Professional Documents
Culture Documents
Fluid Resuscitation
Uploaded by
fbihansipOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fluid Resuscitation
Uploaded by
fbihansipCopyright:
Available Formats
[Downloaded free from http://www.ijaweb.org on Saturday, September 23, 2017, IP: 223.255.228.
83]
Review Article
Perioperative fluid management: From physiology to
improving clinical outcomes
Address for correspondence: Victoria A Bennett, Maurizio Cecconi
Dr.Victoria A Bennett, Department of Intensive Care Medicine, St Georges University Hospitals NHS Foundation Trust and St
St Georges University Georges University of London, London, UnitedKingdom
Hospitals NHS Foundation
Trust, Blackshaw Road.
London SW170QT, ABSTRACT
UnitedKingdom.
Email:v.bennett1@nhs.net
Perioperative fluid management is a key component in the care of the surgical patient. It is an
area that has seen significant changes and developments, however there remains a wide disparity
in practice between clinicians. Historically, patients received large volumes of intravenous fluids
perioperatively. The concept of goal directed therapy was then introduced, with the early studies
showing significant improvements in morbidity and mortality. The current focus is on fluid therapy
guided by an individual patients physiology. Afluid challenge is commonly performed as part of
an assessment of a patients fluid responsiveness. There remains wide variation in how clinicians
perform a fluid challenge and this review explores the evidence for how to administer an effective
challenge that is both reliable and reproducible. The methods for monitoring cardiac output have
Access this article online evolved from the pulmonary artery catheter to a range of less invasive techniques. The different
Website: www.ijaweb.org options that are available for perioperative use are considered. Fluid status can also be assessed
by examining the microcirculation and the importance of recognising the possibility of a lack of
DOI: 10.4103/ija.IJA_456_17
coherence between the macro and microcirculation is discussed. Fluid therapy needs to be targeted
Quick response code
to specific end points and individualised. Not all patients who respond to a fluid challenge will
necessarily require additional fluid administration and care should be aimed at identifying those
who do. This review aims to explain the underlying physiology and describe the evidence base
and the changes that have been seen in the approach to perioperative fluid therapy.
Key words: Cardiac output, fluid, perioperative, physiology
INTRODUCTION fluid therapy administrated has been studied and a
Ushaped curve described, with increased mortality
Worldwide, there are over312 million surgical associated with very high or very low volumes of fluid
procedures performed annually.[1] While many of these administration.[5]
patients fall into a lowrisk group, it has been previously
estimated that up to 10% of patients can be classified Perioperative fluid management has been a focus for
as a high surgical risk. Those patients in the highrisk both anaesthetic and critical care research for a number
group account for 80% of postoperative mortality.[2] of years. With an evolving and changing evidence base,
The European Surgical Outcome Study demonstrated there have been significant developments in clinical
a 4% postoperative, in hospital mortality. Patients practice. Changes have been seen in all domains, from
fluid choice, to volume of administration, to which end
who develop postoperative complications have
both increased morbidity and mortality.[3] Khuri
This is an open access article distributed under the terms of the Creative
et al. demonstrated that patients who developed any Commons AttributionNonCommercialShareAlike 3.0 License, which allows
postoperative complication, in the first 30days after others to remix, tweak, and build upon the work noncommercially, as long as the
author is credited and the new creations are licensed under the identical terms.
surgery had a 30day mortality of 13.3%, compared to
For reprints contact: reprints@medknow.com
0.8% in those without postoperative complications.
This effect persisted when comparing 1 and 5year How to cite this article: Bennett VA, Cecconi M. Perioperative fluid
mortality between the two groups.[4] The association management: From physiology to improving clinical outcomes. Indian
between perioperative morbidity and volume of J Anaesth 2017;61:614-21.
614 2017 Indian Journal of Anaesthesia | Published by Wolters Kluwer - Medknow
Page no. 12
[Downloaded free from http://www.ijaweb.org on Saturday, September 23, 2017, IP: 223.255.228.83]
Bennett and Cecconi: Perioperative fluid management
points to target. Historically, there was a trend for high larger molecules including proteins and an alteration
volume or liberal fluid therapy, this shifted towards a in intra and extravascular oncotic pressure, with a
focus on restrictive fluid therapy. Adifferent way to subsequent movement of water extravascularly.[8]
look at this is by looking at goal directed fluid therapy
rather than focusing on liberal or restrictive approaches. The volume of fluid administered and fluid choice is
As an ever increasing evidence base demonstrates thought to alter the movement of fluid between the body
that perioperative fluid management alters patient compartments. Historically, colloids were frequently
outcomes, there is an increasing awareness of the used; it was believed that as colloids were more likely
need to individualise and target fluid administration to remain intravascularly than crystalloids, and greater
to the specific patient. However, fluid therapy remains haemodynamic stability could be achieved with lower
a particularly contentious area of perioperative volumes. Several large studies have however refuted
medicine.[6] The consequences of hypovolaemia, this. With consistent evidence of increased acute
with haemodynamic compromise, impaired oxygen kidney injury, need for renal replacement therapy
delivery and subsequent organ dysfunction are well and 90day mortality in patients receiving colloids,
recognised. Conversely, fluid overload has resultant particularly starches, compared to patients receiving
multisystemic effects, including interstitial oedema crystalloids, crystalloids now form the mainstay of
with implications on gas exchange, renal function and treatment.[9] A number of the studies on the use of
the gastrointestinal system.[7] So how do we optimally colloids have been performed in critically ill patients.
maintain patients fluid balance? However, a recent metaanalysis included surgical
patients and reported similar results.[10] Given these
This review aims to analyse the existing evidence and findings, the safety profile of starches for perioperative
physiological principles guiding fluid management use has been questioned, and it is the opinion of
strategies. Literature searches were performed using the authors that their use should be avoided, with
PubMed, including the terms perioperative, surgery, crystalloids forming the mainstay of treatment.
fluid therapy, goal directed therapy(GDT), cardiac
output and microcirculation to ensure relevant Which crystalloid to use has also been investigated,
articles were included. Snowballing of references was generally either 0.9% saline or a balanced solution
used, as well as the authors existing knowledge of the such as Hartmanns is used. 0.9% saline has a chloride
publications in the field. concentration of 154 mmol which is significantly
higher than serum chloride. It is well recognised
FLUID CHOICE that its use can lead to a hyperchloremic acidosis.
