Professional Documents
Culture Documents
Warfarin Drug Interactions1 PDF
Warfarin Drug Interactions1 PDF
Uploaded by
Peter HuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Warfarin Drug Interactions1 PDF
Warfarin Drug Interactions1 PDF
Uploaded by
Peter HuCopyright:
Available Formats
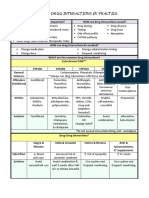
WARFARIN DRUG INTERACTIONS1,2
The drugs in this list are more usually associated with loss of INR control in patients already established
on warfarin. This list is not exhaustive - refer to the British National Formulary (BNF) for further
information. If any of the drugs below are to be started in these patients then the use of alternatives in
the same therapeutic class may be considered. If this is not possible then the patient’s INR should be
monitored as detailed below. Those drugs highlighted in bold are significant interactions and should be
avoided or used with caution.
• Drugs marked * are liver enzyme inhibitors and increase the INR. They act very quickly (can
be within 24 hours) and if the drug is withdrawn the effect disappears quickly depending on
the drug half-life. The INR should if possible be monitored within 72 hours of starting the
interacting drug and on withdrawal.
• Drugs marked $ are liver enzyme inducers and decrease the INR. They act more slowly (up to
a week) with peak effect at 2-3 weeks and can persist for up to 4 weeks after stopping
depending on drug half-life. The INR will need checking after 1 week of concurrent therapy.
• Drugs with neither have other mechanisms, which affect the INR.
N.B. If a patient on warfarin were started on ANY other new medication a repeat INR after 1 week
would be a sensible
Drugs that increase the INR and risk of bleed
Gastrointestinal cimetidine*, omeprazole* and possibly other PPIs
Cardiovascular amiodarone* (liver enzyme inhibition is slow and may persist long
after withdrawal requiring weekly monitoring over 4 weeks),
fibrates, ezetimibe, propafenone*, propranolol,
statins – no clinically relevant interaction will normally be seen
however it is prudent to check INR in the weeks after initiation and
at any dose change
CNS fluvoxamine*, SNRIs, SSRIs*, tramadol
Anti-infectives (anti- azole antifungals* (esp. miconazole including oral gel and
infectives in general may vaginal), co-trimoxazol*, macrolides* (can be serious but unpredictable),
cause raised INR’s) metronidazole*, quinolones* (can be serious but unpredictable),
tetracyclines, influenza vaccine
Endocrine anabolic steroids (and danazol), high dose corticosteroids,
glucagon (high dose 50mg+ over 2 days), flutamide,
levothyroxine
NSAIDs Ibuprofen at lowest effective dose (+/-PPI) is probably safest if NSAID is required
N.B. All NSAIDs can increase the risk of bleeds and should be avoided if
possible
Antiplatelets – increased
bleed risk Aspirin, clopidogrel and dipyridamole
Miscellaneous Alcohol (acute), allopurinol*, benzbromarone*, colchicine, disulfiram, fluorouracil,
interferon paracetamol (prolonged use at high dose), sulfinpyrazone, tamoxifen,
topical salicylates, zafirlucast*
Herbal preparations/Food Carnitine, chamomile, cranberry juice*, curbicin, dong quai, fenugreek, fish oils,
supplements garlic, gingo biloba, glucosamine, grapefruit juice*, lycium*, mango, quilinggao
Drugs that decrease the INR
Miscellaneous Alcohol$ (chronic), azathioprine, barbiturates$, bosentan$, carbamazepine$,
$ $
carbimazole, griseofulvin , mercaptopurine, nevirapine , OCP/HRT,
propylthiouracil, raloxifene, rifampicin$(most potent inducer), trazodone
Herbal preparations etc Avocado, co-enzyme Q10, green tea, natto, soya beans, St Johns wort$ (avoid)
Binding agents Colestyramine, sucralfate
Warfarin antagonist
Vitamin K
Drugs that increase or decrease the INR
Miscellaneous Ginseng, phenytoin, quinidine
1
British National Formularly 55 Edition March 2008
2
Stockley’s Drug Interactions. Edition Eight. Pharmaceutical Press. November 2007
Based on original by Julian Holmes, Nottingham University Hospitals Trust, and further adapted by
NHS Derbyshire County PCT Updated by Aiste Baltramaityte and David Anderton
Derby Hospitals NHS Foundation Trust.
