Professional Documents
Culture Documents
Celiac Disease Final
Uploaded by
acholineOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Celiac Disease Final
Uploaded by
acholineCopyright:
Available Formats
.
ntroduction
A. Brief Description of the Disease Condition
Also called GIuten-Sensitive Enteropathy.
s a disease of the small intestine marked by atrophy of the villi and microvilli caused by
an immune-mediated inflammatory response to Iuten a protein found in common
grains such as wheat rye oats and barley.
t is most common in young children ages 6 to 24 months but can occur at any age.
Symptoms typically diminish or disappear in adolescence and reappear in early
adulthood.
Complications include impaired growth inability to fight infections electrolyte imbalance
clotting disturbance and possible predisposition to malignant lymphoma of the small
intestine.
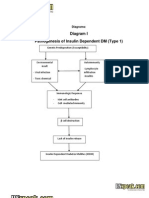
. Pathophysiology of Celiac Disease
A. Cause
Celiac disease is caused by a reaction to gliadin a prolamin (gluten protein) found
in wheat and similar proteins found in the crops of the tribe Triticeae (which includes
other common grains such as barley and rye). Upon exposure to gliadin and specifically
to three peptides found in prolamins the enzyme tissue transglutaminase modifies the
protein and the immune system cross-reacts with the small-bowel tissue causing
an inflammatory reaction. That leads to a truncating of the villi lining the small intestine
(called villous atrophy). This interferes with the absorption of nutrients because
the intestinal villi are responsible for absorption.
B. Risk Factors
People who have a family member with celiac disease are at greater risk for developing
the disease. The disorder is most common in Caucasians and persons of European
ancestry. Women are affected more often than men.
There are various theories as to what determines whether a genetically susceptible
individual will go on to develop coeliac disease. Major theories include infection
by rotavirus or human intestinal adenovirus.
Some research has suggested that smoking is protective against adult-onset Celiac
disease.
People exposed to wheat barley or rye before the gut barrier has fully developed (within
the first three months after birth) had five times the risk of developing Celiac disease
relative to those exposed at four to six months after birth.
Breastfeeding may also reduce risk. A meta-analysis indicates that
prolonging breastfeeding until the introduction of gluten-containing grains into the diet
was associated with a 52% reduced risk of developing Celiac disease in infancy;
whether this persists into adulthood is not clear.
C. Pathophysiologic Processes
The autoimmunity in gluten-sensitive enteropathy involves plasma cells that produce gA
and gG; there is little or no gE involvement. Current theory suggests that ingested d-
gliadin (a component of the gluten protein) and related peptides bind with tissue
transglutaminase (a ubiquitous intracellular enzyme) in enterocytes. The d-gliadin is rich
in glutamine; transglutaminase deamidates glutamine residues forming glutamic acid.
Deamidation enhances the immunogenicity of d-gliadin by creating epitopes that are
recognized as foreign by host cellmediated immunity.
Plasma cells produce gA and gG that are directed against a variety of antigens
including transglutaminase endomysium gliadin and reticulin. Locally elaborated
lymphokines attract inflammatory cells. This intense local inflammatory reaction
produces the villous flattening characteristic of gluten-sensitive enteropathy.
Malabsorption of micronutrients (e.g. vitamins and minerals) and macronutrients (e.g.
protein carbohydrate fat) follows. Small-bowel involvement is most prominent
proximally and may be "patchy especially in patients with "silent celiac disease (i.e.
minimal or no symptoms) and those with dermatitis herpetiformis.
V. Nursing Process
A. Assessment
Ages 3 to 9 months
1. Acutely ill; severe diarrhea and vomiting
2. rritability
. Possible failure to thrive
Ages 9 to 18 months
1. Slackening of weight followed by weight loss
2. Abnormal stools
Pale soft bulky
Offensive odor
Greasy (steatorrhea)
May increase in number
. Abdominal distention
4. Anorexia discoloration of teeth
5. Muscle wasting: most obvious in buttocks and proximal parts of extremities
6. Hypotonia seizures
7. Mood changes: ill humor irritability temper tantrums shyness
8. Mild .Iubbin of finers
9. Vomiting: usually occurs in the evening
10. Aphathous ulcers dermatitis
/er Chi/ an/ A/:t
1. Signs and symptoms are commonly related to nutritional or secondary deficiencies
resulting from disease.
