. Furthermore, the ability to physically fit the organizations, the roots of a new practice concept rest in sharing and
tracheostomy tube into the positive model enabled the team to better synthesizing multiple perspectives, problem solving and collective
70 Can J Respir Ther Vol 51 No 3 Summer 2015
3D printing for tracheostomy management
Figure 6) Photograph of three-dimensional printed positive model sliced along
the medial plane to enable visualization of the cross-section of the trachea, with
a tracheostomy tube modified to fit anatomical abnormalities in situ
Figure 5) Photograph of three-dimensional printed negative model of the References
tracheal lumen corresponding to the stereolithography data shown in Figure 3. 1. Training for Inhalation Therapy Technicians in Canada.
CMAJ 1962;87:818.
A Extensive anatomical abnormality
2. McCaughey TJ. Anesthetic technicians in the province of Quebec.
Can Anaesth Soc J 1975;22:106-10.
3. The National Alliance of Respiratory Therapy Regulatory Bodies.
knowledge construction (12). Through dissemination of this idea, it is National Competency Profile. <http://www.nartrb.ca/eng/
hoped that others will be prompted to share in further exploration and publications.php> (Accessed March 30, 2015).
development of this particular idea, thus fostering new insights. 4. The National Alliance of Respiratory Therapy Regulatory Bodies.
An interesting array of issues worthy of further inquiry have 2011 Respiratory Therapy National Competency Profile. <http://
emerged from this innovation. To evaluate the possible scope of www.nartrb.ca/eng/publications.php> (Accessed March 30, 2015).
applicability of 3D printing in tracheostomy management, it would 5. Kimberly JR. Hospital adoption of innovation: The role of
be valuable to quantify the prevalence and morphology of tracheal integration into external informational environments.
J Health Soc Behav 1978;19:361-73.
abnormalities in clients with long-term tracheostomy. Additionally, 6. Johnson S. Where Good Ideas Come From: The Natural History of
it would also be of great interest to determine whether routine assess- Innovation. New York: Penguin, 2010.
ment using 3D printing technology could impact client outcomes. 7. Kelly K. What Technology Wants. New York: Penguin, 2010.
Finally, we need to consider its application as a tool for professional 8. McKenney S, Reeves TC. Conducting Educational Design
and client education. Research. Florence: Taylor and Francis, 2012.
Beyond spurring interest and inquiry in this new assessment tech- 9. Law JH, Barnhart K, Rowlett W, De La Rocha O, Lowenberg S.
nique, it is also hoped that this discussion will promote wider awareness Increased frequency of obstructive airway abnormalities with long-
term tracheostomy. Chest 1993;104:136-8.
and use of the structural mechanisms available to respiratory therapists
10. Sue RD, Susanto I. Long-term complications of artificial airways.
for sharing knowledge. Supporting an environment of information Clin Chest Med 2003;24:457-71.
exchange and community knowledge generation will lead to enhance- 11. Scardamalia M. Collective cognitive responsibility for the
ments in the support we provide to those with respiratory challenges. advancement of knowledge. In: Liberal Education in a Knowledge
Society. Chicago: Open Court 2002;97:67-98.
DISCLOSURES: The authors have no financial disclosures or conflicts 12. Zhang J, Scardamalia M, Reeve R, Messina R. Designs for collective
of interest to declare. cognitive responsibility in knowledge-building communities.
J Learn Sci 2009;18:7-44.
