Professional Documents
Culture Documents
DALY 2013 Revisado PDF
DALY 2013 Revisado PDF
Uploaded by
Andre CostaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DALY 2013 Revisado PDF
DALY 2013 Revisado PDF
Uploaded by
Andre CostaCopyright:
Available Formats
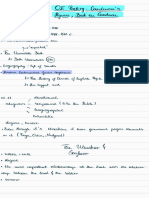
Personal View
Estimating the true global burden of mental illness
Daniel Vigo, Graham Thornicroft, Rifat Atun
We argue that the global burden of mental illness is underestimated and examine the reasons for under-estimation Lancet Psychiatry 2016;
to identify five main causes: overlap between psychiatric and neurological disorders; the grouping of suicide and 3: 171–78
self-harm as a separate category; conflation of all chronic pain syndromes with musculoskeletal disorders; Department of Global Health
and Population, Harvard T.H.
exclusion of personality disorders from disease burden calculations; and inadequate consideration of the
Chan School of Public Health,
contribution of severe mental illness to mortality from associated causes. Using published data, we estimate the Harvard University, Boston,
disease burden for mental illness to show that the global burden of mental illness accounts for 32·4% of years MA, USA (D Vigo MD,
lived with disability (YLDs) and 13·0% of disability-adjusted life-years (DALYs), instead of the earlier estimates Prof R Atun FRCP); Waverley
Place Program, Psychotic
suggesting 21·2% of YLDs and 7·1% of DALYs. Currently used approaches underestimate the burden of mental
Disorder Division, McLean
illness by more than a third. Our estimates place mental illness a distant first in global burden of disease in terms Hospital, Belmont, MA, USA
of YLDs, and level with cardiovascular and circulatory diseases in terms of DALYs. The unacceptable apathy of (D Vigo); and Centre for Global
governments and funders of global health must be overcome to mitigate the human, social, and economic costs of Mental Health, Institute of
Psychiatry, Psychology and
mental illness. Neuroscience, King’s College,
London, UK
Introduction nosology of disorders, but aim to better gauge the disease (Prof G Thornicroft PhD)
Mental health is defined by WHO as “a state of well-being burden of mental illness. An important benefit of a new Correspondence to:
in which every individual realizes his or her own GBD estimation is to inform prioritisation of health Prof Rifat Atun, Department of
Global Health and Population,
potential, can cope with the normal stresses of life, can needs and resource allocation, so our aim is to provide
Harvard T.H. Chan School of
work productively and fruitfully, and is able to make a decision makers, who rely on specialists to design and Public Health, Harvard
contribution to her or his community”.1 This state, implement policies, with a new set of assumptions and University, Boston, MA, USA
however, is disrupted in one of every three individuals— tools to produce more accurate estimations using existing ratun@hsph.harvard.edu
or more—during their lifetimes.2,3 data.
Worldwide the magnitude of mental illness has been
emphasised by studies on the global burden of disease.4 Burden of mental illness: measurement
Yet, in spite of the very considerable burden and their challenges
associated adverse human, economic, and social effects, We argue that the burden of mental illness has been
global policy makers and funders have so far failed to underestimated due to five reasons: the overlap between
prioritise treatment and care of people with mental psychiatric and neurological disorders; the grouping of
illness.5,6 Consequently, people with mental illness suicide and behaviours associated with self-injury as a
worldwide are largely neglected.6 Pervasive stigma and separate category outside the boundary of mental illness;
discrimination7,8 contributes, at least in part, to the the conflation of all chronic pain syndromes with
imbalance between the global burden of disease musculoskeletal disorders; the exclusion of personality
attributable to mental disorders, and the attention these disorders in mental illness disease burden calculations;
conditions receive. Stigma, embodied in discriminatory and inadequate consideration of the contribution of
social structures, policy, and legislation, produces a severe mental illness to mortality from associated causes.
disparity between services geared to physical health and We discuss each of these measurement issues and
mental health, with lower availability, accessibility, and methodological considerations. Diagnostic classifications
quality of services for the latter.9 such as the ICD-10 system present challenges: they need
Globally, rapid economic, demographic, and epi- to consider both the clinical syndrome and the aetiology
demiological transitions mean a growth in populations of each disorder, with the goal of providing a system that
that are living longer, but with greater morbidity and is meaningful at the individual explanatory and
disability.10–13 Mental disorders are a major driver of the therapeutic levels, considering the presentation of the
growth of overall morbidity and disability globally.14,15 illness as well as its natural history. Further, ICD-11,
Five types of mental illness appear in the top 20 causes which is under development and is expected to be
of global burden of disease (GBD): major depression released in 2018 by the World Health Organization, is
(second), anxiety disorders (seventh), schizophrenia identified by the Advisory Group for ICD-11 as a better
(11th), dysthymia (16th), and bipolar disorder (17th) were method for categorising burden of mental illness than
leading causes of years lived with disability (YLDs) in ICD-10, but without specific mention of improvements
2013.11 In this context, this Personal View aims to: offer a in the estimation of GBD related to mental disorders as a
constructive critique of current estimates of GBD related goal for the revision.16
to mental illness; argue that in aggregate mental illness The GBD estimation framework uses a comprehensive,
is underestimated; and explore an alternative approach to mutually exclusive hierarchical list of disorders based on
produce more realistic GBD estimates of mental the ICD-10 classification mainly for two reasons: to take
disorders worldwide. We do not propose a different advantage of a common nosological language, and to
www.thelancet.com/psychiatry Vol 3 February 2016 171
Personal View
account for 100% of the disease burden without double mental disorder. Suicide and all forms of self-harm,
See Online for appendix counting (appendix). But GBD differs from nosological which are to a large extent imputable to mental disorders,
systems: instead of the individual level, it is mainly are coded under injuries, and are excluded from
concerned with the population level; and instead of calculations of the effect of mental illnesses.10,20,21
informing individual aetiology and therapy, it needs to Ferrari and colleagues21 studied mental disorders as
allow for a better understanding of disease distribution risk factors for suicide by reviewing existing literature,
and transitions, to guide prioritisation of population pooling relative-risk estimates, and then estimating what
health needs and organisation of health services. percentage of deaths by suicide could be causally linked
The actual grouping of disorders used by the GBD—a to several mental disorders (mainly mood and anxiety
hierarchical cause list comprising four levels of disorders, substance misuse, and schizophrenia). After
aggregation—is sometimes based on clinical grounds reviewing the psychological autopsy studies available, the
(such as with cardiovascular and circulatory conditions, a authors assign ceiling values to account for cultural
level 2 aggregation), and sometimes on a mix of disease variability in the causal relation between mental illness
or anatomical criteria (such as diabetes, urogenital, and suicide, and suggest an addition of 22 million DALYs
blood, and endocrine disorders, also level 2).17 amounting to 0·9% of total DALYs to the mental illness
Consideration of more pertinent criteria for aggregation burden. These estimates would have been higher if all
is warranted (appendix). self-harm (suicide, attempted suicide, and self-injurious
behaviour) due to mental illness and sub-syndromal
The psychiatric–neurological interface conditions were included. Ferrari and colleagues reduce
Traditionally, disorders both affecting the central nervous the attribution of lethal self-harm to the mental illness
system and producing mental disorders were divided burden based on two arguments: the authors put a cap of
between psychiatric and neurological conditions: if the 68% to suicides attributable to mental illness taking
syndrome had a clear neuroanatomical or neuro- place in China, India, and Taiwan, which account for
physiological basis it was considered neurological; if not, 50·0% of the world’s suicides, and of 85·0% to those
it was deemed psychiatric. However, this dual distinction happening elsewhere, and they do not include suicides
has more to do with professional areas of competence in the context of sub-syndromal states (eg, impulsive
than scientific logic. For example, schizophrenia, states, which are common in the context of personality
considered a psychiatric disorder, affects the brain’s disorders, also excluded from the GBD).
