Professional Documents
Culture Documents
t3 Som 2014 2
Uploaded by
Julio AbarzuaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
t3 Som 2014 2
Uploaded by
Julio AbarzuaCopyright:
Available Formats
Journal of Dental Research
http://jdr.sagepub.com/
Remodeling the Dentofacial Skeleton: The Biological Basis of Orthodontics and Dentofacial
Orthopedics
M.C. Meikle
J DENT RES 2007 86: 12
DOI: 10.1177/154405910708600103
The online version of this article can be found at:
http://jdr.sagepub.com/content/86/1/12
Published by:
http://www.sagepublications.com
On behalf of:
International and American Associations for Dental Research
Additional services and information for Journal of Dental Research can be found at:
Email Alerts: http://jdr.sagepub.com/cgi/alerts
Subscriptions: http://jdr.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
>> Version of Record - Jan 1, 2007
What is This?
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
CRITICAL REVIEWS IN ORAL BIOLOGY & MEDICINE
Remodeling the Dentofacial Skeleton: The Biological Basis
of Orthodontics and Dentofacial Orthopedics
M.C. Meikle INTRODUCTION
Department of Oral Sciences, Faculty of Dentistry, University of
Otago, PO Box 647, Dunedin, New Zealand;
Twhich
he bones and articulations of the craniofacial skeleton grow and
function in an environment of mechanical forces. These forces—
include muscle activity, mastication, the expansile growth of
murray.meikle@dent.otago.ac.nz
the brain, gravity, and man-made orthodontic appliances—influence
J Dent Res 86(1):12-24, 2007 the shape and relative position of each bone in the complex, through
the process of biological adaptation termed 'remodeling' (Moffett,
1971, 1973). With the exception of the cranial base synchondroses
and the temporomandibular joints (TMJ), all the articulations
between the bones of the skull (and teeth) are fibrous joints. Such
ABSTRACT articulations are responsive to alterations in mechanical loading;
Orthodontic tooth movement is dependent upon the indeed, orthodontic treatment is dependent upon the ease with
remodeling of the periodontal ligament and alveolar bone which the periodontal ligament (PDL) and supporting alveolar bone
by mechanical means. Facial sutures are also fibrous can be remodeled by mechanical means. (For a recent review of the
articulations, and by remodeling these joints, one can alter tissue, cellular, and molecular mechanisms regulating orthodontic
the positional relationships of the bones of the facial tooth movement, see Meikle, 2006.)
skeleton. As might be expected from the structure and Numerous well-documented animal studies have also showed
mobility of the temporomandibular joint (TMJ), this that craniofacial sutures, as well as the TMJs, can be remodeled by
articulation is more resistant to mechanical deformation, externally applied mechanical force. The aim of this review is to
and whether functional mandibular displacement can alter discuss the significance of these findings and the extent to which they
the growth of the condyle remains controversial. Clinical can be utilized clinically in the correction of skeletal malocclusion.
investigations of the effects of the Andresen activator and An understanding of the cellular and molecular mechanisms that
its variants on dentofacial growth suggest that the changes enable bones and other connective tissues of the dentofacial skeleton
are essentially dento-alveolar. However, with the to adapt to changes in their mechanical environment is fundamental
popularity of active functional appliances, such as the to the practice of orthodontics and dentofacial orthopedics, based on
Herbst and twin-block based on 'jumping the bite', sound biological and bioengineering principles.
attention has focused on how they achieve dentofacial
change. Animal experimentation enables informed FACIAL SUTURES
decisions to be made regarding the effects of orthodontic Sutures are found only in the skull and have two main functions: (1)
treatment on the facial skeleton at the tissue, cellular, and as a site of active bone growth; and (2) to provide a firm union
molecular levels. Both rat and monkey models have been between adjacent bones, while at the same time permitting slight
widely used, and the following conclusions can be drawn movement in response to mechanical stress. The fibrous and cellular
from such experimentation: (1) Facial sutures readily organization of sutures is not uniform and will vary, depending on
respond to changes in their mechanical environment; (2) site and age, and within the same suture over time (Persson, 1973).
anterior mandibular displacement in rat models does not As a generalization, however, each is formed by a continuation of the
increase the mitotic activity of cells within the condyle to fibrous and cellular periosteum around the margins of adjacent bones,
be of clinical significance, and (3) mandibular united by a central intermediate layer of fibrous tissue and blood
displacement in non-human primates initiates remodeling vessels (Pritchard et al., 1956). The cellular layer provides the cells
activity within the TMJ and can alter condylar growth required for osteogenesis at the sutural margins; the intermediate
direction. This last conclusion may have clinical utility, layer allows for continued growth of the sutural connective tissue and
particularly in an actively growing child. permits small adjustments of the bones relative to each other.
Morphology of Facial Sutures
KEY WORDS: facial sutures, temporomandibular joint,
condylar cartilage, articular remodeling, functional Suture morphology is determined by the site and mechanical stresses
appliances. to which they are exposed. In general, midline sutures are described
as butt-end, while others are of the overlapping beveled type
(Kokich, 1976). During the growth period, sutures have a
predominantly linear configuration, but with age, more complex
beveled and interdigitating sutures develop through functional
modification. Where strong bonds are required, interdigitating
sutures develop to enhance surface contact and resist separation. All
sutures eventually undergo various degrees of fusion by osseous
Received January 30, 2006; Accepted April 19, 2006 union or synostosis. Sutural synostosis begins at different ages in the
12 Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
J Dent Res 86(1) 2007 Remodeling the Dentofacial Skeleton 13
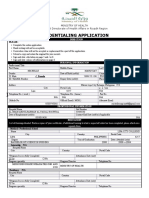
Table 1. Time of Closure of Some Craniofacial Sutures in Humans
Closure Closure
Begins Begins
Cranial Suture (yrs) Facial Suture (yrs)
Interfrontal (metopic) 2 Intermaxillary (palatal) 20-25
Interparietal (sagittal) 22 Frontomaxillary 68-71
Frontoparietal (coronal) 24 Frontonasal 68
Occipitoparietal (lambdoid) 26 Nasomaxillary 68
Frontozygomatic 72
Temporoparietal (squamosal) 35-39 Zygomaticomaxillary 70-72
Data derived from Todd and Lyon (1924, 1925); Kokich (1976, 1986);
Persson and Thilander (1977).
various sutures of the skull and proceeds at the endocranial
slightly earlier than at the ectocranial surface (Todd and Lyon,
1924, 1925). In contrast to cranial sutures, facial sutures can
remain patent quite late into adult life (Table 1).
Patency of Facial Sutures
There are two plausible explanations why cranial and facial
sutures differ in their time of closure, one biochemical, the
other mechanical. Much of what is known about suture biology
at the molecular level comes from human studies of premature
fusion. Despite their widely differing phenotypes, accelerated
suture closure in several autosomal-dominant cranio-
synostoses—such as Crouzon, Apert, Jackson-Weiss, and
Pfeiffer syndromes—has been shown to be due to gain-of-
function mutations in the FGFR-2 (fibroblast growth factor
receptor-2) gene. The extent to which facial sutures are affected
is less clear, although many of these syndromes are
characterized by maxillary hypoplasia. In addition to causing Figure 1. Dorsal view of a miniature pig skull (Sus scrofa) showing
achondroplasia, mutations of the FGFR-3 gene are also average peak strains during mastication. Solid arrows directed toward
sutures indicate compressive strains; open arrows indicate tensile
responsible for Crouzon syndrome with acanthosis nigricans strains. The sutures of the braincase are predominantly tensed, while
and Muenke-type craniosynostosis. (For further discussion and those of the snout are compressed. 500 = 500 microstrains.
references, see Meikle, 2002.) (Redrawn from Rafferty and Herring, 1999)
The evidence from animal models suggests specific roles
for growth factors as well as the BMP (bone morphogenetic
protein), Shh (sonic hedgehog), and FGF signaling pathways.
Nevertheless, where each of these factors and their target genes snout (internasal and nasofrontal), mainly compressive (Fig. 1).
fits into a complex morphogenetic cascade remains poorly Nevertheless, sutural strain is a very dynamic parameter, and
understood. Insulin-like growth factors (IGFs; Bradley et al., many sutures show temporal and regional variations in strain
1999), transforming growth factor- (TGF-) isoforms polarity; some sutures even show a small compressive strain
(Opperman et al., 1997, 1998; Roth et al., 1997)), and FGF-2, before or after the tensile peak (Herring and Mucci, 1991).
FGFR-1, and FGFR-2 (Mehrara et al., 1998) have all been Variations in the strains to which facial sutures are exposed
localized in the cells and matrix of the dura mater, osteoblasts, (tensile, compressive, shear) by masticatory muscle function
and sutures in rats. Their expression is increased during will be reflected in their morphology.
synostosis, suggesting a paracrine signaling role for these Sutures that are exposed to a predominantly compressive
factors; since facial sutures differ from cranial sutures in the strain will continue to grow, however, and it seems likely that,
absence of dura, this may partly explain why facial sutures in sutures with complex interdigitations, the oblique
remain patent longer. arrangement of the fibers of the sutural ligament may convert
The other reason is related to the intermittent mechanical what was initially a compressive load into a tensile strain
loading of the circum-maxillary suture system that occurs (Herring and Rafferty, 2000). For this reason, trying to
during mastication (Behrents et al., 1978; Wagemans et al., establish the loading pattern of a suture from the histological
1988; Jaslow, 1990; Herring and Mucci, 1991). Animal models appearance in animal models can be difficult and prone to
indicate that the various craniofacial sutures are under distinct subjective interpretation.
and dissimilar strain regimes (Rafferty and Herring, 1999).
Experiments conducted on the miniature pig have showed that, REMODELING THE MAXILLA
for the sutures of the calvaria (interparietal, interfrontal, IN NON-HUMAN PRIMATES
coronal), peak strains are mainly tensile, and for those of the The first evidence that changes in maxillary position could be
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
14 Meikle J Dent Res 86(1) 2007
unexpected finding in a study of cervical traction in adult
monkeys was the presence of resorption craters on the articular
surface of the condylar head, suggesting distal displacement of
the mandible by occlusal forces (Brandt et al., 1979).
The maxilla can also be distracted anteriorly by extra-oral
forward traction applied to the dentition (Dellinger, 1973;
Kambara, 1977; Nanda, 1978; Jackson et al., 1979). However,
the drawback of trying to remodel facial sutures by applying
forces directly to the teeth is their tendency to move, thereby
reducing the orthopedic effect. Skeletal anchorage has therefore
been used to exert force directly to the bone via endosseous
implants (Turley et al., 1980; Smalley et al., 1988). Smalley et
al. applied forward traction to osseointegrated titanium
implants inserted into the maxillae of 4 pigtail monkeys.
Cephalometric and dry skull analyses showed that the amount
of skeletal protraction was significantly greater when compared
with that generated by conventional tooth-borne appliances.
Given the importance of these findings, it is surprising that
skeletal anchorage has only recently entered mainstream
clinical orthodontic practice.
CLINICAL REMODELING OF THE MAXILLA
While numerous primate studies have shown that mechanical
forces of appropriate strength and duration can remodel facial
sutures, the extent to which these changes can be utilized
clinically continues to be the subject of debate.
Figure 2. Structure of facial sutures. (A) Photomicrograph of the
zygomatico-frontal suture of an adult Macaca mulatta monkey. Remodeling the Maxilla with Headgear
Hematoxylin and eosin stain, original magnification 75x. Numerous
reversal lines (arrowheads) are indicative of past remodeling activity.