Postoperative hyperchloremia has been linked with
In health, water constitutes approximately 60% of the increased postoperative complications, such as acute
total body weight. This is divided between intra and kidney injury and increased 30day mortality, although
extracellular compartments. The extracellular volume causation has not been proved.[11] Balanced solutions,
can be further divided into interstitial, intravascular which include Hartmanns solution or Plasmalyte, are
and transcellular compartments. Movement between considered more physiological and generally preferred
compartments is limited by membranes. The vascular for perioperative fluid management.[12]
endothelium forms the barrier between the intravascular
and interstitial spaces, with the endothelial glycocalyx LIBERAL VERSUS RESTRICTIVE STRATEGIES
present on the vascular side and the cleft between
endothelial cells closed by tight junctions. In health water Estimating perioperative fluid losses can be challenging.
and electrolytes can diffuse across the endothelium and The period of fasting preoperatively, intraoperative
move freely down their respective pressure gradients surgical time, surgical losses and insensible losses
but the movement of larger molecules such as protein all need to be considered. Replacement based on
is limited by the glycocalyx, and they require an active these estimated values alone incorporates significant
transport system. Perioperatively, fluid homeostasis assumptions. In healthy volunteers, a period of
can be altered by several mechanisms. Systemic preoperative fasting was shown to have no effect on
vasodilatation decreases intracapillary pressure, markers of preload. The value in replacing this volume
altering the pressure gradient and therefore fluid shifts. has therefore been questioned.[13] Similarly, evidence
Disruption to the glycocalyx is reported in a variety of for insensible losses, or third space losses, requiring
disease states, leading to extravascular movement of liberal replacement, is inconsistent.[14]
Indian Journal of Anaesthesia|Volume61|Issue 8|August 2017 615
Page no. 13
[Downloaded free from http://www.ijaweb.org on Saturday, September 23, 2017, IP: 223.255.228.83]
Bennett and Cecconi: Perioperative fluid management
The use of basic haemodynamic variables, for example part of GDT, may have a heart rate and blood pressure
changes from baseline heart rate and blood pressure, within the normal range. The fluid is given with the
leads to reactive rather than proactive management, as it aim of increasing preload and therefore stroke volume
is well acknowledged that 20% of the circulating volume and cardiac output to potentially supranormal targets.
must be lost before any change in these parameters GDT is conducted for a set time period postoperatively.
is seen. These are also variables with multifactorial This is in contrast to patients presenting with sepsis,
influences, and a change may not indicate a change in where the time course may not initially be predictable
fluid status. Both general anaesthesia and neuroaxial and fluids and vasopressors may be required to ensure
anaesthesia can cause perioperative hypotension, adequate end organ perfusion.
which is not necessarily indicative of intravascular
fluid depletion, but decreased vascular tone. There can, While the initial concepts developed by Shoemaker
however, be a tendency to manage this with aggressive have been questioned and actually shown to be
fluid therapy.[14] Conversely, fluid overload may not harmful in some settings,[19] GDT evolved mainly
manifest until adverse end organ effects are seen.[7] focusing on stroke volume optimisation with less
invasive cardiac output monitors.[15] GDT carried
The definition of what constitutes a liberal versus on being studied in different settings, with multiple
a restrictive fluid strategy varies but can be in the studies showing significant decreases in morbidity
region of>5L for a liberal strategy, and<3L for a and mortality, particularly in higher risk patient
conservative strategy.[7] Studies comparing these two groups.[17,2022] Of interest, the improved outcomes
groups have shown differing results, but the trend persisted in longterm followup.[17,20,23] Arulkumaran
is towards increased morbidity and mortality in the et al. performed a metaanalysis which showed that
liberal fluid groups, particularly those undergoing highrisk surgical patients managed with GDT were not
high risk or major surgery.[14] A positive fluid balance at increased risk of treatment related cardiovascular
has been shown to be associated with increased complications. It had been hypothesised that
mortality.[15] However, as one strategy did not appear increased fluid and inotrope use, may predispose
to fit all patient groups, some of these earlier studies to increased complications but in fact, early GDT
commented on a need for individualised GDT.[16] therapy was shown to be associated with decreased
cardiovascular events.[24] More recent studies have
GOAL DIRECTED THERAPY failed to show the same results, the reasons for this
are likely multifactorial.[25] The largest study on GDT
GDT aims to meet the patients increased oxygen to date, OPTIMISE, a multicentre, randomised study
demand incurred in the perioperative period, by targeted in patients undergoing major abdominal surgery,
intervention, guided by haemodynamic monitoring.[17] showed no difference in mortality or postoperative
Increased perioperative oxygen delivery, with reduced complications at 30days.[26] Similarly, POEMAS,
oxygen debt in survivors compared to nonsurvivors was a multicentre, randomised study, conducted in
first observed by Shoemaker etal. in the 1980s. Shoemaker patients undergoing major abdominal surgery
et al. thus hypothesised that targeting supranormal showed no difference in outcomes between the two
physiological parameters in the perioperative setting groups.[27] Clinical practice has changed significantly
would therefore decrease morbidity and mortality. They over the years, particularly with the development
described targets of a cardiac output>4.5L/min/m2, and and increased practice of enhanced recovery after
an oxygen delivery >600ml/min/m2.[18] The management surgery programmes which advocate perioperative
of perioperative fluid administration is a different haemodynamic monitoring. As significant advances
entity to fluid management in the setting of a patient have been incorporated into standard care, it is likely
presenting acutely unwell, for example with sepsis. that the overall quality of care routinely provided has
This difference is explained by the different processes improved. It can therefore become more challenging
occurring at the cellular level in the two conditions to conduct a study that identifies a single intervention
and the different reasons and goals of fluid therapy. that will statistically alter patient outcome.
