Professional Documents
Culture Documents
Ophtha Reviewer
Uploaded by
Toni Sy Encinares0 ratings0% found this document useful (0 votes)
44 views3 pagesOphtha Reviewer
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentOphtha Reviewer
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
44 views3 pagesOphtha Reviewer
Uploaded by
Toni Sy EncinaresOphtha Reviewer
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Pain, Redness, & Swelling Layers of Cornea
HORDEOLUM A Anterior Epithelium
INTERNAL EXTERNAL B Bowman’s Membrane
Meibomian glands Sty/gland of Zeis C Corneal Stroma
Skin or conjunctival Skin D Descemet’s Membrane
surface E Endothelium
Vertical incison Horizontal incision
Layers of Retina
PTERYGIUM PINGUECULA Bruch’s membrane
Crosses the limbus Yellow nodules at nasal Pigment epithelium
side of cornea Rods and cones
UV, drying & windy Does not cross the cornea External limiting membrane
environment Outer nuclear layer
Hyaline + elastic tx Hyaline + elastic tx Outer plexiform layer
Inner nuclear layer
Tx: excision with No treatment or weak
Inner plexiform layer
conjunctival autografts topical steroids
Ganglion cell layer
(prednisolone 0.12%) or
Nerve fiber layer
topical NSAIDs
Internal limiting membrane
MYOPIC HYPEROPIC
HTN Retinopathy
Concave lens Convex lens Grade
0 No visible changes
1 Vascular attenuation
2 Grade 1 + AV nicking
3 Grade 2 + retinal edema, cotton wool spots,
flame hemorrhages
4 Grade 3 + optic disc edema, macular star
Types of Cataract Surgery
Diabetic Retinopathy Classification
ECCE (Extracapsular Cataract Extraction)
1. Non-proliferative Retinopathy
o Phacoemulsification
- microaneurysms
o MSICS (manual sutureless small
- flame-shaped hemorrhages
incision cataract surgery)
- cotton wool spots
ICCE (Intracapsular Cataract Extraction)
- IRMA
Phacofragmentation
2. Maculopathy
Signs of Glaucoma
- Focal or diffuse retinal thickening or edema
enlargement of optic disc cup with disc
- Hard exudates
pallor in area of cupping; “bean pot cup”
nasal displacement of vessels 3. Proliferative Retinopathy
cup:disc > 0.5 - New vessels on optic disk (NUD)
increased intraocular pressure
atrophy of retinal nerve fiber layer
fixed dilated pupils
1st line sa Bailey-Love
Symptoms of Glaucoma - HZVDS
visual field loss 1st line sa Snellen
eye pain - E
haloes Goldmann Applanation Tonometry
nausea and vomiting - gold standard to measure pressure
Management of chemical injury
Types of Glaucoma
- irrigation
OPEN ANGLE ANGLE CLOSURE
Ptosis
Asymptomatic, Sudden onset
progressive, bilateral visual - drooping of the superior eyelid
loss Lamina papyracea
IOP < 21 mmHg IOP >60-80 mmHg - weakest bone of orbit
Degenerative process in Occluded trabecular
trabecular meshwork & meshwork
decrease in aqueous
drainage
1. Draw and label the anterior and posterior chambers of the eye disk or field changes vomiting. Other findings
associated with include increased IOP, a
elevated IOP, a shallow anterior
normal-appearing chamber, a steamy
open anterior chamber cornea, a fixed, and
angle, and no other moderately dilated pupil,
reason for IOP and ciliary injection.
elevation.
Treatment Trabeculectomy – OPHTHALMIC
good option in patients EMERGENCY!
who progress despite Treatment is initially
medical treatment directed at reducing the
IOP. IV and oral
acetazolamide (along with
topical agents such as beta-
blockers & apraclonidine, and, if
necessary, hyperosmotic agents)
will usually reduce the IOP.
