Professional Documents
Culture Documents
Rheumatoid Arthritis Case Study
Uploaded by
Chakrit ThongEk0 ratings0% found this document useful (0 votes)
500 views2 pagesRA case study
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentRA case study
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
500 views2 pagesRheumatoid Arthritis Case Study
Uploaded by
Chakrit ThongEkRA case study
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Rheumatoid Arthritis Case Study
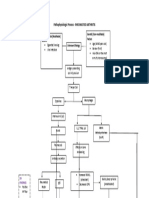
Joy G. is a 48-year old married mother of 3 active
boys, ages 12, 15, and 18. She enjoys attending her
sons’ sporting events and providing “Mom-Taxi”
services for her sons and their friends. She also loves
her part-time job as a hairdresser at a popular salon.
Seven months ago, Joy began noticing stiffness in
both hands in the morning that lasted longer and
longer. Stiffness now lasted more than 1 hour every
morning and included hands, wrists and ankles. She also had increasing difficulty standing for
long periods at work or at home due to foot and ankle pain. She began taking ibuprofen 800mg
3 times daily and found it helped her get through her day with less pain and stiffness.
Three months ago, Joy noticed pain in her right and left shoulders when she would cut or blow
dry her client’s hair. She also began feeling extremely tired and short tempered. She had no
energy to do her usual activities. Ibuprofen was no longer very effective for her pain or
stiffness.
One morning, Joy could not lift her arms at all without extreme shoulder pain. She knew it was
time to get help. She had been speaking with her friends and they encouraged her to see a
doctor. She saw her Primary Care Physician (PCP), who examined her and ran a few preliminary
blood tests. The blood tests revealed positive rheumatoid factor, CCP antibodies, elevated ESR
and C-reactive protein. Joy was informed of these results and her PCP referred her to a
Rheumatologist to be seen as soon as possible.
In order to facilitate a timely consultation, Joy was scheduled with the rheumatology Nurse
Practitioner (NP) for her new patient appointment.
Upon arrival at the rheumatology office, Joy was asked to provide a complete medical history.
At her scheduled appointment time, the Certified Medical Assistant (CMA) escorted Joy into the
exam room, where her weight and height were measured and vital signs taken. The CMA
reviewed her medications and their dosages with her and documented them in the electronic
medical record.
The NP introduced herself and proceeded to take a complete history. She asked about Joy’s
parents’ and grandparents’ medical histories, family illnesses, Joy’s medical and surgical history
and information about her family and work lives. A thorough physical examination was
conducted, including examination of all of Joy’s joints, many of which were tender and swollen.
Her Rapid 3 Score was 21.8, consistent with severe impairment and significant disease activity.
The NP discussed the examination findings with Joy, and reviewed the laboratory tests from her
PCP. The NP ordered x-rays of Joy’s feet, hands and shoulders. Additional laboratories were
ordered and drawn by the CMA.
The NP introduced Joy to the Rheumatologist. Together, they discussed with Joy that her most
likely diagnosis is Rheumatoid Arthritis (RA). General facts about RA and common treatments
were briefly discussed. Joy was prescribed low dose prednisone and corticosteroid injections
were administered in each of her shoulders by the NP. Common side effects of the medications
and expected responses were discussed with Joy and her questions were answered. She was
advised to call the office if she experienced any problems or had questions.
At her follow-up visit with the Rheumatologist 2 weeks later, laboratories had confirmed what
her history and examination indicated, that Joy had established RA (symptoms present for more
than 6 months). Joy’s shoulders felt a little better, though she was still having pain and difficulty
raising her arms. The Rheumatologist recommended she see a Physical Therapist (PT) for
further assessment and treatment of her shoulders and advice on activity modification related
to her work. She was prescribed oral methotrexate and folic acid and advised to continue the
low dose prednisone. Common medication side effects were discussed. The NP provided
written information about the medications and referred her to the clinic Pharmacist for
medication review and to answer any questions.
The NP offered to answer Joy’s questions and discussed tips for living with RA, including energy
conservation and the importance of adequate rest. Written information about RA was
provided. Joy was encouraged to go to the American College of Rheumatology (ACR) website
for additional information and resources.
Joy continued with regular rheumatology office visits as her medications were adjusted,
laboratories were monitored and symptoms improved. By her third month of treatment with
methotrexate, prednisone was discontinued and she had resumed all of her regular activities.
