Professional Documents
Culture Documents
Quick Reference Guide October 2010 PDF
Quick Reference Guide October 2010 PDF
Uploaded by
Najia ChoudhuryOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Quick Reference Guide October 2010 PDF
Quick Reference Guide October 2010 PDF
Uploaded by
Najia ChoudhuryCopyright:
Available Formats
Quick Reference Guide
2010 Clinical Practice Guidelines for the Diagnosis and Management of Osteoporosis in Canada
This guide has been developed to provide healthcare professionals with a quick-reference summary of the most important recom-
mendations from the 2010 Clinical Practice Guidelines for the Diagnosis and Management of Osteoporosis in Canada. For more
detailed information, consult the full guideline document at www.osteoporosis.ca.
Recommendations for Clinical Assessment
Assessment Recommended Elements of Clinical Assessment
o Identify risk factors for low BMD, fractures and falls:
o Prior fragility fractures o High alcohol intake (≥3 units per day)
History o Parental hip fracture o Rheumatoid arthritis
o Glucocorticoid use o Inquire about falls in the previous 12 months
o Current smoking o Inquire about gait and balance
o Measure weight (weight loss of >10% since age 25 is significant)
]
o Measure height annually (prospective loss > 2cm) (historical height loss > 6 cm)
Screening for
Physical o Measure rib to pelvis distance ≤ 2 fingers' breadth
vertebral fractures
Examination o Measure occiput-to-wall distance (for kyphosis) > 5cm
o Assess fall risk by using Get-Up-and-Go Test (ability to get out of chair without using arms, walk several steps
and return)
Recommended Biochemical Tests for Patients Being Assessed for Osteoporosis
o Calcium, corrected for albumin o Thyroid stimulating hormone (TSH)
o Complete blood count o Serum protein electrophoresis for patients with vertebral fractures
o Creatinine o 25-hydroxy vitamin D (25-OH-D)*
o Alkaline phosphatase
*Should be measured after 3-4 months of adequate supplementation and should not be repeated if an optimal level ≥75 nmol/L is achieved.
Indications for BMD Testing
Older Adults (age ≥ 50 years) Younger Adults (age < 50 years)
• All women and men age ≥ 65 years • Fragility fracture
• Menopausal women, and men aged 50-64 years with clinical risk factors for fracture: • Prolonged use of glucocorticoids*
– Fragility fracture after age 40 • Use of other high-risk medications†
– Prolonged glucocorticoid use† • Hypogonadism or premature
– Other high-risk medication use* menopause
– Parental hip fracture • Malabsorption syndrome
– Vertebral fracture or osteopenia identified on X-ray • Primary hyperparathyroidism
– Current smoking • Other disorders strongly associated with
– High alcohol intake rapid bone loss and/or fracture
– Low body weight (< 60 kg) or major weight loss (>10% of weight at age 25 years)
– Rheumatoid arthritis
– Other disorders strongly associated with osteoporosis such as primary hyper-
parathyroidism, type 1 diabetes, osteogenesis imperfecta, uncontrolled hyper-
thyroidism, hypogonadism or premature menopause (< 45 years), Cushing’s
disease, chronic malnutrition or malabsorption, chronic liver disease, COPD and
chronic inflammatory conditions (e.g., inflammatory bowel disease)
†
≥3 months in the prior year at a prednisone equivalent dose ≥7.5 mg daily; *e.g., aromatase inhibitors, androgen deprivation therapy.
Assessment of Basal 10-year Fracture Risk: 2010 CAROC System
Women Men
0.0
-0.5
FEMORAL NECK T-score
Low risk (<10%) -1.0
-1.5
-2.0
-2.5
Moderate risk
-3.0
-3.5
High risk (>20%) -4.0
-4.5
50 55 60 65 70 75 80 85
AGE (years)
Note: 1) Fragility fracture after age 40 or recent prolonged systemic glucocorticoid use increases 2010 CAROC basal risk by one category (i.e., from low
to moderate or moderate to high).
2) Using this model in a patient on therapy only reflects the theoretical risk of a hypothetical patient who is treatment naïve and does not reflect the
risk reduction associated with therapy.