Pilocarpine 2% should be
instilled ½ hour after
commencement of treatment, by
2. Draw the excretory portion of the lacrimal system which time reduction of iris
ischemia and lowering of IOP
allow the sphincter papillae to
respond to the drug.
Topical steroids may also
be used to reduce secondary
inflammation.
Once the IOP is controlled,
laser peripheral
iridotomy should be
undertaken to form a permanent
connection between the anterior
and posterior chambers, thus
preventing recurrence of the iris
bombe. This is most often done
neodymium:YAG
with the
laser. Surgical
peripheral iridectomy is
the conventional treatment if laser
treatment is unsuccessful, but
Tears drain from the lacrimal lake via the upper and lower puncta and ALPI may be performed. The
canaliculi to the lacrimal sac, which lies in the lacrimal fossa. The fellow eye should always undergo
nasolacrimal duct continues downward from the sac and opens into the prophylactic laser
inferior meatus of the nasal cavity, lateral to the inferior turbinate. iridotomy.
Tears are directed into the puncta by capillary attraction & gravity and by the blinking action of Prognosis Without treatment, If treatment is delayed,
the eyelids. The combined forces of capillary attraction in the canaliculi, gravity, and the
pumping action of Horner’s muscle, which is an extension of the orbicularis oculi muscle to a
may progress to the peripheral iris may
point behind the lacrimal sac, all tend to continue the flow of tears down the nasolacrimal duct complete blindness. If adhere to the trabecular
into the nose (page 18). anti-glaucoma drops meshwork (anterior
control the IOP in an synechiae), producing
3. Differentiate open and closed angle glaucoma in terms of eye that suffered irreversible occlusion of
pathophysiology, clinical manifestation, treatment (medical, laser, extensive the anterior chamber
surgical), & prognosis (page 222) glaucomatous angle requiring surgery.
Primary open-angle ACUTE angle-closure damage, the Optic nerve damage is
(page 232) prognosis is good. common.
Pathophysiolo Degenerative process Elevation of intraocular When the process is
gy in the trabecular pressure is a detected early, most
meshwork, including consequence of glaucoma patients can
deposition of obstruction of aqueous be successfully
extracellular material outflow by occlusion of managed medically.
within the canal. The the trabecular meshwork
consequence is a by the peripheral iris. 4. Mom has Open angle glaucoma. What is your advice to her
reduction in aqueous Acute angle closure children? What age should you start screening?
drainage leading to a (“acute glaucoma”) The major problem in detection of primary open-angle glaucoma is the
rise in intraocular occurs when sufficient absence of symptoms until relatively late in the disease. When patient
pressure. iris bombe develops to first notice field loss, substantial optic nerve damage has already
cause occlusion of the occurred. If treatment is to be successful, it must be started early in
anterior chamber angle the disease, and this depends on an active screening program. At
by the peripheral iris. present, it is necessary to rely for early diagnosis predominantly on
Clinical Absence of symptoms Sudden onset of visual regular ophthalmic assessment of first-degree relatives of affected
manifestation until relatively late in loss accompanied by individuals. Age?
the disease. excruciating pain, halos,
Glaucomatous optic and nausea and
5. What is the accommodative power of the eye? Discuss the
physiology of this phenomenon (page 405?)
The eye changes refractive power to focus on near objects by a
process called accommodation. Contraction of the ciliary muscle
results in thickening and increased curvature of the lens, probably due
to relaxation of the lens capsule.
6. Differentiate types of conjunctivitis (cause, treatment, clinical manifestations). Page 83
VIRAL BACTERIAL CHLAMYDIAL ALLERGIC
CAUSE Hyperacute/purulent – N
gonnorhea, Neisseria kochiim N
meningitides
Acute mucopurulent/ catarrhal –
“pinkeye”; S pneumonia, H.
aegyptocus
CLINICAL Bilateral irritation and injection,
MANIFESTATI purulent exudate with sticky lids on
ONS waking, and occasionally lid edema.