anatomy and physiology, and secondarily produces the From a clinical and public health perspective we have
cognitive, affective, and behavioural symptoms that three caveats with the approach used by Ferrari and
constitute the mental syndrome. On the other hand, colleagues:21 first, it does not account for non-lethal self-
epilepsy, typically considered a neurological disorder, harm, which includes both attempted suicide and
includes conditions such as temporal-lobe epilepsy, in self-injurious behaviour; second, by excluding suicides in
which a clearly identifiable psychiatric syndrome is the context of sub-syndromic states and restricting the
frequently accompanied by an absence of electro- assessment to specific disorders, it leaves around 25·0%
encephalographic abnormalities. Given that the of the world’s suicides and 39·0% of suicide burden in
nosological classification for these disorders is in flux the category of injuries, along with traffic accidents,
and the division between them is somewhat arbitrary, where they clearly do not belong; and third, the
other criteria should be used when aggregating diseases assignment of a low ceiling due to cultural considerations
for measuring burden. In this respect, in addition to in China, India, and Taiwan is questionable because
their presentation as psychiatric syndromes, these cultural differences could mean that stigma associated
disorders pose a common challenge at the primary care with mental illness but not with suicide leads to under-
level, particularly in low-income and middle-income reporting of the causal link. For example, in China,
countries, and a common grouping would make this suicide has been established as a frequent outcome in
more visible to planners and funders. the context of mental syndromes, even in the absence of
full diagnostic criteria. Case-control studies of non-lethal
Categorising suicide and intentional self-harm attempted suicide have shown that people had
In 2013, mental illness accounted for 21·2% of the YLDs substantially higher stress, impulsiveness, and
worldwide—higher than any other group of conditions.11 aggression, more severe depressive symptoms, and were
However, using the composite measure disability- more likely to meet criteria for a psychiatric diagnosis. Of
adjusted life-years (DALYs), the burden of mental illness the psychological factors, severity of depressive
accounted for 7·1%, ranking fifth overall in terms of symptoms in the two preceding weeks was the most
GBD.18,19 The gap between the burden of mental illness as substantial, to the extent that suicide in China is linearly
measured by years lived with disability and that measured related to severity of depression.22,23 The limitations of the
by DALYs is explained by the fact that DALYs psychological autopsy studies on which Ferrari and
underestimate mental illness mortality due to suicide, to colleagues base their rationale for excluding a third of the
the disease process itself, and to reasons secondary to the global self-harm disease burden from mental disorders
172 www.thelancet.com/psychiatry Vol 3 February 2016
Personal View
allow for a very different conclusion: the existence of a as disorders of the nervous system by the ICD-10
psychiatric diagnosis was established indirectly by classification but should be considered as mental and
interviewing family members, and personality disorders behavioural disorders) or somatoform disorder
were excluded from the assessment, potentially leading (considered as mental and behavioural disorders in
to substantial under-registry.24 In this context, the ICD-10); the prevalence of these pain disorders in
attribution of self-harm—lethal or not—to impulsiveness, patients with a major affective, anxiety, or stress-related
aggression, and availability of a lethal tool, does not disorder exceeds 30%, and in certain samples with
disprove the existence of an underlying mental disorder. post-traumatic stress disorder reaches 80%; and they
The authors draw attention to these limitations, converge with chronic mental illness at the therapeutic
acknowledging that the conventional wisdom that suicide and service delivery level. These caveats suggest the
is almost always the outcome of mental illness will not be existence of subpopulations with a common syndrome,
altered by their studies.25 In other words, the absence of which are difficult to classify from a nosological
unequivocal evidence of the causal link is not evidence of perspective (appendix). We argue that when estimating
absence of a causal link. Hence, the decision to allocate disease burden, it is reasonable to attribute a proportion
disease burden from suicides to injuries or to mental of these conditions to mental illness.
disorders needs to be carefully considered.
In this context, and with insufficient evidence, what is Including people with personality disorders
the preferred choice between different burden estimation Personality disorders are common (4–15% in point
methods? The rationale by Ferrari and colleagues21 to prevalence community surveys)27 and when severe impose
leave all non-lethal self-harm and a quarter of the world’s a substantial burden both at personal, family, community,
suicides—therefore more than a third of self-harm and population levels. People with personality disorders
DALYs—in the injuries aggregation does not seem have shorter life expectancy and higher comorbidity with
justifiable. We find it preferable from a population health other general and mental illnesses than the general
perspective to aggregate all self-injuries with the mental population.27 However, due to the inconsistent quality of
health-related disease burden, with the caveat that it is the evidence, personality disorders were not included in
likely to incorrectly include the burden of suicides that GBD 2013 estimates within the overall category of mental
can be judged to be non-mental health related, such as illness.26 Although a proportion of the disease burden of
assisted suicide (producing a much smaller error than personality disorders might be under the other mental
the alternative approach). and substance use disorders aggregation, this hardly
captures their true relevance and the need to consider
Chronic pain syndromes them in their own right. Another portion, arguably
Musculoskeletal conditions were the second major cause substantial, might be captured under the musculoskeletal
of YLDs11 and seventh ranked cause of DALYs in 2013 aggregation, given that 30% of people diagnosed with
globally.26 These conditions include anatomically based chronic pain syndromes also have personality disorder.28
disorders (such as osteoarthritis and rheumatoid Finally, we have seen that personality traits such as
arthritis), and also syndromes and symptoms (eg, impulsivity and aggression, as well as depressive
fibromyalgia, low back pain) characterised by pain but symptoms, frequently provide the psychological context in
without specific anatomical correlates. The allocation of which self-harm occurs, providing a rationale to aggregate
the burden corresponding to these syndromes in total to self-harm under the mental disorder burden. Though our For the Global Burden of
the musculoskeletal aggregation is problematic because: re-allocation of self-harm and a fraction of chronic pain Disease Study 2013 data
downloads see http://ghdx.