Anemia vitamin deficiency (A D E K)
Hypoproteinemia with edema
Hypocalcemia hypokalemia hypomagnesemia
Hypoprothrombinemia from vitamin K deficiency
Disaccharide (sugar) intolerance
Osteoporosis due to calcium deficiency
2. norexia, fatigue weight loss.
. May have colicky abdominal pain distention flatulence constipation and
steatorrhea.
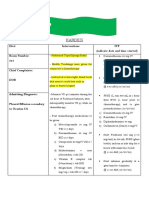
B. Diagnostic Tests
1. Blood Tests
Serological blood tests are the first-line investigation required to make a diagnosis of
celiac disease. gA antiendomysial antibodies can detect celiac disease with
a sensitivity and specificity of 90% and 99% according to a systematic review. The
systematic review estimates that the prevalence of celiac disease in primary care
patients with gastrointestinal symptoms to be about %.
2. nternal Biopsy
An upper endoscopy with biopsy of the duodenum (beyond the duodenal bulb)
or jejunum is performed. t is important for the physician to obtain multiple samples (four
to eight) from the duodenum. Not all areas may be equally affected; if biopsies are taken
from healthy bowel tissue the result would be a false negative.
Most patients with celiac disease have a small bowel that appears normal on
endoscopy; however five concurrent endoscopic findings have been associated with a
high specificity for celiac disease: scalloping of the small bowel folds paucity in the
folds a mosaic pattern to the mucosa (described as a "cracked-mud" appearance)
prominence of the submucosa blood vessels and a nodular pattern to the mucosa.
. Other Diagnostic Tests
At the time of diagnosis further investigations may be performed to identify
complications such as iron deficiency (by full blood count and iron studies) folic
acid and vitamin B
12
deficiency and hypocalcaemia (low calcium levels often due to
decreased vitamin D levels).
Thyroid function tests may be requested during blood tests to identify hypothyroidism
which is more common in people with celiac disease.
[11]
Osteopenia and osteoporosis mildly and severely reduced bone mineral density are
often present in people with celiac disease and investigations to measure bone density
may be performed at diagnosis such as dual energy X-ray absorptiometry (DXA)
scanning to identify risk of fracture and need for bone protection medication.
V. Treatment
A. Diet
At present the only effective treatment is a life-long gluten-free diet. No medication
exists that will prevent damage or prevent the body from attacking the gut when gluten is
present. Strict adherence to the diet allows the intestines to heal leading to resolution of
all symptoms in most cases and depending on how soon the diet is begun can also
eliminate the heightened risk of osteoporosis and intestinal cancer and in some cases
sterility. Dietitian input is generally requested to ensure the patient is aware which foods
contain gluten which foods are safe and how to have a balanced diet despite the
limitations. n many countries gluten-free products are available on prescription and
may be reimbursed by health insurance plans.
B. Refractory Disease
A tiny minority of patients suffer from refractory disease which means they do not
improve on a gluten-free diet. This may be because the disease has been present for so
long that the intestines are no longer able to heal on diet alone or because the patient is
not adhering to the diet or because the patient is consuming foods that are inadvertently
contaminated with gluten. f alternative causes have been eliminated steroids
or immunosuppressants (such as azathioprine) may be considered in this scenario
C. Medical Management
Because patients with severe malabsorption can develop vitamin and mineral
deficiencies vitamin and mineral supplements are important. All patients should take a
multivitamin daily. Patients with iron deficiency anemia should be treated with iron.
Patients with anemia due to folate or B12 deficiency should be treated with folic acid and
B12. Patients with an abnormal ProTime should be treated with vitamin K. Patients with
low blood calcium levels or with osteoporosis should be treated with calcium and vitamin
D supplements.