Perioperative GDT describes fluid administration, with
the aim of optimising a patients cardiac function and ADVANCED ASSESSMENT OF FLUID STATUS
ultimately oxygen delivery. It is used for a time limited
period, both during and after a surgical intervention. In addition to a thorough clinical examination,
Many of the patients given fluids postoperatively, as echocardiography is an increasingly useful bedside
616 Indian Journal of Anaesthesia|Volume61|Issue 8|August 2017
Page no. 14
[Downloaded free from http://www.ijaweb.org on Saturday, September 23, 2017, IP: 223.255.228.83]
Bennett and Cecconi: Perioperative fluid management
tool for the assessment of a patients fluid status. It PiCCO(Pulsion medical systems, Munich, Germany),
is becoming readily available, in intensive care, and LiDCOplus(LiDCO, Cambridge, UK), LiDCOrapid
is moving towards being as common place at the (LiDCO, Cambridge, UK), VolumeView/EV1000
bedside as a stethoscope. Echocardiography can be (Edwards Lifesciences, Irvine CA, USA) and FloTrac
used to assess preload, contractility and afterload (Edwards LifeSciences, Irvine CA, USA). All of these
and changes in these parameters in response to a devices, except the FloTrac require calibration.[27,29]
fluid challenge observed. Although interpretability is
dependent on the individual clinicians skill, it is an Bioimpedance systems apply a highfrequency
increasingly practiced skill. Continuous monitoring is electrical current, of known amplitude and frequency,
required to provide ongoing assessment of a patients across the thorax and measure changes in voltage.
fluid status and as such echocardiography is often The ratio between voltage and current amplitudes
coupled with cardiac output monitors to provide provides a measure of transthoracic direct current
further information. Due to practical constraints it is resistance or impedance. This varies in proportion
more likely to be utilised in the postoperative phase to intrathoracic fluid volume. This is a noninvasive
rather than during surgery. technique, however studies have shown poor
correlation between bioimpedance measurements and
CARDIAC OUTPUT MONITORS cardiac output measurements made using invasive
techniques and it has been deemed to be inaccurate
Significant developments have been made in methods in the intensive care population.[30] Systems using
of assessing cardiac output and oxygen delivery. bioreactance to assess cardiac output and stroke
Historically, this required a pulmonary artery catheter volume variation have been developed. These are also
(PAC), but less invasive methods are now available noninvasive, however, in contrast to bioimpedance
and readily used, including Oesophageal Doppler and systems, they show promising early results in the
pulse contour analysis. assessment of patient fluid responsiveness. Waldron
etal. showed the NICOM, noninvasive cardiac output
A PAC is still considered the gold standard method, monitor(Cheetah Medical, Berkshire, UK) performed
however it is now used less in clinical practice. similarly to the Oesophageal Doppler in guiding
The catheter is inserted via a central vein, typically perioperative fluid therapy in elective colorectal
the internal jugular vein and a thermodilution surgery patients.[31]
technique used to directly measure central venous,
right atrial, right ventricular, pulmonary arterial and Use of these techniques assists assessment of a
pulmonary artery wedge pressures.[27] Some PACs patients cardiac output and intravascular volume
have an automated semicontinuous cardiac output status. This often involves assessment of whether a
monitoring feature. However, as the cardiac output patients preload can be augmented to increase stroke
measurements are updated over a period of minutes, volume with fluid administration. Perioperative fluid
it is difficult to use as a method of assessing response therapy can be guided by whether a patient is fluid
to a fluid challenge where a faster data acquisition is responsive or not.