a substantial proportion of these disorders, which (see below) partially recaptures this burden, there is not
healthdata.org/global-burden-
account for up to 6·1% of DALYs globally, should actually enough data to comprehensively account for the burden disease-study-2013-gbd-2013-
be classified as either chronic pain syndrome (considered of personality disorders. data-downloads
Global burden of disease DALYs (%) Reallocating neurological DALYs (%) Reallocating self-harm† DALYs (%) Reallocating chronic pain DALYs (%)
2013 disorders* syndrome‡
Rank 1 Cardiovascular disease 13·5% Cardiovascular disease 13·5% Cardiovascular disease 13·5% Cardiovascular disease 13·5%
Rank 2 Common infections 10·2% Common infections 10·2% Mental Illness 11·2% Mental illness 13·0%
Rank 3 Cancer 8·1% Mental illness 9·8% Common infections 10·2% Common infections 10·2%
Rank 4 Neonatal 7·7% Cancer 8·1% Cancer 8·1% Cancer 8·1%
Rank 5 Mental illness 7·1% Neonatal 7·7% Neonatal 7·7% Neonatal 7·7%
Analysis based on data from Murray and colleagues (2015) and from the Global Burden of Disease Study 2013 data download website. *Neurological disorders repositioned to mental illness: dementias,
19
epilepsy, migraine, tension-type headache (66 872 300 DALYs). †Self-harm repositioned to mental illness: 35 170 400 DALYs. ‡A third of the 131 697 900 DALYs (1·8%) of potential chronic pain syndrome
currently attributed to musculoskeletal disorders is reattributed to mental disorders.
Table 1: Effect of reallocating disability-adjusted life-years (DALYs) of neurological disorders, self-harm, and a fraction of chronic pain syndrome
www.thelancet.com/psychiatry Vol 3 February 2016 173
Personal View
Global burden of YLDs (%) Reallocating YLDs (%) Reallocating self- YLDs (%) Reallocating YLDs (%)
disease 2013 neurological harm† chronic pain
disorders* syndrome‡
Rank 1 Mental illness 21·2% Mental illness 27·2% Mental illness 27·3% Mental illness 32·4%
Rank 2 Musculoskeletal 20·9% Musculoskeletal 20·9% Musculoskeletal 20·9% Musculoskeletal 15·7%
Analysis based on data from Global Burden of Disease Study 2013 Collaborators. *Neurological disorders repositioned to mental illness: dementias, epilepsy, migraine, and
11
tension-type headache (46 579 100 YLDs). †Self-harm repositioned to mental illness: 231 600 YLDs. ‡Applying the same rationale and repositioning the same proportion as
in table 1 from musculoskeletal to mental illness (5·1 percentage points [about a third of 15·7%], which are the YLDs attributable to chronic pain syndromes and other
musculoskeletal disorders, excluding anatomically based lesions).
Table 2: Effect of reallocating years lived with disability (YLDs) of neurological disorders, self-harm, and chronic pain syndrome
Disease burden as percent of mental illness burden
40
Global burden of disease 2013 YLDs
Authors’ estimates 32·4%
30
Mental illness burden (%)
21·2%
20
Missing from global burden of disease
10
0
n
ty
er
er
c p dis ficit
nd r
e
sy
he
rm
ta as
s
he
e
er
tia
LD
lit
ni
us
us
in
sio
rd
rd
ain ord
xie
tis
lep
ac
to ss
ha
rd
re
ra
bi
ro
Ot
en
lY
ro ivity n de
ug
ol
so
iso
es
of llne
Au
ad
An
iso
ph
ig
isa
pi
lf-
h
m
pr
di
Dr
td
E
co
he
Se
zo
ld
gd
sy
ct io
nt al i
De
De
lar
Al
uc
ra nt
hi
pe
ua
rce nt
tin
po
nd
Sc
pe te
ty
ct
pe Me
Ea
Bi
hy At
lle
n-
Co
ni
te
io
ns
In
Ch
Te
Figure 1: Comparison of Global Burden of Disease 2013 years lived with disability (YLDs) with the authors’ estimates
Analysis based on data from Global Burden of Disease Study 2013 Collaborators.11
Premature mortality The result with current methods, which does not count
People with severe mental illness have up to 60% higher excess deaths due to self-harm and increased overall
chances of dying prematurely from non-communicable mortality, is that in the case of mental illness, DALYs are
diseases29 that are neglected because of the underlying basically YLDs. The issue of self-harm can be partially
mental condition. They die 10–20 years younger than addressed through aggregation (see below), but the issue
their peers in high-income countries, and 30 years of increased mortality due to general conditions poses a
younger in low-income countries.30–32 Charlson and very complex challenge. GBD methodology is based on
colleagues33 estimate that up to 8% of years of life lost zero-sum attribution, which means that if a patient with
globally corresponded to excess deaths due to mental schizophrenia suffers a fatal myocardial infarction at age
health-related conditions including dementia, epilepsy, 55 years as a result of smoking, for which she is at
and migraine. A recent systematic review estimated that increased risk, and neglected metabolic syndrome—a
14·3% of deaths worldwide, or about eight million deaths likely consequence of antipsychotic medication—then
each year, are attributable to mental disorders.32 However, her years of life lost will be included in the cardiovascular
mental disorders appear to only account for 0·5% of total DALYs. In the context of increasing non-communicable
years of life lost because GBD estimates only show deaths disease comorbidities, the tradition of attributing
directly attributed to mental disorders recorded in death mortality to a single disease should be reassessed, and
certificates (mostly due to schizophrenia and substance alternative approaches explored, such as partial attribution
misuse), which leads to zero global deaths attributed to of years of life lost resulting from a single death to
bipolar disorder, depression, and other mental illnesses. different frequently co-occurring disorders.