Several investigations have shown that HG treatment can alter
The absence of cellular activity within the sutural ligament is indicative of the positional relationship of the maxilla to the cranial base
a quiescent suture. (B) Section through the frontomaxillary suture of an (Moore, 1959; Ricketts, 1960; Poulton, 1967; Watson, 1972;
adolescent Macaca mulatta monkey after application of a posteriorly Weislander, 1974, 1975), but others have been unable to detect
directed force to the maxillary teeth. Mallory stain. Original significant orthopedic change, the main effect being tooth
magnification, 120x. This active suture shows a complex pattern of
remodelling activity, with highly cellular new bone (blue) deposited on movement (Badell, 1976; Bernstein et al., 1977; Baumrind et
old bone (red). Sutures consist of type I collagen and non-collagenous al., 1979). The reasons for this have been discussed previously
glycoproteins uniting adjacent bone surfaces; also visible (arrowheads) (Meikle, 1980), but the evidence suggests that optimal
is a central zone of fibroblastic cells. Scale bars not available. conditions for achieving orthopedic change in the maxilla are
fulfilled when (1) the force is of sufficient magnitude (1000 gm
per side) to be transmitted beyond the periodontal joints, and
achieved by the application of load came from cephalometric (2) as many teeth as possible have been incorporated into the
studies of individuals who had worn extra-oral traction or appliance. The direction in which the force is applied (cervical
headgear (HG) during orthodontic treatment (Moore, 1959; vs. occipital) will also influence the outcome, depending upon
Ricketts, 1960). These landmark investigations provided the whether the sutures are exposed to a predominantly tensile or
impetus for research into the effects of externally induced compressive mechanical strain.
mechanical forces on the craniofacial skeleton of the macaque
monkey at the University of Washington (Moffett, 1971), and Prospective Studies of Headgear Treatment
other centers with primate facilities. The only published prospective randomized clinical trial (RCT)
In experiments with both adolescent and adult monkeys, of HG treatment, prior to the three RCTs of Class II treatment
forces have been applied to the dentomaxillary skeleton by a funded by the National Institute of Dental Research in 1988,
wide variety of mechanical devices. Most of the early studies was by Jakobsson (1967), a man clearly ahead of his time. In
involved the use of HG to apply a posterior force, and a Jakobsson's study, 60 children aged 8-9 yrs with a Class II
combination of metallic implants, radiography, in vivo bone division 1 malocclusion were randomly assigned to either an
markers, and histology to analyze the outcome (Sproule, 1968; Andresen activator, HG, or control group. Both HG and
Fredrick, 1969; Cutler et al., 1972; Droschl, 1973; Elder and activator treatments were found to have had a distalizing effect
Tuenge, 1974; Meldrum, 1975; Triftshauser and Walters, 1976). on the maxilla.
All showed that, by using mechanical forces to create controlled In the RCT undertaken at the University of North Carolina
remodeling of facial sutures (Fig. 2), it is possible to alter the (Tulloch et al., 1997a,b, 1998), 166 persons having mixed
positional relationships of the bones of the facial skeleton. In dentitions with an overjet greater than 7 mm were randomly
growing animals, however, this effect is transitory; after the assigned to early treatment with either a headgear or bionator,
termination of HG treatment, the maxilla resumes its normal or to control. There was considerable variation in the pattern of
forward growth pattern (Tuenge and Elder, 1974). In some cases, change in all three groups, with the HG group showing
the remodeling response may even extend to the lower jaw. An restricted forward movement of the maxilla averaging about 1
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
J Dent Res 86(1) 2007 Remodeling the Dentofacial Skeleton 15
mm. The University of Florida RCT involved 249 participants
aged 9-10 years who were randomly assigned to control,
bionator, or HG/biteplate treatments (Keeling et al., 1998).
Neither the HG/biteplate nor the bionator had a significant
effect on maxillary growth, although both appliances were
reported to enhance the growth of the mandible. In a study of
63 participants conducted at the University of Pennsylvania,
early treatment outcome with either a HG or Fränkel functional
regulator were compared (Ghafari et al., 1998). Both treatments
were found to be effective at reducing overjets, but the study
did not include a control group.
Rapid Maxillary Expansion
The most dramatic example of sutural remodeling is the result of
rapid maxillary expansion (RME), when a diastema is opened
between the central incisor teeth. Angell (1860), who introduced
the technique using a screw mechanism, claimed that the
apparatus produced a separation of the two halves of the maxilla.
In commenting on the article, the Editor of the Dental Cosmos,
while being unwilling to assert that such a thing was not utterly
impossible, found this exceedingly doubtful (the italics are the Figure 3. Undue emphasis on the midpalatal suture (11) rather obscures
Editor's). For the next 100 years, RME had a somewhat the fact that, for rapid maxillary expansion to be successful, several
facial sutures, particularly the zygomatico-maxillary (9) and the
checkered history, until Haas (1961, 1965) popularized the fixed zygomatico-frontal (4,5), will need to be extensively remodeled and then
palatal expander in the 1960s, and showed that RME in retained to eliminate any residual strain. (From McMinn et al. (1981), A
adolescents had a predictable outcome. For RME to be effective Colour Atlas of Head and Neck Anatomy, Wolfe Medical Publishers Ltd.
as an orthopedic appliance, the magnitude of the applied force Reproduced with the kind permission of Mr. Ralph Hutchings.)
must be of sufficient magnitude to be transmitted beyond the
periodontal joints; otherwise, the stresses will be absorbed within
the alveolar bone, resulting in tooth movement alone. Although
not usually recognized by orthodontists as such, rapid maxillary desired outcome, but, in many cases, whether for financial
expansion is an example of distraction osteogenesis. reasons or fear of surgery, it may be the only alternative.
It is a common belief that the mid-palatal suture fuses at
around the age of 15 yrs. However, there is some anatomical and Maxillary Protraction
clinical evidence that this is not necessarily true. In a histological Maxillary protraction in the treatment of Class III malocclusion
study of 60 human autopsy specimens aged 0-18 yrs, Melsen has increased in popularity in recent years, due to the work of
(1975) found that growth of the mid-palatal suture continued up Delaire with the orthopedic face mask (Delaire, 1971; Delaire
to the ages of 16 in girls and 18 in boys. Furthermore, Persson et al., 1972), and the animal experimentation discussed earlier
and Thilander (1977) reported, in an older age group (15-35 yrs), showing that the maxilla can be distracted (Dellinger, 1973;
that although palatal sutures may show evidence of obliteration Kambara, 1977; Nanda, 1978; Jackson et al., 1979).
during the juvenile period, a marked degree of closure was rarely Nevertheless, the degree to which maxillary skeletal change
found until the third decade, i.e., 20-30 yrs of age. can be achieved clinically is age- and technique-dependent.
The key issue is not whether osseous union has begun, but Several studies have reported the skeletal and dental effects
the overall percentage of the suture that has actually fused. of maxillary protraction in the correction of skeletal Class III
Persson and Thilander speculated that if osseous bridging of 5% malocclusion, both with RME (Ngan et al., 1996, 1998; Kapust
represented the upper limit for splitting the mid-palatal suture, et al., 1998; Franchi et al., 2004) and without RME (Wisth et
this would not be reached in most people before the age of 25 al., 1987; Takada et al., 1993). Together with the findings of a
years. In a combined radiographic-histological investigation, meta-analysis (Jäger et al., 2001), these studies showed that
Wehrbein and Yildizhan (2001) concluded that if this were true, maxillary protraction is more effective if (1) undertaken in the
RME would have been successful in nine of the 10 individuals late deciduous or early mixed dentition, and (2) combined with
(aged 18-38 yrs) in their study sample. They also showed that a RME. Given that the aim of RME is to loosen the articulations
radiologically invisible suture does not necessarily mean that the of the maxillary complex from the rest of the skull, this is not
suture is fused histologically. In any event, undue focus on the surprising. The next logical step in the evolution of maxillary
palate rather obscures the fact that the greatest resistance to RME distraction techniques is to combine RME with the use of
comes not from the mid-palatal suture, but from the circum- osseous mini-screws to provide forward distraction directly to
maxillary suture network (Isaacson and Ingram, 1964; Wertz, the bones. Not only will this avoid unwanted tooth movement,
1970) that attaches the maxilla to the rest of the skull (Fig. 3). but it will also enable the method to be effective in a much
Clinical studies of RME undertaken in adults (Alpern and older age group than at present.
Yurosko, 1987; Capelozza et al., 1996; Handelman et al., 2000)
further support the histological evidence that palatal expansion EXPERIMENTAL REMODELING OF THE TMJ
without surgery is possible in young adults well into their The major aim of dentofacial orthopedic treatment in Class II
twenties. Nevertheless, the technique remains controversial and individuals with mandibular retrognathia (approximately 70%)
unacceptable to many clinicians. It may not always have the is to enhance or optimize the growth of the condyle by
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
16 Meikle J Dent Res 86(1) 2007
University of Strasbourg have suggested that anterior
displacement of the mandible in growing rats can bring about
additional growth of condylar cartilage (Fig. 4), and hence the
growth of the mandible, by stimulating the cells of the
proliferative zone (PZ) to undergo mitosis (Charlier et al., 1969;
Petrovic et al., 1975; Petrovic and Stutzmann, 1977). Attempts
to reproduce these results, however, using biochemical,
histomorphometric, and autoradiographic methods, have been
unsuccessful (Tonge et al., 1982; Degroote, 1984; Ghafari and
Degroote, 1986; Tewson et al., 1988).
The reasons would seem to be a question of experimental
design and methodology. Histomorphometry is not an exact
science, and it helps to have experience with the technique to
fully understand the problems involved. These include the
following:
(1) Since it is impracticable to carry out a quantitative
analysis of the hundreds of sections cut from each condyle, it is
customary to select 4-5 fields in sections considered to be
'representative' for measurement purposes. This introduces an
element of subjective bias in the choice of experimental and
control sections.
(2) Another source of subjective bias is not counting the
number of 3H-thymidine-labeled cells (Fig. 4) in histological
sections 'blind', which makes any attempt at quantitation
potentially unsafe.
(3) The data are not always normalized. In other words, no
attempt has been made to relate the number of labeled cells to
the total number in a representative field, to establish a labeling
index. This is a fundamental principle of quantitation to
compensate for the variation inherent in all biological systems,
regardless of whether one is using biochemical or histological
techniques. Not all condyles, even in the rat, are the same size.
It has also been suggested that the discrepancies reported in
the literature could be due to differences in appliance
Figure 4. Autoradiograph of a coronal section through the squamo-
mandibular joint of a rat, 24 hrs after an intraperitional injection of 3H- construction and such factors as the degree of opening,
thymidine to label cells synthesizing DNA. Most of the labeled cells are continuous vs. intermittent displacement, and the extent to
located within the proliferative zone. It is the mesenchymal stem cells of which a definite forward shift of the mandible might be
the PZ that differentiate into the chondroblasts of the cartilage layer achieved (Degroote, 1984; Ghafari and Degroote, 1986;
under the influence of function. Counting both labeled and unlabeled
cells in a 'representative' field to obtain a labeling index is a laborious
Tsolakis and Spyropoulos, 1997; Tsolakis et al., 1997). To
procedure, and, in young animals, it is also sometimes difficult to address this problem, Tsolakis et al. (1997) designed a new
distinguish the boundaries between different cellular layers. SJS, device to produce a controlled, stable, and reproducible anterior
superior joint space; D, interarticular disc; AZ, articular zone; PZ, advancement of the mandible in rats by rubber elastics rather
proliferative zone; CC condylar cartilage. Hematoxylin stain. Original than by functional displacement. Following the application of a
magnification, 350x. Scale bar not available.
force of 25 gm for 12 hrs/day for 30 days, they found that
growth of the lower jaw was affected to some extent. Although
linear measurements indicated that mandibles in the
functional anterior displacement of the mandible. The extent to experimental group were longer than in the controls, they were
which this can be achieved, however, and whether it has any unable to conclude if this was due to an increase in the growth
clinical significance are topics of long-standing controversy. of condylar cartilage.