Her Rapid 3 Score had decreased to 4, consistent with low disease activity and severity of illness.
Morning joint stiffness was minimal and she had 3 swollen and tender joints. She no longer had
difficulty raising her arms to cut or blow dry her clients’ hair. She continues to seek out
information about living with arthritis and how to stay physically active from the ACR and
Arthritis Foundation websites.
Karen Duclon, MSN, ARNP
ARHP Practice Committee
You might also like
- Juvenile Rheumatoid Arthritis: Jeffrey A. LuceroDocument10 pagesJuvenile Rheumatoid Arthritis: Jeffrey A. LucerojamilliumNo ratings yet
- Case Study of Rheumatoid Arthritis FinalDocument17 pagesCase Study of Rheumatoid Arthritis FinalKathleen Abian67% (3)
- Rheumatoid ArthritisDocument25 pagesRheumatoid ArthritisGandung PrakosoNo ratings yet
- Rheumatoid Arthritis Case DiscussionDocument23 pagesRheumatoid Arthritis Case DiscussionJanieross LambosoNo ratings yet
- Pathophysiology - Rheumatoid ArthritisDocument1 pagePathophysiology - Rheumatoid ArthritisAngel FiloteoNo ratings yet
- Case Study Rheumatoid ArthritisDocument16 pagesCase Study Rheumatoid ArthritisJessy Mallo100% (2)
- Systemic Lupous Erythematosus (SLE)Document46 pagesSystemic Lupous Erythematosus (SLE)Power La Victoria Floro100% (1)
- Compare and Contrast Two Obstructive Lung Disorders: Asthma vs COPDDocument1 pageCompare and Contrast Two Obstructive Lung Disorders: Asthma vs COPDAriaNo ratings yet
- Cva Case StudyDocument31 pagesCva Case StudyZoe AnnaNo ratings yet
- Lupus, SLEDocument2 pagesLupus, SLEFrances Anne Pasiliao100% (2)
- Septic ArthritisDocument8 pagesSeptic ArthritisLorebell100% (2)
- Managing Upper GI Bleeding in a Male PatientDocument19 pagesManaging Upper GI Bleeding in a Male PatientMary Ann Garcia100% (1)
- Nursing Care Plan for Patient with Sepsis and CellulitisDocument3 pagesNursing Care Plan for Patient with Sepsis and CellulitisMichaelaKatrinaTrinidadNo ratings yet
- Rheumatoid ArthritisDocument52 pagesRheumatoid ArthritisSophia Veron100% (2)
- Systemic Lupus ErythematosusDocument89 pagesSystemic Lupus ErythematosusIke RilleraNo ratings yet
- Diabetes InsipidusDocument48 pagesDiabetes InsipidusAhmed Fraz MamoonNo ratings yet
- Rheumatoid Arthritis Treatment and Management GuideDocument32 pagesRheumatoid Arthritis Treatment and Management GuideamirthaNo ratings yet
- Glasgow Coma ScaleDocument3 pagesGlasgow Coma Scaletoto11885No ratings yet
- Osteoarthritis 1583-170210113823Document34 pagesOsteoarthritis 1583-170210113823Angelic khanNo ratings yet
- OUR LADY OF FATIMA UNIVERSITY Case Study on Post Streptococcal GlomerulonephritisDocument20 pagesOUR LADY OF FATIMA UNIVERSITY Case Study on Post Streptococcal GlomerulonephritisMikaCasimiroBalunanNo ratings yet
- CASE REPORT - Rheumatoid ArthritisDocument13 pagesCASE REPORT - Rheumatoid ArthritisbrightagbotuiNo ratings yet
- Clinical Case StudyDocument20 pagesClinical Case Studyapi-252004748No ratings yet
- Gouty GCPDocument48 pagesGouty GCPKylie GolindangNo ratings yet
- PYOMYOSITISDocument6 pagesPYOMYOSITISChristine CoridoNo ratings yet
- CASE STUDY 80: Rheumatoid ArthritisDocument7 pagesCASE STUDY 80: Rheumatoid Arthritisangelica dizon100% (1)
- Case Study on Graded Return to Work Program for Carpal Tunnel SyndromeDocument11 pagesCase Study on Graded Return to Work Program for Carpal Tunnel SyndromeMargeaux Deb Bartholomew CarleNo ratings yet
