Professional Documents
Culture Documents
Selective Serotonin Reuptake Inhibitors During Pregnancy and Risk of Stillbirth and Infant Mortality
Uploaded by
Riska Diene PratiwiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Selective Serotonin Reuptake Inhibitors During Pregnancy and Risk of Stillbirth and Infant Mortality
Uploaded by
Riska Diene PratiwiCopyright:
Available Formats
ORIGINAL CONTRIBUTION
Selective Serotonin Reuptake Inhibitors
During Pregnancy and Risk of Stillbirth
and Infant Mortality
Olof Stephansson, MD, PhD Importance Maternal psychiatric disease is associated with adverse pregnancy out-
Helle Kieler, MD, PhD comes. Use of selective serotonin reuptake inhibitors (SSRIs) during pregnancy has been
Bengt Haglund, PhD associated with congenital anomalies, neonatal withdrawal syndrome, and persistent
pulmonary hypertension of the newborn. However, the risk of stillbirth and infant mor-
Miia Artama, PhD tality when accounting for previous maternal psychiatric disease remains unknown.
Anders Engeland, PhD Objective To study risk of stillbirth and infant mortality associated with use of SSRIs
Kari Furu, PhD during pregnancy.
Mika Gissler, PhD Design, Setting, and Participants Population-based cohort study from all Nordic
countries (Denmark, Finland, Iceland, Norway, and Sweden) at different periods from 1996
Mette Nrgaard, MD, PhD through 2007. The study included women with singleton births. We obtained informa-
Rikke Beck Nielsen, MSc tion on maternal use of SSRIs from prescription registries. Maternal characteristics, preg-
Helga Zoega, PhD nancy, and neonatal outcomes were obtained from patient and medical birth registries.
Main Outcome Measures We used logistic regression to estimate relative risks of still-
Unnur Valdimarsdottir, PhD
birth, neonatal death, and postneonatal death associated with SSRI use during pregnancy
D
EPRESSION DURING PREG - taking into account maternal characteristics and previous psychiatric hospitalization.
nancy is common with Results Among 1 633 877 singleton births in the study, 6054 were stillbirths; 3609,
prevalences ranging be- neonatal deaths; and 1578, postneonatal deaths. A total of 29 228 (1.79%) of mothers
tween 7% and 19% in eco- had filled a prescription for an SSRI during pregnancy. Women exposed to an SSRI pre-
nomically developed countries.1,2 Ma- sented with higher rates of stillbirth (4.62 vs 3.69 per 1000, P=.01) and postneonatal
ternal depression is associated with death (1.38 vs 0.96 per 1000, P=.03) than those who did not. The rate of neonatal
poorer pregnancy outcomes,3,4 includ- death was similar between groups (2.54 vs 2.21 per 1000, P=.24). Yet in multivariable
models, SSRI use was not associated with stillbirth (adjusted odds ratio [OR], 1.17; 95%
ing increased risk of preterm delivery,
CI, 0.96-1.41; P=.12), neonatal death (adjusted OR, 1.23; 95% CI, 0.96-1.57; P=.11),
which in turn may cause neonatal mor- or postneonatal death (adjusted OR, 1.34; 95% CI, 0.97-1.86; P=.08). Estimates were
bidity and mortality.5 However, it is dif- further attenuated when stratified by previous hospitalization for psychiatric disease. The
ficult to disentangle whether such re- adjusted OR for stillbirth in women with a previous hospitalization for psychiatric dis-
productive hazards are caused by the ease was 0.92 (95% CI, 0.66-1.28; P=.62) and was 1.07 (95% CI, 0.84-1.36; P=.59)
underlying depression, the medical for those who had not been previously hospitalized. The corresponding ORs for neo-
treatment, or possible confounding by natal death were 0.89 (95% CI, 0.58-1.39; P=.62) for women who were hospitalized
lifestyle factors such as stress, alcohol and 1.14 (95% CI, 0.84-1.56; P=.39) for women who were not. For postneonatal death,
use, and smoking status.5 the ORs were 1.02 (95% CI, 0.61-1.69; P=.95) for women who were hospitalized and
1.10 (95% CI, 0.71-1.72; P=.66) for women who were not.
Management of depression during
pregnancy is a clinical challenge. The Conclusions and Relevance Among women with singleton births in Nordic coun-
Nordic countries generally recom- tries, no significant association was found between use of SSRIs during pregnancy and
risk of stillbirth, neonatal mortality, or postneonatal mortality. However, decisions about
mend a careful risk-benefit analysis of
use of SSRIs during pregnancy must take into account other perinatal outcomes and
each patient for treatment decisions. the risks associated with maternal mental illness.
Nonpharmaceutical interventions are JAMA. 2013;309(1):48-54 www.jama.com
generally recommended for milder con-
ditions while major depression is fre- Author Affiliations are listed at the end of this article.
quently treated with antidepressant commonly prescribed drugs for depres- Corresponding Author: Olof Stephansson, MD, PhD,
Clinical Epidemiology Unit, T2, Karolinska University
medication. Selective serotonin reup- sion during pregnancy. 6 Although Hospital Solna, SE-171 76 Stockholm, Sweden (olof
take inhibitors (SSRIs) are now the most somewhat equivocal, the evidence sug- .stephansson@ki.se).