necessary.[28]
FLUID EXPANSION, FLUID RESPONSIVENESS AND
The Oesophageal Doppler is placed at the mid thoracic ITS PREDICTION
level in the oesophagus and measures the velocity of
flow in the descending aorta which is used to calculate Venous return is equal to cardiac output. The
cardiac output and change in stroke volume. FrankStarlin mechanism describes the process by
which the heart is able to accommodate and then
Currently, the most commonly used method of eject all blood returned to it, despite variations
cardiac output measurement in intensive care uses in venous return. An increased venous return, or
pulse contour analysis to indirectly calculate cardiac increased preload increases ventricular filling and the
output. This requires an arterial catheter, classically enddiastolic volume. This increases stretch of the
placed in either the radial or femoral artery and cardiac myocyte, which increases sarcomere length
uses computerbased algorithms to calculate stroke with resultant increased force of contraction leading to
volume from pulse pressure and compliance. There an increase in volume of blood ejected from the heart.[32]
are five main commercially available devices; the In order for a fluid challenge to be effective it therefore
Indian Journal of Anaesthesia|Volume61|Issue 8|August 2017 617
Page no. 15
[Downloaded free from http://www.ijaweb.org on Saturday, September 23, 2017, IP: 223.255.228.83]
Bennett and Cecconi: Perioperative fluid management
needs to be of sufficient volume to cause stretch of the similarly, however in the nonresponders CVP also
cardiac myocytes and test the FrankStarling principle. increased. This means the pressure gradient, which
If the heart is able to accommodate the increased as explained is the driving pressure for venous return,
volume then stroke volume will increase, otherwise only increased in the responders.[36]
the volume will remain within the venous system.[29]
Assessing fluid responsiveness is important every
The total blood volume can theoretically be divided time fluids are given. If possible the response to fluids
into the unstressed and stressed volumes. The should be predicted before their administration. The
unstressed volume is the volume that fills the blood prediction of a patients fluid responsiveness aims
vessels, without causing a rise in pressure. The to identify those who may benefit from an increase
stressed volume is any additional volume, which will in intravenous volume with an increase in stroke
cause both a pressure rise and elastic distension of the volume and cardiac output. Figure2, uses the Frank
vessel wall. When a fluid challenge is given, the aim is Starling Curve to demonstrate whether an increase
to expand the stressed volume. The elastic properties, in preload will result in an increased stroke volume.
or compliance of the vessel, determine the resultant Predictors of fluid responsiveness include high pulse
degree of distension in response to the fluid challenge. pressure variation, stroke volume variation, vena cava
In the cardiovascular system, the pressure related to collapsibility index, dynamic passive leg raising test
the stressed volume and vascular compliance is the and end occlusion expiratory test.[14] These assess beat
mean systemic filling pressure(Pmsf).[33] Pmsf will to beat variations in either pulse pressure or stroke
increase in response to an increase in intravascular volume, however, are only validated in ventilated
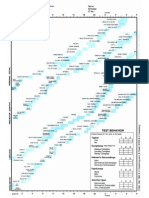
stressed volume, as demonstrated in Figure1. The patients with tidal volumes of more than 8ml/kg and
greater the vascular compliance, the smaller the rise no arrhythmias. Myatra et al. recently demonstrated
in Pmsf in response to a fluid challenge. Pmsf was first that in patients ventilated with a low tidal volume
described in 1894 by Bayliss and Starling using a dog strategy, fluid responsiveness can be predicted by
model. It is defined as the pressure in the vascular transiently incrementing the tidal volume from 6 to
system when the heart is stopped and there is no blood 8ml/kg and recording changes in either pulse pressure
flow, conditions which only occur in cardiac arrest.[34] variation or stroke volume variation.[37]
The determinants of venous return are Pmsf, right When the decision to administer fluids has been made,
atrial pressure and resistance to venous return, as the best way to do it is with a fluid challenge. Afluid
first defined by Guyton.[35] The driving pressure challenge can be used to assess for fluid responsiveness
for venous return is the pressure gradient between without the limitations associated with pulse pressure
Pmsf and central venous pressure(CVP), which then variation or stroke volume variation and it can be
determines cardiac output.[33] Cecconi etal. measured both diagnostic and therapeutic. The aim of using a
a Pmsf analogue(Pmsa) and CVP in response to an small volume of fluid is to reduce the risk associated
effective fluid challenge. They showed that in both with fluid overload if additional resuscitation is not
responders and nonresponders Pmsa increased required.[30] However, if the volume of fluid given is
not adequate to stress the system then the response
of patients who could be fluid responsive may be
misinterpreted. Apatient is deemed fluid responsive
if stroke volume or cardiac output increase by at least
10% following a fluid challenge. Previous work has
shown that only 50% of patients admitted to intensive
care respond to fluid loading.[38]
FLUID CHALLENGE
The assessment of fluid responsiveness relies
on the administration of a fluid challenge, however
the method of administration of a fluid challenge
Figure1: Blood volume can be divided into stressed and unstressed
volumes. Following an effective fluid challenge the stressed volume shows significant interuser variability. At present,
increases, with a subsequent rise in mean systemic filling pressure the type of fluid, the volume of fluid and the rate at
618 Indian Journal of Anaesthesia|Volume61|Issue 8|August 2017
Page no. 16
[Downloaded free from http://www.ijaweb.org on Saturday, September 23, 2017, IP: 223.255.228.83]
Bennett and Cecconi: Perioperative fluid management
Figure2: FrankStarling curve. Afluid challenge at Point A would increase preload and mean systemic filling pressure, with a subsequent increase
in stroke volume, as demonstrated by Point B. This patient would therefore be fluid responsive. At Point C, the same fluid challenge would again
increase preload and mean systemic filling pressure, but there is no significant increase in stroke volume, as shown by Point D. At Point E, an
inadequate fluid challenge is given, too small a volume is given to significantly increase preload and mean systemic filling pressure, therefore,
no increase in stroke volume is seen and this patient would incorrectly be labelled as a nonresponder
which the fluid is administered can vary. One large, Whilst work aims to identify those who respond to
multicentre, observational study showed a wide intravenous fluids, it is important to realise that not
disparity in practice. Crystalloids accounted for 74.3% all who respond will necessarily require the additional
of fluids used for the challenge, of these 45.9% were volume. In a study of healthy volunteers, they were
0.9% saline and 53.5% balanced solutions including shown to demonstrate a significant increase in stroke
Hartmanns solution, a range of colloids accounted volume following a head down tilt. However, it is likely
for the remaining 25.6%. The median amount of that these healthy volunteers do not necessarily require
fluid given as a challenge was 500ml, interquartile an increased intravascular volume.[29] It is important
range 5001000ml, median time of administration that the assessment of fluid responsiveness is used as
24min and median rate of administration 1000ml/h, part of a complete assessment of a patients clinical
interquartile range 5001333ml/h.[39] condition and fluid status to determine whether they
need or it is appropriate for them to receive further
Different authors have reported differing changes in intravenous fluids.