You might also like
- MCCEE Question Bank FOR CANADADocument2 pagesMCCEE Question Bank FOR CANADAcathystar75% (4)
- Cardiovascular Pharmacotherapy CasesDocument49 pagesCardiovascular Pharmacotherapy CasesNaif Al Shaibani100% (3)
- V Chem Next User's ManualDocument23 pagesV Chem Next User's ManualDharmesh Patel100% (1)
- Assessment Hema PDFDocument9 pagesAssessment Hema PDFAnne MorenoNo ratings yet
- AntikoagulanDocument70 pagesAntikoagulanFian AldyNo ratings yet
- S 022 LBLDocument34 pagesS 022 LBLyogeshmotwaniNo ratings yet
- Information For Pharmacists On Managing Warfarin Drug InteractionsDocument4 pagesInformation For Pharmacists On Managing Warfarin Drug InteractionsBelladonna Perdana PutraNo ratings yet
- Drugs To Watch With WARFARINDocument3 pagesDrugs To Watch With WARFARINRajendra RaiNo ratings yet
- Mini Warfarin GuidelinesDocument2 pagesMini Warfarin GuidelinesPeunn NattaphatNo ratings yet
- Pharmaceutical Assessment Plan and Follow Up Sheet DVT 2Document5 pagesPharmaceutical Assessment Plan and Follow Up Sheet DVT 2Turkish DizilerNo ratings yet
- Lorazepam - StatPearls - NCBI Bookshelf PDFDocument6 pagesLorazepam - StatPearls - NCBI Bookshelf PDFCarlos MuñozNo ratings yet
- Pharmacology: Drug MonitoringDocument43 pagesPharmacology: Drug MonitoringMa GynNo ratings yet
- Toradol KetorolacDocument2 pagesToradol KetorolacE100% (4)
- Care Plan:, Wrong, Wrong, Wrong, WrongDocument8 pagesCare Plan:, Wrong, Wrong, Wrong, Wronglovelylife theNo ratings yet
- Rima DylDocument3 pagesRima DylsupravietuireNo ratings yet
- Ibuprofen 150mg + Paracetamol 500mg (Combodex)Document15 pagesIbuprofen 150mg + Paracetamol 500mg (Combodex)ddandan_2No ratings yet
- Supralip 160 MG Film-Coated Tablets - Summary of Product Characteristics (SMPC) - Print Friendly - (Emc)Document8 pagesSupralip 160 MG Film-Coated Tablets - Summary of Product Characteristics (SMPC) - Print Friendly - (Emc)bhavaniNo ratings yet
- C C C CC C MMMM MMMMDocument10 pagesC C C CC C MMMM MMMMFerlyn PanchoNo ratings yet
- Tramadol HydrochlorideDocument5 pagesTramadol HydrochlorideSebastian CruzNo ratings yet
- DiarryDocument10 pagesDiarryVan Ryan CondenoNo ratings yet
- A Guide To Psychotropic DrugsDocument16 pagesA Guide To Psychotropic DrugsNokz M. Raki-inNo ratings yet
- Fenofibrate 160mg Tablets - Summary of Product Characteristics (SMPC) - Print Friendly - (Emc)Document6 pagesFenofibrate 160mg Tablets - Summary of Product Characteristics (SMPC) - Print Friendly - (Emc)bhavaniNo ratings yet
- Drug InteractionsDocument36 pagesDrug Interactionsbaker371100% (2)
- Psychotropic Drugs.Document15 pagesPsychotropic Drugs.Xiaoqing SongNo ratings yet
- Anti-Fungal Amphotericin BDocument4 pagesAnti-Fungal Amphotericin BMargo AlmazanNo ratings yet
- Drug-Food/Drug-Herb Interaction GuideDocument13 pagesDrug-Food/Drug-Herb Interaction GuidechareneadamsNo ratings yet
- Pantozol Control Epar Product Information - enDocument30 pagesPantozol Control Epar Product Information - enDeKa NineNo ratings yet
- KetorolacDocument2 pagesKetorolacJacqueline LimNo ratings yet
- Neuropathic Pain Guidance April 2023 v1.2Document6 pagesNeuropathic Pain Guidance April 2023 v1.2Germán Bernate ObandoNo ratings yet
- SPC Pramipexole 0.7 MGDocument14 pagesSPC Pramipexole 0.7 MGJehan SarahdiniNo ratings yet
- PhenyltriazineDocument2 pagesPhenyltriazineabcdeNo ratings yet
- WEEK2 Course Task (ALFEREZ, DINIELA)Document4 pagesWEEK2 Course Task (ALFEREZ, DINIELA)DINIELA ALLAINE ALFEREZNo ratings yet