Both rat and monkey models have been used to study TMJ
Alterations in Gene Expression following
adaptation to protrusive function, and although the use of non-
Protrusive Function in Rats
human primates has declined, rat models continue to be widely
used. Whether functional appliance therapy can accelerate or enhance
As might be deduced from its structure and function, the the growth of the condyle is a question that has been revived
TMJ is morphologically adapted to resist the effects of recently by Rabie and colleagues, at the University of Hong
mechanical loading, and therefore is more difficult to remodel Kong, who have applied molecular methods to the problem
than fibrous joints. This is due to the physical properties of the (Rabie and Hägg, 2002; Rabie et al., 2003, 2004; Tang et al.,
cartilaginous matrix, the function of which is to protect the 2004). They have showed, in a rat model, that the transcription
subchondral bone from resorptive remodeling. factor Sox-9 and its target gene type II collagen are up-
regulated in the glenoid fossa following forward mandibular
Functional Mandibular Protrusion in Rats positioning. Over an experimental period of 17 days, this
Experiments conducted by Petrovic and his co-workers at the reached a maximum on day 3 but declined thereafter (Rabie et
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
J Dent Res 86(1) 2007 Remodeling the Dentofacial Skeleton 17
al., 2003). Mandibular advancement also triggered an increase
in the expression of the cell-cell signaling molecule Indian
hedgehog (Ihh) in the cells of the PZ and adjacent
chondroblasts (Tang et al., 2004). This coincided with an
increase in cell proliferation within the PZ. Both these
increases proved to be transient, however, reaching a peak after
7 days and returning to control levels by day 14.
Rabie et al. have interpreted these findings as proof that
functional appliances enhance condylar growth by stimulating
the differentiation of PZ cells into chondroblasts. Elegant
though these experiments may be, the temporary nature of the
reported changes does present a problem. The responses of
cells and tissues to mechanically induced strain are well- Figure 5. Summary of remodeling changes in the surface contours of the
established (for reviews, see Sandy et al., 1993; Meikle, 2006), TMJ in the rhesus monkey following experimental anterior mandibular
so it is not surprising to find that mechanically deformed cells displacement. Condylar growth appears to be directed more posteriorly,
in the craniomandibular joint of the rat respond in a similar and the shape of the condyle becomes less rounded; bone is also
deposited along the anterior surface of the post-glenoid tubercle.
manner, in terms of both changes in metabolic activity and Compensatory resorption occurs along the posterior surface of the post-
proliferation. glenoid tubercle, and the insertion of the lateral pterygoid muscle into
If one bears in mind the stimulatory effect of mechanical the neck of the condyle.
stress on cell proliferation and DNA synthesis in other model
systems (Roberts and Jee, 1974; Meikle et al., 1979), the
transient burst in mitotic activity reported by Rabie et al. is
likely to result from the release of G2-blocked cells, allowing summary of the adaptive changes in the TMJ of the rhesus
them to undergo mitosis, as well as enabling G1-blocked cells monkey following anterior mandibular displacement based on
to enter the S phase. Ihh has also been shown to be an essential the above studies is shown in Fig. 5.
component of mechanical force transduction in chondrocyte Breitner believed that forward displacement of the
proliferation (Wu et al., 2001), and to up-regulate the mandible could enhance condylar growth. This conclusion has
expression of cyclin D1, a kinase required for the transition of received support from McNamara and Bryan (1987), in a
cells from G1 to the S phase of the cell cycle (Long et al., cephalometric study of 23 juvenile Macaca mulatta monkeys.
2001). After 144 weeks, the mandibles of treated animals (measured
by the linear distance infradentale-condylion) were 5-6 mm
TMJ Remodeling in Non-human Primates longer than those of controls. Changes between the ramus and
While the evidence from rat experimentation has been body of the mandible were measured by the condylar-ramus-
controversial and subject to various interpretations, anterior occlusal (CRO) angle. In the control group, a closure in the
displacement of the mandible in the rhesus (Macaca mulatta) CRO angle (indicative of a forward growth rotation), averaging
monkey has been shown consistently to produce significant 8.8 degrees, occurred, while in the experimental group, the
morphological changes in the TMJ (Breitner, 1940, 1941; CRO angle opened an average of 2.8 degrees.
Baume and Derichsweiler, 1961; Meikle, 1970; Stockli and As in humans (Björk, 1963; Björk and Skieller, 1972), the
Willert, 1971; Adams et al., 1972). condyle of monkeys undergoes an age-dependent change in
Prior to Carl Breitner, investigations into the effects of growth direction (McNamara and Graber, 1975; Luder, 1987).
orthodontic treatment at the histological level in animal models One interpretation of the above findings is that anterior
had been confined to changes in the PDL and alveolar bone. displacement of the mandible remodeled the condylar head in a
Breitner was the first to look beyond the teeth and study the more posterior direction, thereby neutralizing the forward
tissue changes induced in the TMJ and other sites in the growth rotation observed in the control animals. This would
mandible. His findings were first published in the German account for the increased length of the mandible in the
literature during the 1930s and later in English in two classic experimental group, and provides a valuable indicator as to
papers entitled "Bone changes resulting from experimental what might be happening clinically in growing children treated
orthodontic treatment" and "Further investigations of bone with 'bite jumping' appliances.
changes..." (Breitner, 1940, 1941). These provided convincing
histological evidence that the influence of orthodontic IS CONDYLAR CARTILAGE UNIQUE?
treatment in experimental animals was not limited to the teeth, Condylar cartilage is different in many ways from the articular
but extended to other parts of the mandible, causing remodeling cartilage of long bones and has always held a certain 'mystique'
of the glenoid fossa and condyle. Breitner's papers have been for the dental profession. However, a recent claim (Shen and
criticized for containing only one animal in each experimental Darendeliler, 2005) that "...The most marked uniqueness of
group, and little, if any, evidence of control material. condylar cartilage lies in its capability of adaptive remodeling
Nevertheless, despite the introduction of vital staining, in response to external stimuli during or after natural growth" is
improved histological techniques, metallic bone implants, and not one of them. Nor is the implication that the articular
cephalometric radiography, subsequent investigations have surfaces of long bones are unchanging inert structures that do
added comparatively little new information to Breitner's not undergo endochondral ossification.
original findings (Baume and Derichsweiler, 1961; Meikle,
1970; Stockli and Willert, 1971; Elgoyhen et al., 1972; Remodeling Articular Cartilage
McNamara and Carlson, 1979; Woodside et al., 1987). A It has been known, at least since Alexander Ogston (Ogston,
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
18 Meikle J Dent Res 86(1) 2007
1875, 1878), that articular cartilage has the ability to adapt to Genetic Control Mechanisms
alterations in the mechanical equilibrium of the skeleton, even Both condylar and epiphyseal cartilages share some of the
in the adult. Ogston believed that articular cartilage was genetic control mechanisms regulating chondrogenesis. These
continually renewing itself from a central focus of growth. He include expression of the transcription factor Sox-9, essential
observed that growth occurred outward to compensate for wear for chondrocyte differentiation from mesenchymal stem cells,
and tear at the surface, as well as inward, where it added to the and the negative feedback loop involving PTH-rP (parathyroid
subchondral bone by endochondral osteogenesis. hormone-related protein) and Ihh that controls the rate of
This was confirmed experimentally 90 years later by the differentiation of chondrocytes in the growth plate (Lanske et
autoradiographic studies of Mankin (1962), in which the al., 1996; Vortkamp et al., 1996); PTH-rP is produced mainly
injection of 3 H-thymidine into the knee joint of rabbits in the perichondrium, while the PTH/PTH-rP receptor is
demonstrated the presence of a central zone of proliferative expressed by pre-hypertrophic chondrocytes.
cells in the femoral articular cartilage. Also, in a study of Also common is the degradation of the mineralized matrix
articular remodeling in human synovial joints, Johnson (1959) that occurs during endochondral ossification by a combination
calculated that progressive remodeling added 3 mm of new of osteoclastic action and MMP (matrix metalloproteinases)
bone to the femoral head between the ages of 30 and 60 yrs. expression. All three major classes of MMPs and their inhibitor
The remodeling of articular cartilage is a process of biological TIMPs (tissue inhibitors of metalloproteinases) have been
adaptation to changing environmental circumstances; there is a identified in the chondrocytes and matrix of long bones (Brown
large body of literature on the subject. (For a review of TMJ et al., 1989) and condylar cartilage (Breckon et al., 1994).
remodeling, see Meikle, 1992, 2002.) However, condylar cartilage is not affected by gain-of-function
Condylar Cartilage is Derived from the Periosteum mutations in the FGFR-3 gene (a negative regulator of
Central to an understanding of condylar growth is the chondrocyte differentiation in bones of the primary
question of why cartilage is present in a membrane bone in cartilaginous skeleton) that cause achondroplasia (Rousseau et
the first place. Of the many examples of connective tissues al., 1994; Shiang et al., 1994), as well as other skeletal
adapting to changing mechanical circumstances, the one dysplasias, such as hypochondroplasia and thanatophoric
most relevant to the condyle is from the work of Murray dysplasia in humans.
(1963), who described the development of adventitious
(secondary) cartilage in several articulations in the skull of CLINICAL REMODELING OF THE TMJ
the embryonic chick. He found that secondary cartilage Prior to the introduction of cephalometric radiography, most
always developed in membrane bones, but only at clinicians believed the teaching of the Angle school. With a
articulations that were mobile, or where the musculature set few notable exceptions (Case, 1911), inheritance was dismissed
up conditions of strain. In subsequent experiments with as an etiological factor, and the occurrence of malocclusion in
grafted and paralyzed embryos (Murray and Smiles, 1965), parents and siblings was believed to occur because each had
cartilage did not form, and cells that normally formed experienced exactly the same environment (Dewey, 1914).
cartilage produced bone instead. Malocclusion was considered to be the consequence of
Studies in which mandibular condyles have been inadequate bone growth and could be stimulated by alignment
transplanted into a non-functional environment have also of the teeth—a rather liberal interpretation of Wolff's law. In
showed that the progenitor cells of the PZ differentiate into other words, the stimulating effects of orthodontic tooth
osteoblasts, and not chondroblasts as in situ (Duterloo, 1967; movement and the establishment of normal occlusion, if started
Meikle, 1973a,b). The cells are therefore multipotential and can young enough, would cause the jaws to grow. Malocclusion
form either cartilage or bone, depending upon the could be treated without extracting teeth by growing bone.
environmental circumstances. Simple microscopic observation The first cephalometric investigation of treatment outcome
makes it obvious that the articular and proliferative zones of the (Brodie et al., 1938) effectively destroyed the myth that
condyle are no more than a continuation of the fibrous and orthodontic appliances could stimulate the growth of bone. This
cellular layers of the periosteum. The change from osteogenesis was followed by the first longitudinal cephalometric
to chondrogenesis has resulted from the evolutionary investigation of the early growth of the head (Brodie, 1941),
development of an articular condylar process in the mandible which suggested that the growth pattern of the individual was
(dentary) of mammals and, as a consequence, the altered established at an early age, and that, once attained, it did not
functional demands of the periosteum covering the articular change. At the time, these publications had a profound impact
joint surfaces (Meikle, 1973a,b). on orthodontic thought, giving rise to the linked concepts of (1)
Only by recognizing that condylar cartilage is a product of the immutability of the facial or morphogenetic pattern of the
the periosteum can the differences in cellular kinetics, individual, and (2) the inability of the clinician to alter it in any
structure, and growth that exist between condylar and way. As a result, the old dogma was replaced by a new one.
epiphyseal cartilage be understood. These include failure of the Orthodontic treatment was limited to tooth movement alone.
chondrocytes to divide (growth is appositional as in bone), and, Some clinicians still believe this.
as a result, the cells are not organized into parallel columns. It
is also worth being aware that functional activity also plays a Age-related Changes in the Human Condyle
role in the growth of epiphyseal cartilage. In the absence of Before we discuss the clinical evidence, it is worth considering
function, the growth plates of rat metacarpals fail to maintain a the age-related changes in the morphology of the human TMJ
satisfactory increase in transverse diameter, and the cells of the and condyle that have been reported during the time that
perichondrium at the perimeter differentiate into osteoblasts, growth modification is normally undertaken (Fig. 6). It also
not chondrocytes (Meikle, 1975). helps put the findings of rat and primate experimentation into
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
J Dent Res 86(1) 2007 Remodeling the Dentofacial Skeleton 19
perspective. The material is of necessity limited and is likely to
remain so.
