Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
6 viewsVet Corticosteroid For Dermatitis TX
Vet Corticosteroid For Dermatitis TX
Uploaded by
evelynmiles42Home treatment for dogs
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Basic Life Support: Participant's ManualDocument122 pagesBasic Life Support: Participant's Manualelkyec0% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Vaccines, Social Media and The Public HealthDocument16 pagesVaccines, Social Media and The Public HealthChinmay KalakondaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Maternal and Child Nursing - Student - HandoutsDocument40 pagesMaternal and Child Nursing - Student - HandoutsPaulAliboghaNo ratings yet
- Learn For Help Earn For Learn : Formative Assessment For CBT&A Level-4Document5 pagesLearn For Help Earn For Learn : Formative Assessment For CBT&A Level-4সত্য চন্দ্র প্রামাণিক100% (1)
- Admission LetterDocument2 pagesAdmission LetterzeenahNo ratings yet
- Moved To TearsDocument8 pagesMoved To TearsLuzia PeraNo ratings yet
- Concept Map PedsDocument6 pagesConcept Map Pedsapi-546398486No ratings yet
- Kuisioner Chandra AsriDocument8 pagesKuisioner Chandra AsriTumbal PogoNo ratings yet
- Jacobsen H100Document44 pagesJacobsen H100Lady Marcela RodriguezNo ratings yet
- The Humanistic School of PsychologyDocument17 pagesThe Humanistic School of PsychologyJohnNo ratings yet
- ADC Standard OSCE Communication Marking RubricDocument2 pagesADC Standard OSCE Communication Marking RubricAshik M RasheedNo ratings yet
- Ethical Issues Arising From PandemicDocument6 pagesEthical Issues Arising From PandemicmarengbibNo ratings yet
- MCP 02@3Document150 pagesMCP 02@3Julie ann CamitanNo ratings yet
- Introduction Disaster NursingDocument11 pagesIntroduction Disaster NursingydtrgnNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument8 pagesChronic Obstructive Pulmonary DiseaseGeozel VivienneNo ratings yet
- FV FOS8 Module6Document8 pagesFV FOS8 Module6EsNo ratings yet
- Kontratransfer U Psihoterapiji Poremećaja Ličnosti Ili Kako Biti Šaptač Ljudima?Document21 pagesKontratransfer U Psihoterapiji Poremećaja Ličnosti Ili Kako Biti Šaptač Ljudima?Iva LučićNo ratings yet
- Introduction To Human Resource ManagementDocument5 pagesIntroduction To Human Resource ManagementLianne VonNo ratings yet
- Datasheet: Rigid Box Seals - Fire OnlyDocument2 pagesDatasheet: Rigid Box Seals - Fire OnlyEdgar ArdinazoNo ratings yet
- Philips Pacing PadsDocument12 pagesPhilips Pacing PadsGeneral Health CareNo ratings yet
- Beverly MuseDocument1 pageBeverly MuseEmilioOsorioNo ratings yet
- HPM and H and B - Daryl E. CandoDocument41 pagesHPM and H and B - Daryl E. CandoDaryl CandoNo ratings yet
- Witnesses Claim Babys Death Must Be HomicideDocument2 pagesWitnesses Claim Babys Death Must Be Homicideapi-3750354No ratings yet
- Tarife Servicii Medicale Amb 2Document8 pagesTarife Servicii Medicale Amb 2Ioana RaduNo ratings yet
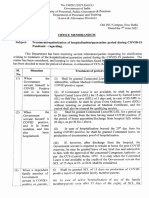
- DoPT Guidelines On Treatment - Regularization of Hospitalization - Quarantine Period During COVID 19 PandemicDocument2 pagesDoPT Guidelines On Treatment - Regularization of Hospitalization - Quarantine Period During COVID 19 PandemictapansNo ratings yet
- Project Management Theory and Practice - MBA 7023Document30 pagesProject Management Theory and Practice - MBA 7023Tharshi100% (1)
- Practice Occupational Health & Safety ProceduresDocument37 pagesPractice Occupational Health & Safety ProceduresEgghead YTCNo ratings yet
- Weight Loss PDFDocument72 pagesWeight Loss PDFMarilda QuiassataNo ratings yet
- The Art of Letting Go Stop Overthinking Stop Negative Spirals and Find Emotional Freedom The Path To Calm Book 13Document170 pagesThe Art of Letting Go Stop Overthinking Stop Negative Spirals and Find Emotional Freedom The Path To Calm Book 13Damayanti SinagaNo ratings yet
- Betty - Speech On Girl Child Education in Uganda August 2017Document9 pagesBetty - Speech On Girl Child Education in Uganda August 2017dennisNo ratings yet
Vet Corticosteroid For Dermatitis TX
Vet Corticosteroid For Dermatitis TX
Uploaded by
evelynmiles420 ratings0% found this document useful (0 votes)
6 views6 pagesHome treatment for dogs
Original Title
Vet Corticosteroid for Dermatitis TX
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentHome treatment for dogs
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views6 pagesVet Corticosteroid For Dermatitis TX
Vet Corticosteroid For Dermatitis TX
Uploaded by
evelynmiles42Home treatment for dogs
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 6
Canine Atopic Dermatitis:
Clinical Disease, Diagnosis, and Treatment
Randall C. Thomas, DVM, DACVD.