- Di Inservice FinalDocument2 pagesDi Inservice Finalapi-277713384No ratings yet
- Fixcom 4® (Tab) : Natrapharm Natrapharm Anti-TB AgentsDocument13 pagesFixcom 4® (Tab) : Natrapharm Natrapharm Anti-TB AgentsApril_Jane_Nat_8299No ratings yet
- Topic 8 - Management of Adverse Drug ReactionsDocument27 pagesTopic 8 - Management of Adverse Drug ReactionsPrincewill SmithNo ratings yet
- Reminyl (Galantamine) : General InformationDocument4 pagesReminyl (Galantamine) : General InformationArcenciel26No ratings yet
- Paracetamol Use GuideDocument13 pagesParacetamol Use GuideShashiprakash KshatriyaNo ratings yet
- Antispastics Emtyaz FDocument57 pagesAntispastics Emtyaz FMuhammed MuhsinNo ratings yet
- Prescribing InformationDocument9 pagesPrescribing InformationasdwasdNo ratings yet
- Drug Study For AMCDocument3 pagesDrug Study For AMCTrixia RiveraNo ratings yet
- Pharma - Week 2 Course TaskDocument6 pagesPharma - Week 2 Course TaskLou KristofferNo ratings yet
- ZOMORPH Capsules 10mgDocument6 pagesZOMORPH Capsules 10mgFlorexan Malanday PasonNo ratings yet
- Anx 130215 enDocument143 pagesAnx 130215 enzekyashawnNo ratings yet
- Generic Name: Quinupristin/Dalfopristin - Injection (Kwin-ue-PRIS-tin/DAL-foe-PRIS-tin)Document4 pagesGeneric Name: Quinupristin/Dalfopristin - Injection (Kwin-ue-PRIS-tin/DAL-foe-PRIS-tin)Jrose CuerpoNo ratings yet
- Antimicrobial Drug Interactionstable220716 PDFDocument4 pagesAntimicrobial Drug Interactionstable220716 PDFBhavin DesaiNo ratings yet
- Drug Classification - PhenytoinDocument3 pagesDrug Classification - Phenytoinkedwards108No ratings yet
- Summary of Product Characteristics 1. Name of The Medicinal ProductDocument13 pagesSummary of Product Characteristics 1. Name of The Medicinal Productddandan_2No ratings yet
- SUMMARY OF PRODUCT CHARACTERISTICS Ibuprofen and Codeine 200mg/12.8mg Film-Coated TabletsDocument12 pagesSUMMARY OF PRODUCT CHARACTERISTICS Ibuprofen and Codeine 200mg/12.8mg Film-Coated TabletsDane WoodNo ratings yet
- Palliative Care FormularyDocument12 pagesPalliative Care FormularyRicardo FernandesNo ratings yet
- Cafergot Patient eDocument3 pagesCafergot Patient eLaurentiu DinuNo ratings yet
- List of Top Ten Drug Interactions in Long-Term CareDocument8 pagesList of Top Ten Drug Interactions in Long-Term Careanon_511980284No ratings yet
- Fludrocortisone For Orthostatic HypotensionDocument5 pagesFludrocortisone For Orthostatic Hypotension4everythingwedoNo ratings yet
- The 10 Most Common Emergency DrugsDocument28 pagesThe 10 Most Common Emergency DrugsKrishna BalsarzaNo ratings yet
- 2160202.PA0749 - 113 - 001..000001product Leaflet Approved.160607Document9 pages2160202.PA0749 - 113 - 001..000001product Leaflet Approved.160607Banwari LalNo ratings yet
- Fenofibrate 267mg Capsules - Summary of Product Characteristics (SMPC) - Print Friendly - (Emc)Document8 pagesFenofibrate 267mg Capsules - Summary of Product Characteristics (SMPC) - Print Friendly - (Emc)bhavaniNo ratings yet
- Anti EpilepticsDocument23 pagesAnti EpilepticsSalman HabeebNo ratings yet
- Pil - Ma032 06401Document7 pagesPil - Ma032 06401ntecbd1No ratings yet
- Flouxetine Drug StudyDocument7 pagesFlouxetine Drug Studyhello poNo ratings yet
- See Full Prescribing Information For Complete Boxed WarningDocument25 pagesSee Full Prescribing Information For Complete Boxed WarningGag PafNo ratings yet
