Professional Documents
Culture Documents
Meningeal Fibroma
Uploaded by
ifanda80Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Meningeal Fibroma
Uploaded by
ifanda80Copyright:
Available Formats
J Neurosurg Pediatrics 14:155159, 2014
AANS, 2014
Meningeal fibroma: a rare meningioma mimic
Report of 2 cases
Aanchal Kakkar, M.D.,1 Mehar C. Sharma, M.D.,1 Nishant Goyal, M.B.B.S., 2
Chitra Sarkar, M.D.,1 Vaishali Suri, M.D.,1 Ajay Garg, M.D., 3
Shashank S. Kale, M.Ch., 2 and Ashish Suri, M.Ch. 2
Departments of 1Pathology, 2Neurosurgery, and 3Neuroradiology, All India Institute of Medical Sciences, New
Delhi, India
Meningeal fibromas are rare intracranial tumors that mimic meningiomas radiologically as well as histologi-
cally. The authors report 2 cases of meningeal fibroma with detailed clinical, radiological, histopathological, and
immunohistochemical features, and discuss the differential diagnosis of this entity. Knowledge of this rare tumor
is essential for pathologists to be able distinguish it from more common meningeal tumors, especially in younger
patients. This knowledge is also essential for neurosurgeons, as incomplete resection may lead to tumor recurrence,
and such patients require close follow-up.
(http://thejns.org/doi/abs/10.3171/2014.5.PEDS13556)
Key Words fibroma meningeal tumor meningioma oncology
solitary fibrous tumor intracranial mesenchymal
F
ibrous proliferative lesions arising from meningeal tent headache and vomiting for 3 months. His parents had
mesenchymal tissue are extremely rare and include noted changes in his personality and behavior over this
fibromatosis, solitary fibrous tumor (SFT), inflam- period. On examination, there was no evidence of any
matory myofibroblastic tumor, fibroma, and cranial fasci- sensorimotor deficits or any stigmata of neurofibromato-
itis.1 The histological appearance of these lesions is simi- sis. Magnetic resonance imaging revealed a large, hetero-
lar to more common tumors such as meningiomas, and geneously enhancing mass lesion in the frontotemporo-
therefore they pose a challenge to the diagnostic skills of parietal region, suggestive of a meningioma (Fig. 1). The
the pathologist. We report 2 cases of meningeal fibroma, patient underwent a right frontoparietal craniotomy and
one in a 15-year-old boy and another in an 8-year-old boy, gross-total excision of the tumor. Intraoperatively, a gray-
both of which mimicked meningioma on radiological as ish-white, hard, extraaxial mass with minimal vascularity
well as on histological examination, causing a diagnostic was noted, attached to the falx. The tumor was excised
dilemma. completely, along with its falcine attachment (Simpson
Grade I excision) and was submitted for histopathological
evaluation. The patient remains recurrence-free 3 years
Case Reports after the surgery.
Case 1. A 15-year-old boy complained of intermit- Case 2. An 8-year-old boy presented with a history
of intermittent headache and abnormal behavior, includ-
Abbreviations used in this paper: EMA = epithelial membrane This article contains some figures that are displayed in color
antigen; GFAP = glial fibrillary acidic protein; SFT = solitary online but in black-and-white in the print edition.
fibrous tumor; SMA = smooth muscle actin.
J Neurosurg: Pediatrics / Volume 14 / August 2014 155
A. Kakkar et al.
Fig. 1.Case 1. Axial contrast-enhanced (left) and bone window
(right) CT scans show a well-defined, homogeneously hyperdense
extraaxial lesion in the left temporoparietal region with perilesional ede-
ma, overlying periosteal reaction, and new bone formation (arrow, right)
from the inner table of the skull. In the anterior portion of the lesion,
hypodensity (asterisk, left) secondary to CSF loculation/cyst is noted.
ing hyperactivity and nonsensical speech, for 1 year. He
had undergone operations twice at another hospital, after
which he had remained symptomatic postoperatively. On
both the previous occasions, a histopathological diagnosis
of WHO Grade I fibroblastic meningioma had been made.