Pmsf in response to a fluid challenge. This may reflect
the different techniques used to administer the fluid MACRO AND MICROCIRCULATION COHERENCE
challenge. If the fluid challenge is to be effective in
testing fluid responsiveness then it needs to increase The focus in fluid management has historically been
Pmsf. Otherwise a patient may be incorrectly labelled on the macrocirculation, with an assumption there
as a nonresponder, when in fact the volume given will be haemodynamic coherence or that correction
may have just filled the unstressed volume. Aya etal. of the haemodynamics at the macrocirculatory level
have studied fluid challenge volumes of 1, 2, 3 and will translate to normalisation of perfusion and
4ml/kg in postsurgical patients, and shown that a oxygen delivery in the microcirculation.[41] However,
fluid challenge of 4ml/kg is the option which most several studies have shown that coherence does not
reliably stresses the cardiac system, to differentiate persist in states of illness. Jhanji etal. perioperatively
responders from nonresponders.[40] studied the microcirculation and macrocirculation
Indian Journal of Anaesthesia|Volume61|Issue 8|August 2017 619
Page no. 17
[Downloaded free from http://www.ijaweb.org on Saturday, September 23, 2017, IP: 223.255.228.83]
Bennett and Cecconi: Perioperative fluid management
in patients undergoing gastrointestinal surgery. They given it should be an effective challenge of the patients
observed that there were no significant differences physiology. Fluid responsiveness should be assessed
in the systemic haemodynamic variables between with an effective fluid challenge that increases Pmsf
patients who did and did not develop postoperative and the response or possible change in cardiac output
complications. However, at the microcirculation level, monitored. Of those that do respond, not all of these
both the proportion and density of perfused small patients will still require ongoing fluid resuscitation
vessels and the microvascular flow index were reduced and there may be a role for bedside microcirculatory
both pre and postoperatively in those patients who assessment, to guide this in the future.
developed postoperative complications.[42]
Financial support and sponsorship
It has been shown a low microcirculatory flow, Nil.
independent of systemic haemodynamics, predicts
the response to a fluid challenge. Surrogate markers of Conflicts of interest
microcirculation such as lactate or skin temperature Dr. Cecconi is a Consultant and Speaker for Edwards
correlate poorly with direct visualisation of flow. Lifesciences, Cheetah, LidCO, Masimo, and is on the
The microcirculation can be examined at the bedside Medical Advisory Board of Directed Systems.
using a hand held microcirculation camera. At
REFERENCES
present, three generations of this technology have
been developed. Patients with macrocirculatory 1. WeiserTG, HaynesAB, MolinaG, LipsitzSR, EsquivelMM,
markers of hypoperfusion may have either low or UribeLeitzT, etal. Estimate of the global volume of surgery in
2012: An assessment supporting improved health outcomes.
normal microcirculatory flow. Pranskunas et al.
Lancet 2015;385Suppl2:S11.
demonstrated that a fluid challenge only resulted in 2. PearseRM, HarrisonDA, JamesP, WatsonD, HindsC,
improvement in clinical markers of hypoperfusion RhodesA, etal. Identification and characterisation of the
highrisk surgical population in the UnitedKingdom. Crit Care
in those with an initial low microcirculatory flow, 2006;10:R81.
which increased or normalised in response to a 3. PearseRM, MorenoRP, BauerP, PelosiP, MetnitzP, SpiesC,
fluid challenge. Of those with an initial normal etal. Mortality after surgery in Europe: A 7day cohort study.
Lancet 2012;380:105965.
microcirculation no improvement in macrocirculatory 4. KhuriSF, HendersonWG, DePalmaRG, MoscaC, HealeyNA,
markers of hypoperfusion was seen following a fluid Kumbhani DJ; Participants in the VA National Surgical Quality
challenge. The study participants change in stroke Improvement Program. Determinants of longterm survival
after major surgery and the adverse effect of postoperative
volume in response to fluid administration was complications. Ann Surg 2005;242:32641.
independent of the microcirculatory changes seen. 5. BellamyMC. Wet, dry or something else? Br J Anaesth
In studies guiding fluid therapy based on parameters 2006;97:7557.
6. CannessonM, GanTJ. Pro: Perioperative goal directed
within the microcirculation, significantly lower therapy is an essential part of an enhanced recovery protocol.
volumes of fluid were administered overall, with the Int Anaesth Res Soc 2016;122:125860.
7. VoldbyAW, BrandstrupB. Fluid therapy in the perioperative
same macrocirculatory outcomes.[42,43] This may be
settingA clinical review. JIntensive Care 2016;4:27.
beneficial given the previously discussed increased 8. EdwardsMR, MythenMG. Fluid therapy in critical illness.
mortality associated with a positive fluid balance.[15] Extrem Physiol Med 2014;3:16.
9. Serpa NetoA, VeeloDP, PeireiraVG, de Assuno MS,
ManettaJA, Espsito DC, etal. Fluid resuscitation with
The choice of fluid has been shown to alter hydroxyethyl starches in patients with sepsis is associated with
coherence. 0.9% saline has been shown to be the least an increased incidence of acute kidney injury and use of renal
effective of the commonly used fluids in improving replacement therapy: A systematic review and metaanalysis
of the literature. JCrit Care 2014;29:185.e17.
microcirculatory flow and promoting haemodynamic 10. PerelP, RobertsI, KerK. Colloids versus crystalloids for fluid
coherence. It has been hypothesised that a focus on resuscitation in critically ill patients. Cochrane Database Syst
Rev 2013;(CD000567).
microcirculation guided fluids may improve outcomes,
11. McCluskeySA, KarkoutiK, WijeysunderaD, MinkovichL,
but this remains to be proved in large studies.[41] TaitG, BeattieWS. Hyperchloremia after noncardiac surgery
is independently associated with increased morbidity and
SUMMARY mortality: A propensitymatched cohort study. Anesth Analg
2013;117:41221.