In a series of 51 human TMJs (24 male, 27 female)
collected at autopsy, Wright and Moffett (1974) observed the
following histological changes from birth to 21 yrs:
Throughout this period, the articular tissue (AZ) consists of
fibrous connective tissue with fibrocytes interspersed among
the collagen fibers, but no cartilage cells were observed at any
time. The proliferative layer (PZ) was approximately 6-10 cells
in width and continuous with the osteogenic layer of the
periosteum; however, no mitoses were observed. The cartilage
layer was 1.25-1.5 mm in thickness at birth and became
progressively thinner with growth, showing no recognizable
increase in thickness at adolescence that might be correlated
with increased pubertal growth.
During the mixed-dentition stage (6-12 yrs), while the Figure 6. Photomicrograph of a sagittal section through the head of the
condyle gradually increased all its dimensions, the cartilage mandibular condyle ( human, aged 10-12 yrs, the age when functional
remained uniformly thin (at 0.3-0.5 mm) and became limited to appliance treatment is usually started). There is some evidence of
the anterosuperior aspect of the condylar head, opposite the endochondral ossification, but chondrogenesis itself does not appear to
be particularly active. IJS, inferior joint space; AZ, articular zone; PZ,
posterior slope of the articular eminence. This is consistent proliferative zone; CC, condylar cartilage. Hematoxylin and eosin stain.
with the role of the cartilage in the protection of the Original magnification, 20x. Scale bar not available.
subchondral bone. At 16-17 yrs, the cartilage becomes thinner,
and a closing plate of bone coalesces below it. Human condylar
cartilage is a rather less impressive structure than it is in the
adolescent monkey or the 6-week-old rat. It is also worth poor research design; it also encourages post hoc deductions. In
bearing in mind that condylar cartilage is not the only site in the new era of evidence-based medicine, the prospective RCT
the condyle where osteogenesis is taking place during growth. is seen by many to be the 'gold standard' for analyzing
treatment outcome, and the only valid source of clinical data.
The Evidence of Retrospective Investigations
Europe has a tradition of dentofacial orthopedics, and most of The Evidence of Prospective Randomized Clinical Trials
the various appliance systems currently used in the treatment The effects of functional appliances of various designs on
method referred to as 'functional jaw orthopedics' originated in mandibular growth in each of the relevant RCTs published to
Europe. The skeletal and dental effects of several functional date are summarized in Table 2. These suggest that (1) small
appliances based on the
Norwegian system (Andresen Table 2. Randomized Clinical Trials of Class II Treatment: Effects on Mandibular Growth
and Häupl, 1942; Korkhaus,
1960; Fränkel, 1966; Marschner Study and Analysis Appliance Number Treated/Control Age Change (mm)a
and Harris, 1966; Demisch,
1972; McNamara et al., 1985), Jakobsson (1967) Andresen activator 17/19 8.5 (mean) NS
as well as more active devices Change in Pog
such as the Herbst and twin-
block (Pancherz, 1979; Nelson et al. (1993) Fränkel FFR 13/17 11.6 (mean) NS
Weislander, 1984; Hägg and Co-Pog Harvold activator 12/17
Pancherz, 1988; DeVincenzo,
1991; Mills and McCulloch, Tulloch et al. (1997a) Bionator 53/61 1 year pre-PHV 1.33b
1998; Baccetti et al, 2000), have Co-Pog
been reported in numerous
investigations. Nearly all have Keeling et al. (1998) Bionator 78/78 9.6 ± 0.8 0.8b
reported successful treatment, Johnston analysis
but whether the appliance in
question altered facial growth, Pancherz (1982) Herbst 22/20 12.1 ± 0.11 2.2
particularly mandibular growth, Pancherz analysis
sufficiently to attain clinical
significance remains Lund and Sandler (1998) Twin-block 36/27 12.4 (mean) 2.4
controversial. Ar-Pog
The scientific value of the
retrospective study has been O'Brien et al. (2003) Twin-block 73/74 8-10 (range) 1.55
criticized for several valid Pancherz analysis 9.7 (mean)
reasons, including selection bias,
inadequate sample size, lack of a Mean difference between experimental and control groups. NS, not significant; all other differences
contemporaneous controls, and are small but statistically significant.
b Mean annualized change (mm/yr). In the Pancherz (1982) study, the treatment time was 6 months.
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
20 Meikle J Dent Res 86(1) 2007
and cone beam computed tomography is showing promise
(Hilgers et al., 2005), the TMJ will continue to be something of
a 'black box'.
• Validity of the measurements
The cephalometric measurements themselves used to quantitate
change are of questionable validity. Linear dimensions such as
condylion-pogonion (Co-Pog), or its surrogate, articulare-
gnathion (Ar-Gn), to quantify changes in mandibular growth
are not valid measurements. They do not take into account
condylar growth rotation (Björk, 1963) and underestimate
condylar growth on average by 3-4 mm (Hägg and Attström,
1992). The Pancherz analysis (Pancherz, 1982) used in some
RCTs (Table 2) will similarly underestimate mandibular
growth, since it is a linear measurement that does not take into
account variations in condylar growth rotation (Meikle, 2005).
To be valid, measurements should be made between pre- and
post-treatment condylions; not only will this give a more
accurate estimate of the amount of condylar growth, but it will
also provide information regarding condylar growth direction.
• The pubertal growth spurt
Variabilities in the timing, magnitude, and duration of the
pubertal growth spurt are difficult to predict accurately. There
are also differences in the timing of peak height velocity (PHV)
and pubertal spurts in facial growth. Velocity curves for a
French-Canadian population (Buschang et al., 1999) showed
that, for males, the average annual growth velocity for the
condyle ranges from 2.1-3.1 mm, with a peak at 14.3 yrs (Fig.
Figure 7. Growth velocity curves for the mandibular condyle based on 7). There was, however, substantial variation. For a male
the movement of the condylion on serial mandibular tracings individual in the 90th percentile, for example, condylar growth
superimposed on natural reference structures (Björk's structures). will average 5 mm/year, while for another in the 25th
Percentiles were used to describe individual variation and growth curves percentile, the annual increment will be as little as 1-2 mm.
drawn by growth rates plotted at each age, with the lines between
smoothed. (Redrawn from Buschang et al., 1999)
This will have a significant effect on treatment outcome.
It is generally recognized that optimal conditions for
achieving growth modification occur when treatment coincides
with the pubertal growth spurt and, in particular, peak height
but statistically significant differences in mandibular length velocity (PHV). Hägg and Pancherz (1988), for example,
were produced in the majority of these studies, and (2) showed that the skeletal contribution to changes in dental arch
functional appliances such as the Herbst and twin-block, based relationship from Class II to Class I will be greater in persons
on the principle of 'jumping the bite', are more effective at treated at PHV or during the succeeding year. The ages of the
modifying mandibular growth than are passive appliances such population samples in Table 2 suggest that many of the
as the Andresen activator and its variants. participants were some distance from achieving PHV. In only
However, unlike a laboratory experiment, in which it is one, the UNC investigation discussed earlier (Tulloch et al.,
possible to limit the differences between experimental and 1997a), was treatment timed to start within 1 yr of PHV, which
control groups to the single factor being investigated, in clinical might explain the differences in their results compared with
investigations, an orthodontic appliance is just one of several those of Keeling et al. (1998), despite both groups using the
variables affecting the outcome. Clinical studies also deal with bionator. It seems likely that, given the above, all the RCTs
population data with an emphasis on averages, not on published to date significantly underestimate mandibular
individuals. Clinicians treat individuals, and population data are change.
of little use in predicting the likely outcome for specific
Can the TMJ be Remodeled Clinically?
individuals, characterized as they are by endless anatomical and
physiological variations. Apart from questions of individual It is clear that functional displacement of the mandible in
compliance and the operator effect, outcome measurements and primate models alters the surface contours of the condyle,
hence conclusions will therefore be influenced by the glenoid fossa, and post-glenoid tubercle. In that respect, it is no
following: different from any other joint. There is also evidence to suggest
that condylar growth can be directed in a more posterior
• The inaccuracy of the cephalometric method direction. Remodeling the TMJ in monkeys is one thing.
The measurement error may be greater than the growth changes Remodeling it clinically is quite another. Nevertheless, there is
one is hoping to identify. Condylion, a key landmark, is evidence, from those treated with the Herbst appliance,
notoriously difficult to identify accurately on conventional suggesting that it might be possible.
cephalometric radiographs. Until imaging techniques improve, In a systematic review of the literature regarding the effects
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
J Dent Res 86(1) 2007 Remodeling the Dentofacial Skeleton 21
of Herbst treatment on TMJ morphology, Popowich et al. Norwegischen Systeme. Leipzig, Germany: Verlag von JA Barthe.
(2003) identified 80 studies related to the topic. Publications Angell EH (1860). Treatment of irregularity of the permanent or adult teeth.
Dental Cosmos 1:540-544; 599-600.
that used transpharyngeal radiographs to document
Baccetti T, Franchi L, Toth LR, McNamara JA Jr (2000). Treatment timing
morphological change were excluded, leaving five publications for Twin-block therapy. Am J Orthod Dentofacial Orthop 118:159-170.
meeting their criteria. In one of these (Ruf and Pancherz, 1998), Badell MC (1976). An evaluation of extraoral combined high-pull traction
magnetic resonance imaging (MRI) was used to analyze TMJ and cervical traction to the maxilla. Am J Orthod 69:431-446.
growth adaptation in 15 consecutive Class II patients treated for Baume L, Derichsweiler J (1961). Is the condylar growth centre responsive
a period of 7 months. After 6-12 wks, signs of condylar to orthodontic therapy? An experimental study in Macaca mulatta.
remodeling were seen at the postero-superior border in 29 of Oral Surg Oral Med Oral Pathol 14:347-362.
Baumrind S, Molthen R, West EE, Miller DM (1979). Distal displacement
the 30 condyles, while glenoid fossa remodeling was noted in of the maxilla and the upper first molar. Am J Orthod 75:630-640.