Charleston, South Carolina
Introduction
Canine atopic dermatitis (AD) is thought to be a genetically inherited, Type | hypersensitivity to
environmental allergens. Common allergens include grass, tree, and weed pollens, molds, house
dust and house dust mites.
‘The incidence of AD in the canine population is unknown. Previous studies have estimated a 3-
15% incidence in the canine population. However, reliable studies are difficult to complete. It is
generally thought that in those geographic areas that support flea development, the incidence of
AD is second to flea allergy dermatitis. In some areas of the country, however, the incidence of
‘AD my exceed that of flea allergy. Studies in human medicine indicate an increased incidence of
‘AD in the human population. Anecdotally, there appears to be a similar increase in canine AD.
As stated above, AD is thought to be a genetically inherited condition. Although progress is being
made, the mode of inheritance has not been definitively determined. The idea of heritability is
supported by the increased incidence within certain breeds, but the clinical manifestations of AD
‘are most likely multifactorial.
Clinical Signs and Diagnosis of Canine Atopic Dermatitis
The clinical signs of canine atopic dermatitis have been characterized over the past several
decades. Erythema and pruritus are considered to be hallmark signs of atopy. Usually, dogs
develop clinical signs between 6 months and 3 years of age. Most dogs wil initially have distinct
seasonality. With time, however, the majority will go on to develop nonseasonal symptoms. In
certain geographic locations, a lack of seasonality from the beginning is common. The more
common areas of pruritus in the atopic dog include the face, ears, paws, extremities, and/or
ventrum. While many dogs will exhibit pruritus in most or all of these locations, some will have
fairly localized symptoms. AD has historically been considered the “itch that rashes,” meaning
that there is no primary lesion associated with initial symptoms. Recently, some dermatologists
have suggested that AD may be associated with a primary eruption such as an erythematous
macule, papule or plaque. With chronicity, secondary lesions such as excoriation, lichenification,
and hyperpigmentation may occur. Secondary bacterial pyoderma and Malassezia dermatitis are
also common. Other symptoms associated with canine AD include changes to the quality of the
hair coat, conjunctivitis, rhinitis, urticaria, pyotraumatic dermatitis, acral lick dermatitis, seborrhea,
and hyperhidrosis. Otitis, with or without secondary infection can be the sole symptom of atopy
in the dog
Differentials for pruritus in the dog include ectoparasites (scabies, demodicosis), infection
(bacterial, fungal), allergies (flea allergy dermatitis, food allergy, contact allergies), ‘metabolic
causes (hepatocutaneous syndrome), and neoplasia (epitheliotropic lymphoma). Differentials
can be narrowed based on history, concurrent clinical signs, and basic diagnostics. A strong
suspicion for atopic dermatitis should be made based on history, physical exam findings, and
ruling out other pruritic diseases before “allergy testing” is performed.