174 www.thelancet.com/psychiatry Vol 3 February 2016
Personal View
40
Disease burden as percent of mental illness burden
Global burden of disease 2013 DALYs
Authors’ estimates
30
Mental illness burden (%)
20
Missing from global burden of disease
13·0%
10
7·1%
0
n
er
er
ivi n rs
so it
er
rm
he
l D as
Ys
he
er
er
er
tia
lit
ps
ni
in
sio
di fic
ra nt rde
rd
rd
rd
ru
AL
ac
ta s
ha
rd
rd
rd
re
ra
bi
ro
Ot
ile
to es
en
ty de
so
iso
ct
es
ad
so
iso
so
pe te so
ph
ig
isa
nd
lf-
of illn
Ep
e
m
pr
di
td
he
sp
di
di
hy At g di
Se
zo
ld
ed
sy
ct io
De
De
lar
nt tal
uc
ty
m
hi
pe
ua
se
ain
us
tin
po
xie
rce en
nd
Sc
tis
lu
ty
ct
ug
cp
Ea
Bi
pe M
lle
Au
n-
An
Co
ho
Dr
ni
te
io
co
ro
ns
In
Al
Ch
Te
Figure 2: Comparison of Global Burden of Disease 2013 disability-adjusted life-years (DALYs) with the authors’ estimates
Analysis based on data from GBD 2013 DALYs and HALE Collaborators.19
Revising DALYs (2013) estimates for mental illness Considering that a fraction of low back, neck pain,
For the reasons set out above we propose that when and 50% of other musculoskeletal pain potentially
estimating disease burden, certain neurological corresponds to chronic pain syndromes, and for the
syndromes (ie, the dementias, epilepsy, tension-type purposes of producing a more accurate estimation and
headache, and migraine) should be aggregated within stimulating debate, we assume given the limited data
the overall category of mental illness. This adjustment that one third (rather than zero percent, as it is now) of
would move the total rank of mental illnesses in the the disease burden of these pain syndromes is
GBD tables from fifth to third place overall, accounting potentially attributable to mental disorders and explore
for 9·8% of DALYs globally (table 1). Repositioning all the effect on mental illness burden calculations:
DALYs related to self-harm from the category of injuries re-allocating 1·8% of global DALYs would increase
to mental health would increase the number of DALYs mental illness burden from 11·2% (with certain
from 9·8% to 11·2%, placing it second in the ranking neurological disorders and self-harm added) to 13·0%
(table 1). of total, practically tied with all cardiovascular and
Chronic pain syndromes can potentially account for a circulatory disorders, which account for 13·5% (table 1).
substantial fraction of the 5·4% of DALYs currently
attributed to low back, neck pain plus other Revising YLDs (2013) estimates for mental illness
musculoskeletal pain, once we exclude entities for In 2013, mental illness accounted for 21·2% of global
which there is evidence of a musculoskeletal critical YLDs, 3·5 times greater than the disability associated
mechanistic level (such as arthritides and gout). As with all infectious diseases (6·0% of YLDs), four times
shown in the appendix, a proportion of the burden that for all injuries combined (5·0% of YLDs), eight times
resulting from these syndromes should be aggregated the disability associated with all cardiovascular and
to the mental rather than musculoskeletal disorder circulatory diseases (2·8% of YLDs), and 24 times the
burden. However, due to a lack of primary disaggregated disability associated with all cancers (0·9% of YLDs).
data it is not possible to gauge with any precision which Musculoskeletal disorders (plus fractures and soft tissue
portion of the burden of musculoskeletal disorders injuries) accounted for 20·8% of total YLDs.11 As we have
corresponds to these chronic pain syndromes or which argued above, a substantial portion, which we assume to
portion of chronic pain syndrome burden corresponds be 5·1 percentage points (table 2), potentially corresponds
to centrally caused syndromes (and therefore to the to chronic pain syndromes that should not be considered
mental or neurological burden as previously defined). musculoskeletal, but are rooted in the CNS and therefore
www.thelancet.com/psychiatry Vol 3 February 2016 175
Personal View
in non-communicable diseases (combined, accounting
Mental illness 0·4% for 82·0% of YLDs; figure 3),35,37 whereas none of the
MDGs referred to mental illness, which received 0·40%
Non-communicable diseases
1·1%
of the development assistance for health despite
(except mental illness)
accounting for 32·4% of YLDs.
Other infectious diseases
The imbalance between disease burden, financing, and
2·7%
service access is reported in countries of different income
levels (appendix): global median spending in mental
Tuberculosis 3·2%
health stands at 2·8% of total government health
spending, more than two thirds of which is on average
Malaria 5·1%
allocated to neuropsychiatric hospitals in spite of
international evidence-based recommendations for
Unallocable 5·6%
community-based services.29 Low-income countries
Sector-wide approaches and spend a very modest 0·5% of national health budgets on
6·0%
health systems support mental health, with up to 90·0% going to stand-alone
psychiatric institutions that provide, in population terms,
Maternal 9·3% very low rates of treatment (contact) coverage. Although
high-income countries provide more services for mental
Child 16·7% illness than low-income and middle-income countries,
there are variations in accessibility and coverage for
Other 22·9% geographical and socio-economic groups.38–40
HIV 27·0% Discussion
The recent GBD (DALY and YLD) estimates produce an
0 5 10 15 20 25 30
Total development assistance for health (%)
underestimate of the true effect of mental disorders on
populations due to: the overlap between psychiatric and
Figure 3: Development assistance for health per area as a percentage of total (US$372·2 billion) from 2000 to neurological disorders; the grouping of suicide and
2014 behaviours associated with self-injury as a separate
Total funding in 2000–04, $372·2 billion; HIV, $100·4 billion; non-communicable diseases (less mental illness),
$4·0 billion; mental illness, $1·5 billion. Analysis based on data from the Institute for Health Metrics and Evaluation
category outside the boundary of mental illness; the
(2015).35 conflation of all chronic pain syndromes with
musculoskeletal disorders; the exclusion of personality
better understood as part of the burden of mental illness. disorders in mental illness disease burden calculations;
Applying our framework, the new YLD estimation of and inadequate consideration of the contribution of
mental health-related burden is 32·4%. severe mental illness to mortality from associated causes.
Our estimations of disability alone (YLDs) and Using the currently available evidence and specified
combined with mortality (DALYs) show that by assumptions to correct the overlap between psychiatric
excluding certain conditions from the mental illness and neurological disorders, the grouping of suicide and
burden current assessments underestimate both YLDs behaviours associated with self-injury as a separate
and DALYs by more than a third (figures 1 and 2). We category outside the boundary of mental illness, and the
also show that mental illness accounts for a third of the conflation of all chronic pain syndromes with
global disability (table 2), instead of a fifth, as currently musculoskeletal disorders, we provide a more accurate
estimated. picture of mental illnesses as a leading cause of GBD.
Mental disorders—in various forms and intensities—
Disproportionately weak global response to affect most of the population in their lifetime.2,3 In most
mental illness cases, people experiencing mild episodes of depression
The global development assistance for health allocated to or anxiety deal with them in ways that allow them to
mental illness is far below the levels warranted by the continue living a productive life. A substantial minority
effect of these disorders. The Millennium Development of the population, however, experience more disabling
Goals (MDGs)34 prioritised child health (MDG 4), conditions such as schizophrenia, bipolar disorder type I,
maternal health (MDG 5), and communicable diseases severe recurrent depression, and severe personality
(MDG 6), which collectively accounted for 46·9% of disorders. Whereas common mild disorders are
DALYs 25 years ago,18 and attracted most of the amenable to self-management and relatively simple
development assistance for health reaching 68·0% of the educational or support measures, severe mental illness
$35·9 billion disbursed in 2014.35,36 Despite the changing demands complex, multi-level care that might need a
burden of disease, characterised by multi-morbidity and longer-term engagement with the individual, and with
disability,12 from 2000 to 2014 only 1·5% of the the family. Hence, a more nuanced and accurate picture
development assistance for health was invested globally of mental health-related burden is crucial to effectively
176 www.thelancet.com/psychiatry Vol 3 February 2016
Personal View
allocate resources and appropriately design health 4 Lopez AD, Murray CC. The global burden of disease, 1990–2020.
systems in proportion to the nature and the scale of these Nat Med 1998; 4: 1241–43.