3) Femoral neck T-score should be derived from NHANES III Caucasian women reference database.
4) Individuals with a fragility fracture of the vertebra or hip, or with more than one fragility fracture are at high fracture risk.
Adapted from Papaioannou A et al. Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ 2010 http://www.cmaj.ca/cgi/doi/10.1503/cmaj.100771.
With permission from the publisher. © Osteoporosis Canada, October 2010. v-09-03-11.
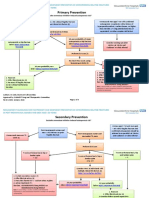
Integrated Management Model
Encourage basic bone health for all individuals including: regular active weight bearing exercise, calcium (diet
and supplements) 1200 mg daily, vitamin D: 800 - 2000 IU daily after age 50 (400 - 1000 for those <age 50 at low risk),
and fall prevention strategies.
Age <50 Age 50 - 64 Age ≥65
•Fragility fractures • Fragility fracture after age 40 • All men and women
•High-risk medication use • Prolonged glucocorticoid or other high-risk
•Hypogonadism medication use
•Malabsorption syndromes • Parental hip fracture
•Chronic inflammatory conditions • Vertebral fracture or osteopenia identified on
•Primary hyperparathyroidism X-ray
•Other disorders strongly associated • High alcohol intake or current smoking
with rapid bone loss and/or • Low body weight (< 60 kg) or major weight
fractures loss (>10% of weight at age 25)
• Other disorders strongly associated with
osteoporosis
Initial BMD Testing
Fracture Risk Assessment
Low Risk Moderate Risk High Risk
10-year fracture risk <10% 10-year fracture risk 10 - 20% 10-year fracture risk > 20%
or
Prior fragility fracture of hip or spine
Unlikely to benefit from Lateral thoracolumbar x-ray (T4-L4) or or
pharmacotherapy vertebral fracture analysis (VFA) may aid More than one fragility fracture
Reassess risk in 5 years in decision-making by identifying
vertebral fractures
Factors that Warrant Consideration for Always consider patient
Pharmacological Therapy: preference
o Additional vertebral fracture(s) identified on VFA or lat-
eral spine X-ray
o Previous wrist fracture in individuals older than age 65
or those with T-score ≤ -2.5
o Lumbar spine T-score much lower than femoral neck Good evidence of benefit from
T-score pharmacotherapy
Repeat BMD
in 1-3 years o Rapid bone loss
and reassess risk o Men receiving androgen-deprivation therapy for
prostate cancer
o Women receiving aromatase-inhibitor therapy for
breast cancer
o Long-term or repeated systemic glucocorticoid use
(oral or parenteral) that does not meet the conven-
tional criteria for recent prolonged systemic glucocor-
ticoid use
o Recurrent falls defined as falling 2 or more times in the
past 12 months
o Other disorders strongly associated with osteoporosis,
rapid bone loss or fractures
First Line Therapies with Evidence for Fracture Prevention in Postmenopausal Women*
Bone Forma-
Antiresorptive Therapy
tion Therapy
Type of
Bisphosphonates Estrogen**
Fracture Teriparatide
Zoledronic Denosumab Raloxifene (Hormone
Alendronate Risedronate Therapy)
Acid
Vertebral ¸ ¸ ¸ ¸ ¸ ¸ ¸
Hip ¸ ¸ ¸ ¸ – ¸ –
Non-vertebral† ¸ ¸ ¸ ¸ – ¸ ¸
†
In Clinical trials, non-vertebral fractures are a composite endpoint including hip, femur, pelvis, tibia, humerus, radius, and clavicle.
* For postmenopausal women, ¸ indicates first line therapies and Grade A recommendation. For men requiring treatment, alendronate, risedronate, and
zoledronic acid can be used as first-line therapies for prevention of fractures (Grade D).
** Hormone therapy (estrogen) can be used as first-line therapy in women with menopausal symptoms.
www.osteoporosis.ca
Adapted from Papaioannou A et al. Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ 2010 http://www.cmaj.ca/cgi/doi/10.1503/cmaj.100771.