48 JAMA, January 2, 2013Vol 309, No. 1 2013 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/926163/ on 05/22/2017
SSRIS DURING PREGNANCY AND INFANT MORTALITY
gests that SSRI use during pregnancy The start of follow-up was defined tation in Finland, Norway, Iceland, and
may be associated with poor birth out- from the initiation of the nationwide Denmark from 2004 onward, and af-
comes, such as congenital anomalies,7 prescription registry in each participat- ter 28 weeks in Sweden and Denmark
spontaneous abortion,8 neonatal with- ing country and end of follow-up by from 1997 through 2003), neonatal
drawal syndrome,9 and persistent pul- availability of registry data. We there- death (death within 0-27 days among
monary hypertension of the new- fore identified all singletons born after live born infants), and postneonatal
born.10,11 The influence of SSRI use on 154 gestational days between January death (death between 28-364 days
risk of stillbirth, neonatal death, and in- 1, 1996, and December 31, 2007, in among neonatal survivors). Informa-
fant death has been less studied.12 Denmark; January 1, 1996, and De- tion on stillbirth was obtained from the
Conversely, discontinuing antidepres- cember 31, 2006, in Finland; January medical birth registries in each coun-
sant treatment has been associated with 1, 2003, and December 31, 2007, in Ice- try and on neonatal and postneonatal
increased risk that pregnant women will land; January 1, 2005, and December deaths from the Nordic causes of death
experience a relapse of major depres- 31, 2007, in Norway; and January 1, registries, which contain information on
sion.13 According to a recent study on 2006, and December 31, 2007, in the date and causes of death for all in-
women delivering in Sweden in 2007, 3% Sweden. dividuals who were residents at the time
of women filled a prescription for anti- of death. All diagnoses and causes of
depressants in the 3-month period be- Ascertainment of Exposure death are classified according to the na-
fore conception while only 1% filled a Exposure was defined as 1 or more filled tional version of International Statisti-
prescription during the third trimes- prescriptions for an SSRI from 3 months cal Classification of Diseases, 10th Re-
ter.14 Maternal mental illness has con- before the start of pregnancy until birth. vision (ICD-10) codes.
sistently been associated with risks of in- Eligible pregnancies were identified
fant mortality15 and in particular sudden through the Nordic medical birth reg- Potential Confounders
infant death syndrome.16 istries along with data on maternal de- or Effect-Modifiers
Because the Nordic countries have mographics, the pregnancy, delivery, As possible confounders, we included
similar nationwide registries of births and neonatal period.18 Determination information from the birth registries on
and dispensed drugs, studies on the ef- of start of pregnancy and gestational age maternal age, parity, birth year, coun-
fect of medications on birth outcomes were based on prenatal ultrasound es- try of birth, and maternal smoking sta-
are possible. By using these data sources timation or on last menstrual pe- tus (not available in Iceland), and in-
and taking into account previous psy- riod.10,19 The prescription registries in formation on maternal diseases from
chiatric disease and maternal charac- the Nordic countries include data on the birth registries and patient registries
teristics, we aimed to elucidate whether dispensed item, substance, brand name, (except for Norway), although only hy-
SSRI exposure during pregnancy was and formulation together with date of pertension and diabetes were retained
associated with increased risks of still- dispensing for more than 95% of the in the final models. Women with dia-
birth, neonatal death, and postneona- total outpatient population. All drugs betes were identified by filled prescrip-
tal death. are classified according to the World tions of antidiabetic medications from
Health Organization Anatomical Thera- 3 months before pregnancy through de-
METHODS peutic Chemical (ATC) classification. livery using prescription registries.
We conducted a registry-based cohort The SSRIs used during the study pe- Complications and maternal diseases
study that included women and their riod and included in the analyses were are recorded according to the ICD-10
infants born in the Nordic countries fluoxetine, citalopram, paroxetine, ser- codes.
(Denmark, Finland, Iceland, Norway, traline, fluvoxamine, and escitalo- Because psychiatric disease has been
and Sweden) between 1996 and 2007. pram (eTable 1 available at http://www associated with the outcomes under
Each Nordic country has national reg- .jama.com). In general, prescriptions are study15 and SSRI use, we obtained avail-
istries, which include prospectively col- filled for a maximum of 3 months.20 We able information from each country on
lected health and social information on excluded pregnancies and births the previous psychiatric hospitaliza-
all inhabitants. All registries include the (n = 5396) of mothers who had used tions of the mothers. The patient reg-
Civil Personal Registration (CPR) num- other antidepressants with an effect on istries in Denmark, Finland, Iceland,
bers, a unique number assigned to each serotonin or norepinephrine activity and Sweden record information on all
resident at birth or immigration. Re- (imipramine, amitriptyline, dulox- hospitalizations (including treatment of
porting to the registries is mandatory etine, dosulepine, melnacipran, trazo- psychiatric disorders), with date of ad-
and regulated by national laws. The na- done, nefazodone, and moklobemide). mission and discharge, and primary and
tional parliaments in the Nordic coun- secondary diagnoses. Additionally, the
tries have on behalf of their popula- Ascertainment of Outcome Danish Psychiatric Central Register in-
tions given informed consent to be We assessed 3 outcomes: stillbirth (in- cludes information on psychiatric treat-
included in the registries.17 trauterine death after 22 weeks of ges- ments at specialized psychiatric clin-
2013 American Medical Association. All rights reserved. JAMA, January 2, 2013Vol 309, No. 1 49
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/926163/ on 05/22/2017
SSRIS DURING PREGNANCY AND INFANT MORTALITY
ics and emergency care units.21 During the study period, we calculated esti- were due to perinatal conditions;
the study period, the Norwegian pa- mates using clustered data in the gen- 28.10%, congenital anomalies; 7.83%,
tient registry did not contain CPR num- eralized estimation equation method. chromosomal abnormalities; 1.57%,
bers, which are needed for linkages to We finally present rates of specific sudden infant death syndrome; 0.29%,
other registries. Thus, we included data causes of death for neonatal and post- external causes; and 6.43%, other causes
on the mothers previous psychiatric neonatal mortality. (eTable 2). Of the postneonatal deaths,
hospitalizations from patient regis- All analyses were conducted using 29.54% were due to congenital anoma-
tries in Denmark, Iceland, Sweden, and SAS software, version 9.2 (SAS Insti- lies; 20.33%, sudden infant death syn-
Finland and from the Danish Psychi- tute Inc). We used a significance level drome; 11.57%, perinatal conditions;
atric Central Register during a 10-year of .05 (2-sided testing). The study was 6.47%, chromosomal abnormalities;
period before giving birth. For Nor- approved by the Regional Ethical Re- 5.10%, external causes; and 26.99%,
way, previous psychiatric treatments view Board at Karolinska Institute in other causes (eTable 2).