5 Bloom DE, Cafiero ET, Jané-Llopis E, et al. The global economic
challenges. burden of noncommunicable diseases. Geneva:
Universal health coverage, identified as a Sustainable World Economic Forum; 2011.
Development Goal,41 offers opportunities for addressing 6 Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for
mental health: scarcity, inequity, and inefficiency. Lancet 2007;
the neglect for mental illnesses, which constitute, along 370: 878–89.
with all cardiovascular plus circulatory disorders (13·0% 7 Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M, and the
and 13·5%, respectively), the leading causes of global INDIGO Study Group. Global pattern of experienced and
anticipated discrimination against people with schizophrenia:
disease burden. Of particular importance is the inclusion a cross-sectional survey. Lancet 2009; 373: 408–15.
of the mental health indicators proposed in the 2015 Global 8 Lasalvia A, Zoppei S, Van Bortel T, et al, and the ASPEN/INDIGO
Reference List of Core Health Indicators42 (appendix). Study Group. Global pattern of experienced and anticipated
The main limitation of this study is the difficulty of discrimination reported by people with major depressive disorder:
a cross-sectional survey. Lancet 2013; 381: 55–62.
quantifying the disease burden associated with 9 Henderson C, Noblett J, Parke H, et al. Mental health-related stigma
personality disorders, excess all-cause mortality in health care and mental health-care settings. Lancet Psychiatry
secondary to mental illness, and chronic pain syndrome 2014; 1: 467–82.
10 Lozano R, Naghavi M, Foreman K, et al. Global and regional
burden as part of the mental illness burden. Regarding mortality from 235 causes of death for 20 age groups in 1990 and
personality disorders and excess all-cause mortality, data 2010: a systematic analysis for the Global Burden of Disease Study
for further evidence-based assumptions are required, so 2010. Lancet 2012; 380: 2095–128.
11 Global Burden of Disease Study 2013 Collaborators. Global,
their contribution remains to be determined. Regarding regional, and national incidence, prevalence, and years lived with
chronic pain syndromes, there is partial evidence to disability for 301 acute and chronic diseases and injuries in
make a scientifically informed assumption that in our 188 countries, 1990–2013: a systematic analysis for the Global
Burden of Disease Study 2013. Lancet 2015; 386: 743–800.
view provides a better estimate than the current 12 Atun R. Transitioning health systems for multimorbidity. Lancet
hypothesis of zero percent attribution. However, the 2015; 386: 721–22.
speculative nature of the portion of the chronic pain 13 Bloom DE. 7 billion and counting. Science 2011; 333: 562–69.
burden considered by the authors to be related to mental 14 Prince M, Patel V, Saxena S, et al. No health without mental health.
Lancet 2007; 370: 859–77.
health—one third—remains hypothetical.
15 Alonso J, Chatterji S, He Y. The burdens of mental disorders:
Globally, achieving effective coverage will demand global perspectives from the WHO World Mental Health Surveys.
concerted global stewardship to increase funding for Cambridge, UK: Cambridge University Press; 2013.
mental illness, better allocate resources, and improve 16 International Advisory Group for the Revision of ICD-10 Mental and
Behavioural Disorders. A conceptual framework for the revision of
integration of services for mental illness with other the ICD-10 classification of mental and behavioural disorders.
health services. World Psychiatry 2011; 10: 86–92.
17 Murray CJL, Ezzati M, Flaxman AD, et al. GBD 2010: design,
Contributors definitions, and metrics. Comprehensive systematic analysis of
DV and RA conceived the study. DV led the analysis with guidance from global epidemiology: definitions, methods, simplification of DALYs,
RA and GT. DV and RA wrote the first draft and the final manuscript and comparative results from the Global Burden of Disease Study
with contribution from GT. All authors have seen and approved the final 2010. Lancet 2012; 380: 2063–66. Appendix.
version of the manuscript. 18 Institute for Health Metrics and Evaluation. Global Burden of
Declaration of interests Disease 2010. Data Vis 2013. http://www.healthdata.org/gbd/data-
visualizations (accessed Dec 27, 2015).
We declare no competing interests.
19 GBD 2013 DALYs and HALE Collaborators. Global, regional, and
Acknowledgments national disability-adjusted life years (DALYs) for 306 diseases and
DV is supported by the Leadership Incubator Fund (Harvard T.H. Chan injuries and healthy life expectancy (HALE) for 188 countries,
School of Public Health) and by the De Fortabat Fellowship (Harvard 1990–2013: quantifying the epidemiological transition. Lancet 2015;
University). GT is supported by the National Institute for Health published online Aug 27. http://dx.doi.org/10.1016/S0140-
Research (NIHR) Collaboration for Leadership in Applied Health 6736(15)61340-X.
Research and Care South London at King’s College London Foundation 20 Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of
Trust. The views expressed are those of the author(s) and not necessarily disease attributable to mental and substance use disorders: findings
those of the National Health Service (NHS), the National Institute for from the Global Burden of Disease Study 2010. Lancet 2013;
382: 1575–86.
Health Research (NIHR), or the Department of Health. GT
acknowledges financial support from the Department of Health via the 21 Ferrari AJ, Norman RE, Freedman G, et al. The burden attributable
to mental and substance use disorders as risk factors for suicide:
NIHR Biomedical Research Centre and Dementia Unit awarded to
findings from the Global Burden of Disease Study 2010. PLoS One
South London and Maudsley NHS Foundation Trust in partnership with 2014; 9: e91936.
King’s College London and King’s College Hospital NHS Foundation
22 Jiang C, Li X, Phillips MR, Xu Y. Matched case-control study of
Trust. GT is supported by the European Union Seventh Framework medically serious attempted suicides in rural China.
Programme (FP7/2007–2013) Emerald project. Shanghai Arch Psychiatry 2013; 25: 22–31.
References 23 Phillips MR, Shen Q, Liu X, et al. Assessing depressive symptoms
1 World Health Organization. Mental health: a state of well-being. in persons who die of suicide in mainland China. J Affect Disord
http://www.who.int/features/factfiles/mental_health/en/ 2007; 98: 73–82.
(accessed Dec 27, 2015). 24 Yang G-H, Phillips MR, Zhou M-G, Wang L-J, Zhang Y-P, Xu D.
2 Ginn S, Horder J. “One in four” with a mental health problem: Understanding the unique characteristics of suicide in China:
the anatomy of a statistic. BMJ 2012; 344: e1302. national psychological autopsy study. Biomed Environ Sci 2005;
3 Steel Z, Marnane C, Iranpour C, et al. The global prevalence of 18: 379–89.
common mental disorders: a systematic review and meta-analysis 25 Phillips MR. Rethinking the role of mental illness in suicide.
