Professional Documents
Culture Documents
In Search of Excellence
Uploaded by
Asare GeorgeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
In Search of Excellence
Uploaded by
Asare GeorgeCopyright:
Available Formats
822 EDITORIAL
Excellence in emergency doctors 7. Analgesia and conscious sedation:
....................................................................................... Managing pain is a fundamental
part of our work. Although it
In search of excellence
becomes a heart sink problem
when faced with the frequent flyer
attendee who has intractable
G Hughes chronic pain that even the pain
clinic has given up on, for the rest,
................................................................................... speedy and appropriate analgesia is
critical. Whether we give it orally,
I
n Search Of Excellence, by Tom Peters Knowledge of basic ventilators and rectally, intranasally, parenterally
and Robert Waterman,1 published in ventilation modalities is a prere- or via a regional block, we should
1982, remains one of the biggest quisite too. offer the service with expertise and
selling and most widely read business timeliness. Conscious sedation for
3. Triage and major incident manage-
books ever. It was then, and still is, minor procedures, with a benzo-
ment: This is core business. As with
touted as a seminal text for those trying diazepine and an opiate or a
resuscitation, it is part of our
to improve systems and deliver quality neuroleptic, should have a safety
armamentarium. These are not
to the public, mainly in the context of record second to none.
easy skills to acquire. We can be
business. I was advised to read it on a proud of our abilities in this speci- 8. Communication: For many reasons,
senior registrar management course I alty, but we can always do it better. sadly one of them being medicole-
attended in 1989. It’s not a page-turning gal, our record keeping, be it
bodice-ripper. I didn’t finish it. I tried 4. Imaging: From time to time we will electronic or hard copy, needs to
hard. always need the skills of a radi- be faultless. We need to set an
I mention this because I came across it ologist to help us interpret films, example for everyone else. Our oral
the other day while perusing the shelves whatever the radiological modality. and written abilities to communi-
of the hospital library. Later that day I A skill we can be excellent at is the cate with each other in a depart-
discussed the book with a friend who use of diagnostic ultrasound in the ment, a hospital, our colleagues in
runs a successful business. He agreed that resuscitation room. Focused assess- the community and pre-hospital
it is still widely referenced in business and ment with sonography for trauma arenas and, last but not least, with
training seminars. He then asked me the scanning, searching for abdominal our patient and their carers should
killer question ‘‘what are you guys [emer- aortic aneurysms in the appropriate be exemplary.
gency doctors] excellent at?’’ He followed context and looking for a dilated 9. Acting rationally to the unexpected and
this up by asking ‘‘don’t you refer every- right ventricle (via an echocardio- unknown, thinking on our feet and
thing on to specialists?’’. I was well gram) in massive pulmonary embo- keeping calm in a crisis: What more is
behaved and refrained from pouring a lism can be core skills. Ultrasound there to say?
jug of water over him. also improves the safety of central
10. Empathy and compassion: Let’s show
So, what are we excellent at? By the cannulation via the internal jugular
to the patient and their carers that
nature of our work, we are generalists and route. It goes without saying that
we care. Among the hurly-burly of
are pretty good at many things, but what fracture recognition on plain film is
our work, we must remember that
are we excellent at? In an era that revels a key skill.
there is more to what we do than
in having ‘‘top-10’’ lists for virtually 5. Electrocardiograms: After measuring intellectual thought, professional
everything, here are 10 things we are or vital signs, the glucose level, and achievement and diagnostic preci-
should be excellent at. I’m sure there will carrying out urine analysis, record- sion. In an age driven by targets,
be disagreement with my selection. ing an electrocardiogram is one of instant gratification and material-
our most common investigations. ism, we need to recall why most of
1. Resuscitation: This is the ‘‘raison
d’etre’’ for our existence. If we In addition to recognising arrhyth- us entered this challengingly com-
don’t do this better than anyone mias, all degrees of heart block, pelling profession. Most of our
else, then we need to shut the shop and the various patterns seen in clientele come to us at a moment
and throw away the keys. (or mimicking) acute coronary of dire need. For those who die, the
Knowledge of protocols, ability to syndrome and oddities, such as J way we manage the early grief and
think 2–3 steps ahead in decision waves in hypothermia, we need to bereavement of their relatives and
making and excellent team leader- be good enough to pick up rare and friends is critical. Let’s maintain
ship should be par for the course. subtle abnormalities which can our humanity and compassion and
have a devastating outcome if protect their dignity.