were obtained from the medical birth Stockholm, Sweden; the National Board
registry; information on past medical of Health, Denmark; the Danish Data SSRIs and Risks of Stillbirth,
history, including treatment for psy- Protection Agency; the National Insti- Neonatal Death,
chiatric disease, is reviewed with the tute for Health and Welfare of Fin- and Postneonatal Death
mother during antenatal care by a gen- land; Statistics Finland; the Data Pro- In total, 135 stillbirths, 74 neonatal
eral practitioner, midwife, or an obste- tection Authority and the National deaths, and 40 postneonatal deaths
trician and then later recorded in the Bioethics Committee in Iceland; and the occurred among mothers exposed to
medical birth registry. Norwegian Data Inspectorate. SSRI during pregnancy. Compared
with women who were unexposed,
Statistical Analyses RESULTS those who were exposed to SSRIs
We used logistic regression analysis to Descriptive Data presented with higher rates of still-
estimate the association of SSRI use dur- In total 1 633 877 singleton births birth (4.62 vs 3.69 per 1000 births)
ing pregnancy with 3 outcomes: still- occurred during the study periods with a crude OR of 1.25 (95% CI,
birth, neonatal death, and postneona- and were included in the analysis. Of 1.06-1.49; P = .01) and postneonatal
tal death. Women with missing data on these, in 29 228 births (1.79%), the death (1.38 vs 0.96 per 1000) with a
any of the covariates were excluded mother had filled a prescription for an crude OR of 1.43 (95% CI, 1.04-1.96;
from the multivariable analysis. Be- SSRI during pregnancy. Of those P = .03; TABLE 2). Selective serotonin
cause information on cigarette smok- women, 91.21% used a single SSRI. reuptake inhibitor use was not asso-
ing was missing in 9.5% of exposed and Filling of SSRI prescriptions was more ciated with increased risk of neonatal
6.2% of unexposed women, we per- common in the later years of the death (2.54 vs 2.21 per 1000) with a
formed a sensitivity analysis that in- study period (TABLE 1). The mothers crude OR of 1.15 (95% CI, 0.91-1.45;
cluded women whose smoking status who had filled a prescription with an P = .24). After adjusting for maternal
was missing by adding smoking as a SSRI were generally older, more often characteristics, country, and year of
separate category in the multivariable smokers, previously hospitalized for birth, SSRI exposure was no longer
analysis. psychiatric disease, and more likely to significantly associated with stillbirth
Analyses were performed using crude have diabetes and hypertension than (adjusted OR, 1.17; 95% CI, 0.96-
and adjusted odds ratios (ORs) with mothers not using SSRIs. The most 1.41; P = .12) or postneonatal death
95% CIs. In stratified analyses, we fur- frequently filled SSRI prescription was (adjusted OR, 1.34; 95% CI, 0.97-
ther explored whether history of ma- for citalopram (6.49 per 1000) fol- 1.86; P = .08). The adjusted OR for
ternal psychiatric hospitalization modi- lowed by fluoxetine (4.66 per 1000) neonatal death was 1.23 (95% CI,
fied the association between SSRI use and sertraline (3.93 per 1000). The 0.96-1.57; P = .11). In the sensitivity
during pregnancy and risk of still- distribution of the different SSRI use analysis including women with miss-
birth, neonatal death, and postneona- is presented in eTable 1 (available at ing data on smoking in early preg-
tal death. We also analyzed ORs for http://www.jama.com). nancy, the estimates were only mar-
SSRIs by time of exposure during preg- The 6054 stillbirths corresponded to ginally altered.
nancy divided into (1) only within 3 a rate of 3.71 per 1000 births. The 3609 When we stratified by previous psy-
months before first trimester, (2) only neonatal deaths corresponded to a rate chiatric hospitalization, estimates for
before and during first trimester, (3) be- of 2.22 per 1000 live births, and 1578 stillbirth, neonatal death, and postneo-
fore and during first and second tri- postneonatal deaths corresponded to a natal death were attenuated (Table 2).
mester, and (4) before and during the rate of 0.97 per 1000 live births. A cause The adjusted OR for stillbirth in women
entire pregnancy. Because observa- of death was reported in 96.92% of neo- who were previously hospitalized for
tions are not independent in women natal and 96.96% of postneonatal a psychiatric disease was 0.92 (95% CI,
who delivered more than once during deaths. Of the neonatal deaths, 55.77% 0.66-1.28; P=.62) and was 1.07 (95%
50 JAMA, January 2, 2013Vol 309, No. 1 2013 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/926163/ on 05/22/2017
SSRIS DURING PREGNANCY AND INFANT MORTALITY
CI, 0.84-1.36; P=.59) for women who COMMENT Data on potential risks of stillbirth
were not. For neonatal death, the ad- The present study of more than 1.6 mil- and infant mortality by SSRI use are
justed ORs were 0.89 (95% CI, 0.58- lion births suggests that SSRI use dur- scarce. Recently the Danish Medi-
1.39; P=.62) for women previously hos- ing pregnancy was not associated with cines Agency reported 2 cases of neo-
pitalized and 1.14 (95% CI, 0.84-1.56; increased risks of stillbirth, neonatal natal death following use of fluox-
P=.39) for women who were not. For death, or postneonatal death. The in- etine in pregnancy.22 To our knowledge,
postneonatal death, the adjusted OR was creased rates of stillbirth and postneo- only 2 studies have specifically ad-
1.02 (95% CI, 0.61-1.69; P = .95) for natal mortality among infants ex- dressed the risk of stillbirth or infant
women who were hospitalized and 1.10 posed to an SSRI during pregnancy were death after prenatal SSRI exposure. Ku-
(95% CI, 0.71-1.72; P=.66) for women explained by the severity of the under- lin et al23 did not find any increased risk