1980–2013. Int J Epidemiol 2014; 43: 476–93. Am J Psychiatry 2010; 167: 731–33.
www.thelancet.com/psychiatry Vol 3 February 2016 177
Personal View
26 Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life-years 34 UN. The Millennium Development Goals report. 2015. http://www.
(DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%20
a systematic analysis for the Global Burden of Disease Study 2010. 2015%20rev%20(July%201).pdf (accessed Dec 27, 2015).
Lancet 2012; 380: 2197–223. 35 Institute for Health Metrics and Evaluation. Financing global health
27 Tyrer P, Reed GM, Crawford MJ. Classification, assessment, 2014: shifts in funding as the MDG era closes. 2015.
prevalence, and effect of personality disorder. Lancet 2015; DOI: 10.1377/hlthaff.26.4.921.
385: 717–26. 36 Atun R. Decisive action to end apathy and achieve 25×25 NCD
28 Sansone RA, Sansone LA. Chronic pain syndromes and borderline targets. Lancet 2014; 384: 384–85.
personality. Innov Clin Neurosci 2012; 9: 10–14. 37 Eaton J, McCay L, Semrau M, et al. Scale up of services for mental
29 WHO. Mental health action plan 2013–2020. Geneva: World Health health in low-income and middle-income countries. Lancet 2011;
Organization; 2013. 378: 1592–603.
30 Lawrence D, Hancock KJ, Kisely S. The gap in life expectancy from 38 WHO. The mental health context—mental health policy and service
preventable physical illness in psychiatric patients in Western guidance package. Geneva: World Health Organization; 2003.
Australia: retrospective analysis of population based registers. BMJ 39 WHO. WHO mental health atlas. Geneva: World Health
2013; 346: f2539. Organization; 2011.
31 Fekadu A, Medhin G, Kebede D, et al. Excess mortality in severe 40 PAHO. Strategy and plan of action on mental health. Washington
mental illness: 10-year population-based cohort study in rural DC: Pan American Health Organization; 2009.
Ethiopia. Br J Psychiatry 2015; 206: 289–96. 41 UN. Resolution adopted by the General Assembly on 27 July 2012.
32 Walker ER, McGee RE, Druss BG. Mortality in mental disorders 2012. http://www.un.org/ga/search/view_doc.asp?symbol=A/
and global disease burden implications: a systematic review and RES/66/288&Lang=E (accessed Dec 27, 2015).
meta-analysis. JAMA Psychiatry 2015; 72: 334–41. 42 WHO Department of Health Statistics and Information Systems.
33 Charlson FJ, Baxter AJ, Dua T, Degenhardt L, Whiteford HA, Vos T. 2015 global reference list of 100 core health indicators. Geneva:
Excess mortality from mental, neurological and substance use World Health Organization; 2015.
disorders in the Global Burden of Disease Study 2010.
Epidemiol Psychiatr Sci 2015; 24: 121–40.
178 www.thelancet.com/psychiatry Vol 3 February 2016
You might also like
- Economics Desire IAS MindmapDocument115 pagesEconomics Desire IAS MindmapShimla95% (21)
- Inclusive Education in The Philippines: Study Guide For Module No. 1 (Las 2)Document9 pagesInclusive Education in The Philippines: Study Guide For Module No. 1 (Las 2)Maia GabrielaNo ratings yet
- Van Os J, Kapur S. Schizophrenia - Lancet 2009 374 635-45 PDFDocument11 pagesVan Os J, Kapur S. Schizophrenia - Lancet 2009 374 635-45 PDFVictorVeroneseNo ratings yet
- Doyle, Kant, Liberal LegaciesDocument32 pagesDoyle, Kant, Liberal LegaciesMatheus LamahNo ratings yet
- Andrews G.2000Document9 pagesAndrews G.2000Gitdistra Cøøl MusiçiañsNo ratings yet
- No Health Without Mental Health PDFDocument19 pagesNo Health Without Mental Health PDFAmany IbrahimNo ratings yet
- SSM - Population Health: ArticleDocument11 pagesSSM - Population Health: ArticleRezky PradessetyaNo ratings yet
- Gender 1Document15 pagesGender 1MiEtaineNo ratings yet
- Vacarolis Chapter OutlinesDocument181 pagesVacarolis Chapter Outlinesamashriqi100% (1)
- Violencia y Trastornos MentalesDocument12 pagesViolencia y Trastornos MentalesPSIQUIATRIA HEJENo ratings yet
- Why Does The Burden of Disease Persist Relating THDocument10 pagesWhy Does The Burden of Disease Persist Relating THArina CismaruNo ratings yet
- Suicide Prevention in Psychiatric PatientsDocument11 pagesSuicide Prevention in Psychiatric PatientsDaniela DiazNo ratings yet
- Evaluation of Depression and Coping Skill Among HIV-Positive People in Kolkata, IndiaDocument6 pagesEvaluation of Depression and Coping Skill Among HIV-Positive People in Kolkata, IndiaAFINA AZIZAHNo ratings yet
- Mental Health Is Biological Health. Why Tackling Diseases of The Mind Is An Imperative For Biological Anthropology in The 21st CenturyDocument31 pagesMental Health Is Biological Health. Why Tackling Diseases of The Mind Is An Imperative For Biological Anthropology in The 21st CenturyWalter VillalobosNo ratings yet
- World Psychiatry - 2021 - Fusar Poli - Preventive Psychiatry A Blueprint For Improving The Mental Health of Young PeopleDocument22 pagesWorld Psychiatry - 2021 - Fusar Poli - Preventive Psychiatry A Blueprint For Improving The Mental Health of Young PeopleCinthia Edith Sariñana NúñezNo ratings yet
- C5 Anxiety Disorders and General Medical ConditionsDocument9 pagesC5 Anxiety Disorders and General Medical ConditionsMilagros Saavedra RecharteNo ratings yet
- Artículo Evidencia de Recaídas (Hardelveld)Document8 pagesArtículo Evidencia de Recaídas (Hardelveld)María CastilloNo ratings yet
- Suicide and Mental HealthDocument3 pagesSuicide and Mental HealthAmar narayanNo ratings yet
- 5 Western Models For Mental Health BentallDocument4 pages5 Western Models For Mental Health BentallimanuelcNo ratings yet
- Saraceno B Freeman M Funk M. PUBLIC MENTAL HEALTHDocument20 pagesSaraceno B Freeman M Funk M. PUBLIC MENTAL HEALTHenviosmentalmedNo ratings yet
- Bipolaridad 1Document12 pagesBipolaridad 1JambisNo ratings yet