2. Resuscitation procedures: Apart from
missed, such as long QT syndrome Emerg Med J 2006;23:822.
basics such as the correct way to
maintain an airway, cannulate, and tri-fascicular block. doi: 10.1136/emj.2006.041673
defibrillate and perform external 6. Wounds and soft tissue infections pro-
Correspondence to: Geoff Hughes, The
cardiac massage, we need to be blems: This is core business. In Emergency Department, Royal Adelaide
excellent at rapid sequence induc- addition to managing everyday pro- Hospital, North Terrace, Adelaide 5000,
tion and intubation, recognition blems with skill and precision, we Australia; cchdhb@yahoo.com
and management of the difficult need to promptly recognise occa-
Accepted 29 August 2006
airway, advanced cannulation (be sional conditions such as erythema
it central or peripheral, arterial or nodosum, necrotising fasciitis and Competing interests: None declared.
venous) and intercostal drain so forth. Our accuracy for appropri-
insertion. We need to perform to ate and timely referral to surgical REFERENCE
the same standard as our anaes- specialties for both wounds and 1 Peters T, Waterman R. In search of excellence.
thetic and intensivist colleagues. infections needs to be spot on. 1982.
www.emjonline.com
You might also like
- Occlusion Made EasyDocument225 pagesOcclusion Made Easydruzair00791% (22)
- What I Wish I Knew SoonerDocument3 pagesWhat I Wish I Knew SoonerJoao Joaquim Ferreira NetoNo ratings yet
- Emergency Medicine Exercises - 24-X-2022Document4 pagesEmergency Medicine Exercises - 24-X-2022LORA AEMPPI UTENo ratings yet
- Pearls of Glaucoma ManagementDocument469 pagesPearls of Glaucoma ManagementMacarena AlvarezNo ratings yet
- Orthodontic Learning Curve: A Journey We All MakeDocument2 pagesOrthodontic Learning Curve: A Journey We All MakeeltonNo ratings yet
- SPE 77509 Would You Know A Good Decision If You Saw One?Document11 pagesSPE 77509 Would You Know A Good Decision If You Saw One?saladinayubi1234No ratings yet
- RCEM Human Factors IBook v2Document41 pagesRCEM Human Factors IBook v2dr.gergely.halaszNo ratings yet
- Survey: OccasionalDocument4 pagesSurvey: OccasionalAlfonso LeeNo ratings yet
- Optimize Your Mind For AnalysisDocument8 pagesOptimize Your Mind For AnalysisZen TraderNo ratings yet
- Do No Harm by Henry Marsh ExtractDocument15 pagesDo No Harm by Henry Marsh ExtractAyu Hutami SyarifNo ratings yet
- Vital 971Document1 pageVital 971Celso FelipeNo ratings yet
- NURS - 4634 Transitions - Leadership Interviews & Reflection - Clinical Activity Name: DateDocument9 pagesNURS - 4634 Transitions - Leadership Interviews & Reflection - Clinical Activity Name: DateKaylee KippNo ratings yet
- Retreatmeant1 2 3Document15 pagesRetreatmeant1 2 3Alaa MadmoujNo ratings yet
- Pain Medicine A Case Based Learning Series The Spine 1St Edition Steven D Waldman Full ChapterDocument67 pagesPain Medicine A Case Based Learning Series The Spine 1St Edition Steven D Waldman Full Chapterethel.martin368100% (3)
- StreetThesis LieDetectionCogProcesses UCL2013 PDFDocument318 pagesStreetThesis LieDetectionCogProcesses UCL2013 PDFMihaiviorel87No ratings yet
- Carpel Tunnel ReleaseDocument14 pagesCarpel Tunnel ReleaseHadi SalimNo ratings yet
- Bad Spay DayDocument5 pagesBad Spay DayRizwanNo ratings yet
- Dissertation Michael MunzDocument7 pagesDissertation Michael MunzPayToWriteAPaperMinneapolis100% (1)
- Professional Portfolio - GenericDocument17 pagesProfessional Portfolio - GenericGracie S. VergaraNo ratings yet
- Jorgen Rasmussen - Provocative PDFDocument300 pagesJorgen Rasmussen - Provocative PDFDavidBailey100% (3)
- Habit Change Theory and PracticeDocument32 pagesHabit Change Theory and PracticeGeorgiaMaNo ratings yet
- Michael Grinder - Fundamentals of Group Dynamics (1998) (OCR)Document17 pagesMichael Grinder - Fundamentals of Group Dynamics (1998) (OCR)NeoFu26100% (1)