who were not. Because information on lying maternal psychiatric disease and of stillbirth among 267 women ex-
previous hospitalization could not be ob- unfavorable distribution of maternal posed to SSRIs. Colvin et al24 recently
tained from Norway, we performed a characteristics such as cigarette smok- reported no increased risk of stillbirth
sensitivity analysis excluding Norwe- ing and advanced maternal age. but found an increased risk of infant
gian data, which demonstrated only mar-
ginal changes in the point estimates
(eTable 3, available at http://www.jama Table 1. Maternal Characteristics by Exposure to Selective Serotonin Reuptake Inhibitors
.com). When restricting the analysis for From 3 Months Before Pregnancy Until Birth Among Singleton Births
stillbirths to include gestational age 22 No. (%) of Births
weeks or longer, the adjusted OR was Total Unexposed SSRI
1.16 (95% CI, 0.92-1.47; P=.21) and for (N=1 633 877) (n = 1 604 649) (n = 29 228)
28 weeks or longer, 1.07 (95% CI, 0.86- Country
1.34; P=.55). Denmark 687 756 (42.1) 677 349 (42.2) 10 407 (35.6)
TABLE 3 presents associated risks Finland 611 245 (37.4) 600 946 (37.5) 10 299 (35.2)
Iceland 19 567 (1.2) 18 262 (1.1) 1305 (4.5)
with SSRI use by trimester of expo-
Norway 166 783 (10.2) 164 030 (10.2) 2753 (9.4)
sure. Among women exposed from 3
Sweden 148 526 (9.1) 144 062 (9.0) 4464 (15.3)
months before pregnancy and during
Year of birth
the first trimester, there was an in- 1996-1999 417 672 (25.6) 414 521 (25.8) 3151 (10.8)
crease in the OR for stillbirth com- 2000-2003 469 603 (28.7) 462 205 (28.8) 7398 (25.3)
pared with unexposed (adjusted OR, 2004-2007 746 602 (45.7) 727 923 (45.4) 18 679 (63.9)
1.56; CI, 1.06-2.30; P = .03), whereas Maternal age, y
this was not observed when the expo- 24 266 627 (16.3) 261 313 (16.3) 5314 (18.2)
sure window included from 3 months 25-34 1 081 309 (66.2) 1 063 726 (66.3) 17 583 (60.2)
before pregnancy to the first and sec- 35-44 284 063 (17.4) 277 794 (17.3) 6269 (21.4)
ond trimester or entire pregnancy. For 45 1878 (0.1) 1816 (0.1) 62 (0.2)
women exposed to an SSRI from be- Birth order
1 690 209 (42.2) 677 628 (42.2) 12 581 (43.0)
fore pregnancy through the first tri-
2-3 818 471 (50.1) 804 809 (50.2) 13 662 (46.7)
mester, the adjusted OR for stillbirth
4 117 944 (7.2) 115 082 (7.2) 2862 (9.8)
among women hospitalized for a psy-
Missing 7253 (0.4) 7130 (0.4) 123 (0.4)
chiatric disease was 1.04 (95% CI, 0.54-
Smoking in early pregnancy
2.02; P = .90) and was 1.64 (95% CI, No 1 275 808 (78.1) 1 257 358 (78.4) 18 450 (63.1)
1.08-2.50; P=.02) for women who were Yes 255 243 (15.6) 247 229 (15.4) 8014 (27.4)
not hospitalized. For neonatal and post- Missing 102 826 (6.3) 100 062 (6.2) 2764 (9.5)
neonatal deaths, no significant associa- Previous psychiatric hospitalization a
tions were observed by trimester of ex- No 1 570 597 (96.1) 1 549 430 (96.6) 21 167 (72.4)
posure. We then estimated risks of Yes 63 280 (3.9) 55 219 (3.4) 8061 (27.6)
neonatal and postneonatal mortality by Diabetes b
No 1 617 247 (99.0) 1 588 610 (99.0) 28 637 (98.0)
cause of death. However, no signifi- Yes 16 630 (1.0) 16 039 (1.0) 591 (2.0)
cant associations between maternal Hypertension
SSRI and specific causes of death were No 1 624 395 (99.4) 1 595 378 (99.4) 29 017 (99.3)
found (eTable 2). Yes 9482 (0.6) 9271 (0.6) 211 (0.7)
Finally, absolute rates of stillbirth, Abbreviation: SSRI, selective serotonin reuptake inhibitor.
a Maternal hospitalizations for a psychiatric diagnosis during a 10-year period before giving birth recorded in patient reg-
neonatal death, and postneonatal death istries for Denmark, Finland, Iceland, and Sweden, and the Danish Psychiatric Central Register. For Norway defined as
varied by specific SSRI type during preg- psychiatric disease recorded in the birth registry.
b Defined as use of antidiabetes drugs from 90 days before last menstrual period to birth.
nancy (eTable 4).
2013 American Medical Association. All rights reserved. JAMA, January 2, 2013Vol 309, No. 1 51
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/926163/ on 05/22/2017
SSRIS DURING PREGNANCY AND INFANT MORTALITY
Table 2. Exposure to Selective Serotonin Reuptake Inhibitors From 3 Months Before Pregnancy Until Birth and Risk of Stillbirth and Infant Mortality
Exposure
SSRI No SSRI
Crude OR P Adjusted a OR P
No. Per 1000 No. Per 1000 (95%CI) Value (95%CI) Value
Stillbirth 135 4.62 5919 3.69 1.25 (1.06-1.49) .01 1.17 (0.96-1.41) .12
No previous psychiatric hospitalization 84 3.97 5542 3.58 1.11 (0.89-1.38) .34 1.07 (0.84-1.36) .59
Previous psychiatric hospitalization b 51 6.33 377 6.83 0.93 (0.69-1.25) .61 0.92 (0.66-1.28) .62
Neonatal death 74 2.54 3535 2.21 1.15 (0.91-1.45) .24 1.23 (0.96-1.57) .11
No previous psychiatric hospitalization 45 2.13 3297 2.14 1.00 (0.74-1.34) .99 1.14 (0.84-1.56) .39
Previous psychiatric hospitalization b 29 3.62 238 4.34 0.83 (0.56-1.24) .37 0.89 (0.58-1.39) .62
Postneonatal death 40 1.38 1538 0.96 1.43 (1.04-1.96) .03 1.34 (0.97-1.86) .08
No previous psychiatric hospitalization 23 1.09 1401 0.91 1.20 (0.80-1.82) .38 1.10 (0.71-1.72) .66
Previous psychiatric hospitalization b 17 2.13 137 2.51 0.85 (0.51-1.41) .52 1.02 (0.61-1.69) .95
Abbreviation: OR, odds ratio; SSRI, serotonin reuptake inhibitor.
a Adjusted for country and year of birth, maternal age, birth order, smoking in early pregnancy, and maternal diabetes and hypertension. Women with no SSRI were the reference.
b Maternal hospitalizations for a psychiatric diagnosis during a 10-year period before giving birth recorded in patient registries for Denmark, Finland, Iceland, Sweden, and the Danish
Psychiatric Central Register. For Norway defined as psychiatric disease recorded in the birth registry.
womenwithpreviouspsychiatricdisease.