With permission from the publisher. © Osteoporosis Canada, October 2010. v-09-03-11.
You might also like
- INBDE High-Yield Conditions To KnowDocument17 pagesINBDE High-Yield Conditions To KnowРами Кальмат100% (1)
- 26 50Document4 pages26 50Najia ChoudhuryNo ratings yet
- Work and Social Adjustment Scale (W&sas)Document1 pageWork and Social Adjustment Scale (W&sas)Najia ChoudhuryNo ratings yet
- Drug Study - AspirinDocument1 pageDrug Study - AspirinStefano James Pajarillo0% (1)
- Case Study #2: Mrs. BRDocument46 pagesCase Study #2: Mrs. BRGrape JuiceNo ratings yet
- Osteoporosis - Quick - Reference - Guide - 2010Document2 pagesOsteoporosis - Quick - Reference - Guide - 2010richiesiteNo ratings yet
- Osteoporosis GuidelineDocument3 pagesOsteoporosis Guidelinechendm123No ratings yet
- BMD Recommendations Slides Aug 05Document28 pagesBMD Recommendations Slides Aug 05Nurlaila ElaNo ratings yet
- Osteoporosis PPT - LFP PDFDocument55 pagesOsteoporosis PPT - LFP PDFFarhan FauziNo ratings yet
- Geriatric Assessment: Fundamentals of Aging Summer, 2021Document35 pagesGeriatric Assessment: Fundamentals of Aging Summer, 2021lesslyNo ratings yet
- Osteoporosis GuidelinesDocument10 pagesOsteoporosis GuidelinesMia DangaNo ratings yet
- Osteoprosis Presentation 2Document38 pagesOsteoprosis Presentation 2Shaz RizwanNo ratings yet
- Osteoporosis Screening, Diagnosis, and Treatment Guideline: Last Guideline Approval: April 2019Document12 pagesOsteoporosis Screening, Diagnosis, and Treatment Guideline: Last Guideline Approval: April 2019Mia DangaNo ratings yet
- OsteoporosisDocument43 pagesOsteoporosisMuna Hassan Mustafa100% (1)
- Osteoporosis - Screening & TestingDocument28 pagesOsteoporosis - Screening & TestingJoseNo ratings yet
- OsteoporosisDocument5 pagesOsteoporosisjsdlzjNo ratings yet
- Pharmacotherapy Handbook 7th Edition-1-31-43Document13 pagesPharmacotherapy Handbook 7th Edition-1-31-43Erfin NingoNo ratings yet
- Paratiroid and OsteoporosisDocument48 pagesParatiroid and OsteoporosisMuhammad Nur DelaphanEnamNo ratings yet
- Hyperparathyrodism Hypoparathyrodism: Dr. A. Wahyudi Pababbari, SPPD, FinasimDocument48 pagesHyperparathyrodism Hypoparathyrodism: Dr. A. Wahyudi Pababbari, SPPD, FinasimKahfiyahNo ratings yet
- Dr. Nur Aisiyah Widjaja, SpA (K) - PRESENTASI STUNTING WB 2019Document46 pagesDr. Nur Aisiyah Widjaja, SpA (K) - PRESENTASI STUNTING WB 2019ShellaAprillia100% (6)
- Osteoporosis: by Ali Naqvi, Jeff Hughes, and Shuktika NandkekolyarDocument19 pagesOsteoporosis: by Ali Naqvi, Jeff Hughes, and Shuktika NandkekolyarAdelaide SharfinaNo ratings yet
- Osteoporosis20 02 2016 160620141900 PDFDocument20 pagesOsteoporosis20 02 2016 160620141900 PDFenam professorNo ratings yet
- Osteoporosis Identification and Management in Primary Care (Nov 2018)Document6 pagesOsteoporosis Identification and Management in Primary Care (Nov 2018)Tony NgNo ratings yet
- Materi Fatty Liver Rsu Hermina & PLNDocument15 pagesMateri Fatty Liver Rsu Hermina & PLNifa virdiyasNo ratings yet
- Vitamin D DeficiencyDocument4 pagesVitamin D DeficiencyBaba AhmadNo ratings yet