Can J Respir Ther Vol 51 No 3 Summer 2015 71
You might also like
- Statement of Purpose Example 45Document8 pagesStatement of Purpose Example 45akshayNo ratings yet
- Schneider Protection Application GuideDocument293 pagesSchneider Protection Application GuideFrancisco Martinez100% (1)
- 43 An Automated Deep Learning Based Software For Total Lung Volume Calculation and Lung 3D Model ReconstructionDocument8 pages43 An Automated Deep Learning Based Software For Total Lung Volume Calculation and Lung 3D Model ReconstructionHuy HoangNo ratings yet
- 3-D Segmentation AlgorithmDocument13 pages3-D Segmentation Algorithmkoushikraj900No ratings yet
- State-Of-The-Art On Cone Beam CT Imaging For Preoperative Planning of Implant PlacementDocument7 pagesState-Of-The-Art On Cone Beam CT Imaging For Preoperative Planning of Implant Placementanimeilove3No ratings yet
- BJR 71 846 9849380Document8 pagesBJR 71 846 9849380BitaNo ratings yet
- Prosch2012 (Jurnal 7)Document11 pagesProsch2012 (Jurnal 7)MayNo ratings yet
- Immobilisation FFFDocument8 pagesImmobilisation FFFSrinivas VenkataramanNo ratings yet
- Sarti 2012Document12 pagesSarti 2012mariaNo ratings yet
- Lee. C. D.Document14 pagesLee. C. D.GiovanniNo ratings yet
- Research Paper On Computed TomographyDocument8 pagesResearch Paper On Computed Tomographyafmcsmvbr100% (1)
- Icru Report 83Document103 pagesIcru Report 83Marlon SantosNo ratings yet
- 3D Printing Techniques in A Medical Setting: A Systematic Literature ReviewDocument21 pages3D Printing Techniques in A Medical Setting: A Systematic Literature ReviewIsabella GallardoNo ratings yet
- Research Article: Automated Quantification of Pneumothorax in CTDocument8 pagesResearch Article: Automated Quantification of Pneumothorax in CTAnnisa HidayatiNo ratings yet
- PravallikaDocument28 pagesPravallikaVegesana SumythriNo ratings yet
- An Overview of Volumetric Imaging Technologies and Their Quality Assurance For IGRTDocument9 pagesAn Overview of Volumetric Imaging Technologies and Their Quality Assurance For IGRTBounegta AhmedNo ratings yet
- PIIS093665552100368XDocument2 pagesPIIS093665552100368XAnharNo ratings yet
- 11.deep Learning Applications in Medical Image Analysis-Brain TumorDocument4 pages11.deep Learning Applications in Medical Image Analysis-Brain TumorVenky Naidu BalineniNo ratings yet
- Bio Med PaperDocument13 pagesBio Med PaperironmanjrpNo ratings yet
- LDNNET Towards Robust Classification of Lung Nodule and Cancer Using Lung Dense Neural NetworkDocument20 pagesLDNNET Towards Robust Classification of Lung Nodule and Cancer Using Lung Dense Neural Networkswathi sNo ratings yet
- J Ejmp 2020 02 017Document2 pagesJ Ejmp 2020 02 017Camilo SotomayorNo ratings yet
- Orp 3 CombDocument8 pagesOrp 3 CombControl de Equipos InternosNo ratings yet
- An Efficient Visualization and Segmentation of Lung CT Scan Images For Early Diagnosis of CancerDocument5 pagesAn Efficient Visualization and Segmentation of Lung CT Scan Images For Early Diagnosis of Cancermaruthi631No ratings yet
- Computer Methods and Programs in BiomedicineDocument12 pagesComputer Methods and Programs in BiomedicineJay PatelNo ratings yet
- EasyChair Preprint 545Document6 pagesEasyChair Preprint 545Greeni MarcoNo ratings yet
- CT Scan Research PapersDocument4 pagesCT Scan Research Paperspxihigrif100% (1)
- The Future of Hybrid Imaging-Part 2: PET/CT: Insights Into Imaging June 2011Document11 pagesThe Future of Hybrid Imaging-Part 2: PET/CT: Insights Into Imaging June 2011maaddy001No ratings yet
- Anapub Paper TemplateDocument10 pagesAnapub Paper Templatebdhiyanu87No ratings yet
- Eano GlioblastomaDocument10 pagesEano GlioblastomaMEILYN MEDINA FAÑANo ratings yet
- Robot-Assisted Microwave Thermoablation of Liver Tumors: A Single-Center ExperienceDocument9 pagesRobot-Assisted Microwave Thermoablation of Liver Tumors: A Single-Center ExperienceMamanya Fadhil HaniNo ratings yet
- Korir 2015Document11 pagesKorir 2015Rimo RimoNo ratings yet