V. Nursing Diagnoses and Expected Outcomes
mbalanced Nutrition: less than body requirements related to malabsorption secondary to Celiac
disease
Monitor dietary intake fluid intake and output weight serum electrolytes and hydration
status.
Make sure that the diet is free from causative agent but inclusive of essential nutrients
such as protein fats vitamins and minerals.
Maintain NPO status during initial treatment of celiac crisis or during diagnostic testing.
Stress that the disorder is lifelong; however changes in the mucosal lining of the
intestine and in general clinical conditions are reversible when dietary gluten is avoided.
Altered comfort: pain related to the inflammatory of the small intestine secondary to Celiac
disease.
Assess level of pain by observation
Subjective assessment by accepting patient's description of pain. Acknowledge the pain
experience and convey acceptance of patient's response to pain.
Monitor vital signs
Administer medications as ordered
E INFO)
There is no cure for celiac disease. The treatment of celiac disease is a gluten free diet. Celiac
disease patients vary in their tolerance of gluten; some patients can ingest small amounts of
gluten without developing symptoms while others experience massive diarrhea with only minute
amounts of gluten. The standard treatment of disease patients calls for complete avoidance of
gluten for life. The principles of a gluten free diet include:
1. Avoid all foods made from wheat rye and barley. Examples are breads cereals pasta
crackers cakes pies cookies and gravies.
2. Avoid oats. Some patients with celiac disease can tolerate oats in the diet. But long-term safety
of oats in celiac disease patients is unknown. Also some oat preparations can be contaminated
with wheat. Thus it is probably best to avoid oats at least during the initial treatment with a
gluten free diet. Once disease remission is achieved with a strict gluten free diet small
quantities of oats can be reintroduced into the diet under medical supervision.
. Pay attention to processed foods that may contain gluten. Wheat flour is a common ingredient in
many processed foods. Examples of foods that may contain gluten to name only a few include:
O canned soups
O salad dressings
O ice cream
O candy bars
O instant coffee
O luncheon meats
O ketchup
O mustard
O processed and canned meats
O yogurt
O sausages and
O pasta.
4. Beware of tablets capsules and vitamin preparations that contain gluten. Wheat starch
is commonly employed as a binding agent in tablets and capsules. Gluten also can be
found in many vitamin products and cosmetic products such as lipstick.
5. Avoid beer
6. t is all right to drink wine brandy whiskey and other non-wheat or barley alcohol (in
moderation!)
7. Avoid milk and other dairy products that contain lactose. Untreated patients with celiac disease
often are lactose intolerant. With successful treatment dairy products can be reintroduced
slowly into the diet later.
8. t is alright to consume fish fresh meats rice corn soybean potato poultry fruits vegetables
and dairy products (for patients who are not lactose intolerant)
9. Consult dietitians and national celiac disease societies for lists of gluten free foods. Read the
food and product labels before buying or consuming any product. This is necessary because a
manufacturer may change a product's ingredients at any time. A product that was gluten-free in
the past may now contain gluten. Even branded products may be gluten free in one country but
contain gluten in another country. f one is not certain after reading the labels call the
manufacturer.