Preoperative MRI of his head showed a well-defined fal-
cine region mass that was hypointense on T2-weighted
images and showed peripheral dense enhancement on Fig. 2. Case 2. An axial T2-weighted MR image shows a well-de-
fined hypointense mass in the region of the floor of the anterior cranial
T1-weighted images with contrast administration. There fossa (A). No foci of calcifications are observed on a T2-weighted gra-
was no evidence of calcification. Repeat imaging revealed dient echo image (B). On contrast administration, the peripheral por-
a residual tumor (Fig. 2). The tumor was approached tion of the tumor shows dense contrast enhancement on a T1-weighted
through a bifrontal craniotomy. Intraoperatively, a well- image (C). A postoperative T1-weighted image after Gd administration
demarcated, firm, lobulated, poorly vascularized tumor shows residual tumor (D).
was noted attached to the middle third of the falx cere-
bri, which was reaching up to the base of the falx, more 1 labeling index, at least 500 cells were counted using
on the right side. Simpson Grade II tumor excision was a 1-square-mm eyepiece pinhole. For each batch, appro-
achieved, and the operative specimen was submitted for priate positive and negative controls were taken. Electron
histopathological examination. Sections from the prima- microscopic examination was performed on paraffin-em-
ry tumor stained with H & E were also reviewed. The pa- bedded tumor tissue, after deparaffinization, rehydration,
tient was followed up for a period of 1 year, during which and postfixation in osmium tetroxide.
time no further recurrence or metastasis occurred.
Microscopic Examination. Sections stained with H
Pathological Examination. Tumor tissue was fixed & E from tumors from both patients showed similar fea-
in 10% neutral-buffered formalin, routinely processed, tures (Fig. 3). The tumors were sparsely cellular, com-
and paraffin embedded. Five-micron-thick sections were posed of elongated spindled-shaped cells with a scant to
cut for routine H & E staining and immunohistochemi- moderate amount of pale eosinophilic cytoplasm, and
cal analysis. A labeled streptavidin biotin kit (Universal, normochromatic oval to elongated nuclei with delicate
Dako) was used as a detection system. Antigen retrieval chromatin and inconspicuous nucleoli. The tumor cells
was performed in a microwave oven using citrate buf- were arranged in long parallel fascicles that were embed-
fer at pH 6.0 for all antibodies. Monoclonal antibodies ded in a densely collagenized matrix. Areas of hyaliniza-
against vimentin (Diagnostic BioSystems, 1:100), epithe- tion were present and were more prominent around blood
lial membrane antigen (EMA; Dako, 1:100), pan cytoker- vessels. Sections from both cases showed focal myxoid
atin (Neomarkers, 1:200), claudin-1 (Neomarkers, 1:50), change in the stroma. The tumor cells did not demon-
smooth muscle actin (SMA; Dako, 1:50), progesterone strate nuclear atypia, pleomorphism, mitoses, or areas of
receptors (Neomarkers, 1:50), estrogen receptors (Neo- necrosis. There was no evidence of meningothelial dif-
markers, 1:50), CD34 (Dako, 1:100), bcl-2 (Neomark- ferentiation in the form of whorl formation or sheeting of
ers, 1:100), CD99 (Dako, 1:100), desmin (Dako, 1:50), the tumor cells. Mast cells were observed interspersed be-
glial fibrillary acidic protein (GFAP; Dako, 1:1500), beta tween the tumor cells. Review of sections prepared from
catenin (BD Transduction, 1:200), p53 protein (Santa tumors excised at the first and second surgeries in Case 2
Cruz Biotechnology, 1:1000), and proliferation marker showed similar histomorphological features.
MIB-1 (Dako, 1:200) were used. For assessing the MIB- The tumor cells were immunopositive for vimentin;
156 J Neurosurg: Pediatrics / Volume 14 / August 2014
Meningeal fibroma
Fig. 3. Photomicrographs showing tumor cells in long intersecting fascicles (A and B) with areas of hyalinization (C), focal
myxoid change (D), and thick bundles of collagen in the stroma (E). High magnification shows bland spindle-shaped cells with
elongated nuclei (F), perivascular hyalinization (G), and interspersed mast cells (H). H & E, original magnification 40 (A), 100
(B and C), 200 (D and E), and 400 (FH).