Table 3. Exposure to Selective Serotonin Reuptake Inhibitor per Trimester and Risk of Stillbirth In our study, when taking disease sever-
and Infant Mortality
ity and maternal characteristics into con-
No. of
Outcome, Trimester Women Adjusted OR P sideration, women taking SSRIs did not
of SSRI Exposure a Exposed Per 1000 (95% CI) b Value have an increased risk of stillbirth or in-
Stillbirth fant death.
T0 49 4.92 1.19 (0.87-1.65) .28
We were able to study risk of still-
T0-T1 31 6.17 1.56 (1.06-2.30) .03
birth and infant mortality among SSRI
T0-T2 8 4.94 1.11 (0.50-2.48) .80
users by trimester of pregnancy. Al-
T0-T3 14 3.71 0.94 (0.53-1.65) .83
though the risk of stillbirth appeared to
Other 33 3.73 1.01 (0.70-1.46) .94
be increased among women exposed be-
Unexposed 5919 3.69 1 [Reference]
Neonatal death
fore pregnancy through the first trimes-
T0 22 2.22 1.04 (0.66-1.64) .86 ter, these results should be interpreted
T0-T1 12 2.40 1.16 (0.61-2.21) .65 with caution due to the few observa-
T0-T2 4 2.48 1.35 (0.51-3.62) .55 tions for each category of exposure. Yet,
T0-T3 13 3.45 1.56 (0.86-2.83) .14 a possible explanation for this finding
Other 23 2.61 1.31 (0.85-2.02) .22 may be the increased risk of congenital
Unexposed 3535 2.21 1 [Reference] anomalies reported to be associated with
Postneonatal death SSRI use including fluoxetine and ser-
T0 14 1.42 1.28 (0.72-2.26) .40 traline.7 Risk estimates for neonatal death
T0-T1 5 1.00 1.02 (0.42-2.46) .96
appeared not to differ by trimester ex-
T0-T2 3 1.87 2.06 (0.66-6.39) .21
posure. However, the number of ex-
T0-T3 6 1.60 1.76 (0.79-3.93) .17
posed women in this analysis was re-
Other 12 1.36 1.31 (0.72-2.37) .38
stricted and estimates should be
Unexposed 1538 0.96 1 [Reference]
interpreted with caution.
Abbreviations: OR, odds ratio, SSRI, selective serotonin reuptake inhibitor.
a T0 denotes from 3 months before until last menstrual period before pregnancy; T1, first trimester; T2, second trimes-
ter; and T3, third trimester.
b Adjusted for country and year of birth, maternal age, birth order, smoking in early pregnancy, and maternal diabetes
Strengths and Limitations
and hypertension. This cohort study was population
based, using information on almost all
singleton births in the 5 Nordic coun-
mortality among 3703 Australian wom- bySSRIusehavemostlybeensmall(250 tries during the study period. The large
en exposed to SSRIs. Whether the risk of exposedwomen)andsomehavereported size enabled us to study rare preg-
infant mortality was due to prenatal ex- increasedrisks,25 whileothershavenot.23,26 nancy outcomes such as stillbirth, neo-
posure to SSRIs or underlying maternal The small size of the studies along with natal death, and postneonatal death.
psychiatric disease could not be deter- other methodological problems has ham- The minimal clinically detectable dif-
mined from these studies. The few stud- peredsolidconclusions.16 Finally,1study15 ferences for an assumed power of 86%
iesexploringpotentialrisksofmiscarriages found increased infant mortality among (given 1.6 million pregnancies, 2% of
52 JAMA, January 2, 2013Vol 309, No. 1 2013 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/926163/ on 05/22/2017
SSRIS DURING PREGNANCY AND INFANT MORTALITY
mothers exposed to SSRIs, and the an- women without previous psychiatric sants when planning pregnancy. Con-
ticipated rates of outcomes) were ORs hospitalization. sequently, we may have underesti-
of 1.3 for stillbirth, 1.4 for neonatal We also do not know what psychi- mated the proportion of women using
death, and 1.6 for postneonatal death. atric disease was responsible for hos- SSRIs during pregnancy. The start of the
Because these are small, the study is un- pitalizations. Although SSRIs are used study period varied by country be-
likely to be underpowered. for depression, they also may be used cause it was set by the year prescrip-
In addition, information on SSRI for women with a history of bipolar dis- tion data were available. This should not
exposure and maternal characteristics order or schizophrenia. Because the out- introduce bias because we have com-
was prospectively collected, excluding come under study is rare, we may have plete follow-up data for all pregnan-
the possibility of recall bias. The study reduced power in stratified analyses by cies and end points for each country
included information on maternal previous psychiatric hospitalization and during the periods they provided data.
smoking, which was more common for specific trimester use during preg- Furthermore, we included both coun-
among women with SSRI use and has nancy, as seen by the wide CIs. Con- try of origin and calendar year in our
been associated with stillbirth and sequently, despite being the largest models.