You might also like
- Hypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Celiac Disease Case StudyDocument13 pagesCeliac Disease Case Studyapi-258654446No ratings yet
- Case Study 1-1Document9 pagesCase Study 1-1api-242226130No ratings yet
- Celiac Disease: An Autoimmune Condition Triggered by GlutenDocument2 pagesCeliac Disease: An Autoimmune Condition Triggered by GlutenGiabellNo ratings yet
- Case Study 1 - Mrs. SmithDocument3 pagesCase Study 1 - Mrs. SmithJulia CooperNo ratings yet
- CnsDocument15 pagesCnsArun GeorgeNo ratings yet
- Case Study2Document11 pagesCase Study2Jainet Aira S. AmanteNo ratings yet
- Typhoid FeverDocument17 pagesTyphoid FeverKyle Margaret Flores100% (1)
- Case Study Benign Tumors of The Uterus: MyomaDocument3 pagesCase Study Benign Tumors of The Uterus: MyomaToto RyanNo ratings yet
- Kardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313Document2 pagesKardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313kuro hanabusaNo ratings yet
- Gouty Arthritis: Presented By: Petit Ivy Mae B. NacarioDocument21 pagesGouty Arthritis: Presented By: Petit Ivy Mae B. NacarioMarivic DianoNo ratings yet
- Discharge PlanDocument1 pageDischarge PlanKamille Bianca Macapagal ÜNo ratings yet
- Community Nutrition Quiz AnswersDocument3 pagesCommunity Nutrition Quiz AnswersAli Aufar HutasuhutNo ratings yet
- Diabetes PathophysiologyDocument2 pagesDiabetes PathophysiologyRyan MulanoNo ratings yet
- Inflammatory Bowel Disease .. Last EditDocument22 pagesInflammatory Bowel Disease .. Last EditRashed ShatnawiNo ratings yet
- Tenofovir Disoproxil Fumarate: Therese M. Chapman, Jane K. Mcgavin and Stuart NobleDocument12 pagesTenofovir Disoproxil Fumarate: Therese M. Chapman, Jane K. Mcgavin and Stuart NobleBagusHibridaNo ratings yet
- Case Study - Leukemia2Document4 pagesCase Study - Leukemia2shaiya08No ratings yet
- Drug StudyDocument4 pagesDrug StudyFrances Oscar GaviolaNo ratings yet
- DB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaDocument5 pagesDB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaNeil Alcazaren かわいいNo ratings yet
- Celiac DiseaseDocument8 pagesCeliac DiseaseKristine KaneichiNo ratings yet
- Epidemiology and Pathophysiology of Colonic Diverticular DiseaseDocument8 pagesEpidemiology and Pathophysiology of Colonic Diverticular DiseaseAnonymous Hz5w55No ratings yet
- Rle Week 13Document8 pagesRle Week 13Roselyn Yu QuintoNo ratings yet
- AcetylcysteineDocument2 pagesAcetylcysteineJonah Camille Yap FortunaNo ratings yet
- MalnutritionDocument5 pagesMalnutritionCarlo Pasaol Alang Jr.No ratings yet
- Midterm Exam Antiinfective, Biotic, ViralDocument5 pagesMidterm Exam Antiinfective, Biotic, ViralJojo Justo100% (2)
- MedSurg Notes - Cancer of The LiverDocument2 pagesMedSurg Notes - Cancer of The LiverMae CeaesarNo ratings yet
- Hashimoto EncephalopathyDocument37 pagesHashimoto EncephalopathyIbrahim IbrahimNo ratings yet
- Health Teaching PlanDocument17 pagesHealth Teaching Planvictoria joy patauegNo ratings yet
- Case StudyDocument17 pagesCase StudyNikko DioNo ratings yet
- Drugs Study Ward 9 (Corvera)Document5 pagesDrugs Study Ward 9 (Corvera)Herbert Almendras HuyoNo ratings yet
- Case Report of PneumoniaDocument3 pagesCase Report of PneumoniaCobzaru Mihai0% (1)
- Importance of Honesty in MedicineDocument3 pagesImportance of Honesty in MedicineSuiweng WongNo ratings yet