22 joints. Behrents RG, Carlson DS, Abdelnour T (1978). In vivo analysis of bone
Of interest is the major study (Paulsen, 1997) of 100 strain about the sagittal suture in Macaca mulatta during masticatory
consecutive patients treated with the Herbst appliance. This movements. J Dent Res 57:904-908.
was not included in the Popowich et al. review, since Bernstein L, Ulbrich RW, Gianelly AA (1977). Orthopedics versus
orthopantomographic and transpharyngeal radiography were orthodontics in class II treatment: an implant study. Am J Orthod
72:549-559.
used to obtain the condylar images. Paulsen reported that, in
Björk A (1963). Variations in the growth pattern of the human mandible:
most cases, a visible change in the morphology of the condyle longitudinal radiographic study by the implant method. J Dent Res
occurred—a double contour of the postero-superior part of the 42(Pt 2):400-411.
condyle, and sometimes at the distal surface of the ramus. In Björk A, Skieller V (1972). Facial development and tooth eruption. An
children/youth at the peak of puberty, the double contour was implant study at the age of puberty. Am J Orthod 62:339-383.
distinct only for a short time, while in late puberty it persisted Bradley JP, Han VR, Roth DA, Levine JP, McCarthy JG, Longaker MT
(1999). Increased IGF-I and IGF-II mRNA and IGF-I peptide in fusing
for several months. Paulsen concluded that the observed
rat cranial sutures suggest evidence for a paracrine role of insulin-like
changes were due to bone remodeling. growth factors in suture fusion. Plastic Reconstr Surg 104:129-138.
These findings suggest that condylar growth occurred in a Brandt HC, Shapiro PA, Kokich VG (1979). Experimental and
more posterior direction, which is consistent with the evidence postexperimental effects of posteriorly directed extraoral traction in
from functional mandibular displacement in monkeys. They adult Macaca fascicularis. Am J Orthod 75:301-317.
further suggest that remodeling of the TMJ with the Herbst Breckon JJ, Hembry RM, Reynolds JJ, Meikle MC (1994). Regional and
appliance (and probably the twin-block) can be regarded as a temporal changes in the synthesis of matrix metalloproteinases and
TIMP-1 during development of the rabbit mandibular condyle. J Anat
definite clinical possibility, particularly in an actively growing 184:99-110.
child. Breitner C (1940). Bone changes resulting from experimental orthodontic
treatment. Am J Orthod 26:521-547.
Growth Stimulation vs. Growth Remodeling Breitner C (1941). Further investigations of bone changes resulting from
Mechanical stimuli arising from the functional activity of the experimental orthodontic treatment. Am J Orthod 27:605-632.
TMJ are essential for the differentiation and maintenance of Brodie AG (1941). On the growth pattern of the human head from the third
condylar cartilage. Put simply, no function, no cartilage. month to the eighth year of life. Am J Anat 68:209-262.
Brodie AG, Downs WB, Goldstein A, Myer E (1938). Cephalometric
However, is one then justified in concluding that so-called
appraisal of orthodontic results: a preliminary report. Angle Orthod
functional appliances increase chondrogenesis and bone 8:261-265.
formation, or do the transient changes in cell proliferation and Brown CC, Hembry RM, Reynolds JJ (1989). Immunolocalization of
metabolism reported by some groups simply represent localized metalloproteinases and their inhibitor in the rabbit growth plate. J Bone
adjustments to alterated mechanical strain? Joint Surg Am 71:580-593.
Given the ambiguity of the experimental and anatomical Buschang PH, Santos-Pinto A, Demirjian A (1999). Incremental growth
charts for condylar growth between 6 and 16 years of age. Eur J Orthod
evidence, the hypothesis that functional mandibular
21:167-173.
displacement stimulates the mitosis of PZ cells, and hence the Capelozza Filho L, Cardoso Neto J, da Silva Filho OG, Ursi WJ (1996).
growth of the condyle in humans, should remain firmly in the Non-surgically assisted rapid maxillary expansion in adults. Int J Adult
category labeled 'unproven'. It would seem to be a weak basis Orthodon Orthognath Surg 11:57-66; discussion 67-70.
on which to make statements such as, '...this indicates that Case CS (1911). The question of extraction in orthodontia. Trans Nat Dent
functional appliance therapy can truly enhance condylar Assoc. Reprinted (1964) as part of the series "Extraction debate of 1911
growth' (Rabie et al., 2003). It would be nice to think so, but by Case, Dewey and Cryer", Am J Orthodont 50:656-691, 751-768,
843-851, 900-911.
clinical experience suggests otherwise. The point may be Charlier JP, Petrovic A, Herrmann-Stutzmann J (1969). Effects of
regarded as largely one of semantics, but from the clinical point mandibular hyperpropulsion on the prechondroblastic zone of the
of view, the term growth remodeling seems preferable to young rat condyle. Am J Orthod 55:71-74.
growth stimulation for describing the morphological changes in Cutler BS, Hassig FH, Turpin DL (1972). Dentofacial changes produced
the TMJ that result from the use of dentofacial orthopedic during and after use of a modified Milwaukee brace on Macaca
appliances. mulatta. Am J Orthod 61:115-137.
Degroote CW (1984). Alterability of mandibular condylar growth in the
young rat and its implications [doctoral thesis]. Leuven, Belgium:
REFERENCES Catholic University of Louvain.
Adams CD, Meikle MC, Norwick KW, Turpin DL (1972). Dentofacial Delaire J (1971). La croissance maxillaire: déductions thérapeutiquue
remodelling produced by intermaxillary forces in Macaca mulatta. [Maxillary growth: therapeutic conclusions]. Trans Eur Orthod Soc 81-
Arch Oral Biol 17:1519-1535. 102 [article in French].
Alpern MC, Yurosko JJ (1987). Rapid palatal expansion in adults with and Delaire J, Verdon P, Lumineau JP, Cherga-Negrea A, Talmant J, Boisson M
without surgery. Angle Orthod 57:245-263. (1972). Quelques rèsultats des tractions extra-orales a appui fronto-
Andresen J, Häupl K (1942). Funktionkieferorthopädie. Die Grundlage des mentonnier dans le traitment orthopèdique des malformations maxillo-
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
22 Meikle J Dent Res 86(1) 2007
mandibulaires de classe III et des sèquelles osseuses des fentes labio- young Macaca nemestrina. Am J Orthod 75:319-333.
maxillaires [Some results of extra-oral tractions with front-chin rest in Jäger A, Braumann B, Kim C, Wahner S (2001). Skeletal and dental effects
the orthodontic treatment of class 3 maxillomandibular malformations of maxillary protraction in patients with angle class III malocclusion. A
and of bony sequelae of cleft lip and palate]. Rev Stomatol Chir meta-analysis. J Orofac Orthop 62:275-284 [article in English/German].
Maxillofac 73:633-642 [article in French]. Jakobsson SO (1967). Cephalometric evaluation of treatment effect on Class
Dellinger EL (1973). A preliminary study of anterior maxillary II, Division I malocclusions. Am J Orthod 53:446-457.
displacement. Am J Orthod 63:509-516. Jaslow CR (1990). Mechanical properties of cranial sutures. J Biomech
Demisch A (1972). Effects of activator therapy on the craniofacial skeleton 23:313-321.
in class II, division 1 malocclusion. Trans Eur Orthod Soc 295-310. Johnson LC (1959). Kinetics of osteoarthritis. Lab Invest 8:1223-1241.
DeVincenzo JP (1991). Changes in mandibular length before, during, and Kambara T (1977). Dentofacial changes produced by extraoral forward
after successful orthopedic correction of Class II malocclusions, using a force in Macaca irus. Am J Orthod 71:249-277.
functional appliance. Am J Orthod Dentofacial Orthop 99:241-257. Kapust AJ, Sinclair PM, Turley PK (1998). Cephalometric effects of face
Dewey M (1914). Practical orthodontia. St. Louis, MO: C.V. Mosby mask/expansion therapy in Class III children: a comparison of three age
Company, pp. 87-90. groups. Am J Orthod Dentofacial Orthop 113:204-212.
Droschl H (1973). The effect of heavy orthopedic forces on the maxilla in Keeling SD, Wheeler TT, King GJ, Garvan CW, Cohen DA, Cabassa S, et
the growing Saimiri sciureus (squirrel monkey). Am J Orthod 63:449- al. (1998). Anteroposterior skeletal and dental changes after early Class
461. II treatment with bionators and headgear. Am J Orthod Dentofacial
Duterloo HS (1967). In vivo implantation of the mandibular condyle of the Orthop 113:40-50.
rat. An experimental investigation of the growth of the lower jaw Kokich VG (1976). Age changes in the human frontozygomatic suture. Am
[thesis]. The Netherlands: University of Nijmegen. J Orthod 69:411-430.
Elder JR, Tuenge RH (1974). Cephalometric and histologic changes Kokich VG (1986). Biology of sutures. In: Craniosynostosis: diagnosis,
produced by extraoral high-pull traction to the maxilla in Macaca evaluation and management. Cohen MM Jr, editor. New York: Raven
mulatta. Am J Orthod 66:599-617. Press, pp. 81-103.
Elgoyhen JC, Moyers RM, McNamara JA Jr, Riolo ML (1972). Craniofacial Korkhaus G (1960). Present orthodontic thought in Germany. Am J Orthod
adaptation of protrusive function in young rhesus monkeys. Am J 46:187-206.
Orthod 62:469-480. Lanske B, Karaplis AC, Lee K, Luz A, Vortkamp A, Pirro A, et al. (1996).
Franchi L, Baccetti T, McNamara JA (2004). Postpubertal assessment of PTH/PTHrP receptor in early development and Indian hedgehog-
treatment timing for maxillary expansion and protraction therapy regulated bone growth. Science 273:663-666.
followed by fixed appliances. Am J Orthod Dentofacial Orthop Long F, Zhang XM, Karp S, Yang Y, McMahon AP (2001). Genetic
126:555-568. manipulation of hedgehog signalling in the endochondral skeleton
Fränkel R (1966). The theoretical concept underlying treatment with reveals a direct role in the regulation of chondrocyte proliferation.
function correctors. Rep Congr Eur Orthod Soc 42:233-254. Development 128:5099-5108.
Fredrick DL (1969). Dentofacial changes produced by extraoral high-pull Luder HU (1987). Growth direction in the mandibular condyle of pre-
traction to the maxilla of Macaca mulatta; a histologic and serial pubertal and pubertal monkeys (Macaca fascicularis) studied by
cephalometric study [MSD thesis]. Seattle: University of Washington. morphometry and radioautography. Arch Oral Biol 32:239-247.
Ghafari J, Degroote C (1986). Condylar cartilage response to continuous Lund DI, Sandler PJ (1998). The effects of twin blocks: a prospective
mandibular displacement in the rat. Angle Orthod 56:49-57. controlled study. Am J Orthod Dentofacial Orthop 113:104-110.
Ghafari J, Shofer FS, Jacobsson-Hunt U, Markowitz DL, Laster LL (1998). Mankin HJ (1962). Localization of tritiated thymidine in articular cartilage of
Headgear versus function regulator in the early treatment of Class II rabbits. I. Growth in immature cartilage. J Bone Joint Surg 44:682-688.
division 1 malocclusion: a randomized clinical trial. Am J Orthod Marschner JF, Harris JE (1966). Mandibular growth and class II treatment.