however, they were immunonegative for EMA, S100 pro- nopositivity for p53 protein was noted. Ultrastructural
tein, claudin-1, estrogen receptors, progesterone recep- examination (Fig. 5) of paraffin-embedded tumor tissue
tors, CD34, CD99, bcl-2, beta catenin, desmin, SMA, from both cases showed the presence of artifacts; how-
pan cytokeratin, and GFAP (Fig. 4). The MIB-1 labeling ever, the features were sufficient to recognize the tumor
index was less than 1% in both tumors, and no immu- cells as fibroblasts. Spindle-shaped tumor cells with
J Neurosurg: Pediatrics / Volume 14 / August 2014 157
A. Kakkar et al.
droid metaplasia may be encountered in these tumors,1
the absence of whorls and meningothelial features helps
to distinguish them from fibroblastic meningiomas.12 Im-
munoreactivity with EMA, claudin-1, S100 protein, and
progesterone receptors in meningiomas further aids in this
distinction.12 Another close differential diagnosis is SFT.
These tumors also arise from the meninges, but are usually
observed in adults.1 Solitary fibrous tumors are more cellu-
lar than fibromas, and are composed of interlacing fascicles
Fig. 4. Tumor cells in both cases were found to be immunoposi- of spindle cells rather than long parallel fascicles.1 They are
tive for vimentin (left), and the MIB-1 labeling index was less than 1% immunopositive for CD34, CD99 and bcl-2, while fibro-
(right). Original magnification 400 (left) and 200 (right).
mas are negative for these markers.12 Meningeal gliomas
elongated nuclei, some of which appeared indented, and are extremely rare; the absence of collagen accompanied
abundant dilated rough endoplasmic reticulum were iden- by immunopositivity for GFAP helps to differentiate be-
tified. Some of the cells showed the presence of elongated tween the two tumors.12 Fibromatosis is a histologically
processes. Bundles of collagen fibers were present in the benign but locally invasive condition involving the dura,
extracellular matrix. Intercellular junctions and interdigi- but it has infiltrative margins, whereas fibromas are well
tations were not observed, excluding the possibility of a circumscribed.10 Fibromatosis may occur de novo or at the
meningothelial origin. site of previous surgery or trauma.6 Intracranial myxomas
are rare lesions that arise from the skull bones and may
show attachment to the dura. Radiologically, they are usu-
Discussion ally limited to the inner and outer tables of the skull, while
Intracranial fibromas are rare, benign, fibrous lesions histologically, they are typified by a loose myxoid matrix
that arise from the meninges or from within the brain pa- containing spindled- to stellate-shaped cells with minimal
renchyma.1,4,5 Less than 20 such cases have been described pleomorphism.8 Cranial fasciitis is a reactive proliferation
to date, and their incidence remains unknown.1,2,4,5,7,9,1113 of fibroblastic and myofibroblastic cells in a variably hya-
At our institute, they accounted for 0.12% (2/1648) of all linized and myxoid stroma, which involves the soft tissue
meningeal tumors excised over a 10-year period. Intra- of the scalp and adjacent cranium, and may extend to in-
cranial fibroma was first described in the English litera- volve the dura. Its predilection for the first 6 years of life,
ture by Koos et al. in 1971 in an 11-month-old boy.4 These presence of a lytic skull lesion, prominent myxoid matrix,
fibromas are frequently noted in the first 2 decades of life, and inflammatory cell infiltrate on histology help to distin-
and show a male preponderance.12 These tumors are usu- guish it from meningeal fibroma.3
ally bulky, well-circumscribed masses that, on histologi- Nonmeningothelial tumors of the meninges, includ-
cal examination, are found to be composed of elongated ing fibromas, are much less common than meningiomas.
spindle cells in a dense, eosinophilic, hyalinized collag- Knowledge of these entities is essential for pathologists
enous matrix.1 Due to the rarity of these tumors, no defi- to include them in the differential diagnosis of menin-
nite management protocol is defined for meningeal fibro- giomas, especially in younger patients; this knowledge is
mas. Because these tumors are benign lesions, complete also essential for neurosurgeons because incomplete re-
resection is curative. However, incomplete resection can section may lead to tumor recurrence, and these patients
lead to recurrence or regrowth of the tumor, as noted in need to be closely followed up.
one of our cases.
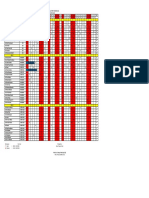
The differential diagnoses of meningeal fibroma in- Disclosure
clude meningioma, SFT, fibromatosis, cranial fasciitis, The authors report no conflict of interest concerning the mate-
meningeal myxoma, and meningeal glioma (Table 1). rials or methods used in this study or the findings specified in this
While psammomatous calcification and osseous and chon- paper.