- Secondary OsteoporosisDocument22 pagesSecondary OsteoporosisBenny Chris TantoNo ratings yet
- Leaflet SCOREDocument2 pagesLeaflet SCOREAdeline DevitaNo ratings yet
- How To Prevent MalnutritionDocument33 pagesHow To Prevent Malnutritionelia karosekaliNo ratings yet
- Bone Density Testing in General PracticeDocument4 pagesBone Density Testing in General PracticeYooyoPatoNo ratings yet
- OSTEOPOROSISDocument34 pagesOSTEOPOROSISVissalini JayabalanNo ratings yet
- OsteoporosisDocument47 pagesOsteoporosisSasha VaidyaNo ratings yet
- Menopause PPT AssessmentDocument46 pagesMenopause PPT Assessmentharry sallyNo ratings yet
- Adaptation MalnutritionDocument117 pagesAdaptation Malnutritionantidius john0% (1)
- Nice Osteoporosis Slide SetDocument21 pagesNice Osteoporosis Slide SetstrivingforjannahNo ratings yet
- Week 11 - Musculoskeletal System - STUDENTDocument53 pagesWeek 11 - Musculoskeletal System - STUDENTHarper EppsNo ratings yet
- How To Read Adx As Can by Ibrahima LaliDocument71 pagesHow To Read Adx As Can by Ibrahima Lalihussamhussama1995No ratings yet
- Risk Stratification in CVD Prevention: How To Identify Cardiovascular Risk in The OfficeDocument28 pagesRisk Stratification in CVD Prevention: How To Identify Cardiovascular Risk in The OfficeJuwanto Wakimin100% (1)
- Menopause: Dr. Triono Adisuroso, Spog, M.Med, M.PhilDocument57 pagesMenopause: Dr. Triono Adisuroso, Spog, M.Med, M.Philutin putiNo ratings yet
- Treatment of Thalassemia: Nadirah Rasyid Ridha Dasril DaudDocument30 pagesTreatment of Thalassemia: Nadirah Rasyid Ridha Dasril DaudIfah Inayah D'zatrichaNo ratings yet
- OsteoporosisDocument77 pagesOsteoporosisSaqib Bhat0% (1)
- Osteoporosis: Bagian Penyakit Dalam FK Nomensen - MedanDocument46 pagesOsteoporosis: Bagian Penyakit Dalam FK Nomensen - MedanE. Tito Julianda SinagaNo ratings yet
- Metronidazole: IntravenousDocument4 pagesMetronidazole: IntravenousShiela May GoNo ratings yet
- 1 - Short StatureDocument45 pages1 - Short StatureAmmar AlnajjarNo ratings yet
- Lecture No.4 Rheumatoid Arthritis by DR Chaman Lal PTDocument51 pagesLecture No.4 Rheumatoid Arthritis by DR Chaman Lal PTChaman Lal KarotiaNo ratings yet
- Postmenopausal Osteoporosis:: Latest GuidelinesDocument12 pagesPostmenopausal Osteoporosis:: Latest Guidelinesmedicina internaNo ratings yet
- 2019 Official Positions Adult 1Document35 pages2019 Official Positions Adult 1koro senseiNo ratings yet
- Osteodensitometry 2015 ISCD Official PositionsDocument15 pagesOsteodensitometry 2015 ISCD Official PositionsAlina Maria VoicuNo ratings yet
- MOD 23.2 Non-Surgical - Interventions - in - Severely - Obese - Patients-NEWDocument54 pagesMOD 23.2 Non-Surgical - Interventions - in - Severely - Obese - Patients-NEWVic GoNo ratings yet
- Materi - Exposure Dan Outcome - GM IPBDocument38 pagesMateri - Exposure Dan Outcome - GM IPBsalehahnhNo ratings yet
- Fhsis IndicatorDocument117 pagesFhsis IndicatorTherese Mae MadroneroNo ratings yet
- Reumatology DR - RehabDocument59 pagesReumatology DR - RehabMohammed Saad NabhanNo ratings yet