Dentofacial Orthop 113:51-61. Angle Orthod 36:89-93.
Haas AJ (1961). Rapid expansion of the maxillary dental arch and nasal McMinn RMH, Hutchings RT, Logan BM (1981). A colour atlas of head
cavity by opening the midpalatal suture. Angle Orthod 31:73-90. and neck anatomy. London: Wolfe Medical Publishers, Ltd.
Haas AJ (1965). The treatment of maxillary deficiency by opening the McNamara JA Jr, Bryan FA (1987). Long-term mandibular adaptations to
midpalatal suture. Angle Orthod 35:200-217. protrusive function: an experimental study in Macaca mulatta. Am J
Hägg U, Attström K (1992). Mandibular growth estimated by four Orthod Dentofacial Orthop 92:98-108.
cephalometric measurements. Am J Orthod Dentofacial Orthop McNamara JA Jr, Carlson DS (1979). Quantitative analysis of
102:146-152. temporomandibular adaptations to protrusive function. Am J Orthod
Hägg U, Pancherz H (1988). Dentofacial orthopaedics in relation to 76:593-611.
chronological age, growth period and skeletal development. An McNamara JA Jr, Graber LW (1975). Mandibular growth in the rhesus
analysis of 72 male patients with Class II division 1 malocclusion monkey (Macaca mulatta). Am J Phys Anthropol 42:15-24.
treated with the Herbst appliance. Eur J Orthod 10:169-176. McNamara JA Jr, Bookstein FL, Shaughnessy TG (1985). Skeletal and
Handelman CS, Wang L, BeGole EA, Haas AJ (2000). Nonsurgical rapid dental changes following functional regulator therapy on class II
maxillary expansion in adults: report on 47 cases using the Haas patients. Am J Orthod 88:91-110.
expander. Angle Orthod 70:129-144. Mehrara BJ, Mackool RJ, McCarthy JG, Gittes GK, Longaker MT (1998).
Herring SW, Mucci RJ (1991). In vivo strain in cranial sutures: the Immunolocalization of basic fibroblast growth factor and fibroblast
zygomatic arch. J Morphol 207:225-239. growth factor receptor-1 and receptor-2 in rat cranial sutures. Plast
Herring SW, Rafferty KL (2000). Cranial and facial sutures: functional Reconstr Surg 102:1805-1817; discussion 1818-1820.
loading in relation to growth and morphology. In: Biological Meikle MC (1970). The effect of a class II intermaxillary force on the
mechanisms of tooth eruption, resorption and replacement by implants. dentofacial complex in the adult Macaca mulatta monkey. Am J Orthod
Davidovitch Z, Mah J, editors. Boston, MA: Harvard Society for the 58:323-340.
Advancement of Orthodontics, pp. 269-276. Meikle MC (1973a). In vivo transplantation of the mandibular joint of the
Hilgers ML, Scarfe WC, Scheetz JP, Farman AG (2005). Accuracy of linear rat: an autoradiographic investigation into cellular changes at the
temporomandibular joint measurements with cone beam computed condyle. Arch Oral Biol 18:1011-1020.
tomography and digital cephalometric radiography. Am J Orthod Meikle MC (1973b). The role of the condyle in the postnatal growth of the
Dentofacial Orthop 128:803-811. mandible. Am J Orthod 64:50-62.
Isaacson RJ, Ingram AH (1964). Forces produced by rapid maxillary Meikle MC (1975). The influence of function on chondrogenesis at the
expansion. II. Forces present during treatment. Angle Orthod 34:261- epiphyseal cartilage of a growing long bone. Anat Rec 182:387-399.
270. Meikle MC (1980). The dentomaxillary complex and overjet correction in
Jackson GW, Kokich VG, Shapiro PA (1979). Experimental and Class II division 1 malocclusion: objectives of skeletal and alveolar
postexperimental response to anteriorly directed extraoral force in remodelling. Am J Orthod 77:184-197.
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
J Dent Res 86(1) 2007 Remodeling the Dentofacial Skeleton 23
Meikle MC (1992). Remodelling. In: The temporomandibular joint—a Persson M (1973). Structure and growth of facial sutures. Odont Revy
biological basis for clinical practice. 4th ed. Sarnat BG, Laskin DM, 24(Suppl 26):1-146.
editors. Orlando, FL: W.B. Saunders & Company, pp. 93-107. Persson M, Thilander B (1977). Palatal suture closure in man from 15 to 35
Meikle MC (2002). Craniofacial development, growth and evolution. years of age. Am J Orthod 72:42-52.
Bressingham, Norfolk, England: Bateson Publishing. Petrovic AG, Stutzmann JJ (1977). Further investigations into the
Meikle MC (2005). What do prospective randomized clinical trials tell us functioning of the peripheral comparator of the servosystem in the
about the treatment of class II malocclusions? A personal viewpoint control of the condylar cartilage growth rate and the lengthening of the
[guest editorial]. Eur J Orthod 27:105-114. jaw. In: The biology of occlusal development. McNamara JA, editor.
Meikle MC (2006). The tissue, cellular and molecular regulation of Monograph 7. Ann Arbor, MI: Center for Human Growth and
orthodontic tooth movement: 100 years after Carl Sandstedt. Eur J Development, University of Michigan, pp. 255-291.
Orthod 28:221-240. Petrovic AG, Stutzmann JJ, Oudet C (1975). Control processes in the
Meikle MC, Reynolds JJ, Sellers A, Dingle JT (1979). Rabbit cranial postnatal growth of the condylar cartilage of the mandible. In:
sutures in vitro: a new experimental model for studying the response of Determinants of mandibular form and growth. McNamara JA, editor.
fibrous joints to mechanical stress. Calcif Tissue Int 28:137-144. Monograph 4. Ann Arbor, MI: Center for Human Growth and
Meldrum RJ (1975). Alterations in the upper facial growth of Macaca Development, University of Michigan, pp. 101-153.
mulatta resulting from high-pull headgear. Am J Orthod 67:393-411. Popowich K, Nebbe B, Major PW (2003). Effect of Herbst treatment on
Melsen B (1975). Palatal growth studied on human autopsy material. A temporomandibular joint morphology: a systematic literature review.
histologic microradiographic study. Am J Orthod 68:42-54. Am J Orthod Dentofacial Orthop 123:388-394.
Mills CM, McCulloch KJ (1998). Treatment effects of the twin block Poulton DR (1967). The influence of extraoral traction. Am J Orthod 53:8-
appliance: a cephalometric study. Am J Orthod Dentofacial Orthop 18.
114:15-24. Pritchard JJ, Scott JH, Girgis FG (1956). The structure and development of
Moffett B (1971). Remodelling of the craniofacial articulations by various cranial and facial sutures. J Anat 90:73-86.
orthodontic appliances in rhesus monkeys. Trans Eur Orthod Soc, 207- Rabie AB, Hägg U (2002). Factors regulating mandibular condylar growth.
216. Am J Orthod Dentofacial Orthop 122:401-409.
Moffett BC (1973). Remodelling of the craniofacial skeleton produced by Rabie AB, She TT, Harley VR (2003). Forward mandibular positioning up-
orthodontic forces. In: Symposia of the Fourth International Congress regulates SOX9 and type II collagen expression in the glenoid fossa. J
of Primatology. Vol. 3. Basel: S. Karger, pp. 180-190. Dent Res 82:725-730.
Moore AW (1959). Observations on facial growth and its clinical Rabie AB, Tang GH, Hägg U (2004). Cbfa1 couples chondrocytes
significance. Am J Orthod 45:397-423. maturation and endochondral ossification in rat mandibular condylar
Murray PDF (1963). Adventitious (secondary) cartilage in the chick, and the cartilage. Arch Oral Biol 49:109-118.
development of certain bones and articulation in the chick skull. Aust J Rafferty KL, Herring SW (1999). Craniofacial sutures: morphology, growth
Zool 11:368-430. and in vivo masticatory strains. J Morphol 242:167-179.
Murray PDF, Smiles M (1965). Factors in the evocation of adventitious Ricketts RM (1960). The influence of orthodontic treatment on facial
(secondary) cartilage in the chick embryo. Aust J Zool 13:351-382. growth and development. Angle Orthod 30:103-133.
Nanda R (1978). Protraction of maxilla in rhesus monkeys by controlled Roberts WE, Jee WS (1974). Cell kinetics of orthodontically-stimulated and
extraoral forces. Am J Orthod 74:121-141. non-stimulated periodontal ligament in the rat. Arch Oral Biol 19:17-
Nelson C, Harkness M, Herbison P (1993). Mandibular changes during 21.
functional appliance treatment. Am J Orthod Dentofacial Orthop Roth DA, Longaker MT, McCarthy JG, Rosen DM, McMullen HF, Levine,
104:153-161. JP, et al. (1997). Studies in cranial suture biology: Part I. Increased
Ngan P, Hägg U, Yiu C, Merwin D, Wei SH (1996). Soft tissue and immunoreactivity for TGF-beta isoforms (beta1, beta2, and beta3)
dentoskeletal profile changes associated with maxillary expansion and during rat cranial suture fusion. J Bone Min Res 12:311-321.
protraction headgear treatment. Am J Orthod Dentofacial Orthop Rousseau F, Bonaventure J, Legeai-Mallet L, Pelet A, Rozet JM, Maroteaux
109:38-49. P, et al. (1994). Mutations in the gene encoding fibroblast growth factor
Ngan P, Yiu C, Hu A, Hägg U, Wei SH, Gunel E (1998). Cephalometric and receptor-3 in achondroplasia. Nature 371:252-254.
occlusal changes following maxillary expansion and protraction. Eur J Ruf S, Pancherz H (1998). Temporomandibular joint growth adaptation in
Orthod 20:237-254. Herbst treatment: a prospective magnetic resonance imaging and
O'Brien K, Wright J, Conboy F, Sanjie Y, Mandall N, Chadwick S, et al. cephalometric Roentgenographic study. Eur J Orthod 20:375-388.
(2003). Effectiveness of early orthodontic treatment with the Twin- Sandy JR, Farndale RW, Meikle MC (1993). Recent advances in
block appliance: a multicenter, randomized, controlled trial. Part 1: understanding mechanically induced bone remodeling and their
Dental and skeletal effects. Am J Orthod Dentofacial Orthop 124:234- relevance to orthodontic theory and practice. Am J Orthod Dentofacial
243. Orthop 103:212-222.
Ogston A (1875). On articular cartilage. J Anat Physiol 10:48-74. Shen G, Darendeliler MA (2005). The adaptive remodeling of condylar
Ogston A (1878). The growth and maintenance of the articular ends of adult cartilage—a transition from chondrogenesis to osteogenesis. J Dent Res
bones. J Anat 12:503-517. 84:691-699.
Opperman LA, Nolen AA, Ogle RC (1997). TGF-beta1, TGF-beta2 and Shiang R, Thompson LM, Zhu YZ, Church DM, Fielder TJ, Bocian M, et
TGF-beta3 exhibit distinct patterns of expression during cranial suture al. (1994). Mutations in the transmembrane domain of FGFR3 cause
formation and obliteration in vivo and in vitro. J Bone Min Res 12:301- the most common genetic form of dwarfism, achondroplasia. Cell
310. 78:335-342.
Opperman LA, Chhabra A, Nolen AA, Bao Y, Ogle RC (1998). Dura mater Smalley WM, Shapiro PA, Hohl TH, Kokich VG, Brånemark PI (1988).
maintains rat cranial sutures in vitro by regulating suture cell Osseointegrated titanium implants for maxillofacial protraction in
proliferation and collagen production. J Craniofac Genet Dev Biol monkeys. Am J Orthod Dentofacial Orthop 94:285-295.