Allergy Testing
If the dog’s history and clinical signs are consistent with other pruritic diseases, | attempt to rule
them out prior to doing allergy testing. In addition, | recommend allergy testing only for the
development of a therapy. There is no benefit to knowing which specific reactions the dog has if
the owners have no interest in pursuing allergen-specfic immunotherapy (ASIT)
Many labs offer serum allergy testing, and an enti lecture could be given regarding this subject.
Current available in vitro tests are typically RAST or ELISA tests. Most labs use polyclonal anti
IgE for the detection of allergen-specific IgE in patients’ serum. One lab utlizes a unique
recombinant fragment of the extracellular portion of the human high-affinity IgE receptor (FoeRIa)
for detection. Because each lab's techniques are different, comparison between labs is difficult.
Traditionally, a lack of specificity (false positive reactions) has plagued serum allergy testing
Procedures. Newer technology has helped to diminish (but not eliminate) false positives,
Intradermal testing involves injection of small quantities of allergen within the dermis and
‘observation for immediate wheal and flare reaction. While most dermatologists have considered
this to be the "gold standard” for allergy testing in the dog, itis not infalible. The disadvantage of
skin testing is lower sensitivity (false negative reactions). This can be limited by appropriate
withdrawal of medications that suppress wheal and flare reactions (systemic and topical
corticosteroids and antihistamines).
Results of serum and intradermal allergy tests on the same patient rarely correlate. In the past,
many have used this lack of correlation as evidence that serum-based tests are inaccurate. This
may not be the case, however. In my practice, | recommend intradermal testing as the most
reliable method for developing allergen-specific immunotherapy. However, for those dogs in
which sedation, clipping, and/or withdrawal of medications is not possible, we will utlize serum
allergy testing.
Once the allergy test results are available, it is your responsibilty to choose the relevant allergens
that should be included in the allergy immunotherapy. This may have more influence on your
success than the allergy test you choose. First of all, only those allergens that are found in the
patient's environment should be considered. The seasonally of the positive reactions needs to
be compared to the dog's symptoms. Lastly, avoidance should be practiced whenever possible.
Ina flea allergic dog, strict flea control should be practiced. ASIT with flea antigen has typically
been unrewarding.
Therapy
‘Secondary Infections
Managing secondary infections is a critical part of treating any atopic dog. For dogs with
superficial pyoderma, 3 weeks of an appropriate antibiotic is recommended. If deep pyoderma is
present 4-8 weeks or longer may be necessary. A good antibacterial shampoo should also be
recommended to assist in resolution of the infection. if Malassezia dermatitis is present, topical
therapy alone, or in conjunction with systemic antifungal therapy should be utilized. A significant
reduction in pruritus will usually be seen when secondary infections are resolved. In addition,
both steroidal and nonsteroidal antipruritic therapies will be more effective if the patient is free of
secondary infections.
Topical Antipruritic Therapy
Don't forget the beneficial effects of water. Cool water baths decrease pruritus by soothing the
skin and washing away inflammatory mediators and potential allergens.
Colloidal oatmeal is a safe and relatively effective antiprurtic, although the exact mechanism of
this effect is poorly understood. Veterinary oatmeal-based products are available as shampoos,
conditioners, and bath treatments. Some velerinary products have combined colloidal oatmeal
with diphenhydramine, and one product is formulated as a “leave-on” conditioner to provide a
residual effect. Topical anesthetics are also available, and may have temporary antipruritic
effects. Pramoxine has been the topical anesthetic of choice in veterinary medicine. Other
products, such as lidocaine and benzocaine may cause cutaneous sensitivity or toxic effects
(methemoglobinemia). Pramoxine is usually combined in shampoo or rinses with colloidal
‘oatmeal. Itis also available as a spray and a leave-on conditioner.
Colloidal-oatmeal products, with or without additional ingredients, are most useful for mild
pruritus. They are safe for chronic use in most patients. When secondary infections are present,
they should be resolved with systemic or topical antimicrobial therapy. Patients that are free of
these infections will be most responsive to the colloidal-oatmeal topicals.
Lime suffur (LymDyp®, DVM Pharmaceuticals) is a very effective, nonsteroidal antipruritc.