- Pathophysiology Diabetic Foot UlcerDocument7 pagesPathophysiology Diabetic Foot UlcerAnnisa ClaraNo ratings yet
- University of Northern PhilippinesDocument1 pageUniversity of Northern PhilippinesCezanne CruzNo ratings yet
- Rheumatoid Arthritis - Case ReportDocument33 pagesRheumatoid Arthritis - Case ReportWarren Lie100% (1)
- OSTEOMYELITISDocument14 pagesOSTEOMYELITISKristine Alejandro0% (1)
- Pathophysiology of ObesityDocument1 pagePathophysiology of ObesityPoldo Josef AngeloNo ratings yet
- SEPTICARTHRITISDocument2 pagesSEPTICARTHRITISapi-3822433No ratings yet
- Rheumatoid ArthritisDocument62 pagesRheumatoid ArthritisChuah Wei HongNo ratings yet
- Pathophysiology of mesenchymal chondrosarcomaDocument7 pagesPathophysiology of mesenchymal chondrosarcomaMaria Grace Raquel Ormeneta100% (1)
- External HemorrhoidsDocument61 pagesExternal HemorrhoidsitsmeayaNo ratings yet
- OsteoarthritisDocument29 pagesOsteoarthritischan park100% (1)
- Ra Case StudyDocument52 pagesRa Case StudyMiracle Guillermo100% (4)
- Nursing Care Plan for Acute Pain PatientDocument2 pagesNursing Care Plan for Acute Pain PatientAnni BarbaNo ratings yet
- AppendicitisDocument16 pagesAppendicitisFiras AbusharikhNo ratings yet
- HyperphosphatemiaDocument2 pagesHyperphosphatemiatephNo ratings yet
- GoutDocument12 pagesGoutEarle Jimenez Niervo RN100% (1)
- Multiple Sclerosis: Case Study by Trcoski ElenaDocument43 pagesMultiple Sclerosis: Case Study by Trcoski ElenaElena TrcoskiNo ratings yet
- Thromboangiitis Obliterans (Buerger's Disease): A Case PresentationDocument16 pagesThromboangiitis Obliterans (Buerger's Disease): A Case PresentationYan VencerNo ratings yet
- EBNDocument22 pagesEBNLouis Ann BautistaNo ratings yet
- Page 17 ACUTE PAIN Related To Joint Stiffness Secondary To Aging.Document3 pagesPage 17 ACUTE PAIN Related To Joint Stiffness Secondary To Aging.Senyorita KHayeNo ratings yet
- Case Study PnuemoniaDocument10 pagesCase Study PnuemoniaKyle B. Nacionales Ü100% (1)
- Buerger Disease Diagnosis and TreatmentDocument10 pagesBuerger Disease Diagnosis and Treatmentautorace007No ratings yet
- Nursing Care Plan for Diabetic Patient with DehydrationDocument2 pagesNursing Care Plan for Diabetic Patient with DehydrationRodolfo Bong SemaneroNo ratings yet
- Rheumatoid Arthritis Case StudyDocument21 pagesRheumatoid Arthritis Case StudyKatrene LequiganNo ratings yet
- GoutDocument6 pagesGoutNhoydaleen SandovalNo ratings yet
- Potts DiseaseDocument8 pagesPotts Diseaseaimeeros0% (2)
- Rheumatoid ArthritisDocument11 pagesRheumatoid ArthritisVerli Fajriati Nofli0% (1)
- Lupus Case ReportDocument1 pageLupus Case ReportMendy HararyNo ratings yet
- NCP PainDocument1 pageNCP PaindwightciderNo ratings yet
- Potts Disease Case AnalysisDocument5 pagesPotts Disease Case AnalysisAdrian MallarNo ratings yet
- Avascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAvascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 4 out of 5 stars4/5 (2)
- Juvenile Idiopathic Arthritis Case StudyDocument4 pagesJuvenile Idiopathic Arthritis Case StudyBruno PereiraNo ratings yet
- Nervous System Case Study Assignment 2023Document3 pagesNervous System Case Study Assignment 2023Elijah HallNo ratings yet
- OsteosarcomaDocument87 pagesOsteosarcomaCob CornNo ratings yet
- Charlotte Gerson - The Gerson Way - Healing Auto-Immune DiseasesDocument25 pagesCharlotte Gerson - The Gerson Way - Healing Auto-Immune Diseasesbrunacp92283% (6)