- REVALIDADocument53 pagesREVALIDAMercy Anne EcatNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD) and Bronchial AsthmaDocument16 pagesChronic Obstructive Pulmonary Disease (COPD) and Bronchial AsthmaAngel Joy CatalanNo ratings yet
- Case+Study AGN MINEDocument66 pagesCase+Study AGN MINEJm BernardoNo ratings yet
- Nursing Research PaperDocument15 pagesNursing Research Paperapi-502994344No ratings yet
- Anaphylactic ReactionDocument9 pagesAnaphylactic ReactionZahir Jayvee Gayak IINo ratings yet
- Ulcerative ColitisDocument18 pagesUlcerative ColitisHoussein EL HajjNo ratings yet
- Ulcerative ColitisDocument14 pagesUlcerative ColitisdeepuNo ratings yet
- Individual PediaDocument37 pagesIndividual PediaLianna M. MilitanteNo ratings yet
- 12 Rights of Drug AdministrationDocument1 page12 Rights of Drug Administrationkarendelarosa06277No ratings yet
- Acute Glomerulonephritis 1Document19 pagesAcute Glomerulonephritis 1Jane Ann AlolodNo ratings yet
- Bacillary DysenteryDocument32 pagesBacillary Dysenteryapi-199163990% (1)
- Gordon's health patternsDocument5 pagesGordon's health patternsnerlynNo ratings yet
- Supersize Me by Morgan Spurlock 1Document7 pagesSupersize Me by Morgan Spurlock 1api-317451959No ratings yet
- Presentation PathophysiologyDocument11 pagesPresentation PathophysiologyJade DeopidoNo ratings yet
- Liver Cirosis Case StudyDocument18 pagesLiver Cirosis Case StudyDaniel LaurenteNo ratings yet
- Assessment 2 - Nursing Case Study - 2019Document2 pagesAssessment 2 - Nursing Case Study - 2019Chinney ArceNo ratings yet
- Family Nursing Care Plan TypologyDocument6 pagesFamily Nursing Care Plan TypologyLouwella RamosNo ratings yet
- Edward JennerDocument5 pagesEdward JennerAnto FreistyawanNo ratings yet
- Lactating MotherDocument5 pagesLactating MotherAljane VistoNo ratings yet
- Example of Health GenogramDocument1 pageExample of Health Genogramapi-322059527No ratings yet
- Pregnant Woman in LaborDocument2 pagesPregnant Woman in LaborRabena, Steven Allen100% (1)
- Leukemia (: American English British English Cancer Blood Bone Marrow White Blood Cells BlastsDocument7 pagesLeukemia (: American English British English Cancer Blood Bone Marrow White Blood Cells BlastsArulmani MurugesanNo ratings yet
- Gordon's Functional Health PatternsDocument2 pagesGordon's Functional Health PatternsJelai D0% (1)
- Chronic Kidney Disease Secondary To Type 2 Diabetes MellitusDocument84 pagesChronic Kidney Disease Secondary To Type 2 Diabetes Mellituswar5No ratings yet
- Gastrointestinal System Disorders NCLEX Practice QuizDocument82 pagesGastrointestinal System Disorders NCLEX Practice QuizZhailyn Joy DumlaoNo ratings yet
- A Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsNo ratings yet
- NCP (Sabanal)Document3 pagesNCP (Sabanal)acholineNo ratings yet
- Resource Unit On Hirschsprung's DiseaseDocument26 pagesResource Unit On Hirschsprung's DiseaseacholineNo ratings yet
- JRADocument9 pagesJRAacholineNo ratings yet
- Resource Unit On The Care of Depressed, Withdrawn and Suicidal PatientsDocument19 pagesResource Unit On The Care of Depressed, Withdrawn and Suicidal PatientsacholineNo ratings yet
- Computer Engineering SyllabusDocument47 pagesComputer Engineering SyllabusLily ChanNo ratings yet
- Parapsychology QP - WikiDocument371 pagesParapsychology QP - WikiAdamNo ratings yet
- Welcome Students!: Week 8 (3 Quarter)Document28 pagesWelcome Students!: Week 8 (3 Quarter)Erika Lloren Luyun-GaliaNo ratings yet