Fig. 5. Electron photomicrographs showing a tumor cell with elongated nucleus and dilated endoplasmic reticulum (asterisk,
A). Higher magnification shows an indentation in the nucleus and margination of chromatin (B). Bundles of collagen fibers are
noted around the tumor cell (C).
158 J Neurosurg: Pediatrics / Volume 14 / August 2014
Meningeal fibroma
TABLE 1: Immunohistochemical panel for differential diagnosis of fibroma from other meningeal tumors*
Tumor Vimentin EMA S100 SMA CD34 CD99 Bcl-2 Claudin-1 PR GFAP
fibroma + focal +/
meningioma + + +/- + +
SFT + focal +/ + + +
glioma + + +
* PR = progesterone receptors; + = positive; = negative.
Author contributions to the study and manuscript preparation myxoma of the lateral skull base: a rare entity in clinical prac-
include the following. Conception and design: Sharma, Kakkar. tice. Turk Neurosurg 20:8689, 2010
Acquisition of data: Kakkar, Goyal, Kale, A Suri. Analysis and inter- 9. Palma L, Spagnoli LG, Yusuf MA: Intracerebral fibroma:
pretation of data: Sharma, Kakkar, Sarkar, V Suri, Garg. Drafting light and electron microscopic study. Acta Neurochir (Wien)
the article: Kakkar, Goyal. Critically revising the article: Sharma. 77:152156, 1985
Reviewed submitted version of manuscript: all authors. Approved 10. Paulus W, Scheithauer BW, Perry A: Mesenchymal, non-me-
the final version of the manuscript on behalf of all authors: Sharma. ningothelial tumours, in Louis DN, Ohgaki H, Wiestler OD,
et al (eds): WHO Classification of Tumours of the Central
References Nervous System, ed 4. Lyon: IARC Press, 2007, pp 173177
11. Pollack LF, Hamilton RL, Fitz C, Orenstein DM: An intra-
1. Ceyhan K, Berk Q, Caglar S, Src S: A calcifying fibroma sylvian fibroma in a child with cystic fibrosis: case report.
of the meninges report of a case and review of the literature. Neurosurgery 46:744747, 2000
Pathol Res Pract 196:747752, 2000 12. Reyes-Mugica M, Chou P, Gonzalez-Crussi F, Tomita T: Fibro-
2. Hirano A, Llena JF, Chung HD: Fine structure of a cerebellar ma of the meninges in a child: immunohistological and ultra-
fibroma. Acta Neuropathol 32:175186, 1975 structural study. Case report. J Neurosurg 76:143147, 1992
3. Keyserling HF, Castillo M, Smith JK: Cranial fasciitis of 13. Wright DH, Naul LG, Hise JH, Bauserman SC: Intraventricu-
childhood. AJNR Am J Neuroradiol 24:14651467, 2003 lar fibroma: MR and pathologic comparison. AJNR Am J
4. Koos WT, Jellinger K, Sunder-Plassmann M: Intracerebral fi- Neuroradiol 14:491492, 1993
broma in an 11-month-old infant. Case report. J Neurosurg
35:7781, 1971
5. Llena JF, Chung HD, Hirano A, Feiring EH, Zimmerman HM: Manuscript submitted October 17, 2013.
Intracerebellar fibroma. Case report. J Neurosurg 43:98 Accepted May 7, 2014.
101, 1975 Please include this information when citing this paper: pub-
6. Mitchell A, Scheithauer BW, Ebersold MJ, Forbes GS: Intra- lished online June 20, 2014; DOI: 10.3171/2014.5.PEDS13556.
cranial fibromatosis. Neurosurgery 29:123126, 1991 Address correspondence to: Mehar Chand Sharma, M.D.,
7. Mooney JE, Papasozomenos SC: Leptomeningeal fibroma. F.R.C.Path., Department of Neuropathology, All India Institute of
Clin Neuropathol 15:9295, 1996 Medical Sciences, New Delhi 110029, India. email: sharmamehar@