- Kirkbridge Et Al - 2024 - The Social Determinants of Health and DisorderDocument33 pagesKirkbridge Et Al - 2024 - The Social Determinants of Health and DisorderVictor Hugo Loaiza SeguraNo ratings yet
- Definitions of Mental IllnessDocument2 pagesDefinitions of Mental Illnessgivemore hoveNo ratings yet
- Change in Communities Resolving A Crisis 1Document21 pagesChange in Communities Resolving A Crisis 1api-410237738No ratings yet
- 2018 Scientific ReportDocument10 pages2018 Scientific ReportAlfredo Martin Blasco CabreraNo ratings yet
- Fpsyt 11 565239Document16 pagesFpsyt 11 565239Moira LudwigNo ratings yet
- DialoguesClinNeurosci 11 7 PDFDocument14 pagesDialoguesClinNeurosci 11 7 PDFTry Wahyudi Jeremi LoLyNo ratings yet
- Lifestyle Medicine - 2021 - PiotrowskiDocument12 pagesLifestyle Medicine - 2021 - PiotrowskiDavidConversNo ratings yet
- Basic Research: Psycho-OncologyDocument10 pagesBasic Research: Psycho-OncologyDivia RainaNo ratings yet
- Cure Therapeutics and Strategic Prevention: Raising The Bar For Mental Health ResearchDocument7 pagesCure Therapeutics and Strategic Prevention: Raising The Bar For Mental Health ResearchShivaniDewanNo ratings yet
- Bipolar Lancet 2015Document12 pagesBipolar Lancet 2015Javier Alonso Jara CánovasNo ratings yet
- The Need For Mental Health Promotion: Helen HerrmanDocument7 pagesThe Need For Mental Health Promotion: Helen Herrmanshah khalidNo ratings yet
- Shukla-Rishi2018 Article HealthLocusOfControlPsychosociDocument8 pagesShukla-Rishi2018 Article HealthLocusOfControlPsychosociMarie McFressieNo ratings yet
- 10 1016@j Jad 2020 04 048Document5 pages10 1016@j Jad 2020 04 048VIA RUSTIANINo ratings yet
- Current Psychosomatic Practice: Special ArticleDocument18 pagesCurrent Psychosomatic Practice: Special Articlere septian IlhamsyahNo ratings yet
- WPS 19 360Document21 pagesWPS 19 360Stella LenzNo ratings yet
- Mental Health in The US Student Name Institution: Course: InstructorDocument5 pagesMental Health in The US Student Name Institution: Course: Instructorcofoje9006No ratings yet
- Mental Health Effect To The FamilyDocument10 pagesMental Health Effect To The FamilyJamie CalaguasNo ratings yet
- Mental Illness Is Like Any Other Medical IllnessDocument9 pagesMental Illness Is Like Any Other Medical IllnessSunny ValeNo ratings yet
- PsychopathologyDocument24 pagesPsychopathologySwarn Raj SahukariNo ratings yet
- JurnalDocument16 pagesJurnalNyche Vouresha NurseNo ratings yet
- Prac2 CpsirDocument30 pagesPrac2 CpsirSrishti GaurNo ratings yet
- Archives of Psychiatric Nursing: Valeria Cremonini, Nicola Pagnucci, Franco Giacometti, Ivan RubbiDocument7 pagesArchives of Psychiatric Nursing: Valeria Cremonini, Nicola Pagnucci, Franco Giacometti, Ivan RubbileticiaNo ratings yet
- The Structure of Genetic and Environmental Risk Factors For Syndromal and Subsyndromal Common DSM-IV Axis I and All Axis II DisordersDocument19 pagesThe Structure of Genetic and Environmental Risk Factors For Syndromal and Subsyndromal Common DSM-IV Axis I and All Axis II DisordersPatriciaNo ratings yet
- Davydow 2010 Psychiatric MorbidityDocument9 pagesDavydow 2010 Psychiatric MorbidityAndrew EdisonNo ratings yet
- NIH Public Access: Author ManuscriptDocument13 pagesNIH Public Access: Author ManuscriptSnehaNo ratings yet
- Consecuencias de Los Conflictos Armados Sobre La Salud Mental en Adultos Revisión de Revisiones de La LiteraturaDocument25 pagesConsecuencias de Los Conflictos Armados Sobre La Salud Mental en Adultos Revisión de Revisiones de La LiteraturazulmaurregoNo ratings yet
- Physical Exercise and Major Depressive Disorder in Adults Systematic Review and Meta AnalysisDocument17 pagesPhysical Exercise and Major Depressive Disorder in Adults Systematic Review and Meta AnalysisErick NunesNo ratings yet
- Lee El Al., 2024 Exercício e DemênciaDocument16 pagesLee El Al., 2024 Exercício e DemêncialalaNo ratings yet
- Mental DisordersDocument4 pagesMental DisordersFatin AfyqahNo ratings yet
- A Review of Bipolar Disorder Among Adults PDFDocument13 pagesA Review of Bipolar Disorder Among Adults PDFNadyaNo ratings yet
- Documen 2 TDocument11 pagesDocumen 2 TRhodius NogueraNo ratings yet
- Determinantes Sociales Salud MentalDocument13 pagesDeterminantes Sociales Salud MentalYajaira Saavedra JimenezNo ratings yet
- Mental Health Act 2022Document17 pagesMental Health Act 2022saran.19bpsNo ratings yet
- 8th Journal Reading Ancog Clint NCM 117Document4 pages8th Journal Reading Ancog Clint NCM 117shadow gonzalezNo ratings yet
- Preventing The Onset of Depressive Disorders in Low and Middle Income Countries An OverviewDocument6 pagesPreventing The Onset of Depressive Disorders in Low and Middle Income Countries An OverviewDarien Alfa CiptaNo ratings yet
- Covi̇dde Tükenmi̇şli̇kDocument8 pagesCovi̇dde Tükenmi̇şli̇kTalipNo ratings yet
- Drug and Alcohol Dependence: Short CommunicationDocument7 pagesDrug and Alcohol Dependence: Short CommunicationRiski NovitaNo ratings yet
- A Systematic Review and Meta-Analysis of Dyadic Psychological InterventionsDocument22 pagesA Systematic Review and Meta-Analysis of Dyadic Psychological InterventionsCristina MPNo ratings yet
- Psi Reinhardt 15Document13 pagesPsi Reinhardt 15Natalia MenottiNo ratings yet
- Pi Is 2215036621003953Document14 pagesPi Is 2215036621003953MIGUEL ANGEL TEHERÁN MARTINEZNo ratings yet
- Arvanitakis, Shah, Bennett - 2019 - Diagnosis and Management of Dementia ReviewDocument11 pagesArvanitakis, Shah, Bennett - 2019 - Diagnosis and Management of Dementia ReviewJuan Carlos AlfaroNo ratings yet