Infection usually starts in one eye
and may be spread to the eye by
direct contact form the hands. It
may be spread from one to another
by fomites.
TREATMENT
7. Clinical manifestation of epithelial and stromal herpetic keratitis
(page 121?)
Epithelial Keratitis – the epithelial changes vary widely from simple
edema and vacuolation to minute erosions, filament formation, partial
keratinization, etc. The lesions vary also in their location on the cornea.
Types: see page 121
Stromal Keratitis – accumulation of inflammatory cells; edema
manifested as corneal thickening, opacification, or scarring; “melting”
or necrosis, which may lead to thinning or perforation; and
vascularization.
You might also like
- CNMC Eye OSPE Problems With SolutionsDocument26 pagesCNMC Eye OSPE Problems With SolutionsShahbaz AAnsariNo ratings yet
- part1Document15 pagespart1solimanmahmoudaNo ratings yet
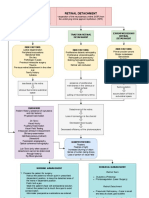
- Retinal Detachment: Traction Retinal Detachment Rhegmatogenous Detachment Exudative/Serous Retinal DetachmentDocument3 pagesRetinal Detachment: Traction Retinal Detachment Rhegmatogenous Detachment Exudative/Serous Retinal DetachmentJordz Placi100% (1)
- Care For Patients With Alteration in Perception and CoordinationDocument12 pagesCare For Patients With Alteration in Perception and Coordinationevlujtrep9690100% (1)
- Red EyeDocument54 pagesRed EyeT786 kharNo ratings yet
- Glaucoma Diagnosis and TreatmentDocument47 pagesGlaucoma Diagnosis and Treatmentnurul ramadhiniNo ratings yet
- Post Test JWB NCLDocument12 pagesPost Test JWB NCLSummer SnowNo ratings yet
- Guide to Managing Common Ocular Trauma InjuriesDocument50 pagesGuide to Managing Common Ocular Trauma Injuriesaditya brahmantio sujakaNo ratings yet
- عملي السليداتDocument92 pagesعملي السليداتSandyDavidNo ratings yet
- 10 Lids and Lashes 2016Document13 pages10 Lids and Lashes 2016willemlrouxNo ratings yet
- Corneal Dystrophies: Retinal DetachmentDocument5 pagesCorneal Dystrophies: Retinal DetachmentCake ManNo ratings yet
- Anatomy & Degenerations of Peripheral RetinaDocument29 pagesAnatomy & Degenerations of Peripheral RetinaNeelam Khatwani100% (1)
- SOPS For Blunt Trauma02Document2 pagesSOPS For Blunt Trauma02jawad awanNo ratings yet
- Tatalaksana GlaukomaDocument53 pagesTatalaksana GlaukomaVeronika Marampa AllolinggiNo ratings yet
- Angle Closure GlaucomaDocument21 pagesAngle Closure Glaucomasri sinagaNo ratings yet
- EGurukul - Uveitis and Uveal TractDocument10 pagesEGurukul - Uveitis and Uveal TractOscar Daniel MendezNo ratings yet
- Glaucoma 2 Lecture PACG MBBS BY Prof Munim SuriDocument28 pagesGlaucoma 2 Lecture PACG MBBS BY Prof Munim SuriMunim SuriNo ratings yet
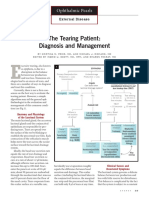
- The Tearing Patient: Diagnosis and Management: Ophthalmic PearlsDocument3 pagesThe Tearing Patient: Diagnosis and Management: Ophthalmic PearlsAnonymous otk8ohj9No ratings yet
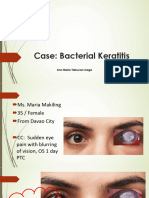
- Case Bacterial KeratitisDocument44 pagesCase Bacterial KeratitisPagolu BavyaNo ratings yet