Because it is applied as a rinse and allowed to dry on the animal, it provides residual effect. Lime
sulfur is safe for use in both dogs and cats. However, | recommend that cats have an E-collar
applied until dry, as there are anecdotal reports of Gi upset and pharyngitis following ingestion of
the dip. | often recommend the use of lime sulfur dips while animals are being withdrawn from
antihistamines and corticosteroids for allergy testing. In addition to its antipruritic effects, lime
sulfur is antiparasitic and antifungal.
A recently introduced product may be an effective antipruritic by combining novel ingredients.
‘Allermy® (Virbac) contains linoleic acid and a monosaccharide, L-rhamnose in a microemulsion.
Topical application of linoleic acid has previously been shown to improve cutaneous barrier
function in the dog. Barrier function is a protective mechanism of the skin, and may be defective
in dogs with atopic dermatitis. In vitro, L-hamnose has been shown to decrease inflammatory
mediators that may be involved in the pathogenesis of atopic dermatitis. In addition to the
shampoo, Allermy! lotion has recently been introduced. This product can be sprayed onto
localized areas of pruritus between baths.
Topical corticosteroids are very effective antipruritic drugs, and are commonly used in treatment
of pruritus in humans. Until recently, most veterinary topical steroid products came as ointments,
‘creams, or powders for localized use. Generalized use of these products in our veterinary
patients has been limited by the hair coat and concern over ingestion of the product. In recent
years, products that lend themselves to generalized use have become available.
‘Two corticosteroid-containing shampoo products are available, CortiSoothe® (Virbac) is a 1-%
hydrocortisone containing shampoo with a colloidal oatmeal base. Capex® shampoo (formerly
known as F/S Shampoo) contains 0.01% fluocinolone acetonide, a fluorinated corticosteroid.
While topical application of fluorinated corticosteroids can be associated with systemic
absorption, use of this product twice weekly did not result in systemic evidence of absorption or
adrenal suppression, There is minimal residual activity noted with use of corticosteroid
shampoos.
A 1-% hydrocortisone, leave-on conditioner is also available (ResiCort®, Virbac). This product
may be applied to the entire body and allowed to dry. The base of the product is non-irtating,
znd is not intended to be rinsed off. When this product was applied to normal and allergic dogs
twice weekly for 6 weeks, mean values for hematological, biochemical and adrenal response to
exogenous ACTH remained within normal limits. In one dog with inflamed skin, a lack of
response to exogenous ACTH was detected at the end of the study, suggesting that absorption of
the product was increased through inflamed skin. For that reason, even use of 1%-hydrocortisone
should be done cautiously in small dogs with generalized erythema and pruritus.
Fluorinated corticosteroid products are also available as ointments, creams, and sprays. While
these products are effective antipruritics, they are only intended for short-term, localized use.
Numerous studies have demonstrated that application of fluorinated corticosteroids to the skin,
‘ears, and eyes can result in systemic absorption and suppression of the adrenal axis. In addition
to systemic effects, localized cutaneous atrophy, alopecia, comedone formation, and pyoderma
may occur. Subepidermal bullous dermatosis has also been associated with topical application of
some fluorinated corticosteroids.
Genesis Topical Spray@ (Virbac) has recently been introduced to veterinary medicine. This is a
0.015% triamcinolone spray, approved by the FDA for generalized use in the pruritic dog. In a
blinded, placebo-controlled ‘study of 103 dogs with pruritus of various causes, 67% showed
significant reductions in erythema, pruritus, and eruption over 28 days. In that study,
hematological and biochemical results of treated dogs did not change significantly over the
course of treatment. in a separate study, the product was demonstrated to be effective for
symptomatic treatment of flea allergy dermatitis in the dog. This product is intended for
‘generalized use over short periods of time (28 days or less) as an alternative to oral or injectable
corticosteroids.
Antihistamines and Tricyclic Antidepressants
Histamine is a potent inflammatory mediator, and may be @ major mediator of pruritus in the dog.
For that reason, antihistamines have been advocated for antiprurtic therapy. The first generation
antihistamines are H1 receptor blockers. In this manner, they antagonize the physiologic effects
of histamine following its release. Some, such as hydroxyzine, also inhibit mast cell
degranulation. Because the first generation antihistamines readily cross the blood-brain barrier
(GBB), they may lead to increased sedation. The second-generation antihistamines are also H1
receptor antagonists. They are less lipid soluble, and therefore do not readily cross the BBB.