- Wellbutrin SR Pi MG PDFDocument37 pagesWellbutrin SR Pi MG PDFAlfyGototronNo ratings yet
- Tachipirina Orosolubile: 500 MG Granules, Strawberry-Vanilla FlavorDocument3 pagesTachipirina Orosolubile: 500 MG Granules, Strawberry-Vanilla Flavordenis troshaniNo ratings yet
- Vol 14 No 2a Vortioxetine For Depression Jan 2016Document2 pagesVol 14 No 2a Vortioxetine For Depression Jan 2016John SmithNo ratings yet
- Basic Pharmacology And Drug Calculations [Practice Questions And Answers]From EverandBasic Pharmacology And Drug Calculations [Practice Questions And Answers]Rating: 4 out of 5 stars4/5 (1)
- Medical Encyclopedia XXL: Prof. J.P. Schadé, M.D., Ph.D. D.Sc.hcFrom EverandMedical Encyclopedia XXL: Prof. J.P. Schadé, M.D., Ph.D. D.Sc.hcNo ratings yet
- Thinking Outside The Lungs: A Case of Disseminated Abdominal TuberculosisDocument6 pagesThinking Outside The Lungs: A Case of Disseminated Abdominal TuberculosisDumitru RadulescuNo ratings yet
- Journal of Medical Case ReportsDocument5 pagesJournal of Medical Case ReportsDumitru RadulescuNo ratings yet
- Case Report: A Case Report of Peritoneal Tuberculosis: A Challenging DiagnosisDocument4 pagesCase Report: A Case Report of Peritoneal Tuberculosis: A Challenging DiagnosisDumitru RadulescuNo ratings yet
- Caz Bun 7Document2 pagesCaz Bun 7Dumitru RadulescuNo ratings yet
- Peritoneal Carcinomatosis and Its Mimics - Review of CT Findings For Differential DiagnosisDocument6 pagesPeritoneal Carcinomatosis and Its Mimics - Review of CT Findings For Differential DiagnosisDumitru RadulescuNo ratings yet
- Endoscopia: Diagnostic Approach of Intestinal Tuberculosis: Case and Literature ReviewDocument4 pagesEndoscopia: Diagnostic Approach of Intestinal Tuberculosis: Case and Literature ReviewDumitru RadulescuNo ratings yet
- Caz Bun 3Document7 pagesCaz Bun 3Dumitru RadulescuNo ratings yet
- Tuberculous Peritonitis The Effectiveness of Diagnostic Laparoscopy and The Perioperative Infectious Prevention - A Case ReportDocument4 pagesTuberculous Peritonitis The Effectiveness of Diagnostic Laparoscopy and The Perioperative Infectious Prevention - A Case ReportDumitru RadulescuNo ratings yet
- Pooled Analysis of 163 Published Tuberculous Peritonitis Cases From TurkeyDocument7 pagesPooled Analysis of 163 Published Tuberculous Peritonitis Cases From TurkeyDumitru RadulescuNo ratings yet
- Tuberculous Peritonitis Presenting As An Acute Abdomen: A Case ReportDocument4 pagesTuberculous Peritonitis Presenting As An Acute Abdomen: A Case ReportDumitru RadulescuNo ratings yet
- Analysis of Recent Cases of Intestinal Tuberculosis in JapanDocument6 pagesAnalysis of Recent Cases of Intestinal Tuberculosis in JapanDumitru RadulescuNo ratings yet
- Peritoneal Tuberculosis: The Great Mimicker: Case StudyDocument5 pagesPeritoneal Tuberculosis: The Great Mimicker: Case StudyDumitru RadulescuNo ratings yet
- NLR Blood Neutrophil To Lymphocyte Count As A Prognostic Marker in Liver Cirrhosis PDFDocument124 pagesNLR Blood Neutrophil To Lymphocyte Count As A Prognostic Marker in Liver Cirrhosis PDFDumitru RadulescuNo ratings yet
- Factors Contributing To SMALL INTESTINE Suture Line Disruption PDFDocument117 pagesFactors Contributing To SMALL INTESTINE Suture Line Disruption PDFDumitru RadulescuNo ratings yet
- A Prospective Comparative Study Between Staplers and Conventional Hand-Sewn Anastomosis in Gastrointestinal SurgeryDocument126 pagesA Prospective Comparative Study Between Staplers and Conventional Hand-Sewn Anastomosis in Gastrointestinal SurgeryDumitru RadulescuNo ratings yet