- ENT Trans Disorders of The External EarDocument4 pagesENT Trans Disorders of The External EarJared Ezrach Cacal SanidadNo ratings yet
- 27a. Retinal Disease 1Document44 pages27a. Retinal Disease 1Aa SsNo ratings yet
- Retinal Diseases George Pile, MD: RetinaDocument5 pagesRetinal Diseases George Pile, MD: RetinaPrincess Cate MercadoNo ratings yet
- Eyelids and Lacrimal ApparatusDocument6 pagesEyelids and Lacrimal Apparatussarguss14No ratings yet
- Ectropion and Corneal Ulcer CareDocument31 pagesEctropion and Corneal Ulcer CareapriliaNo ratings yet
- Surgery B PracticalDocument12 pagesSurgery B PracticalMohamed KhaledNo ratings yet
- GlaucomaDocument1 pageGlaucomashakyaNo ratings yet
- Materi Bimbingan Kepaniteraan Klinik Ilmu Penyakit Mata: No Pembimbing Topik Sub TopikDocument2 pagesMateri Bimbingan Kepaniteraan Klinik Ilmu Penyakit Mata: No Pembimbing Topik Sub TopikRizka ChairaniNo ratings yet
- Occupational Hazards in Dental, Textile Industry and MechanicDocument20 pagesOccupational Hazards in Dental, Textile Industry and MechanicimtahifNo ratings yet
- Referat Acute Liver FailureDocument124 pagesReferat Acute Liver FailurepanduNo ratings yet
- Medical History Taking Project Ppt-Converted NoDocument17 pagesMedical History Taking Project Ppt-Converted Noabdul qayyumNo ratings yet
- Cataract Surgery Complications GuideDocument130 pagesCataract Surgery Complications GuideMauVeeNo ratings yet
- Trauma MataDocument57 pagesTrauma MataFatmala Umi MaisarahNo ratings yet
- Glaucoma: Camille N. LibrandaDocument35 pagesGlaucoma: Camille N. LibrandaCamilleNo ratings yet
- Corneal Dystrophies, Contact Lenses, and Retinal Detachment GuideDocument6 pagesCorneal Dystrophies, Contact Lenses, and Retinal Detachment GuideMarissa AsimNo ratings yet
- Roughtly: LayerDocument18 pagesRoughtly: LayerS SwaminathanNo ratings yet
- Ocular Emergencies GuideDocument7 pagesOcular Emergencies GuidePatricia ManaliliNo ratings yet
- 8a) Chronic DacryocystitisDocument5 pages8a) Chronic DacryocystitisDasNo ratings yet
- White dot syndromes: causes, signs and treatmentDocument43 pagesWhite dot syndromes: causes, signs and treatmentJasmine MinoNo ratings yet
- Common Eye Diseases 2022Document33 pagesCommon Eye Diseases 2022Shia LevyNo ratings yet
- Brain AbscessDocument3 pagesBrain AbscessAndrew JavierNo ratings yet
- EGurukul GlaucomaDocument15 pagesEGurukul GlaucomaOscar Daniel Mendez100% (1)
- Keratoconjunctivitis Sicca: in DogsDocument8 pagesKeratoconjunctivitis Sicca: in DogsGABRIELA VERGARA PEREZNo ratings yet
- Opt Halm OlogyDocument1 pageOpt Halm OlogyAnonymous q16bp7No ratings yet
- Ophthalmology EmergenciesDocument60 pagesOphthalmology Emergenciesasraf amirullahNo ratings yet
- The Acute Painful Red Eye: History of Presenting Complaint - The Time and Speed of OnsetDocument4 pagesThe Acute Painful Red Eye: History of Presenting Complaint - The Time and Speed of Onsetleigh_zaliNo ratings yet
- Ocular EmergencyDocument86 pagesOcular EmergencyMohammadNo ratings yet