Several studies have evaluated the efficacy of systemic antihistamines in the dog. Significant
improvement has been seen in 0% to 30% of patients in these studies. The first-generation
antihistamines diphenhydramine, hydroxyzine, chlorpheniramine, and clemastine have been
shown to be relatively effective in non-blinded, uncontrolled studies. Trimeprazine was shown to
be ineffective alone, but has been demonstrated to significantly decrease the dose of prednisone
(by about 30%) necessary to control pruritus.
Because antihistamines are metabolized by the liver, they should be used with caution in the
presence of hepatic disease. Due to their anticholinergic properties, they should be used
cautiously in patients with glaucoma, gastrointestinal atony or urinary retention problems.
The tricyclic antidepressant (TCA) drugs, amitriptyline, and doxepin have also been
recommended in the dog for control of pruritus. Both these drugs have potent antihistamine
effects. In one study, doxepin did not provide relief for any of 30 dogs. Amitriptyline has been
shown to be effective in approximately 30% of dogs. In my practice, sedation is the most
commonly reported side effect. | usually start patients on half of the therapeutic dose for the first
1-2 weeks in order to acclimate to the drug. After 1-2 weeks, most dogs will tolerate the full dose
without significant sedation. Other, rarely reported side effects of TCA’s include dry mouth,
hypersalivation, vomiting, cardiac arrhythmias, sedation, and urinary retention. Use of TCA’s is
contraindicated in dogs with cardiac problems or hepatic disease. Use is also contraindicated
with other monoamine oxidase inhibitors like amitraz.
From an efficacy standpoint, itis important to note that there is tremendous variation in individual
response to antihistamines. Therefore, it is often necessary to try several different products
before finding the one that works best in each patient. In order to appropriately evaluate the
efficacy of antihistamines, secondary infections should be resolved. In addition, the combination
of antihistamines with essential fatty acid supplements (below) may be synergistic.
Antihistamines in the dog
Drug Dosage
Diphenhydramine (Benadryl) 2.2 mgikg q 8 hrs.
Hydroxyzine HCI (Aterax) or pamoate 2.2 mglkg q 8 hrs.
‘Chiorpheniramine (Chlor-Trimeion) 02.0.8 mokkg 8 hrs.
Clemastine fumarate (Tavist) (0.05-0.1 mg/kg q 12 brs
Loratidine (Clariton) 10 maldog 24 hrs
Cetirizine (Zyrtec) 510 mg/ dog q 24 hrs
‘Amitriptyline (Elavil) 4-2 mghkg q 12 hrs.
Doxepin (Sinequan)
4-2 mglkg q 12 brs.
Essential Fatty Acids
Fatty acid supplements have been reported to be beneficial in management of pruritus in dogs
and cats. There are numerous veterinary and over-the-counter products available. Very few
products have been critically evaluated in good, scientific studies.
‘The way in which EFA’s work is complicated, and a lecture unto itself. Simply put, however, the
EFA's are incorporated into the epithelial cell membrane, and compete with arachidonic acid for
Utilization of lipoxygenase and cyclo-oxygenase pathways. This results in the production of less
inflammatory mediators within the skin.
Several studies have evaluated the efficacy of DVM DermCaps@. Depending on the study,
significant improvement was seen in 11% to 27% of dogs. Additionally, a double-blinded,
placebo-controlled study using high doses of marine fish oils (180 mg EPA and 120 mg DHA per
40 # body weight) has been published. In this study, treated dogs had significantly less pruritus
and alopecia, and significantly better hair coat quality than placebo-treated dogs.
‘Some diets have been fortified with essential fatty acids. These include Eukanuba Response
Formula (FP) and Science Diet Sensitive Skin, Since these diets have such high levels of fatty
acids, additional supplementation is unnecessary. Essential fatty acids must be incorporated into
the cell membrane before they can effect a change in the inflammatory cascade, so it may take
Up to eight weeks before improvement is noted.
Side effects due to fatty acid supplements are rare, but may include pancreatitis, weight gain,
diarthea, flatulence, and fish-breath. In addition, high doses of fatty acids may affect platelet
aggregation, so use in dogs with known coagulation problems is contraindicated.