18:150-158. Sproule WR (1968). Dentofacial changes produced by extraoral cervical
Pancherz H (1979). Treatment of class II malocclusions by jumping the bite traction to the maxilla of Macaca mulatta; a histologic and serial
with the Herbst appliance. A cephalometric investigation. Am J Orthod cephalometric study [MSD thesis]. Seattle: University of Washington.
76:423-442. Stockli PW, Willert HG (1971). Tissue reactions in the temporomandibular
Pancherz H (1982). The mechanism of Class II correction in Herbst joint resulting from anterior displacement of the mandible in the
appliance treatment. A cephalometric investigation. Am J Orthod monkey. Am J Orthod 60:142-155.
82:104-113. Takada K, Petdachai S, Sakuda M (1993). Changes in dentofacial
Paulsen HU (1997). Morphological changes in the TMJ condyles of 100 morphology in skeletal Class III children treated by a modified
patients treated with the Herbst appliance in the period of puberty to maxillary protraction headgear and a chin cup: a longitudinal
adulthood: a long-term radiographic study. Eur J Orthod 19:657-668. cephalometric appraisal. Eur J Orthod 15:211-221.
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
24 Meikle J Dent Res 86(1) 2007
Tang GH, Rabie AB, Hägg U (2004). Indian hedgehog: a mechano- J Orthod Dentofacial Orthop 113:62-72.
transduction mediator in condylar cartilage. J Dent Res 83:434-438. Turley P, Shapiro PA, Moffett BC (1980). The loading of bioglass-coated
Tewson DH, Heath JK, Meikle MC (1988). Biochemical and aluminium oxide implants to produce sutural expansion of the
autoradiographic evidence that anterior mandibular displacement in the maxillary complex in the pigtail monkey (Macaca nemestrina). Arch
young growing rat does not stimulate cell proliferation or matrix Oral Biol 25:459-469.
formation at the mandibular condyle. Arch Oral Biol 33:99-107. Vortkamp A, Lee K, Lanske B, Segre GV, Kronenberg HM, Tabin CJ
Todd TW, Lyon DW (1924). Endocranial suture closure, its progress and (1996). Regulation of rate of cartilage differentiation by Indian
age relationship. I. Adult males of white stock. Am J Phys Anthrop hedgehog and PTH-related protein. Science 273:613-621.
7:325-384. Wagemans PA, van de Velde JP, Kuijpers-Jagtman AM (1988). Sutures and
Todd TM, Lyon DW (1925). Cranial suture closure. Its progress and age forces: a review. Am J Orthod Dentofacial Orthop 94:129-141.
relationship. Part II. Ectocranial closure in adult males of white stock. Watson WG (1972). A computerized appraisal of the high-pull face-bow.
Am J Phys Anthrop 8:23-45. Am J Orthod 62:561-579.
Tonge EA, Heath JK, Meikle MC (1982). Anterior mandibular displacement Wehrbein H, Yildizhan F (2001). The mid-palatal suture in young adults. A
and condylar growth. An experimental study in the rat. Am J Orthod radiological-histological investigation. Eur J Orthod 23:105-114.
82:277-287. Weislander L (1974). The effect of force on craniofacial development. Am J
Triftshauser R, Walters RD (1976). Cervical traction of the maxillae in the Orthod 65:531-538.
Macaca mulatta monkey using heavy orthopedic force. Angle Orthod Weislander L (1975). Early or late cervical traction therapy of Class II
46:37-46. malocclusion in the mixed dentition. Am J Orthod 67:432-439.
Tsolakis AI, Spyropoulos MN (1997). An appliance designed for Weislander L (1984). Intensive treatment of severe Class II malocclusions
experimental mandibular hyperpropulsion in rats. Eur J Orthod 19:1-7. with a headgear-Herbst appliance in the early mixed dentition. Am J
Tsolakis AI, Spyropoulos MN, Katsavrias E, Alexandridis K (1997). Effects Orthod 86:1-13.
of altered mandibular function on mandibular growth after Wertz RA (1970). Skeletal and dental changes accompanying rapid
condylectomy. Eur J Orthod 19:9-19. midpalatal suture opening. Am J Orthod 58:41-66.
Tuenge RH, Elder JR (1974). Posttreatment changes following extraoral Wisth PJ, Tritrapunt A, Rygh P, Boe OE, Norderval K (1987). The effect of
high-pull traction to the maxilla of Macaca mulatta. Am J Orthod maxillary protraction on front occlusion and facial morphology. Acta
66:618-644. Odontol Scand 45:227-237.
Tulloch JF, Phillips C, Koch G, Proffit WR (1997a). The effect of early Woodside DG, Metaxas A, Altuna G (1987). The influence of functional
intervention on skeletal pattern in Class II malocclusion: a randomized appliance therapy on glenoid fossa remodeling. Am J Orthod
clinical trial. Am J Orthod Dentofacial Orthop 111:391-400. Dentofacial Orthop 92:181-198.
Tulloch JF, Proffit WR, Phillips C (1997b). Influences on the outcome of Wright DM, Moffett BC (1974). The postnatal development of the human
early treatment for Class II malocclusion. Am J Orthod Dentofacial temporomandibular joint. Am J Anat 141:235-249.
Orthop 111:533-542. Wu Q, Zhang Y, Chen Q (2001). Indian hedgehog is an essential component
Tulloch JF, Phillips C, Proffit WR (1998). Benefit of early Class II of mechanotransduction complex to stimulate chondrocyte
treatment: progress report of a two-phase randomized clinical trial. Am proliferation. J Biol Chem 276:35290-35296.
Downloaded from jdr.sagepub.com at PONTIFICIA UNIVERSIDAD CATOLICA DE CHILE on September 22, 2014 For personal use only. No other uses without permission.
International and American Associations for Dental Research
You might also like
- Biology of Tooth MovementDocument16 pagesBiology of Tooth MovementLanaNo ratings yet
- Biology of Orthodontic Tooth MovementDocument16 pagesBiology of Orthodontic Tooth MovementGowri ShankarNo ratings yet
- Bone Remodelling: Scientific SectionDocument7 pagesBone Remodelling: Scientific SectionRohini TondaNo ratings yet
- J Tissue Eng Regen Med - 2014 - Detsch - The Role of Osteoclasts in Bone Tissue EngineeringDocument17 pagesJ Tissue Eng Regen Med - 2014 - Detsch - The Role of Osteoclasts in Bone Tissue EngineeringVinícius Gabriel da SilvaNo ratings yet
- DPSC-Derived Extracellular Vesicles Promote Rat Jawbone RegenerationDocument9 pagesDPSC-Derived Extracellular Vesicles Promote Rat Jawbone Regenerationc607322000No ratings yet
- Roles of Osteoclasts in Alveolar Bone RemodelingDocument18 pagesRoles of Osteoclasts in Alveolar Bone RemodelingYogi Ajik YNo ratings yet
- Bone Remodeling Process: Mechanics, Biology, and Numerical ModelingFrom EverandBone Remodeling Process: Mechanics, Biology, and Numerical ModelingNo ratings yet
- J DENT RES 2009 Krishnan 597 608Document12 pagesJ DENT RES 2009 Krishnan 597 608Jenny ColombeauNo ratings yet
- Zhu 2021Document31 pagesZhu 2021Nazmi ZegarraNo ratings yet
- Ossseointegration of Impl.Document11 pagesOssseointegration of Impl.Claudiu CampeanNo ratings yet
- Osteoblasts, Osteoclasts, and Osteocytes: Unveiling Their Intimate-Associated Responses To Applied Orthodontic ForcesDocument12 pagesOsteoblasts, Osteoclasts, and Osteocytes: Unveiling Their Intimate-Associated Responses To Applied Orthodontic ForcesMariya NazimNo ratings yet
- Gene Expression Profile Altered by Orthodontic Tooth Movement During Healing of Surgical Alveolar Defect.Document9 pagesGene Expression Profile Altered by Orthodontic Tooth Movement During Healing of Surgical Alveolar Defect.Angie AriasNo ratings yet
- Primary Role of Functional Matrices in Facial GrowthDocument12 pagesPrimary Role of Functional Matrices in Facial GrowthPranshu MathurNo ratings yet
- Multiscale Modeling of Bone Tissue MechanobiologyDocument12 pagesMultiscale Modeling of Bone Tissue MechanobiologyLina AvilaNo ratings yet
- Ojsadmin, 4Document5 pagesOjsadmin, 4janeNo ratings yet
- 1985 Australian Orthodontic Journal, MelbourneDocument19 pages1985 Australian Orthodontic Journal, MelbourneMariyamNo ratings yet
- NIH Public Access: Author ManuscriptDocument23 pagesNIH Public Access: Author ManuscriptBastion ReinhartNo ratings yet
- ImplantDocument46 pagesImplantMosica VladNo ratings yet
- Perez Et Al. - 2018 - Tissue Engineering and Cell-Based Therapies For Fractures and Bone DefectsDocument23 pagesPerez Et Al. - 2018 - Tissue Engineering and Cell-Based Therapies For Fractures and Bone DefectsAlif FakhriNo ratings yet
- Why MechanobiologyDocument14 pagesWhy MechanobiologyNICOLAS CARVANo ratings yet
- 3Document12 pages3kris.halim1997No ratings yet
- Skeletal and Dental Considerations in OrthodonticDocument11 pagesSkeletal and Dental Considerations in OrthodonticZaid DewachiNo ratings yet
- A Comparative Study On Complete and ImDocument8 pagesA Comparative Study On Complete and ImAbraham Gomez BautistaNo ratings yet
- Advances in Biology of Orthodontic Tooth Movement - A ReviewDocument10 pagesAdvances in Biology of Orthodontic Tooth Movement - A ReviewMarwan AlareqiNo ratings yet
- Regional Acceleratory Phenomenon: Carlalberta VernaDocument8 pagesRegional Acceleratory Phenomenon: Carlalberta VernaPoramate PITAK-ARNNOPNo ratings yet
- Bone Mechanical Properties in Healthy and Diseased StatesDocument31 pagesBone Mechanical Properties in Healthy and Diseased StatesThauane MaiaNo ratings yet
- A Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthDocument17 pagesA Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthErnest Gabriel Cruz AdvinculaNo ratings yet
- Biology Tooth MovementDocument8 pagesBiology Tooth MovementMargarita Lopez MartinezNo ratings yet
- BP MecanismDocument14 pagesBP MecanismAdryana StefyNo ratings yet
- Orthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFrom EverandOrthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFederico BrugnamiNo ratings yet
- Maxillary Sinus Bone GraftingDocument181 pagesMaxillary Sinus Bone GraftingTuấn Hành TrầnNo ratings yet
- Osseteointegration of Dental ImplantDocument24 pagesOsseteointegration of Dental ImplantFajar Kusuma Dwi KurniawanNo ratings yet