neonatal mortality.27 Furthermore, in study investigating this question, the In conclusion, we found that after
sensitivity analyses, we evaluated lack of power in the subanalyses has to taking maternal characteristics and psy-
women with missing data on smoking be considered a limitation and these re- chiatric disease hospitalizations into ac-
in early pregnancy. We did not have sults should be interpreted with count, there was no significant asso-
information on alcohol intake during caution. ciation between use of SSRIs during
pregnancy or use of illegitimate drugs, In the present study, we did not have pregnancy and risk of stillbirth, neo-
and the use of these could be related information on spontaneous and in- natal mortality, or postneonatal mor-
to SSRI use as well as stillbirth and duced abortions. It is therefore pos- tality. However, decisions regarding use
infant death. However, since we did sible that we have underestimated an of SSRIs during pregnancy must take
not observe any association between association between SSRI use and ad- into account other perinatal outcomes
SSRIs and stillbirth or infant death, verse pregnancy outcome if women ex- and the risks associated with maternal
the absence of this information may posed to SSRIs were more likely to have mental illness.
be of limited concern. a spontaneous or induced abortion be- Author Affiliations: Centre for Pharmacoepidemiol-
Our study considered previous psy- cause of a severe congenital abnormal- ogy and Clinical Epidemiology Unit, Department of
Medicine Solna, Karolinska Institutet, Stockholm (Drs
chiatric disease. For Denmark, Fin- ity. Because inclusion of stillbirths by Stephansson, Kieler, and Haglund); Department of
land, Iceland, and Sweden, this infor- gestational age differed between coun- Womens and Childrens Health, Karolinska Institu-
tet, Stockholm (Dr Stephansson); and the Nordic School
mation was obtained from recorded tries for the study period, we pre- of Public Health, Gothenburg (Dr Gissler), Sweden;
hospitalizations. In Norway, informa- sented estimates for stillbirths from the THL National Institute for Health and Welfare, Hel-
tion on previous psychiatric disease was gestational age of 22 weeks and longer sinki, Finland (Drs Artama and Gissler); Division of Epi-
demiology, Department of Pharmacoepidemiology,
obtained from the birth registry, which and for the gestational age of 28 weeks Norwegian Institute of Public Health, Oslo (Drs En-
may be a concern because it differs from and longer. However, choice of gesta- geland and Furu); Department of Public Health and
Primary Health Care, University of Bergen, Bergen (Dr
the data from the other countries. How- tional week for defining stillbirth did Engeland); Department of Pharmacy, University of
ever, excluding Norwegian data did not not influence the results because we Troms, Troms, Norway (Dr Furu); Department of
Clinical Epidemiology, Institute of Clinical Medicine,
alter the results. found no association between SSRI ex- Aarhus University Hospital, Aarhus, Denmark (Dr
Apart from previous psychiatric hos- posure and stillbirth for either gesta- Nrgaard and Mrs Nielsen); Centre of Public Health
Sciences, School of Health Sciences, University of Ice-
pitalization, we did not have detailed tional age cutoff. land, Reykjavik, Iceland (Drs Zoega and Valdimars-
information on the severity of the dis- Information on dispensed drugs is dottir); Department of Epidemiology, School of Pub-
ease or any information on mild de- not the same as intake of drugs. A re- lic Health, Harvard University, Boston, Massachusetts
(Dr Valdimarsdottir); and Institute for Translational Epi-
pression treated in outpatient psychi- cent Swedish study showed close to demiology, Mount Sinai School of Medicine, New York,
atric clinics or by general practitioners. 60% agreement of maternal antidepres- New York (Dr Zoega).
Author Contributions: Dr Stephansson had full ac-
Relative risk estimates for adverse out- sant use, when comparing informa- cess to all of the data in the study and takes respon-
comes by SSRI use during pregnancy tion on dispensed drugs and reported sibility for the integrity of the data and the accuracy
of the data analysis.
were generally higher among women drug intake at the first antenatal care Study concept and design: Stephansson, Kieler,
without previous hospitalization for visit.14 Whether this moderate agree- Haglund, Artama, Engeland, Gissler, Nrgaard,
psychiatric disease than women with ment reflects a lower drug intake com- Valdimardottir.
Acquisition of data: Kieler, Haglund, Engeland, Furu,
previous hospitalization. Hence it is pared with dispensing or unwilling- Gissler, Nrgaard, Nielsen, Zoega, Valdimardottir.
possible that residual confounding ness to report intake of antidepressants Analysis and interpretation of data: Stephansson,
Kieler, Haglund, Engeland, Nrgaard, Zoega,
due to unmeasured mild psychiatric at antenatal care is unknown. We also Valdimardottir.
disorders treated in outpatient clinics did not have information on dosage lev- Drafting of the manuscript: Stephansson,
Valdimardottir.
or among general practitioners affects els. In addition, it is possible that Critical revision of the manuscript for important in-
our estimates in the population of women lower their dose of antidepres- tellectual content: Stephansson, Kieler, Haglund,
2013 American Medical Association. All rights reserved. JAMA, January 2, 2013Vol 309, No. 1 53
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/926163/ on 05/22/2017
SSRIS DURING PREGNANCY AND INFANT MORTALITY
Artama, Engeland, Furu, Gissler, Nrgaard, Nielsen, nancy and neonatal outcomes. Am J Psychiatry. 2009; take inhibitors and the risk of spontaneous abortions.
Zoega, Valdimardottir. 166(5):557-566. CNS Spectr. 2008;13(11):960-966.
Statistical analysis: Haglund. 6. Bakker MK, Kolling P, van den Berg PB, de Walle 17. Rosen M. National Health Data Registers: a Nordic
Obtained funding: Kieler. HE, de Jong van den Berg LT. Increase in use of se- heritage to public health. Scand J Public Health. 2002;
Administrative, technical, or material support: Kieler, lective serotonin reuptake inhibitors in pregnancy dur- 30(2):81-85.
Haglund, Artama, Nrgaard, Zoega. ing the last decade, a population-based cohort study 18. Gissler M, Louhiala P, Hemminki E. Nordic Medi-
Study supervision: Kieler, Nrgaard. from the Netherlands. Br J Clin Pharmacol. 2008; cal Birth Registers in epidemiological research. Eur J
Conflict of Interest Disclosures: All authors have com- 65(4):600-606. Epidemiol. 1997;13(2):169-175.
pleted and submitted the ICMJE Form for Disclosure 7. Louik C, Lin AE, Werler MM, Hernandez-Daz S, 19. Hgberg U, Larsson N. Early dating by ultra-
of Potential Conflicts of Interest and none were re- Mitchell AA. First-trimester use of selective serotonin- sound and perinatal outcome: a cohort study. Acta Ob-
ported. reuptake inhibitors and the risk of birth defects. N Engl stet Gynecol Scand. 1997;76(10):907-912.