- CHS-WWW - Polsteel. TUBOS METALICOS PDFDocument3 pagesCHS-WWW - Polsteel. TUBOS METALICOS PDFEduardo TorreNo ratings yet
- Wily Walnut BRAIN SQUEEZERS Vol.1Document116 pagesWily Walnut BRAIN SQUEEZERS Vol.1tarzaman88% (8)
- Deks Olje ArticleDocument5 pagesDeks Olje ArticleTomMacNaughtonNo ratings yet
- GLOBAL GAME AFK IN THE ZOMBIE APOCALYPSE GAME Chapter 201-250Document201 pagesGLOBAL GAME AFK IN THE ZOMBIE APOCALYPSE GAME Chapter 201-250ganesh sarikondaNo ratings yet
- Fire and Blast in The Future OffshoreDocument45 pagesFire and Blast in The Future OffshoredrgNo ratings yet
- Circuit Diagram:: Experiment No: 3 Title: Characteristics of Filament Lamp ObjectivesDocument2 pagesCircuit Diagram:: Experiment No: 3 Title: Characteristics of Filament Lamp ObjectivesAsrar Hussain BhatNo ratings yet
- Stereochemistry MSCDocument29 pagesStereochemistry MSCBapu Thorat50% (2)
- BrosurDocument68 pagesBrosurKiki Xhui7No ratings yet
- Factory made uPVC windows installationDocument2 pagesFactory made uPVC windows installationAmit Singh100% (2)
- SK716 Pengintegrasian Mekanisme Nilai Karbon (English)Document13 pagesSK716 Pengintegrasian Mekanisme Nilai Karbon (English)Isti HanifahNo ratings yet
- Hydraulic Excavator RH 200 1,568 kW 30.5 m3Document8 pagesHydraulic Excavator RH 200 1,568 kW 30.5 m3mchan1965100% (1)
- GROHE Specification Sheet 19443000-1Document2 pagesGROHE Specification Sheet 19443000-1Fred PrzNo ratings yet
- Design of A Tuned Intake Manifold - H. W. Engelman (ASME Paper 73-WA/DGP-2)Document9 pagesDesign of A Tuned Intake Manifold - H. W. Engelman (ASME Paper 73-WA/DGP-2)david_luzNo ratings yet
- Thalassemia: Submitted By: Jovan Pierre C. Ouano Submitted To: Mark Gil T. DacutanDocument8 pagesThalassemia: Submitted By: Jovan Pierre C. Ouano Submitted To: Mark Gil T. DacutanJvnpierre AberricanNo ratings yet
- Physics Formulas and Symbols: Physics I Symbol FormulaDocument5 pagesPhysics Formulas and Symbols: Physics I Symbol Formulakaparthy100% (9)
- Category D Fluid ServiceDocument2 pagesCategory D Fluid Serviceaslam.ambNo ratings yet
- Management Foreign BodyDocument6 pagesManagement Foreign BodyRahmatia SyukrinaNo ratings yet
- Bosch EBike Product Catalogue MY2021 enDocument92 pagesBosch EBike Product Catalogue MY2021 enIvanNo ratings yet
- Air release plug and lifting lug details for 15 MVA 66/11.55 kV transformer radiatorDocument1 pageAir release plug and lifting lug details for 15 MVA 66/11.55 kV transformer radiatorshravan Kumar SinghNo ratings yet
- Brochure - 2018 - Hitfact Mkii 2Document2 pagesBrochure - 2018 - Hitfact Mkii 2diaa ahmedNo ratings yet
- Design & Operation of Clean Room-1Document39 pagesDesign & Operation of Clean Room-1Hafizur Rahman0% (1)
- The Storage Handling and Transportation of Ammonium Nitrate Based Fertilisers 2015Document58 pagesThe Storage Handling and Transportation of Ammonium Nitrate Based Fertilisers 2015Minh Đức TạNo ratings yet
- Creme Brulee - Printer Friendly PDFDocument1 pageCreme Brulee - Printer Friendly PDFmtlpcguysNo ratings yet
- Random Variate Generation-1Document21 pagesRandom Variate Generation-1Christian Delas AlasNo ratings yet
- MetdsgffggDocument263 pagesMetdsgffggVishal Singh GaharwarNo ratings yet
- Interpuls Novinki 2014Document64 pagesInterpuls Novinki 2014BaklanovaSVNo ratings yet
- Genética, Modificaciones y MutacionesDocument12 pagesGenética, Modificaciones y MutacionespokemaniacoplancheNo ratings yet