- Radiation Dose Reduction Techniques For Chest CT Principles and Clinical ResultsDocument11 pagesRadiation Dose Reduction Techniques For Chest CT Principles and Clinical ResultsSantiago TapiaNo ratings yet
- Development and Research IssuesDocument3 pagesDevelopment and Research IssuesGAGANPREET SINGHNo ratings yet
- Technical Innovations & Patient Support in Radiation OncologyDocument9 pagesTechnical Innovations & Patient Support in Radiation OncologyDiana MitreaNo ratings yet
- Final DraftDocument18 pagesFinal Draftapi-334402872No ratings yet
- البحث الخامسDocument6 pagesالبحث الخامسAbd El-Rahman MohamedNo ratings yet
- GEC-ESTRO Recommendations III For HDR BTDocument8 pagesGEC-ESTRO Recommendations III For HDR BTClaudia Morales Ulloa100% (2)
- Prostate Segmentation ThesisDocument9 pagesProstate Segmentation Thesisgj9ggjry100% (2)
- Imaging in Polytrauma e Principles and Current ConceptsDocument8 pagesImaging in Polytrauma e Principles and Current ConceptsJJCONo ratings yet
- Lung Intervention by Using CT Fluoroscopy With Repository FrameworkDocument5 pagesLung Intervention by Using CT Fluoroscopy With Repository FrameworkerpublicationNo ratings yet
- Detection of Lung Nodules in Computed Tomography Images: F E U PDocument127 pagesDetection of Lung Nodules in Computed Tomography Images: F E U PcuongncNo ratings yet
- Bookshelf NBK592664Document13 pagesBookshelf NBK592664Ng Yi XuanNo ratings yet
- Different Styles of IGRTDocument10 pagesDifferent Styles of IGRTPeter CaldwellNo ratings yet
- Perfusion 1Document12 pagesPerfusion 1zixdiddyNo ratings yet
- CancerDocument9 pagesCancerMARIA JOSE RIVERA AVILANo ratings yet
- Pulmonary Airway Tissue Extraction For Lesion Detection Using HRCT ImagesDocument12 pagesPulmonary Airway Tissue Extraction For Lesion Detection Using HRCT ImagesArul SelviNo ratings yet
- Virtual SimulationDocument7 pagesVirtual SimulationNephtali LagaresNo ratings yet
- Utilization Patterns of Multidetector Computed Tomography in Elective and Emergency Conditions: Indications, Exposure Risk, and Diagnostic GainDocument4 pagesUtilization Patterns of Multidetector Computed Tomography in Elective and Emergency Conditions: Indications, Exposure Risk, and Diagnostic GainJorge RodriguezNo ratings yet
- Screenshot 2024-05-10 at 2.21.25 AMDocument8 pagesScreenshot 2024-05-10 at 2.21.25 AMp6tsr5mg97No ratings yet
- Ghid Plex Brahial Conturaj PDFDocument7 pagesGhid Plex Brahial Conturaj PDFMiruna MafteiNo ratings yet
- Cine CT Withou A RespiratoryDocument20 pagesCine CT Withou A RespiratoryCan Trần KimNo ratings yet
- 2004 06578 PDFDocument19 pages2004 06578 PDFSumaNo ratings yet
- 2023-智能图像配准-attention guided refine and deformationDocument13 pages2023-智能图像配准-attention guided refine and deformationbo zhaoNo ratings yet
- Cone-Beam Computed Tomography and Its Applications in Dental and Maxillofacial RadiologyDocument11 pagesCone-Beam Computed Tomography and Its Applications in Dental and Maxillofacial RadiologyenzoNo ratings yet
- The Potential For Undertaking Slow CT Using A Modern CT ScannerDocument7 pagesThe Potential For Undertaking Slow CT Using A Modern CT ScannerAndreas RonaldNo ratings yet
- EHF2017 EK FinalPaperDocument9 pagesEHF2017 EK FinalPaperdanimalxNo ratings yet
- CT Scan in VeterinaryDocument4 pagesCT Scan in VeterinarySurajNo ratings yet
- Chapter 22 - Computed Tomography Simulation ProceduresDocument30 pagesChapter 22 - Computed Tomography Simulation ProceduresCarlo Gangcuangco ValdezNo ratings yet
- IEEE PAPER BATCH NO-03 A NOVEL OBJECT DETECTION MODEL (YOLOv5) FOR IMPROVED LUNG NODULE IDENTIFICATION IN MEDICAL IMAGESDocument7 pagesIEEE PAPER BATCH NO-03 A NOVEL OBJECT DETECTION MODEL (YOLOv5) FOR IMPROVED LUNG NODULE IDENTIFICATION IN MEDICAL IMAGESS.GOPINATH5035No ratings yet
- Optimization in Radiology Eur J Med PhysDocument6 pagesOptimization in Radiology Eur J Med PhysobbebbiNo ratings yet
- Deepa Govind - Worker Health and Safety Awareness in 4 Steps Certificate 1Document1 pageDeepa Govind - Worker Health and Safety Awareness in 4 Steps Certificate 1api-354040213No ratings yet