Funding/Support: This study was funded by the Swed- J Med. 2007;356(26):2675-2683. 20. Furu K, Wettermark B, Andersen M, Martikainen
ish Pharmacy Company and by the authors affilia- 8. Hemels ME, Einarson A, Koren G, Lanctot KL, JE, Almarsdottir AB, Srensen HT. The Nordic coun-
tions. Olof Stephansson was supported by a postdoc- Einarson TR. Antidepressant use during pregnancy and tries as a cohort for pharmacoepidemiological research.
torate scholarship from the Swedish Society of the rates of spontaneous abortions: a meta-analysis. Basic Clin Pharmacol Toxicol. 2010;106(2):86-
Medicine. Ann Pharmacother. 2005;39(5):803-809. 94.
Disclaimer: The Swedish Pharmacy Company was not 9. Sanz EJ, De-las-Cuevas C, Kiuru A, Bate A, Edwards 21. Munk-Jrgensen P, Mortensen PB. The Danish
involved in the design and conduct of the study; col- R. Selective serotonin reuptake inhibitors in pregnant Psychiatric Central Register. Dan Med Bull. 1997;
lection, management, analysis, or interpretation of the women and neonatal withdrawal syndrome: 44(1):82-84.
data; and preparation, review, or approval of the manu- a database analysis. Lancet. 2005;365(9458):482- 22. Agency DM. Risk of death or serious side ef-
script. 487. fects in newborns following exposure to antidepres-
Online-Only Material: The eTables are available at 10. Kieler H, Artama M, Engeland A, et al. Selective sants (fluoxetine and other SSRIs). 2011; http:
http://www.jama.com. serotonin reuptake inhibitors during pregnancy and //laegemiddelstyrelsen.dk/en/topics/side-effects
risk of persistent pulmonary hypertension in the new- -and-trials/side-effects/news/risk-of-death-or
born: population based cohort study from the five Nor- -serious-side-effects-in--ther-ssris. Accessed Decem-
REFERENCES dic countries. BMJ. 2012;344:d8012. ber 7, 2012.
11. Chambers CD, Hernandez-Diaz S, Van Marter 23. Kulin NA, Pastuszak A, Sage SR, et al. Pregnancy
1. Evans J, Heron J, Francomb H, Oke S, Golding J. LJ, et al. Selective serotonin-reuptake inhibitors and outcome following maternal use of the new selective
Cohort study of depressed mood during pregnancy risk of persistent pulmonary hypertension of the serotonin reuptake inhibitors: a prospective con-
and after childbirth. BMJ. 2001;323(7307):257- newborn. N Engl J Med. 2006;354(6):579-587. trolled multicenter study. JAMA. 1998;279(8):
260. 12. Udechuku A, Nguyen T, Hill R, Szego K. Antide- 609-610.
2. Lee AM, Lam SK, Sze Mun Lau SM, Chong CS, Chui pressants in pregnancy: a systematic review. Aust 24. Colvin L, Slack-Smith L, Stanley FJ, Bower C. Early
HW, Fong DY. Prevalence, course, and risk factors for N Z J Psychiatry. 2010;44(11):978-996. morbidity and mortality following in utero exposure
antenatal anxiety and depression. Obstet Gynecol. 13. Cohen LS, Altshuler LL, Harlow BL, et al. Relapse to selective serotonin reuptake inhibitors: a population-
2007;110(5):1102-1112. of major depression during pregnancy in women who based study in Western Australia. CNS Drugs. 2012;
3. Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W. De- maintain or discontinue antidepressant treatment. 26(7):e1-e14.
pression and anxiety during pregnancy: a risk factor JAMA. 2006;295(5):499-507. 25. Klieger-Grossmann C, Weitzner B, Panchaud A,
for obstetric, fetal and neonatal outcome? a critical 14. Stephansson O, Granath F, Svensson T, Haglund et al. Pregnancy outcomes following use of escitalo-
review of the literature. J Matern Fetal Neonatal Med. B, Ekbom A, Kieler H. Drug use during pregnancy in pram: a prospective comparative cohort study. J Clin
2007;20(3):189-209. Swedenassessed by the Prescribed Drug Register and Pharmacol. 2012;52(5):766-770.
4. Yonkers KA, Wisner KL, Stewart DE, et al. The the Medical Birth Register. Clin Epidemiol. 2011; 26. Chalmers JW, Shanks E, Paterson S, McInneny
management of depression during pregnancy: a re- 3:43-50. K, Baird D, Penney G. Scottish data on intrapartum
port from the American Psychiatric Association and 15. Nilsson E, Hultman CM, Cnattingius S, Olausson related deaths are in same direction as Welsh data.
the American College of Obstetricians and PO, Bjork C, Lichtenstein P. Schizophrenia and BMJ. 1998;317(7157):539-540.
Gynecologists. Gen Hosp Psychiatry. 2009;31(5): offsprings risk for adverse pregnancy outcomes and 27. Cnattingius S. The epidemiology of smoking dur-
403-413. infant death. Br J Psychiatry. 2008;193(4):311- ing pregnancy: smoking prevalence, maternal char-
5. Wisner KL, Sit DK, Hanusa BH, et al. Major de- 315. acteristics, and pregnancy outcomes. Nicotine Tob Res.
pression and antidepressant treatment: impact on preg- 16. Gentile S. Pregnancy exposure to serotonin reup- 2004;6(suppl 2):S125-S140.