- The Mental Mirror: Reflections on Psychiatry: Beyond the Looking Glass: The Enigmatic Odyssey of the MindFrom EverandThe Mental Mirror: Reflections on Psychiatry: Beyond the Looking Glass: The Enigmatic Odyssey of the MindNo ratings yet
- TL OriginalDocument1 pageTL OriginalRodrigo SilvaNo ratings yet
- Overview On The Digical Symbols: Often Used AbbreviationsDocument7 pagesOverview On The Digical Symbols: Often Used AbbreviationsRodrigo SilvaNo ratings yet
- Convocatoria Neae Curso 2021-2022Document19 pagesConvocatoria Neae Curso 2021-2022Rodrigo SilvaNo ratings yet
- Principios Básicos Sobre Diseño Periodístico: January 2001Document1 pagePrincipios Básicos Sobre Diseño Periodístico: January 2001Rodrigo SilvaNo ratings yet
- COMS11500: Introduction To CDocument15 pagesCOMS11500: Introduction To CRodrigo SilvaNo ratings yet
- Name Synopsis Description: CurlDocument1 pageName Synopsis Description: CurlRodrigo SilvaNo ratings yet
- Name Synopsis: #Include Curlshcode Curl - Share - Cleanup (Curlsh Share - Handle)Document1 pageName Synopsis: #Include Curlshcode Curl - Share - Cleanup (Curlsh Share - Handle)Rodrigo SilvaNo ratings yet
- Week3 1Document89 pagesWeek3 1Rodrigo SilvaNo ratings yet
- Name Synopsis: #Include Void Curl - Slist - Free - All (Struct Curl - Slist List)Document1 pageName Synopsis: #Include Void Curl - Slist - Free - All (Struct Curl - Slist List)Rodrigo SilvaNo ratings yet
- Reference ManualDocument1 pageReference ManualRodrigo SilvaNo ratings yet
- Week2 2Document66 pagesWeek2 2Rodrigo SilvaNo ratings yet
- COMS11500: Introduction To C: Julian GoughDocument53 pagesCOMS11500: Introduction To C: Julian GoughRodrigo SilvaNo ratings yet
- PoseWriter Panel GUIDEDocument9 pagesPoseWriter Panel GUIDERodrigo SilvaNo ratings yet
- Casino Royale Strategy Game DemonstrationDocument11 pagesCasino Royale Strategy Game DemonstrationRodrigo SilvaNo ratings yet
- COMS11500: Introduction To CDocument37 pagesCOMS11500: Introduction To CRodrigo SilvaNo ratings yet
- CW4: COMS11500 Coursework Weeks 7 and 8: VigenèreDocument5 pagesCW4: COMS11500 Coursework Weeks 7 and 8: VigenèreRodrigo SilvaNo ratings yet
- COMS11500: Introduction To C: Julian GoughDocument21 pagesCOMS11500: Introduction To C: Julian GoughRodrigo SilvaNo ratings yet
- COMS11500: Introduction To C: Dimitrios V. VavoulisDocument27 pagesCOMS11500: Introduction To C: Dimitrios V. VavoulisRodrigo SilvaNo ratings yet
- Assessment Form: Name ID (Xy12345)Document1 pageAssessment Form: Name ID (Xy12345)Rodrigo SilvaNo ratings yet
- Population Supp M16066 - A 49Document1 pagePopulation Supp M16066 - A 49Rodrigo SilvaNo ratings yet
- Possible Worlds in Narrative SpaceDocument19 pagesPossible Worlds in Narrative SpaceMariia Mandrikova100% (1)
- Jasunjski Manastir Svetog Jovana PreteceDocument6 pagesJasunjski Manastir Svetog Jovana PreteceMaja JovanovicNo ratings yet
- DiPietro 1976 Significance of FMA To ProsDocument12 pagesDiPietro 1976 Significance of FMA To ProsomidNo ratings yet
- Evangelism Report To Kuchibuyi Community-1Document2 pagesEvangelism Report To Kuchibuyi Community-1Collins OnyebuchiNo ratings yet
- English 10 ReviewerDocument4 pagesEnglish 10 Reviewerathea garciaNo ratings yet
- Senior High School Student Permanent Record: Republic of The Philippines Department of EducationDocument3 pagesSenior High School Student Permanent Record: Republic of The Philippines Department of EducationfretzNo ratings yet
- Hi!!Document5 pagesHi!!Venus Clamaña100% (1)
- CMucat Application FormDocument1 pageCMucat Application FormJiyan Litohon100% (1)
- Balotario Ingles Vi Primera ParteDocument7 pagesBalotario Ingles Vi Primera ParteAron Alexis Lloclla SandovalNo ratings yet
- Lecture PDF IIT BombayDocument593 pagesLecture PDF IIT BombayKhan SalimNo ratings yet
- PRIMARY vs. SECONDARY SOURCESDocument2 pagesPRIMARY vs. SECONDARY SOURCESShannise Dayne ChuaNo ratings yet
- The Surrealist Roots of Video EssaysDocument5 pagesThe Surrealist Roots of Video EssayspsicorticoNo ratings yet
- Az-900 PrepAway PDFDocument82 pagesAz-900 PrepAway PDFNisha PrasadNo ratings yet
- LGBTQ Mental HealthDocument15 pagesLGBTQ Mental HealthDiana Teodora PiteiNo ratings yet
- A Critical Review of The Equivalent Stoichiometric Cloud Model Q9 in Gas Explosion ModellingDocument25 pagesA Critical Review of The Equivalent Stoichiometric Cloud Model Q9 in Gas Explosion ModellingAndrzej BąkałaNo ratings yet
- COP-WFP-APD-03-2013-v1 IWP TimelineDocument1 pageCOP-WFP-APD-03-2013-v1 IWP TimelineAbdul AzizNo ratings yet
- Vocabulary: Task 1 Task 4Document2 pagesVocabulary: Task 1 Task 4Anto VegaNo ratings yet
- The Role of CSR Programs On The Buying Behavior ofDocument6 pagesThe Role of CSR Programs On The Buying Behavior ofReduNo ratings yet
- Unit 6 Short Test 2A: GrammarDocument1 pageUnit 6 Short Test 2A: GrammarGordanaNo ratings yet
- John McDowell, Wittgenstein On Following A Rule', Synthese 58, 325-63, 1984.Document40 pagesJohn McDowell, Wittgenstein On Following A Rule', Synthese 58, 325-63, 1984.happisseiNo ratings yet
- Abstract WritingDocument11 pagesAbstract WritingMuhammad UsmanNo ratings yet
- Marketing Research Report:Netflix: Presented By: Rida Ahmad Ali Jawad Meeral ZiaDocument12 pagesMarketing Research Report:Netflix: Presented By: Rida Ahmad Ali Jawad Meeral ZiaAli JawadNo ratings yet
- Acceeration MechanismDocument33 pagesAcceeration MechanismDavid nelsonNo ratings yet
- OMS NaturopatiaDocument33 pagesOMS NaturopatiaJoão Augusto Félix100% (1)
- Generalized Anxiety DisorderDocument17 pagesGeneralized Anxiety DisorderFathima MohammedNo ratings yet
- 12 ConclusionDocument50 pages12 Conclusionriyamirza36365No ratings yet
- The Wanderer & Seafearer - 230228 - 151524Document8 pagesThe Wanderer & Seafearer - 230228 - 151524Nikolett LakatosNo ratings yet