- KeratoconusssDocument15 pagesKeratoconusssnurfatminsari almaidinNo ratings yet
- Orbita, Palpebra & Sistem Lakrimal: Dr. I Gede Suparta SP.MDocument43 pagesOrbita, Palpebra & Sistem Lakrimal: Dr. I Gede Suparta SP.Mbasyit bafadhalNo ratings yet
- Retinal Detachment SlideDocument54 pagesRetinal Detachment SlideHerin NataliaNo ratings yet
- Expansion With Excision: George Clooney Nasal Dorsum Length of Eye Angle of Mandible/jawDocument4 pagesExpansion With Excision: George Clooney Nasal Dorsum Length of Eye Angle of Mandible/jawChristine Evan HoNo ratings yet
- Dermatology Revision E6.5 'Document35 pagesDermatology Revision E6.5 'Riya SharmaNo ratings yet
- Fundamentals of OpthalmologyDocument4 pagesFundamentals of OpthalmologyMuhammad HaziqNo ratings yet
- Pediatrics2 Se4 High2Document23 pagesPediatrics2 Se4 High2Daryl Gay NanoNo ratings yet
- Papiledema 3Document27 pagesPapiledema 3nellieauthorNo ratings yet
- Opthalmology Visuals New PDF-1Document100 pagesOpthalmology Visuals New PDF-1singh0% (1)
- Eyes Lecture 2Document4 pagesEyes Lecture 2Rue Cheng MaNo ratings yet
- ConjunctivitisDocument4 pagesConjunctivitisKumar ShivamNo ratings yet
- Clinical Ophthalmology for UndergraduatesFrom EverandClinical Ophthalmology for UndergraduatesRating: 4 out of 5 stars4/5 (5)
- ASEAN Stability GuidelineDocument37 pagesASEAN Stability GuidelinevarizzzNo ratings yet
- Mock Claim Form 2Document2 pagesMock Claim Form 2Toni Sy EncinaresNo ratings yet
- Qualitative Test For Amino AcidsDocument1 pageQualitative Test For Amino AcidsToni Sy EncinaresNo ratings yet
- PhilHealth ClaimForm2 Guidelines PDFDocument8 pagesPhilHealth ClaimForm2 Guidelines PDFToni Sy EncinaresNo ratings yet
- Extraction of Lipids From Chicken Egg YolkDocument5 pagesExtraction of Lipids From Chicken Egg YolkToni Sy Encinares100% (2)
- Pharmacology Types of ReceptorsDocument2 pagesPharmacology Types of ReceptorsToni Sy EncinaresNo ratings yet
- Toxicology Qualitative TestDocument5 pagesToxicology Qualitative TestToni Sy EncinaresNo ratings yet
- Effect of PH On Invertase ActivityDocument4 pagesEffect of PH On Invertase ActivityToni Sy Encinares100% (2)
- Sythesization and Purification of Acetanilide by Acetylation and Re CrystallizationDocument4 pagesSythesization and Purification of Acetanilide by Acetylation and Re CrystallizationToni Sy EncinaresNo ratings yet
- PCARE Calculation NotesDocument10 pagesPCARE Calculation NotesToni Sy EncinaresNo ratings yet
- Determination of Ethanol Content From Ginebra Gin by Fractional DistillationDocument4 pagesDetermination of Ethanol Content From Ginebra Gin by Fractional DistillationToni Sy EncinaresNo ratings yet
- NCP&SOAPIEDocument4 pagesNCP&SOAPIEMica OmotsosircNo ratings yet
- Cosmecueticals Mod1Document35 pagesCosmecueticals Mod1Top 10No ratings yet
- Continued Sports Activity, Using A Pain - Monitoring Model, During Rehabilitation in Patients With Achilles TendinopathyDocument10 pagesContinued Sports Activity, Using A Pain - Monitoring Model, During Rehabilitation in Patients With Achilles TendinopathyMichele MarengoNo ratings yet