- Osteoporosis Medscape, IncompletoDocument58 pagesOsteoporosis Medscape, IncompletolssucllaNo ratings yet
- Geriatric PediatricDocument60 pagesGeriatric PediatricHossen AliNo ratings yet
- Calcium Vitamin DDocument24 pagesCalcium Vitamin DLoong Mo MaiNo ratings yet
- Bone DensitometryDocument42 pagesBone DensitometryWira Dat100% (1)
- OsteopeniaDocument20 pagesOsteopeniaAM100% (1)
- Ophthalmic Epidemiology:: A Clouded VisionDocument31 pagesOphthalmic Epidemiology:: A Clouded Visionnutrifmeal arifNo ratings yet
- Diabetes Leena M 091015125843 Phpapp01Document36 pagesDiabetes Leena M 091015125843 Phpapp01THARINDUNo ratings yet
- Prinsip Dasar EpidemiologiDocument46 pagesPrinsip Dasar EpidemiologiAnonymous 7XZZ37FHUHNo ratings yet
- Medical Check Up Standard Operating Procedure For Diagnosis 1. BMIDocument25 pagesMedical Check Up Standard Operating Procedure For Diagnosis 1. BMIlita agustinNo ratings yet
- Nutrition and Chronic Illness: Kathaleen Briggs Early, PHD, RD, Cde Assistant Professor of Biochemistry and NutritionDocument30 pagesNutrition and Chronic Illness: Kathaleen Briggs Early, PHD, RD, Cde Assistant Professor of Biochemistry and NutritionAbdiqani Mohamed AdanNo ratings yet
- The Diabetic FootDocument33 pagesThe Diabetic Footpagar bersihNo ratings yet
- Update On Arthritis in Kids and Adults: Jia, Ra and OaDocument68 pagesUpdate On Arthritis in Kids and Adults: Jia, Ra and OaDian Hayuningtyas PNo ratings yet
- The Ideal Prediabetes Diet Cookbook; The Super Diet Guide To Lose Weight, Manage And Reverse Prediabetes With Nutritious RecipesFrom EverandThe Ideal Prediabetes Diet Cookbook; The Super Diet Guide To Lose Weight, Manage And Reverse Prediabetes With Nutritious RecipesNo ratings yet
- Yale-Brown Obsessive Compulsive Scale (Y-BOCS)Document1 pageYale-Brown Obsessive Compulsive Scale (Y-BOCS)Najia ChoudhuryNo ratings yet
- Recurrent Psychotic Episodes With A Near - Monthly CycleDocument4 pagesRecurrent Psychotic Episodes With A Near - Monthly CycleNajia ChoudhuryNo ratings yet
- Brain Stimulation in Psychiatry by Kellner PDFDocument1 pageBrain Stimulation in Psychiatry by Kellner PDFNajia ChoudhuryNo ratings yet
- Perimenstrual Psychiatric Hospitalization Case Report and Literature ReviewDocument7 pagesPerimenstrual Psychiatric Hospitalization Case Report and Literature ReviewNajia ChoudhuryNo ratings yet
- Kellner Flyer R1Document1 pageKellner Flyer R1Najia ChoudhuryNo ratings yet
- 1 25Document4 pages1 25Najia ChoudhuryNo ratings yet
- Vic Acc Hospital PESCI Org ChartDocument1 pageVic Acc Hospital PESCI Org ChartNajia ChoudhuryNo ratings yet
- PMCV Computer Match Info Session Flyer 2015Document2 pagesPMCV Computer Match Info Session Flyer 2015Najia ChoudhuryNo ratings yet
- General/Rural Pathway Eligibility Guide - AGPT 2015: IMPORTANT NOTICE: Applicants Subject To Section 19AB Cannot BeDocument1 pageGeneral/Rural Pathway Eligibility Guide - AGPT 2015: IMPORTANT NOTICE: Applicants Subject To Section 19AB Cannot BeNajia ChoudhuryNo ratings yet
- Cat Eye SyndromeDocument3 pagesCat Eye SyndromeNajia ChoudhuryNo ratings yet