- Anil LaulDocument48 pagesAnil LaulYogesh BhardwajNo ratings yet
- Getting Dementia Care Right: What's Not Working and How It Can Change (EXCERPT)Document22 pagesGetting Dementia Care Right: What's Not Working and How It Can Change (EXCERPT)Health Professions Press, an imprint of Paul H. Brookes Publishing Co., Inc.No ratings yet
- The Power of Professional Closeness: A Guide to Taking a Holistic Approach to Your BusinessFrom EverandThe Power of Professional Closeness: A Guide to Taking a Holistic Approach to Your BusinessNo ratings yet
- UNIT 13 F.07 THE FILIPINO SURGEON Part 1 CLERKSHIP INTERNSHIP AND RESIDENCYDocument7 pagesUNIT 13 F.07 THE FILIPINO SURGEON Part 1 CLERKSHIP INTERNSHIP AND RESIDENCYCHYNNA ALBERTNo ratings yet
- Advanced Dementia Symptoms & Management - Part 1 Text Overview of VideoDocument4 pagesAdvanced Dementia Symptoms & Management - Part 1 Text Overview of VideoJayanti Ika siwiNo ratings yet
- Hoon - Medical First Aid HandoutDocument100 pagesHoon - Medical First Aid HandoutSaptarshi BasuNo ratings yet
- Surgical Metacognition: Smarter Decision-making for SurgeonsFrom EverandSurgical Metacognition: Smarter Decision-making for SurgeonsNo ratings yet
- 10 Steps 2019Document80 pages10 Steps 2019Jose Daniel Lomeli MorenoNo ratings yet
- RMH Cardiac AnaesthesiaDocument40 pagesRMH Cardiac Anaesthesiamarcelo100% (1)
- The Truth-Seeker's Handbook: A Science-Based GuideDocument53 pagesThe Truth-Seeker's Handbook: A Science-Based GuideJune Lyn100% (1)
- Second Edition: Understanding, Stopping, & Reversing Pattern Hair LossDocument28 pagesSecond Edition: Understanding, Stopping, & Reversing Pattern Hair LossDante404100% (1)
- Orion ManualDocument61 pagesOrion ManualLuis Fernando Ortiz ViñasNo ratings yet
- AENJ Clinical Tips Current Collection 2018Document18 pagesAENJ Clinical Tips Current Collection 2018Em Wahyu ArNo ratings yet
- The Auditor WW 108 1975Document7 pagesThe Auditor WW 108 1975Andreas GroßNo ratings yet
- Mayans 227Document14 pagesMayans 227OnenessNo ratings yet
- An Introduction - RCEM Induction - RCEMLearningDocument1 pageAn Introduction - RCEM Induction - RCEMLearningaoran zhangNo ratings yet
- 2003.5.2. Gastric SurgeryDocument59 pages2003.5.2. Gastric SurgeryMetric HawkNo ratings yet
- Revcrejv H 934y8 HrejndiuhidhvldsuvfdsvDocument10 pagesRevcrejv H 934y8 HrejndiuhidhvldsuvfdsvLuisa CruzNo ratings yet
- @enbook Self-Regulation and MindfulnessDocument197 pages@enbook Self-Regulation and MindfulnessGleyciane100% (3)
- Myofascial Release Literature ReviewDocument4 pagesMyofascial Release Literature Reviewafdttatoh100% (1)
- The CitadelDocument5 pagesThe Citadelamiry4390No ratings yet
- Craniotomy For Aneurysm Clipping Surgical Medi-CardDocument2 pagesCraniotomy For Aneurysm Clipping Surgical Medi-CardDr. Chaim B. ColenNo ratings yet
- The Power Behind Your Eyes: Improving Your Eyesight with Integrated Vision TherapyFrom EverandThe Power Behind Your Eyes: Improving Your Eyesight with Integrated Vision TherapyNo ratings yet
- So Much To Do : Volume Vii, Issue 6 St. Pat'S Day 2009Document4 pagesSo Much To Do : Volume Vii, Issue 6 St. Pat'S Day 2009Manuel Ferreira PTNo ratings yet
- Case StudyDocument4 pagesCase StudyThomasRasen Jake PattungNo ratings yet
- Occlusion Made EasyDocument225 pagesOcclusion Made EasyTurhan Didinen100% (1)
- REWIRE for SUCCESS: An easy guide for using neuroscience to improve choices for work, life and well-beingFrom EverandREWIRE for SUCCESS: An easy guide for using neuroscience to improve choices for work, life and well-beingNo ratings yet
- Beyond ATLS: Demystifying The Expert Resuscitationist: See Related Article, P. 289Document3 pagesBeyond ATLS: Demystifying The Expert Resuscitationist: See Related Article, P. 289surya rajNo ratings yet
- Harvard 18Document3 pagesHarvard 18MiguelNo ratings yet
- I'm Just A Sense Making AnalystDocument1 pageI'm Just A Sense Making AnalystTim SeniorNo ratings yet
