100% found this document useful (2 votes)
783 views17 pagesNeurologic Assessment
This document provides guidance on performing a neurological assessment. It outlines three key objectives: establishing a baseline, determining changes from the baseline, and identifying emergent changes. The assessment involves interviewing the patient, performing a physical exam, and ordering specific diagnostic tests. The physical exam evaluates cranial nerves, motor and sensory function, balance, coordination, muscle strength, sensation, mental status, and reflexes. Any changes in these areas should be reported promptly.
Uploaded by
Jamal P. AlawiyaCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as RTF, PDF, TXT or read online on Scribd
100% found this document useful (2 votes)
783 views17 pagesNeurologic Assessment
This document provides guidance on performing a neurological assessment. It outlines three key objectives: establishing a baseline, determining changes from the baseline, and identifying emergent changes. The assessment involves interviewing the patient, performing a physical exam, and ordering specific diagnostic tests. The physical exam evaluates cranial nerves, motor and sensory function, balance, coordination, muscle strength, sensation, mental status, and reflexes. Any changes in these areas should be reported promptly.
Uploaded by
Jamal P. AlawiyaCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as RTF, PDF, TXT or read online on Scribd
- Objectives: Explains the goals and methodology of evaluating neurological assessments, highlighting key areas of focus.
- Neurological Assessment: Details the methods and steps involved in conducting a neurological assessment with specific emphasis on cranial nerves and sensory functions.
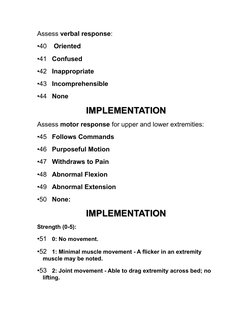
- Motor Examination: Discusses the evaluation of motor functions, examining posture and strength in various physical states.
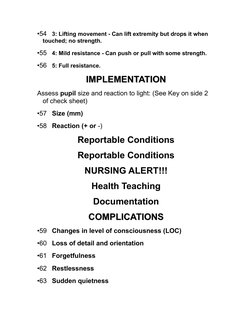
- Implementation: Outlines procedural steps for implementing neurological assessments, recording observations, and interpreting results.
- Role of Neurological Investigations: Highlights different diagnostic imaging techniques and their purposes in neurological testing, including CT scans and MRIs.
- Application: A Case Analysis: Provides a practical case analysis demonstrating the application of neurological assessment principles in a clinical scenario.
- Summary: Summarizes the main components of neurological assessments and the three core aspects reviewed.