- Ncma 219 Finals CompleteDocument70 pagesNcma 219 Finals CompleteKENSEY MOORE EBROLENo ratings yet
- BulletsDocument14 pagesBulletsstuffednurseNo ratings yet
- Complete Ahn Pre Board Guess Paper For Dow Mid Exam by Hamid KhanDocument10 pagesComplete Ahn Pre Board Guess Paper For Dow Mid Exam by Hamid KhanShayan ShayanNo ratings yet
- Golden Milk Turmeric LatteDocument4 pagesGolden Milk Turmeric LatteHelena AzevedoNo ratings yet
- Final Exam (Lec) NCM 112 Wo AnsDocument10 pagesFinal Exam (Lec) NCM 112 Wo AnsJR Rolf NeuqeletNo ratings yet
- Symptoms: Rheumatoid ArthritisDocument17 pagesSymptoms: Rheumatoid Arthritismehrasa nikandishNo ratings yet
- Best Homeopathic Remedies for Knee PainDocument29 pagesBest Homeopathic Remedies for Knee PainKrish MotupalliNo ratings yet
- MR Supple All 2014Document429 pagesMR Supple All 2014Regita Ayu LestariNo ratings yet
- Health Benefits of Cascade Fermented Foods - "You'll Just Have To Live With It!" (No Thank You!)Document105 pagesHealth Benefits of Cascade Fermented Foods - "You'll Just Have To Live With It!" (No Thank You!)BiologicalMed99100% (4)
- DR MinaDocument23 pagesDR MinaMina Magdy FahmyNo ratings yet
- A Comparative Clinical Study On The Effect of Kottamchukkadi and Kolakulathadi Upanaha Sweda in JanusandhigatavataDocument6 pagesA Comparative Clinical Study On The Effect of Kottamchukkadi and Kolakulathadi Upanaha Sweda in JanusandhigatavataInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Health Appraisal Record: I. Personal Data: II. Physical and Medical ExaminationDocument2 pagesHealth Appraisal Record: I. Personal Data: II. Physical and Medical ExaminationJA BerzabalNo ratings yet
- Antemortem and Post Mortem InspectionDocument15 pagesAntemortem and Post Mortem InspectionMuhammad SiddiqueNo ratings yet
- Bromelain MonographDocument8 pagesBromelain Monographluis_garcia_28100% (1)
- Gouty PowerpointDocument14 pagesGouty PowerpointBSN4ANo ratings yet
- MRCPUK Part 1 SyllabusDocument62 pagesMRCPUK Part 1 Syllabusthargyikyaw100% (5)
- AyurvedaDocument892 pagesAyurvedaPankaj Gupta0% (1)
- Reactive ArthritisDocument8 pagesReactive ArthritisamereNo ratings yet
- Diagnostic Approach To Polyarticular Joint Pain - American Family PhysicianDocument12 pagesDiagnostic Approach To Polyarticular Joint Pain - American Family PhysicianKalin TsenovNo ratings yet
- Nursing Care Plan Rheumatoid ArthritisDocument4 pagesNursing Care Plan Rheumatoid ArthritisLighto RyusakiNo ratings yet
- RESNICK - Bone and Joint Imaging, 3rd Ed. CONTENIDODocument3 pagesRESNICK - Bone and Joint Imaging, 3rd Ed. CONTENIDOfabianNo ratings yet
- Diseases and Disorders of The Skeletal SystemDocument11 pagesDiseases and Disorders of The Skeletal SystemJames Roy100% (1)
- Consolidated Annotated Frequency List: We Make NO CLAIMS As To The Accuracy or Efficacy of The Frequencies Posted Here!Document69 pagesConsolidated Annotated Frequency List: We Make NO CLAIMS As To The Accuracy or Efficacy of The Frequencies Posted Here!Matimba SimangoNo ratings yet
- Musculoskeletal Disorders Part 1Document246 pagesMusculoskeletal Disorders Part 1Carmela Lacsa DomocmatNo ratings yet
- Drug StudyDocument4 pagesDrug StudyPam RomeroNo ratings yet
- Ikfr - MM Sken 3Document3 pagesIkfr - MM Sken 36130017050 RISMA MIFTAHUL JANNAHNo ratings yet
- PalliationDocument16 pagesPalliationPartha ChakrabortyNo ratings yet
- Medical Marijuana TincturesDocument15 pagesMedical Marijuana TincturesCaress Mae Gubaton CabudoyNo ratings yet