- Population Health Risk Assessment and ManagementDocument6 pagesPopulation Health Risk Assessment and ManagementNajia ChoudhuryNo ratings yet
- Ludwig AnginaDocument5 pagesLudwig AnginaSiti Aprilia wahyuniNo ratings yet
- Esa Filling in The Form FactsheetDocument32 pagesEsa Filling in The Form Factsheetandrewmmwilmot100% (1)
- Loxapine Drug StudyDocument5 pagesLoxapine Drug Studyshadow gonzalezNo ratings yet
- DementiaDocument39 pagesDementiaAudria Graciela100% (2)
- Drug StudyDocument24 pagesDrug Studyabulan100% (1)
- The Role of Madness in BulgakovDocument2 pagesThe Role of Madness in BulgakovRaminta UselytėNo ratings yet
- NAL Glossary GlGlossary - Glosarioosario 2012Document1,008 pagesNAL Glossary GlGlossary - Glosarioosario 2012tarunkusumNo ratings yet
- Acquired Heart DiseasesDocument41 pagesAcquired Heart DiseasesSaman SarKoNo ratings yet
- Puerarie Radix by TCM WikiDocument4 pagesPuerarie Radix by TCM WikiSarahMaulinaNo ratings yet
- Catcher in The Rye On DepressionDocument2 pagesCatcher in The Rye On DepressionjanvimadhaniNo ratings yet
- 2021 Jce BiologyDocument12 pages2021 Jce BiologyMalack ChagwaNo ratings yet
- Negations in Mullukurumba and Kattunaikka Tribes in NilgirisDocument5 pagesNegations in Mullukurumba and Kattunaikka Tribes in NilgirisEditor IJTSRDNo ratings yet
- Quiz 3Document7 pagesQuiz 3abezareljvenNo ratings yet
- 2012olympiadstageiv PDFDocument29 pages2012olympiadstageiv PDFTO Chau100% (1)
- NEET PG 2020 Question Paper With SolutionsDocument385 pagesNEET PG 2020 Question Paper With SolutionsmedpoxNo ratings yet
- Homeopathic Approach To COVID-19 A ReviewDocument6 pagesHomeopathic Approach To COVID-19 A ReviewAgasthya anikiniNo ratings yet
- OP Case Management For Complex AdultsDocument542 pagesOP Case Management For Complex Adultspfi_jenNo ratings yet
- COURSE TASK 2 - PeraltaDocument2 pagesCOURSE TASK 2 - PeraltaPaola CruzNo ratings yet
- Shackshop - Hydrogen WaterDocument13 pagesShackshop - Hydrogen WaterHeinrich Nel100% (2)
- PNLE: Community Health Nursing Exam 1 - RNpediaDocument13 pagesPNLE: Community Health Nursing Exam 1 - RNpediaLot Rosit100% (2)
- Fhsis Annual 2018Document496 pagesFhsis Annual 2018shenric16No ratings yet
- Factors Associated With 1-Year Outcome ofDocument8 pagesFactors Associated With 1-Year Outcome ofuricomasNo ratings yet
- First Aid 2016 Guidelines - EN PDFDocument192 pagesFirst Aid 2016 Guidelines - EN PDFKai HarukaNo ratings yet
- 10 Assessment and Care of Ent Problems: S Carter, C LairdDocument13 pages10 Assessment and Care of Ent Problems: S Carter, C LairdRemaja IslamNo ratings yet
- Gastrointestinal VirusesDocument25 pagesGastrointestinal VirusesgopscharanNo ratings yet
- Bahasa Inggris MakalahDocument6 pagesBahasa Inggris MakalahtrisnaulandariNo ratings yet
- Nutrients: Resveratrol Role in Autoimmune Disease-A Mini-ReviewDocument22 pagesNutrients: Resveratrol Role in Autoimmune Disease-A Mini-ReviewMihaela ȚarnăNo ratings yet
- Robert Lustig-Tooth Decay and Liver Decay-The Nexus of Doctors and DentistsDocument154 pagesRobert Lustig-Tooth Decay and Liver Decay-The Nexus of Doctors and DentistsEmine Alaaddinoglu100% (2)