12. SweeneyRM, McKendryRA, BediA. Perioperative intravenous
In summary, fluid therapy remains a contentious area fluid therapy for adults. Ulster Med J 2013;82:1718.
of perioperative medicine, with differing approaches 13. AlvesDR, RibeirasR. Does fasting influence preload
responsiveness in ASA 1 and 2 volunteers? Braz J Anesthesiol
seen. It is vital that patients receive fluids targeted to 2017;67:1729.
their individual physiology. When a fluid challenge is 14. AditianingsihD, GeorgeYW. Guiding principles of fluid
620 Indian Journal of Anaesthesia|Volume61|Issue 8|August 2017
Page no. 18
[Downloaded free from http://www.ijaweb.org on Saturday, September 23, 2017, IP: 223.255.228.83]
Bennett and Cecconi: Perioperative fluid management
and volume therapy. Best Pract Res Clin Anaesthesiol using noninvasive cardiac output monitoring in major
2014;28:24960. abdominal surgery: A prospective, randomized, multicenter,
15. VaaraST, KorhonenAM, KaukonenKM, NisulaS, InkinenO, pragmatic trial: POEMAS Study(PeriOperative goaldirected
HoppuS, etal. Fluid overload is associated with an increased thErapy in Major Abdominal Surgery). Anesth Analg
risk for 90day mortality in critically ill patients with renal 2014;119:57987.
replacement therapy: Data from the prospective FINNAKI 28. CoveME, PinskyMR. Perioperative hemodynamic monitoring.
study. Crit Care 2012;16:R197. Best Pract Res Clin Anaesthesiol 2012;26:45362.
16. HolteK, FossNB, AndersenJ, ValentinerL, LundC, BieP, etal. 29. CecconiM, ParsonsAK, RhodesA. What is a fluid challenge?
Liberal or restrictive fluid administration in fasttrack colonic Curr Opin Crit Care 2011;17:2905.
surgery: A randomized, doubleblind study. Br J Anaesth 30. MarikPE. Noninvasive cardiac output monitors: A stateof
2007;99:5008. theart review. JCardiothorac Vasc Anesth 2013;27:12134.
17. CecconiM, CorredorC, ArulkumaranN, AbuellaG, BallJ, 31. WaldronNH, MillerTE, ThackerJK, ManchesterAK,
GroundsRM, etal. Clinical review: Goaldirected therapywhat WhiteWD, NardielloJ, etal. A prospective comparison of
is the evidence in surgical patients? The effect on different risk a noninvasive cardiac output monitor versus esophageal
groups. Crit Care 2013;17:209. Doppler monitor for goaldirected fluid therapy in colorectal
18. ShoemakerWC, AppelPL, KramHB, WaxmanK, LeeTS. surgery patients. Anesth Analg 2014;118:96675.
Prospective trial of supranormal values of survivors as 32. PattersonSW, PiperH, StarlingEH. The regulation of the heart
therapeutic goals in highrisk surgical patients. Chest beat. JPhysiol 1914;48:465513.
1988;94:117686. 33. MaasJJ. Mean systemic filling pressure: Its measurement and
19. HayesMA, TimminsAC, YauEH, PalazzoM, HindsCJ, WatsonD. meaning. Neth J Crit Care 2015;19:611.
Elevation of systemic oxygen delivery in the treatment of 34. BaylissWM, StarlingEH. Observations on venous pressures
critically ill patients. NEngl J Med 1994;330:171722. and their relationship to capillary pressures. JPhysiol
20. HamiltonMA, CecconiM, RhodesA. Asystematic review 1894;16:159318.
and metaanalysis on the use of preemptive hemodynamic 35. GuytonAC. Determination of cardiac output by equating
intervention to improve postoperative outcomes in venous return curves with cardiac response curves. Physiol
moderate and highrisk surgical patients. Anesth Analg Rev 1955;35:1239.
2011;112:1392402. 36. CecconiM, AyaHD, GeisenM, EbmC, FletcherN, GroundsRM,
21. PearseR, DawsonD, FawcettJ, RhodesA, GroundsRM, etal. Changes in the mean systemic filling pressure during
BennettED. Early goaldirected therapy after major surgery a fluid challenge in postsurgical intensive care patients.
reduces complications and duration of hospital stay. Intensive Care Med 2013;39:1299305.