- De TradusDocument13 pagesDe TradusDumitru RadulescuNo ratings yet
- Articol Pneumonii 2016Document18 pagesArticol Pneumonii 2016Dumitru RadulescuNo ratings yet
- RCCHEM Semi-Auto ChemistryV1.1Document61 pagesRCCHEM Semi-Auto ChemistryV1.1Sumit AhirNo ratings yet
- Pulmonary EmbolismDocument23 pagesPulmonary EmbolismBianca Dizon50% (2)
- Hemostasis Intensive Exam Rationale - Louise MDocument9 pagesHemostasis Intensive Exam Rationale - Louise MKai YoungNo ratings yet
- Seminar - Hemorrhage 25-06-2020Document75 pagesSeminar - Hemorrhage 25-06-2020Chandra dimpleNo ratings yet
- Test For Secondary HemostasisDocument32 pagesTest For Secondary Hemostasistitania izaNo ratings yet
- Sample-Questions-Part 2-OSCEDocument10 pagesSample-Questions-Part 2-OSCEaram meyedyNo ratings yet
- Transfusi BlokDocument96 pagesTransfusi BlokTutde SedanaNo ratings yet
- CAP Cross CheckDocument4 pagesCAP Cross CheckRafat ElshemiNo ratings yet
- Research Proposal Draft 3Document40 pagesResearch Proposal Draft 3layla kambalaNo ratings yet
- Humaclot Duo Plus MANUAL PDFDocument54 pagesHumaclot Duo Plus MANUAL PDFRodrigo RiveraNo ratings yet
- Evaluare Pacient - Scor HAS-BLED: H A S B L E DDocument2 pagesEvaluare Pacient - Scor HAS-BLED: H A S B L E Dviorel79No ratings yet
- PDF Nursing Care PlanDocument16 pagesPDF Nursing Care PlanMichael MabiniNo ratings yet
- BOOST Pharm Review - Introduction To Pharm, PNS, Cardiac - ANSWERSDocument24 pagesBOOST Pharm Review - Introduction To Pharm, PNS, Cardiac - ANSWERSHwi GNDCNo ratings yet
- FSBGD MCQ Study Questions 2001Document84 pagesFSBGD MCQ Study Questions 2001api-2629165192% (12)
- Mateo NCM 118Document12 pagesMateo NCM 118Nicole SedaNo ratings yet
- Surgery RobaDocument26 pagesSurgery Robaroba shukreNo ratings yet
- Clinical Predictors of Prognosis in Patients With Traumatic Brain Injury Combined With Extracranial TraumaDocument9 pagesClinical Predictors of Prognosis in Patients With Traumatic Brain Injury Combined With Extracranial TraumaVinnie Juliana YonatanNo ratings yet
- CardinalDocument64 pagesCardinalMarc Conrad MolinaNo ratings yet
- Bloody Easy - Coagulation ExplainedDocument25 pagesBloody Easy - Coagulation ExplainedDaniela GreereNo ratings yet
- Nursing Quiz AnticoagulantsDocument3 pagesNursing Quiz AnticoagulantsChieChay Dub100% (4)
- Bridging Anticoagulation JACC 2015Document12 pagesBridging Anticoagulation JACC 2015Frans LiwangNo ratings yet
- Teaching Medical Students Basic Principles of Laboratory MedicineDocument14 pagesTeaching Medical Students Basic Principles of Laboratory MedicineIrish De VeraNo ratings yet
- Anticoagulant ReversalDocument4 pagesAnticoagulant Reversalapi-647779956No ratings yet
- Cardiovascular Practice Questions Answers and RationalesFALL2019-1Document11 pagesCardiovascular Practice Questions Answers and RationalesFALL2019-1titilayo loveNo ratings yet
- PBM Module1 MTP Template 0Document2 pagesPBM Module1 MTP Template 01234chocoNo ratings yet
- DsDocument4 pagesDseloisa rabanesNo ratings yet





























































![Basic Pharmacology And Drug Calculations [Practice Questions And Answers]](https://imgv2-2-f.scribdassets.com/img/word_document/475660044/149x198/2c7fc45015/1691161640?v=1)











