54 JAMA, January 2, 2013Vol 309, No. 1 2013 American Medical Association. All rights reserved.
Downloaded From: http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/926163/ on 05/22/2017
You might also like
- TensimeterDocument10 pagesTensimeterRiska Diene PratiwiNo ratings yet
- Journal of Substance Abuse Treatment: Carla J. Rash, PH.D., Sheila M. Alessi, PH.D., Nancy M. Petry, PH.DDocument6 pagesJournal of Substance Abuse Treatment: Carla J. Rash, PH.D., Sheila M. Alessi, PH.D., Nancy M. Petry, PH.DRiska Diene PratiwiNo ratings yet
- (New) Pemeriksaan Radiologi Pada Kegawat DaruratanDocument107 pages(New) Pemeriksaan Radiologi Pada Kegawat DaruratanRiska Diene PratiwiNo ratings yet
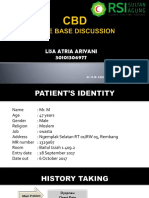
- Case Based Discussion (CBD) : AdvisorDocument92 pagesCase Based Discussion (CBD) : AdvisorRiska Diene PratiwiNo ratings yet
- Riska Diene Pratiwi 30101307064: Advisor: Dr. H. M. Saugi Abduh, SP - PD., KKV, FinasimDocument62 pagesRiska Diene Pratiwi 30101307064: Advisor: Dr. H. M. Saugi Abduh, SP - PD., KKV, FinasimRiska Diene PratiwiNo ratings yet
- High-Flow Nasal Cannulae in Very Preterm Infants After ExtubationDocument9 pagesHigh-Flow Nasal Cannulae in Very Preterm Infants After ExtubationRiska Diene PratiwiNo ratings yet
- Lisa Atria Ariyani 30101306977: Advisor: Dr. H. M. Saugi Abduh, SP - PD., KKV, FinasimDocument62 pagesLisa Atria Ariyani 30101306977: Advisor: Dr. H. M. Saugi Abduh, SP - PD., KKV, FinasimRiska Diene PratiwiNo ratings yet
- Maternal MicronutrientDocument8 pagesMaternal MicronutrientRiska Diene PratiwiNo ratings yet
- Maternal Diet, BreastfeedingDocument6 pagesMaternal Diet, BreastfeedingRiska Diene PratiwiNo ratings yet
- Effects of Targeting Higher Vs Lower Arterial Oxygen Saturations On Death or Disability in Extremely Preterm InfantsDocument10 pagesEffects of Targeting Higher Vs Lower Arterial Oxygen Saturations On Death or Disability in Extremely Preterm InfantsRiska Diene PratiwiNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Rita Ora - Shine Ya LightDocument4 pagesRita Ora - Shine Ya LightkatparaNo ratings yet
- DBA Daily StatusDocument9 pagesDBA Daily StatuspankajNo ratings yet
- 2501 Mathematics Paper+with+solution EveningDocument10 pages2501 Mathematics Paper+with+solution EveningNenavath GaneshNo ratings yet
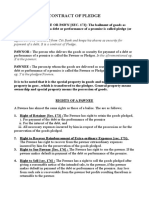
- Contract of PledgeDocument4 pagesContract of Pledgeshreya patilNo ratings yet
- Thermal Physics Questions IB Question BankDocument43 pagesThermal Physics Questions IB Question BankIBBhuvi Jain100% (1)
- Favis vs. Mun. of SabanganDocument5 pagesFavis vs. Mun. of SabanganAyra CadigalNo ratings yet
- HRM and The Business EnvironmentDocument18 pagesHRM and The Business Environmentsuzzette91No ratings yet
- Personal Philosophy of Education-Exemplar 1Document2 pagesPersonal Philosophy of Education-Exemplar 1api-247024656No ratings yet
- Digital Sytems Counters and Registers: Dce DceDocument17 pagesDigital Sytems Counters and Registers: Dce DcePhan Gia AnhNo ratings yet
- LittorinidaeDocument358 pagesLittorinidaeSyarif Prasetyo AdyutaNo ratings yet
- ImpetigoDocument16 pagesImpetigokikimasyhurNo ratings yet
- August Strindberg's ''A Dream Play'', inDocument11 pagesAugust Strindberg's ''A Dream Play'', inİlker NicholasNo ratings yet
- Master Books ListDocument32 pagesMaster Books ListfhaskellNo ratings yet
- Business Administration: Hints TipsDocument11 pagesBusiness Administration: Hints Tipsboca ratonNo ratings yet
- AdvacDocument13 pagesAdvacAmie Jane MirandaNo ratings yet
- Cognitive ApprenticeshipDocument5 pagesCognitive ApprenticeshipRandall RobertsNo ratings yet
- The Gower Handbook of Project Management: Part 1: ProjectsDocument2 pagesThe Gower Handbook of Project Management: Part 1: ProjectschineduNo ratings yet
- MPCDocument193 pagesMPCpbaculimaNo ratings yet
- Hero Cash Cash Lyrics - Google SearchDocument1 pageHero Cash Cash Lyrics - Google Searchalya mazeneeNo ratings yet
- Aff Col MA Part IIDocument90 pagesAff Col MA Part IIAkanksha DubeyNo ratings yet
- Ielts Reading Whale CultureDocument4 pagesIelts Reading Whale CultureTreesa VarugheseNo ratings yet
- CogAT 7 PlanningImplemGd v4.1 PDFDocument112 pagesCogAT 7 PlanningImplemGd v4.1 PDFBahrouniNo ratings yet
- Chapter 9 - PPT (New)Document43 pagesChapter 9 - PPT (New)Syarifah NourazlinNo ratings yet
- Sample Questions 2019Document21 pagesSample Questions 2019kimwell samson100% (1)
- Communication and Globalization Lesson 2Document13 pagesCommunication and Globalization Lesson 2Zetrick Orate0% (1)
- Unidad 12 (libro-PowerPoint)Document5 pagesUnidad 12 (libro-PowerPoint)Franklin Suarez.HNo ratings yet
- 800 Pharsal Verb Thong DungDocument34 pages800 Pharsal Verb Thong DungNguyễn Thu Huyền100% (2)
- PSYC1111 Ogden Psychology of Health and IllnessDocument108 pagesPSYC1111 Ogden Psychology of Health and IllnessAleNo ratings yet
- Michel Agier - Between War and CityDocument25 pagesMichel Agier - Between War and CityGonjack Imam100% (1)
- Physics Syllabus PDFDocument17 pagesPhysics Syllabus PDFCharles Ghati100% (1)