Arandomised, controlled trial[ISRCTN38797445]. Crit Care 37. MyatraSN, PrabuNR, DivatiaJV, MonnetX, KulkarniAP,
2005;9:R68793. TeboulJL. The changes in pulse pressure variation or stroke
22. LoboSM, RonchiLS, OliveiraNE, Brando PG, FroesA, volume variation after a tidal volume challenge reliably
CunrathGS, etal. Restrictive strategy of intraoperative predict fluid responsiveness during low volume ventilation.
fluid maintenance during optimization of oxygen delivery Crit Care Med 2017;45:41521.
decreases major complications after highrisk surgery. Crit 38. MichardF, TeboulJL. Predicting fluid responsiveness in
Care 2011;15:R226. ICU patients: A critical analysis of the evidence. Chest
23. RhodesA, CecconiM, HamiltonM, PolonieckiJ, WoodsJ, 2002;121:20008.
BoydO, etal. Goaldirected therapy in highrisk surgical 39. CecconiM, HoferC, TeboulJL, PettilaV, WilkmanE, MolnarZ,
patients: A 15year followup study. Intensive Care Med etal. Fluid challenges in intensive care: The FENICE
2010;36:132732. study: Aglobal inception cohort study. Intensive Care Med
24. ArulkumaranN, CorredorC, HamiltonMA, BallJ, GroundsRM, 2015;41:152937.
RhodesA, etal. Cardiac complications associated with 40. AyaHD, RhodesA, Chis SterI, FletcherN, GroundsRM,
goaldirected therapy in highrisk surgical patients: A CecconiM. Hemodynamic effect of different doses of fluids for
metaanalysis. Br J Anaesth 2014;112:64859. a fluid challenge: Aquasirandomized controlled study. Crit
25. ChallandC, StruthersR, SneydJR, ErasmusPD, MellorN, Care Med 2017;45:e1618.
HosieKB, etal. Randomized controlled trial of intraoperative 41. InceC. Hemodynamic coherence and the rationale for
goaldirected fluid therapy in aerobically fit and unfit patients monitoring the microcirculation. Crit Care 2015;19Suppl3:S8.
having major colorectal surgery. Br J Anaesth 2012;108:5362. 42. JhanjiS, VivianSmithA, LucenaAmaroS, WatsonD,
26. PearseRM, HarrisonDA, MacDonaldN, GilliesMA, HindsCJ, PearseRM. Haemodynamic optimisation improves
BluntM, AcklandG, etal. Effect of a perioperative, cardiac tissue microvascular flow and oxygenation after major surgery:
outputguided hemodynamic therapy algorithm on outcomes A randomised controlled trial. Crit Care 2010;14:R151.
following major gastrointestinal surgery: A randomized 43. PranskunasA, KoopmansM, KoetsierPM, PilvinisV,
clinical trial and systematic review. JAMA 2014;311:218190. BoermaEC. Microcirculatory blood flow as a tool to select
27. Pestaa D, EspinosaE, EdenA, Njera D, CollarL, AldecoaC, ICU patients eligible for fluid therapy. Intensive Care Med
etal. Perioperative goaldirected hemodynamic optimization 2013;39:6129.
Indian Journal of Anaesthesia|Volume61|Issue 8|August 2017 621
Page no. 19
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- MetalCut User ManualDocument71 pagesMetalCut User Manualnammaris0% (1)
- The Facility Manager's HandbookDocument362 pagesThe Facility Manager's HandbookLuân Châu100% (14)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Architecture After Modernism - Diane GhirardoDocument10 pagesArchitecture After Modernism - Diane GhirardoCebo DharuNo ratings yet
- Consumer Behaviour of Titan WatchesDocument57 pagesConsumer Behaviour of Titan Watchesmanu100% (1)
- 2017 PanduanPraktikKlinisDocument37 pages2017 PanduanPraktikKlinisYanita DikaningrumNo ratings yet
- Tes Buta Warna 24 Plate.Document33 pagesTes Buta Warna 24 Plate.Agung Tri UtomoNo ratings yet
- 2017 PanduanPraktikKlinisDocument37 pages2017 PanduanPraktikKlinisYanita DikaningrumNo ratings yet
- Method Statement For Planter WaterproofingDocument8 pagesMethod Statement For Planter WaterproofingMonali Varpe0% (1)
- Acog Committee Opinion: Cesarean Delivery On Maternal RequestDocument5 pagesAcog Committee Opinion: Cesarean Delivery On Maternal RequestfbihansipNo ratings yet
- PMK No. 57 Tahun 2013 Tentang PTRMDocument9 pagesPMK No. 57 Tahun 2013 Tentang PTRMfbihansipNo ratings yet
- Modelling Survival Prediction in Medical DataDocument13 pagesModelling Survival Prediction in Medical DatafbihansipNo ratings yet
- SkizofreniaDocument26 pagesSkizofreniafbihansipNo ratings yet
- Proton Pump Inhibitors vs. Histamine - Receptor Antagonists For Stress Ulcer ProphylaxisDocument19 pagesProton Pump Inhibitors vs. Histamine - Receptor Antagonists For Stress Ulcer ProphylaxisfbihansipNo ratings yet
- Hydronephrosis LWDocument8 pagesHydronephrosis LWfbihansipNo ratings yet
- HB CodDocument65 pagesHB CodranggadrNo ratings yet
- PPI - Isolation Precaution PDFDocument52 pagesPPI - Isolation Precaution PDFfbihansipNo ratings yet
- Formato Denver IIDocument1 pageFormato Denver IIMelly AnidaNo ratings yet
- P 114Document7 pagesP 114Sleepy WinterNo ratings yet
- National Code of Autopsy PracticeDocument22 pagesNational Code of Autopsy PracticefbihansipNo ratings yet