Misoprostel
Prostaglandin E; (PGE;) has been shown to inhibit the late-phase reaction (LPR), but not the
immediate reaction to intradermally injected allergens in atopic people. This inhibition is the result
of decreased eosinophil chemotaxis and survival. in addition, histamine release from basophils
‘and mast cells is also inhibited by misoprostel. In a blinded, placebo-controlled study of 20 atopic
dogs, misoprostel resulted in a significant reduction in lesional and pruritus scores. Dogs were
treated with § mgc/kg, orally, three times daily for three weeks. The median reduction in lesional
‘and pruritus scores was about 30%. The drug was well tolerated by all patients, with only one
‘owner reporting intermittant (but tolerable) diarrhea during the course of the study. This drug
provides moderate relief of pruritus in some atopic dogs, but probably gets very little use due to
Its high cost.
Pentoxifylline
Pentoxifyline (PTX) is @ phosphodiesterase inhibitor with muifiple immune modulating
effects. Its use in human medicine is primarily for circulatory problems. However, its effects on
the immune system have resulted in its evaluation for treatment of contact allergy and atopic
dermatitis in the dog. In a small, blinded, placebo controlled study, PTX was used in dogs with
‘atopic dermatitis. Dogs were given 10 mgkkg twice dally during the study. A significant reduction
in pruritus and erythema was seen in treated dogs. The half-ife of this drug is extremely short in
the dog, so the authors of the study have suggested more frequent administration (three times
dally). In addition, PTX has been evaluated for treatment of canine familial dermatomyositis at
higher doses (20-25 mg/kg twice daily). In my practice, | typically recommend trying PTX at 10-
20 mg/kg twice daily for atopic dogs.
Corticosteroids
Corticosteroids have long been a standard therapy for allergies in the dog. Corticosteroids work
primarily by gene repression, which prevents the activation of many immune cells involved in the
allergic response. These drugs also decrease the conversion of membrane phospholipids into
arachidonic acid (AA). With decreased AA, there is a reduction in the secretion of inflammatory
mediators of the cyclooxygenase and lipoxygenase pathways.
Despite common use, there are relatively few controlled studies evaluating the efficacy of
corticosteroids in the treatment of canine allergies. In one study, atopic dogs treated with
prednisolone at 0.5mg/kg/day had a median reduction in pruritus scores by 81%. In another
study, 57% of dogs treated with prednisolone (0.4 mg/kg/day) had a “good to excellent” reduction
in pruritus, while 77% of dogs treated with prednisolone plus antihistamine had a good to
excellent response.
‘When using corticosteroids for treatment of AD, | generally recommend using prednisone at 5
mab once daily for 7 days, then 0.25 mgllb once daily for 7 days, then 0.25 mgjlb every other
day.
The acute side effects of corticosteroids are well known, and include polyuria, polydipsia,
polyphagia, and excessive panting. If these adverse effects are excessive, methylprednisolone
(starting at 0.4mg/ib daily) or another corticosteroid with fewer mineralocorticoid effects can be
utilized,
Chronic use of corticosteroids can lead to iatrogenic Cushing's disease, pancreatitis,
gastrointestinal ulceration, opportunistic infections (especially UTI), obesity, and musculoskeletal
Problems (muscle wasting, CCR). Dogs should be treated with the lowest effective dose
necessary to control symptoms. Concurrent use of antihistamines and topical therapy may have
a “steroid-sparing” effect. When chronic use is necessary, owners should be advised that every
other day dosing is always safer than daily dosing. There is no pharmacologic advantage to
Using injectable corticosteroids over oral preparations. Due to the increased likeliood of adverse
effects, the use of injectable, long-acting corticosteroid formulations is not recommended for the
treatment of canine AD.