- Drug study overviewDocument3 pagesDrug study overvieweliza luisNo ratings yet
- Fordyce GranuleDocument3 pagesFordyce GranulenediaNo ratings yet
- Abu Dhabi Plan Drug ListDocument45 pagesAbu Dhabi Plan Drug ListicebreakNo ratings yet
- Danile Fast BrochureDocument2 pagesDanile Fast BrochureLito Dela PeñaNo ratings yet
- Clinical Nutrition General BrochureDocument40 pagesClinical Nutrition General Brochureds.neetaNo ratings yet
- Factors Affecting Body Alignment & Activity 1. 2. 3.Document5 pagesFactors Affecting Body Alignment & Activity 1. 2. 3.LE-JEAN BRENA100% (2)
- Ketamine Administration Guideline 080114 راهنماDocument14 pagesKetamine Administration Guideline 080114 راهنماBabak AsliNo ratings yet
- Septage FAQ Brochure - EnglishDocument2 pagesSeptage FAQ Brochure - EnglishMeghan EbuezaNo ratings yet
- Shell Tellus S2 MX 68: Safety Data SheetDocument16 pagesShell Tellus S2 MX 68: Safety Data SheettinaseNo ratings yet
- cp201007 Spotlight Febuxostat-261Document2 pagescp201007 Spotlight Febuxostat-261Rafaeyza Al KarimNo ratings yet
- Ethics Documents For Physio TherapistsDocument21 pagesEthics Documents For Physio TherapistsDeeksha JainNo ratings yet
- Elyse Torres Resume NowDocument2 pagesElyse Torres Resume Nowapi-395806896No ratings yet
- Ocular InjuryDocument46 pagesOcular InjurysnyNo ratings yet
- Bedbug Propoxur LabelDocument3 pagesBedbug Propoxur LabeluncleadolphNo ratings yet
- Vacuum PumpDocument90 pagesVacuum PumpEnrique S OcampoNo ratings yet
- Dipyridamole Tablets Leaflet SectionsDocument1 pageDipyridamole Tablets Leaflet SectionsAat Prayoga MuhtarNo ratings yet
- Resume March2023Document2 pagesResume March2023api-625227498No ratings yet
- CBT of DepressionDocument15 pagesCBT of DepressionRidwan MuttaqinNo ratings yet
- Complementary and Alternative TherapyDocument16 pagesComplementary and Alternative TherapyDevangi Bhorsat100% (1)
- Sample EssayDocument9 pagesSample EssayBrian SrotaNo ratings yet
- State Apple Health Handbook PDFDocument28 pagesState Apple Health Handbook PDFRohan KunwerNo ratings yet
- The Efficacy of Mechanical Vibration Analgesia For Relief of Heel Stick Pain in NeonatesDocument10 pagesThe Efficacy of Mechanical Vibration Analgesia For Relief of Heel Stick Pain in NeonatesmustafasacarNo ratings yet
- Effect of Micronutrients and Organics on Baby Corn-Chickpea YieldDocument3 pagesEffect of Micronutrients and Organics on Baby Corn-Chickpea YieldRitesh MistryNo ratings yet
- Pterygium: Surgical Techniques and ChoicesDocument2 pagesPterygium: Surgical Techniques and ChoicesJohny Marquez TrochezNo ratings yet
- Ayurvedic treatment of anemia in pregnancyDocument6 pagesAyurvedic treatment of anemia in pregnancypooja huilgolNo ratings yet
- 1-Collection, Storage and Transportataion of MicrobiologicalDocument49 pages1-Collection, Storage and Transportataion of MicrobiologicalSummi NizNo ratings yet
- Manual Usuario (Enghlis) Babylog 8000 PlusDocument172 pagesManual Usuario (Enghlis) Babylog 8000 PlusJuan Carlos LopezNo ratings yet