8. Oruckaptan HH, Sarac S, Gedikoglu G: Primary intracranial yahoo.co.in.
J Neurosurg: Pediatrics / Volume 14 / August 2014 159
You might also like
- Raber DS Lantai Bawah Dan Pinere 09-03-22 GHDocument14 pagesRaber DS Lantai Bawah Dan Pinere 09-03-22 GHifanda80No ratings yet
- Mapping Mina 2 MEI 2022: No. Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TD K1B1Document22 pagesMapping Mina 2 MEI 2022: No. Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TD K1B1ifanda80No ratings yet
- Mustafa M. Amin, LK, 53 THNDocument3 pagesMustafa M. Amin, LK, 53 THNifanda80No ratings yet
- Mapping Luar Mina Lantai 2-24 Mei 2022Document31 pagesMapping Luar Mina Lantai 2-24 Mei 2022ifanda80No ratings yet
- Bone MalformationDocument6 pagesBone Malformationifanda80No ratings yet
- Mapping MINA 1 24-05-2022Document29 pagesMapping MINA 1 24-05-2022ifanda80No ratings yet
- Mapping Dr. Nur Astini, SP.S (K) : Mina 1Document8 pagesMapping Dr. Nur Astini, SP.S (K) : Mina 1ifanda80No ratings yet
- Raudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDDocument3 pagesRaudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDifanda80No ratings yet
- Raber DS Lantai Bawah Dan Pinere 05-03-22 GHDocument10 pagesRaber DS Lantai Bawah Dan Pinere 05-03-22 GHifanda80No ratings yet
- Mapping Dr. ImranDocument12 pagesMapping Dr. Imranifanda80No ratings yet
- Dr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1Document4 pagesDr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1ifanda80No ratings yet
- Mina 1 (K6, 7.1-3)Document9 pagesMina 1 (K6, 7.1-3)ifanda80No ratings yet
- DR DR SYAHRUL, SP.S (K)Document28 pagesDR DR SYAHRUL, SP.S (K)ifanda80No ratings yet
- MAPPING DR Elsa 30211016Document7 pagesMAPPING DR Elsa 30211016ifanda80No ratings yet
- DR DR SYAHRUL, SP.S (K)Document28 pagesDR DR SYAHRUL, SP.S (K)ifanda80No ratings yet
- Mapping Dr. ImranDocument12 pagesMapping Dr. Imranifanda80No ratings yet
- MAPPING: Dr. NASRUL MUSADIR SP.S, FINA (TGL 7/10/21) Mina 1Document11 pagesMAPPING: Dr. NASRUL MUSADIR SP.S, FINA (TGL 7/10/21) Mina 1ifanda80No ratings yet
- Jadwal Jaga Ppds Neurologi Agustus 2021 Revisi IIDocument1 pageJadwal Jaga Ppds Neurologi Agustus 2021 Revisi IIifanda80No ratings yet
- Raudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDDocument3 pagesRaudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDifanda80No ratings yet
- Dr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1Document4 pagesDr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1ifanda80No ratings yet
- Dr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1Document4 pagesDr. Dr. Nova Dian Lestari, SP.S (K) 06/11/2021: Mina 1ifanda80No ratings yet
- Raudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDDocument3 pagesRaudha 2: N O Kamar Identitas Subjektif Diagnosis Laboratorium Terapi Planing Keluhan GCS TDifanda80No ratings yet
- Intracerebral Hemorrhage ICHDocument52 pagesIntracerebral Hemorrhage ICHStaporn KasemsripitakNo ratings yet
- DR DR SYAHRUL, SP.S (K)Document28 pagesDR DR SYAHRUL, SP.S (K)ifanda80No ratings yet
- JADWAL JAGA PPDS NEUROLOGI AGUSTUS 2021 REVISI II-dikonversiDocument4 pagesJADWAL JAGA PPDS NEUROLOGI AGUSTUS 2021 REVISI II-dikonversiifanda80No ratings yet
- MINA 2 (K5, Iso, 7.4-6)Document9 pagesMINA 2 (K5, Iso, 7.4-6)ifanda80No ratings yet
- MINA 2 (K5, Iso, 7.4-6)Document9 pagesMINA 2 (K5, Iso, 7.4-6)ifanda80No ratings yet
- MAPPING AQSA 2, Kamis 29 April 2021 (BARU)Document21 pagesMAPPING AQSA 2, Kamis 29 April 2021 (BARU)ifanda80No ratings yet