- 1 s2.0 S1607551X17307647 Main PDFDocument8 pages1 s2.0 S1607551X17307647 Main PDFindrayaniNo ratings yet
- 393-Article Text-823-1-10-20210420.id - enDocument6 pages393-Article Text-823-1-10-20210420.id - ensittymasitaNo ratings yet
- Changes in Bone Metabolisim Around Osseointegrated Implants Under LoadingDocument17 pagesChanges in Bone Metabolisim Around Osseointegrated Implants Under LoadingAomChanumpornNo ratings yet
- Craniofacial Bone Grafting Wolff's Law RevisitedDocument13 pagesCraniofacial Bone Grafting Wolff's Law RevisitedR KNo ratings yet
- Functional Matrix HypothesisDocument14 pagesFunctional Matrix Hypothesispriyab710No ratings yet
- Alveolar BoneDocument18 pagesAlveolar BoneGabriela ChapaNo ratings yet
- Foc 2003 14 2 9Document8 pagesFoc 2003 14 2 9Andy HongNo ratings yet
- Maxilary Sinus Graft ArunDocument181 pagesMaxilary Sinus Graft ArunJose Fernando Fragozo MendozaNo ratings yet
- Healing of Tooth Extraction Socket: Dr. Pankaj Datta Dr. Shilpa Khullar Dr. Mittal ADocument3 pagesHealing of Tooth Extraction Socket: Dr. Pankaj Datta Dr. Shilpa Khullar Dr. Mittal AwatidinaNo ratings yet
- Journal of The World Federation of OrthodontistsDocument7 pagesJournal of The World Federation of Orthodontistsvighanesh kadamNo ratings yet
- Bone Regeneration in Implant Dentistry Which Are TDocument30 pagesBone Regeneration in Implant Dentistry Which Are TLEONARDO ALBERTO CRESPIN ZEPEDANo ratings yet
- Reference and Techniques Used in Alveolar Bone ClassificationDocument5 pagesReference and Techniques Used in Alveolar Bone ClassificationAna Carolina LoyolaNo ratings yet
- Biology of Tooth Movement - Ortho / Orthodontic Courses by Indian Dental AcademyDocument62 pagesBiology of Tooth Movement - Ortho / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Materials 14 04224 v3Document16 pagesMaterials 14 04224 v3B01Aadarsh SharmaNo ratings yet
- Recent Advances in Orthodontic Tooth MovementDocument19 pagesRecent Advances in Orthodontic Tooth MovementNaveenNo ratings yet
- Accelerated Orthodontic Tooth Movement: Molecular MechanismsDocument13 pagesAccelerated Orthodontic Tooth Movement: Molecular MechanismsMonojit DuttaNo ratings yet
- Research Paper On BonesDocument5 pagesResearch Paper On Bonesvshyrpznd100% (1)
- HUESOSDocument22 pagesHUESOSmacarena vignaNo ratings yet
- 1 s2.0 S1090023317301260 MainDocument2 pages1 s2.0 S1090023317301260 MainAntonio MartinezNo ratings yet
- Bone Tissue Regeneration and Fracture RepairDocument6 pagesBone Tissue Regeneration and Fracture RepairElizabeth GithinjiNo ratings yet
- Surface Texturing of Implant MaterialsDocument17 pagesSurface Texturing of Implant MaterialsYashi VermaNo ratings yet
- Bone RegenereationDocument15 pagesBone Regenereationhayet debbichNo ratings yet
- Skeletal and Dental Considerations in Orthodontic Treatment Mechanics - A Contemporary ViewDocument10 pagesSkeletal and Dental Considerations in Orthodontic Treatment Mechanics - A Contemporary ViewambersNo ratings yet
- Bisht2021 Article AdvancesInTheFabricationOfScafDocument23 pagesBisht2021 Article AdvancesInTheFabricationOfScafOxy Dental Clinic MakassarNo ratings yet
- Mechanical Properties of Compact Bone Defined by TDocument16 pagesMechanical Properties of Compact Bone Defined by T01fe18bme033No ratings yet
- Functional Matrix HypothesisDocument16 pagesFunctional Matrix HypothesisUddyot ChaudharyNo ratings yet
- 2-Referencias y Tecnicas Usadas en Clasificacion Hueso Alveolar - SeriwatanachaiDocument5 pages2-Referencias y Tecnicas Usadas en Clasificacion Hueso Alveolar - SeriwatanachaimnhjrtbnzbNo ratings yet
- Biological Basis For Orthodontic Tooth MovementDocument31 pagesBiological Basis For Orthodontic Tooth Movementindumathi thevanNo ratings yet
- Roberts, Stephen, BeightonDocument10 pagesRoberts, Stephen, BeightonJulio AbarzuaNo ratings yet
- Roberts, Stephen, BeightonDocument10 pagesRoberts, Stephen, BeightonJulio AbarzuaNo ratings yet
- Treatment Timing and Multidisciplinary Approach in Apert SyndromeDocument6 pagesTreatment Timing and Multidisciplinary Approach in Apert SyndromeJulio AbarzuaNo ratings yet
- 2Document13 pages2Elena PruniciNo ratings yet
- Roberts, Stephen, BeightonDocument10 pagesRoberts, Stephen, BeightonJulio AbarzuaNo ratings yet
- Caring For Infants and Their Families: CraniosynostosisDocument13 pagesCaring For Infants and Their Families: CraniosynostosisJulio AbarzuaNo ratings yet
- Skull Base Embryology ReviewDocument10 pagesSkull Base Embryology ReviewJulio AbarzuaNo ratings yet
- Embriologia Humana y Biologia Del Desarrollo CarlsonDocument14 pagesEmbriologia Humana y Biologia Del Desarrollo CarlsonJulio AbarzuaNo ratings yet
- Caring For Infants and Their Families: CraniosynostosisDocument13 pagesCaring For Infants and Their Families: CraniosynostosisJulio AbarzuaNo ratings yet
- Sajnani, 2015Document8 pagesSajnani, 2015Julio AbarzuaNo ratings yet
- 11Document9 pages11Din PcNo ratings yet
- t2 Cendekiawan 2010 PDFDocument9 pagest2 Cendekiawan 2010 PDFJulio AbarzuaNo ratings yet
- Factors Leading to Maxillary Canine ImpactionDocument7 pagesFactors Leading to Maxillary Canine ImpactionJulio AbarzuaNo ratings yet
- t3 Som 2014 1Document8 pagest3 Som 2014 1Julio AbarzuaNo ratings yet
- Va Medica: Atypical Swallowing: A ReviewDocument11 pagesVa Medica: Atypical Swallowing: A ReviewJulio AbarzuaNo ratings yet
- Topical Review: Sleep Bruxism, Headaches, and Sleep-Disordered Breathing in Children and AdolescentsDocument10 pagesTopical Review: Sleep Bruxism, Headaches, and Sleep-Disordered Breathing in Children and AdolescentsJulio AbarzuaNo ratings yet
- Sajnani, 2015Document8 pagesSajnani, 2015Julio AbarzuaNo ratings yet
- Andersson El Al%2ssssssc 2012Document8 pagesAndersson El Al%2ssssssc 2012Julio AbarzuaNo ratings yet
- DR. J. A. SALZMANN'S Department of Orthodontic Abstracts and ReviewsDocument6 pagesDR. J. A. SALZMANN'S Department of Orthodontic Abstracts and ReviewsNataly ComettaNo ratings yet
- Factors Leading to Maxillary Canine ImpactionDocument7 pagesFactors Leading to Maxillary Canine ImpactionJulio AbarzuaNo ratings yet
- Frazier-Bowers Et Al, 2016Document11 pagesFrazier-Bowers Et Al, 2016Julio AbarzuaNo ratings yet
- The Gerson TherapyDocument43 pagesThe Gerson Therapyboboacer100% (1)
- ACC8278 Annual Report 2021Document186 pagesACC8278 Annual Report 2021mikeNo ratings yet
- Emergency Preparedness Response PowerpointDocument13 pagesEmergency Preparedness Response PowerpointRandy SianenNo ratings yet
- Module 1 GastroDocument66 pagesModule 1 GastroAngelica AmandoNo ratings yet
- CCRN-PCCN Review RenalDocument11 pagesCCRN-PCCN Review RenalGiovanni MictilNo ratings yet
- Check your well-being with this situations listDocument2 pagesCheck your well-being with this situations listArlen Mae RayosNo ratings yet
- Movement Disorders: Akinetic-Rigid SyndromesDocument8 pagesMovement Disorders: Akinetic-Rigid SyndromesMarwan M.No ratings yet
- Knee Pain Secret RemediesDocument36 pagesKnee Pain Secret RemediesVAIBHAV PHULARE50% (2)
- Case Study (Uti)Document7 pagesCase Study (Uti)Ferreze AnnNo ratings yet
- Nursing Procedure Checklist: Applying A Transdermal PatchDocument2 pagesNursing Procedure Checklist: Applying A Transdermal PatchOrl TrinidadNo ratings yet
- AP Psychology 2010 - 2011 Final Project AssignmentDocument3 pagesAP Psychology 2010 - 2011 Final Project AssignmentKIRUBNo ratings yet
- Transparency Concerns Led To Energy Minister Change: Remembering An Uprising, 25 Years OnDocument88 pagesTransparency Concerns Led To Energy Minister Change: Remembering An Uprising, 25 Years OnThe Myanmar TimesNo ratings yet
- Ra 11058Document69 pagesRa 11058Art Corbe0% (1)
- December IssueDocument104 pagesDecember Issuemiltonwcraft100% (1)
- NRS 2002Document1 pageNRS 2002LunaMarinaAzizahNo ratings yet
- Adding Nitrogen to Corn SilageDocument2 pagesAdding Nitrogen to Corn SilageleegunalNo ratings yet
- Heswall Local May 2012Document40 pagesHeswall Local May 2012Talkabout PublishingNo ratings yet
- Patient Information Gastroesophageal Reflux Disease (Hiatal Hernia and Heartburn)Document7 pagesPatient Information Gastroesophageal Reflux Disease (Hiatal Hernia and Heartburn)Gail AidNo ratings yet
- Nurture Debate Team Open StatementDocument2 pagesNurture Debate Team Open StatementRAQUEL VILLAROSANo ratings yet
- Analysis of Antibacterial Antiinflammatory and Skinwhitening Effect of Centella Asiatica L Urban2018journal of Plant BiotechnologyOpen AccessDocument8 pagesAnalysis of Antibacterial Antiinflammatory and Skinwhitening Effect of Centella Asiatica L Urban2018journal of Plant BiotechnologyOpen AccessRika DestianaNo ratings yet
- APPLY TAFE NSW COURSESDocument4 pagesAPPLY TAFE NSW COURSESiltiNo ratings yet
- Annotated BibliographyDocument9 pagesAnnotated Bibliographyapi-340697796No ratings yet
- Houghton Hocut 795 - BDocument5 pagesHoughton Hocut 795 - BErwinNo ratings yet
- Mojwh 08 00237Document9 pagesMojwh 08 00237EndalkNo ratings yet
- Credentialing Application Form MichDocument5 pagesCredentialing Application Form MichHarlyn MagsinoNo ratings yet
- Drug Calculations 2015Document35 pagesDrug Calculations 2015Anonymous DWMeAjhD1cNo ratings yet
- Technical Proposal - RFP 044-2023Document20 pagesTechnical Proposal - RFP 044-2023Nadya AlizaNo ratings yet
- R104 - Fire Protection SystemsDocument11 pagesR104 - Fire Protection SystemsMariel Paz MartinoNo ratings yet
- Entendimiento de Los Datos DisponiblesDocument10 pagesEntendimiento de Los Datos DisponiblesJose Miguel González PeraltaNo ratings yet
- Clostridium Tetani NotesDocument10 pagesClostridium Tetani NotesGame GameNo ratings yet
- Sustainable Rural Development-Andrew Shepherd (Auth.) - (1998)Document305 pagesSustainable Rural Development-Andrew Shepherd (Auth.) - (1998)Jackelinne CerqueraNo ratings yet