- Assignment 1 - Article Summary WordDocument3 pagesAssignment 1 - Article Summary Wordapi-354040213No ratings yet
- Nejm 200005043421801Document8 pagesNejm 200005043421801api-354040213No ratings yet
- Health 1Document3 pagesHealth 1api-354040213No ratings yet
- EncoderDocument6 pagesEncoderHue BachNo ratings yet
- Compal Confidential: P1VE6 LA7071P Schematics DocumentDocument37 pagesCompal Confidential: P1VE6 LA7071P Schematics DocumentChristiam OrtegaNo ratings yet
- A231 - BKAM3023 Guidelines For Project 2-Service LearningDocument4 pagesA231 - BKAM3023 Guidelines For Project 2-Service LearningKhar FattNo ratings yet
- Street Photography - The Complete Guide (PDFDrive)Document130 pagesStreet Photography - The Complete Guide (PDFDrive)Paolo FasselliNo ratings yet
- Advanced Shipping Configuration With Websphere Commerce Calculation FrameworkDocument49 pagesAdvanced Shipping Configuration With Websphere Commerce Calculation FrameworkjaneeshpjNo ratings yet
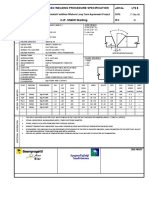
- Wps SmawDocument1 pageWps SmawFedericoC67% (3)
- Ict National and Intl PoliciesDocument38 pagesIct National and Intl PoliciesWeendy Gayle T. VelilaNo ratings yet
- Montealegre-Training Proposal For Demonstration TeachingDocument12 pagesMontealegre-Training Proposal For Demonstration TeachingMarcela Consigo Ramos100% (1)
- Asr Install FlowDocument1 pageAsr Install FlowKamaldeep NainwalNo ratings yet
- Hareda 427466857Document86 pagesHareda 427466857Abhishek HandaNo ratings yet
- ZA550KL RF Hardware Trouble Shooting GuideDocument42 pagesZA550KL RF Hardware Trouble Shooting GuideWenderson FeltrinNo ratings yet
- Obtaining Wien's Displacement Law of Electromagnetic RadiationDocument10 pagesObtaining Wien's Displacement Law of Electromagnetic RadiationVikas TanwarNo ratings yet
- 03 SM-Series Hardware (SM150)Document81 pages03 SM-Series Hardware (SM150)John WickNo ratings yet
- C5-Mechanical Propertise of Hardened Concrete Base On Sample Made in C4Document8 pagesC5-Mechanical Propertise of Hardened Concrete Base On Sample Made in C4Muhammad khairinNo ratings yet
- TOTAL Welding Control Procedure Rev.2 PDFDocument116 pagesTOTAL Welding Control Procedure Rev.2 PDFWenney N Pali100% (1)
- 030 826 4Document2 pages030 826 4Diego Orlando Santos BuitragoNo ratings yet
- Igcse English A Past Paper Quesstions and AnswersDocument6 pagesIgcse English A Past Paper Quesstions and Answersmsml kml100% (2)
- Chapter 1 Managers and ManagementDocument32 pagesChapter 1 Managers and ManagementHaris FadillahNo ratings yet
- Atmel 8051 Microcontroller Family - Product Selection GuideDocument17 pagesAtmel 8051 Microcontroller Family - Product Selection GuideRahul GargNo ratings yet
- BCL IndustriesDocument1 pageBCL IndustriesRanjan BeheraNo ratings yet
- Recording Studio DesignDocument16 pagesRecording Studio DesignValentino FantiniNo ratings yet
- Marijauna Grow Basics - Jorge CervantesDocument242 pagesMarijauna Grow Basics - Jorge Cervantessosh_s97% (36)
- Pipelines and Pipe NetworksDocument56 pagesPipelines and Pipe NetworksAlok KumarNo ratings yet
- Credits: o 267 State Council For Technical Education Nagaland Semester Mark SheetDocument9 pagesCredits: o 267 State Council For Technical Education Nagaland Semester Mark SheetU Are NiceNo ratings yet
- Water Plane ComputationDocument14 pagesWater Plane ComputationAchonk Gio VelenoNo ratings yet
- Android Guide With Imtiaz Saifullah: Email: Ping/Text: +92-331-7370872Document6 pagesAndroid Guide With Imtiaz Saifullah: Email: Ping/Text: +92-331-7370872Ali Hassan NaqviNo ratings yet
- DS4600 Series For Retail: The Versatile Scanner That Does More For Your Retail OperationsDocument4 pagesDS4600 Series For Retail: The Versatile Scanner That Does More For Your Retail Operationsndfgdfs oishdfNo ratings yet
- Lab - #3. - Riverine HydraulicsDocument8 pagesLab - #3. - Riverine HydraulicsJuan CallesNo ratings yet