- Managing Acute Behavioural Disturbance in A Neurology Ward: ReviewDocument15 pagesManaging Acute Behavioural Disturbance in A Neurology Ward: ReviewDaniel FodorNo ratings yet
- The Behavioural Science Guide ToDocument48 pagesThe Behavioural Science Guide ToBarbara RocíoNo ratings yet
- Trauma Life SupportDocument25 pagesTrauma Life Supporthailemariamgebrehiwot02No ratings yet
- New Editing StylesDocument221 pagesNew Editing StylesvirendhemreNo ratings yet
- Locomotor SyllabusDocument5 pagesLocomotor SyllabusAyeshaKhalidNo ratings yet
- Laporan Sisa Stock ObatDocument9 pagesLaporan Sisa Stock ObatYulya MayasaryNo ratings yet
- The PRISMAFLEX System: Making Possible PersonalDocument12 pagesThe PRISMAFLEX System: Making Possible PersonalluisfulaNo ratings yet
- JMM 29 119Document8 pagesJMM 29 119subanant11No ratings yet
- LGU Validation ToolDocument22 pagesLGU Validation ToolKirsten Calvo100% (3)
- Ch06 Blocked Fallopian TubesDocument80 pagesCh06 Blocked Fallopian TubesAasia Najaf SoomroNo ratings yet
- Biofeedback 2000x-Pert Hardware ManualDocument45 pagesBiofeedback 2000x-Pert Hardware ManualNery BorgesNo ratings yet
- Trends of Violence Against Healthcare by ShaheerDocument9 pagesTrends of Violence Against Healthcare by ShaheerShaheer zia100% (1)
- What Are Thrombosed External Hemorrhoids?Document3 pagesWhat Are Thrombosed External Hemorrhoids?Hanine HassanNo ratings yet
- Clinical ReflectionDocument3 pagesClinical ReflectionNaomi MasudaNo ratings yet
- Act 1 Urinary SystemDocument20 pagesAct 1 Urinary Systemisabellamarie.castillo.crsNo ratings yet
- Pharmacology Book - PharmaceuticsDocument48 pagesPharmacology Book - PharmaceuticsRuchi SinghNo ratings yet
- Home Remedies Using Onion Prophet666Document2 pagesHome Remedies Using Onion Prophet666Hussainz AliNo ratings yet
- Best Aid To OphthalmologyDocument501 pagesBest Aid To OphthalmologyMilthon Catacora Contreras67% (3)
- SA Anesthesia Drug Dosages 2022Document3 pagesSA Anesthesia Drug Dosages 2022KRLITHIU Borja100% (1)
- Teknik SAB Ideal-1Document31 pagesTeknik SAB Ideal-1Buatlogin DoangNo ratings yet
- ProliaDocument17 pagesProliamktantumNo ratings yet
- C1 Introduction For Genzyme: Unlock Insights. Activate GrowthDocument8 pagesC1 Introduction For Genzyme: Unlock Insights. Activate GrowthRobertFWainblatIIINo ratings yet
- Microsurgery BookDocument335 pagesMicrosurgery BookProforVictor100% (2)
- Roles and Responsibilities of ASHADocument3 pagesRoles and Responsibilities of ASHAmohanpskohli8310No ratings yet
- Schizophrenia Coursework - Jack Kerouac PresentationDocument16 pagesSchizophrenia Coursework - Jack Kerouac PresentationCMNo ratings yet
- Medical Image ProcessingDocument24 pagesMedical Image ProcessingInjeti satish kumarNo ratings yet
- Ethics and The Pharmaceutical Industry PDFDocument2 pagesEthics and The Pharmaceutical Industry PDFDonaldNo ratings yet
- Basics of Pharmacology: Speaker - DR - SantoshDocument76 pagesBasics of Pharmacology: Speaker - DR - SantoshRamya ChallaNo ratings yet
- Morning Report: Supervisor: Dr. Rusdhy A.H., SP - OG Medical StudentsDocument8 pagesMorning Report: Supervisor: Dr. Rusdhy A.H., SP - OG Medical StudentsEra MoetzNo ratings yet
- Alternative DietDocument31 pagesAlternative Dietiri_balNo ratings yet
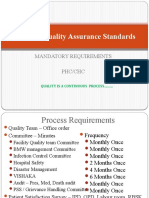
- National Quality Assurance Standards: Mandatory Requirements PHC/CHCDocument14 pagesNational Quality Assurance Standards: Mandatory Requirements PHC/CHCSathish KumaarNo ratings yet
- DENR - Proper Handling of Hazardous WasteDocument16 pagesDENR - Proper Handling of Hazardous WasteNisha HernandezNo ratings yet
- Hepar Sulph - The Homeopathic AntibioticDocument54 pagesHepar Sulph - The Homeopathic AntibioticGer DersenNo ratings yet
- Consulta de MedicamentosDocument39 pagesConsulta de MedicamentosJhonWainerLopezNo ratings yet