- ASA Physical Status Classification System PDFDocument6 pagesASA Physical Status Classification System PDFfbihansipNo ratings yet
- Daftar Nama Panitia Student Day 2018 Sie Pangus 1 I Dewa Gede Yoga Paramartha (KOOR) 1608511038 FmipaDocument19 pagesDaftar Nama Panitia Student Day 2018 Sie Pangus 1 I Dewa Gede Yoga Paramartha (KOOR) 1608511038 FmipafbihansipNo ratings yet
- List To DoDocument1 pageList To DofbihansipNo ratings yet
- Circulatory ShockDocument9 pagesCirculatory ShockTri UtomoNo ratings yet
- Fluids in Septic Shock: Crystalloid, Colloids, or Blood?: CrystalloidsDocument10 pagesFluids in Septic Shock: Crystalloid, Colloids, or Blood?: CrystalloidsfbihansipNo ratings yet
- Jadwal Belajar Persiapan KOASDocument3 pagesJadwal Belajar Persiapan KOASfbihansipNo ratings yet
- Choices in Fluid Type and Volume During Resuscitation Impact On Patient Outcomes PDFDocument13 pagesChoices in Fluid Type and Volume During Resuscitation Impact On Patient Outcomes PDFfbihansipNo ratings yet
- DystosiaDocument8 pagesDystosiaMuhammed GambarovNo ratings yet
- D-Dimer Plasma Levels in Ishemic StrokeDocument7 pagesD-Dimer Plasma Levels in Ishemic StrokefbihansipNo ratings yet
- HBA1c Stroke PatientDocument8 pagesHBA1c Stroke PatientfbihansipNo ratings yet
- Nihms 224791Document21 pagesNihms 224791fbihansipNo ratings yet
- Choices in Fluid Type and Volume During Resuscitation Impact On Patient Outcomes PDFDocument13 pagesChoices in Fluid Type and Volume During Resuscitation Impact On Patient Outcomes PDFfbihansipNo ratings yet
- Biomarkers To Enhance Accuracy and Precision of Prediciton of Short Term and Long Term Outcome ICHDocument6 pagesBiomarkers To Enhance Accuracy and Precision of Prediciton of Short Term and Long Term Outcome ICHfbihansipNo ratings yet
- Albumin Serum and Stroke OutcomeDocument6 pagesAlbumin Serum and Stroke OutcomefbihansipNo ratings yet
- Wind Hydro 2Document6 pagesWind Hydro 2Vani TiwariNo ratings yet
- Training Report PRASADDocument32 pagesTraining Report PRASADshekharazad_suman85% (13)
- Lesson Plan in ESPDocument4 pagesLesson Plan in ESPkaren daculaNo ratings yet
- NAFTA CertificateDocument2 pagesNAFTA Certificateapi-522706100% (4)
- To Quantitative Analysis: To Accompany by Render, Stair, Hanna and Hale Power Point Slides Created by Jeff HeylDocument94 pagesTo Quantitative Analysis: To Accompany by Render, Stair, Hanna and Hale Power Point Slides Created by Jeff HeylNino NatradzeNo ratings yet
- Bahasa Inggris RanggaDocument3 pagesBahasa Inggris RanggaArdiyantoNo ratings yet
- Q3 SolutionDocument5 pagesQ3 SolutionShaina0% (1)
- Annual Reading Plan - Designed by Pavan BhattadDocument12 pagesAnnual Reading Plan - Designed by Pavan BhattadFarhan PatelNo ratings yet
- Organic Vapour List PDFDocument1 pageOrganic Vapour List PDFDrGurkirpal Singh MarwahNo ratings yet
- Since 1977 Bonds Payable SolutionsDocument3 pagesSince 1977 Bonds Payable SolutionsNah HamzaNo ratings yet
- Dreamers Chords by Jungkook (정국) tabs at Ultimate Guitar ArchiveDocument4 pagesDreamers Chords by Jungkook (정국) tabs at Ultimate Guitar ArchiveLauraNo ratings yet
- ASTM D5895 - 2020 Tiempo SecadoDocument4 pagesASTM D5895 - 2020 Tiempo SecadoPablo OrtegaNo ratings yet
- Dental Pulp TissueDocument77 pagesDental Pulp TissueJyoti RahejaNo ratings yet
- Risus License Information PDFDocument1 pageRisus License Information PDFSam CorbenNo ratings yet
- Computer 8 Q2 Set B ModuleDocument6 pagesComputer 8 Q2 Set B ModuleEmvie Loyd Pagunsan-ItableNo ratings yet
- Automation & Artificial Intelligence: Robots and Their ApplicationsDocument93 pagesAutomation & Artificial Intelligence: Robots and Their ApplicationsManal AndhereNo ratings yet
- Vertical Transportation SystemDocument15 pagesVertical Transportation SystemAnupama MorankarNo ratings yet
- Wave Optics - I: Created by C. Mani, Principal, K V No.1, AFS, Jalahalli West, BangaloreDocument16 pagesWave Optics - I: Created by C. Mani, Principal, K V No.1, AFS, Jalahalli West, BangaloreNitesh Gupta100% (1)
- Business English 2, (ML, PI, U6, C3)Document2 pagesBusiness English 2, (ML, PI, U6, C3)Ben RhysNo ratings yet
- English 3 PDFDocument177 pagesEnglish 3 PDFÇèrela ĆlavəcillasNo ratings yet
- DOCS-#165539-v8-Technical Manual FOB4 TS Section 5 - MaintenanceDocument108 pagesDOCS-#165539-v8-Technical Manual FOB4 TS Section 5 - MaintenanceBME AOHNo ratings yet
- HE HOUSEKEEPING GR11 Q1 MODULE-6-for-teacherDocument25 pagesHE HOUSEKEEPING GR11 Q1 MODULE-6-for-teacherMikaela YtacNo ratings yet
- Cash Surrender Value: Valix, C. T. Et Al. Intermediate Accounting Volume 1. (2019) - Manila: GIC Enterprises & Co. IncDocument8 pagesCash Surrender Value: Valix, C. T. Et Al. Intermediate Accounting Volume 1. (2019) - Manila: GIC Enterprises & Co. IncJoris YapNo ratings yet