- Mina 1 (K6, 7.1-3)Document9 pagesMina 1 (K6, 7.1-3)ifanda80No ratings yet
- Mapping Dr. Ika Sp.s (K)Document3 pagesMapping Dr. Ika Sp.s (K)ifanda80No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- MCQs 2Document2 pagesMCQs 2Yahya AlbornoNo ratings yet
- Intl J Gynecology Obste - 2018 - Berek - Cancer of The Ovary Fallopian Tube and PeritoneumDocument20 pagesIntl J Gynecology Obste - 2018 - Berek - Cancer of The Ovary Fallopian Tube and PeritoneumHưng Nguyễn - Yola T.A.No ratings yet
- Hematologic ManagementDocument17 pagesHematologic ManagementAlyssa MontimorNo ratings yet
- Caso 2Document78 pagesCaso 2Khairul ScNo ratings yet
- K Taping in PediatricsDocument154 pagesK Taping in PediatricsNoval Dita Arfina100% (2)
- Acne VulgarisDocument60 pagesAcne Vulgarischarmaine_olivia_1100% (2)
- Pathophysiology of Brain TumorDocument1 pagePathophysiology of Brain TumorAlinor Abubacar100% (1)
- BCPS Study 10monthDocument5 pagesBCPS Study 10monthMagdy Ali ELsherbenyNo ratings yet
- Chronic SinusitisDocument3 pagesChronic SinusitisGabriela Cocieru MotelicaNo ratings yet
- The Stabilization of Plaques Using Darapladib (Solid) - Timi 52 Trial: Primary ResultsDocument23 pagesThe Stabilization of Plaques Using Darapladib (Solid) - Timi 52 Trial: Primary ResultsAnnisa Dwi AndrianiNo ratings yet
- GI MnemonicsDocument14 pagesGI Mnemonicsjonnyahn100% (1)
- Article - Yoga For Women PDFDocument8 pagesArticle - Yoga For Women PDFinsane88No ratings yet
- LuteinDocument38 pagesLuteinirfanmuhfiNo ratings yet
- Chapter 14. Abdominal PainDocument10 pagesChapter 14. Abdominal PaindekergnpNo ratings yet
- A To Z of Phrasal Verbs and Useful Vocabulary Oet 2.0 1 File DownloadDocument3 pagesA To Z of Phrasal Verbs and Useful Vocabulary Oet 2.0 1 File DownloadNurse OetNo ratings yet
- Aspergillus NomiusDocument7 pagesAspergillus NomiusMuh. Ade ArtasastaNo ratings yet
- Science, Technology and Society: (Complimentary and Alternative Medicine)Document26 pagesScience, Technology and Society: (Complimentary and Alternative Medicine)meanneclavioNo ratings yet
- Notiuni Elementare - Linia RomanaDocument123 pagesNotiuni Elementare - Linia RomanaLarla0% (1)
- Peptic Ulcer Disease: Manisha 2 Year, M.SC NursingDocument47 pagesPeptic Ulcer Disease: Manisha 2 Year, M.SC NursingManisha ShakyaNo ratings yet
- Major R Cance Er Miles Stones: Overvie EwDocument14 pagesMajor R Cance Er Miles Stones: Overvie Ewtkobosz4877No ratings yet
- ASME Mag - 0815Document68 pagesASME Mag - 0815Rahman HakimNo ratings yet
- Immunity and Vaccines As Biology Answers AQA OCR EdexcelDocument3 pagesImmunity and Vaccines As Biology Answers AQA OCR EdexcelShela HuangNo ratings yet
- Medical AbbreviationDocument76 pagesMedical AbbreviationNajwa AbdullahNo ratings yet
- Rajiv Gandhi University of Health Sciences Bangalore, KarnatakaDocument7 pagesRajiv Gandhi University of Health Sciences Bangalore, KarnatakaWirawanSiregarNo ratings yet
- Celiac Disease FinalDocument7 pagesCeliac Disease FinalacholineNo ratings yet
- ALZENTALDocument2 pagesALZENTALmahgadNo ratings yet
- 19 Ag 10 PDFDocument4 pages19 Ag 10 PDFfebyan yohanesNo ratings yet
- Nephrotic SyndromeDocument56 pagesNephrotic Syndromeapi-19916399No ratings yet
- Lecture 1-Drinking Water Quality StandardsDocument35 pagesLecture 1-Drinking Water Quality StandardsRoberto Taibo NúñezNo ratings yet
- Housing Letter PDFDocument1 pageHousing Letter PDFLaxmi AbundanceNo ratings yet