Allergen-specific immunotherapy
‘Allergen-specific immunotherapy (ASIT) is a safe and effective nonsteroidal therapy for dogs with
atopic dermatitis. Most studies indicate that 65-70% of patients will show significant (>50%)
improvement with immunotherapy. When possible, intradermal testing should be utilized in order
to formulate ASIT. It is important for owners to realize that ASIT is a chronic therapy for atopy,
and it may take 3-6 months or longer to see a significant reduction in symptoms. In order for
immunotherapy to be effective, control of secondary infections and concurrent allergies is critical
In addition, frequent follow-up (by phone or in person) is necessary. A recent study has shown
that immunotherapy is most successful in those dogs whose owners have frequent contact with
their dermatologist. In my practice, immunotherapy schedules are individualized to each patient
depending on the response to therapy. A cookbook approach to immunotherapy is less likely to
be effective.
Cyclosporine for Treatment of Canine Atopy
Cyclosporine (CsA) is an immunosuppressive drug originally developed to prevent
human organ transplant rejection. Modified cyclosporine was developed to have more reliable
absorption and greater bioavalability following oral dosing. CsA has been used in the
‘management of human atopic dermatitis, and recent studies have demonstrated that CsA is an
effective therapy for canine atopic dermatitis (AD), as well
The recommended dose for treatment of canine AD is 5 mg/kg, once daily, using the
‘modified formulation of CsA (Atopica®, Novartis). In some dogs, the dose can be reduced to
every other day after 4-8 weeks. With chronic use, twice weekly dosing may be effective for some
patients. The most common side effects include vomiting and diarthea. These side effects are
usually transient, and resolve spontaneously within a few days. Cutaneous flushing, excessive
panting, hepatotoxicity, renal changes, gingival hyperplasia, muscle tremors, and secondary
infections have been reported on rare occasions. People taking CsA for long periods of time have
occasionally developed malignancies. While this has not been reported in the dog, CsA should
not be used in dogs with a history of malignancy. | recommend doing a CBC and serum
chemistry panel prior to, and 30 days after initiating therapy. If no abnormalities are seen,
repeating these tests every 3-6 months may be prudent. Urinalysis and/or urine cultures should
be done 1-2 times yearly to monitor for bacterial cystitis. While some have advocated measuring
serum levels of CsA, | have not found this to be useful or necessary. Serum levels do not
necessarily correspond to a clinical reduction in pruritus. | make adjustments in the dose regimen
based on the patient's clinical signs, rather than serum levels. Many drugs, including
ketoconazole and cimetidine may interact with CsA, so caution is recommended when using CsA
with other drugs. Modified CsA, as Atopica®, has recently been FDA-approved for the treatment
of atopic dermatitis in the dog.
While CsA appears to be a promising new treatment, the principles of managing canine AD have
not changed. Other pruritic diseases (sarcoptic mange, FAD, food hypersensitivity) must be
effectively ruled out or managed. In addition, secondary infections need to be controlled
Allergen-specific immunotherapy is still the only therapy that directly addresses the cause of
canine AD.
Chronic Management of the Atopic Dog
Client education is one of the most important aspects of managing an atopic dog. Owners must
understand that AD cannot be “cured.” Long-term management with drugs that are safe for the
patient is the goal of therapy.
For those patients with relatively short seasons, aggressive therapy is often unnecessary. As
‘always, secondary infections should be managed. In addition, nonspecific therapies, such as
antihistamines and corticosteroids should be utlized. | usually recommend a combination of
topical therapy, antihistamines, and a short course of oral corticosteroids. Depending on the
length of the patient's allergy season and/or adverse effects to corticosteroids, cyclosporine could
be incorporated into therapy for distinctly seasonal patients.
In those patients with lengthy or nonseasonal symptoms, ASIT is indicated. ASIT is typically
utlized in combination with other therapies. | commonly have owners bathing regularly, utilizing
systemic medications, and using ASIT in order to manage their pruritic dogs. Both corticosteroids
and cyclosporine can be used on conjunction with ASIT. Management of concurrent allergies
(fiea and food allergy) is also necessary.
Even the most successfully managed atopic dog will have occasional flares. When these flares
‘occur, look first for the presence of secondary infection and flea exposure. If pruritus persists
‘once these problems are addressed, then try adding in concurrent therapies in order to keep the
patient comfortable.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Basic Life Support: Participant's ManualDocument122 pagesBasic Life Support: Participant's Manualelkyec0% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Vaccines, Social Media and The Public HealthDocument16 pagesVaccines, Social Media and The Public HealthChinmay KalakondaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Maternal and Child Nursing - Student - HandoutsDocument40 pagesMaternal and Child Nursing - Student - HandoutsPaulAliboghaNo ratings yet
- Learn For Help Earn For Learn : Formative Assessment For CBT&A Level-4Document5 pagesLearn For Help Earn For Learn : Formative Assessment For CBT&A Level-4সত্য চন্দ্র প্রামাণিক100% (1)
- Admission LetterDocument2 pagesAdmission LetterzeenahNo ratings yet
- Moved To TearsDocument8 pagesMoved To TearsLuzia PeraNo ratings yet
- Concept Map PedsDocument6 pagesConcept Map Pedsapi-546398486No ratings yet
- Kuisioner Chandra AsriDocument8 pagesKuisioner Chandra AsriTumbal PogoNo ratings yet
- Jacobsen H100Document44 pagesJacobsen H100Lady Marcela RodriguezNo ratings yet
- The Humanistic School of PsychologyDocument17 pagesThe Humanistic School of PsychologyJohnNo ratings yet
- ADC Standard OSCE Communication Marking RubricDocument2 pagesADC Standard OSCE Communication Marking RubricAshik M RasheedNo ratings yet
- Ethical Issues Arising From PandemicDocument6 pagesEthical Issues Arising From PandemicmarengbibNo ratings yet
- MCP 02@3Document150 pagesMCP 02@3Julie ann CamitanNo ratings yet
- Introduction Disaster NursingDocument11 pagesIntroduction Disaster NursingydtrgnNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument8 pagesChronic Obstructive Pulmonary DiseaseGeozel VivienneNo ratings yet
- FV FOS8 Module6Document8 pagesFV FOS8 Module6EsNo ratings yet
- Kontratransfer U Psihoterapiji Poremećaja Ličnosti Ili Kako Biti Šaptač Ljudima?Document21 pagesKontratransfer U Psihoterapiji Poremećaja Ličnosti Ili Kako Biti Šaptač Ljudima?Iva LučićNo ratings yet
- Introduction To Human Resource ManagementDocument5 pagesIntroduction To Human Resource ManagementLianne VonNo ratings yet
- Datasheet: Rigid Box Seals - Fire OnlyDocument2 pagesDatasheet: Rigid Box Seals - Fire OnlyEdgar ArdinazoNo ratings yet
- Philips Pacing PadsDocument12 pagesPhilips Pacing PadsGeneral Health CareNo ratings yet
- Beverly MuseDocument1 pageBeverly MuseEmilioOsorioNo ratings yet
- HPM and H and B - Daryl E. CandoDocument41 pagesHPM and H and B - Daryl E. CandoDaryl CandoNo ratings yet
- Witnesses Claim Babys Death Must Be HomicideDocument2 pagesWitnesses Claim Babys Death Must Be Homicideapi-3750354No ratings yet
- Tarife Servicii Medicale Amb 2Document8 pagesTarife Servicii Medicale Amb 2Ioana RaduNo ratings yet
- DoPT Guidelines On Treatment - Regularization of Hospitalization - Quarantine Period During COVID 19 PandemicDocument2 pagesDoPT Guidelines On Treatment - Regularization of Hospitalization - Quarantine Period During COVID 19 PandemictapansNo ratings yet
- Project Management Theory and Practice - MBA 7023Document30 pagesProject Management Theory and Practice - MBA 7023Tharshi100% (1)
- Practice Occupational Health & Safety ProceduresDocument37 pagesPractice Occupational Health & Safety ProceduresEgghead YTCNo ratings yet
- Weight Loss PDFDocument72 pagesWeight Loss PDFMarilda QuiassataNo ratings yet
- The Art of Letting Go Stop Overthinking Stop Negative Spirals and Find Emotional Freedom The Path To Calm Book 13Document170 pagesThe Art of Letting Go Stop Overthinking Stop Negative Spirals and Find Emotional Freedom The Path To Calm Book 13Damayanti SinagaNo ratings yet
- Betty - Speech On Girl Child Education in Uganda August 2017Document9 pagesBetty - Speech On Girl Child Education in Uganda August 2017dennisNo ratings yet