Professional Documents
Culture Documents
Treatment Plan 6
Uploaded by
api-433536062Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Treatment Plan 6
Uploaded by
api-433536062Copyright:
Available Formats
INTERVENTION PLAN FOR COMMUNITY CLIENT WITH REFLECTION
Copy/paste one LTG and the matching STG from your evaluation SOAP note. This will be the goal set around which you design your treatment session.
For this and all subsequent weeks, please answer the following questions before designing your treatment plan for the next week. If you were unable to see
your client the past week, you do not need to answer these questions. Answer the questions based on the treatment that you implemented:
What went well with your treatment? Did things go as you planned or not? Explain. What will you do differently with this next treatment plan?
Client did not attend treatment session due to a family funeral.
Long-Term Goal: By discharge, client will independently place contacts in both eyes with use of a one-handed
technique.
Short-Term Goal: Within 2 sessions, client will independently use finger to manipulate eyelid 80% wide in
preparation for placement of contact.
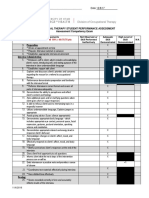
OCCUPATIONAL OPM and CPM TREATMENT SESSION GRADING THE ACTIVITY
PERFORMANCE PROBLEM AND RATIONALE DESCRIPTION Choose one client factor or
Specifically identify only the client Identify your OPM and all relevant Provide details of how you will set up performance skill that you address
factors and/or performance skills CPM’s that best addresses the the activity and how your intervention in your treatment session. Describe
that are barriers to the performance problem and describe addresses the performance problem. one way (only one) that you can
achievement of this goal. This how each will be used to design Your description should detail how grade the activity up and one way
should not be a bullet list, rather treatment for this client’s specific the activity will be set up to make it (only one) to grade the activity
you should describe how the client problems. therapeutic. down based on that one factor or
factor impacts this client’s skill.
performance of the occupation in
the goal. Factor/Skill:
PEO: Ways to facilitate task:
Our client is currently unable to put The main outcome of this model is First we will work on opening the Make the activity closed chain by
his contacts in independently due to increase the client’s satisfaction contact container. The client will use placing his L elbow on a table to
to his inability to grip and with their occupational his R hand to stabilize the bottom of decrease the number of joints used
manipulate objects, as well as grab performance. Our client is currently the container, and use his L hand to in his LUE
and release objects with his R dissatisfied with being dependent untwist the top open. Once the
hand. He can initially use a pincer on his girlfriend to put his contacts container has been opened, he will Provide something for his 3rd digit to
grasp and a 3-jaw chuck to grab in. The client will need use his L index finger to take the create friction to open up his eye
and release 1 inch items, but after modifications and adaptations to contact out of the container. He will better, such as a rubber thimble
3-5 repetitions, his tone increases the occupation/task as well as the then lift his R hand and place it close
in digits 1-3 and he cannot extend environment to be able to put his to his body at about chest level in a Utilize a mirror
his fingers to grab and release contacts in independently. This will, pronated fist position, where he will
items. Once his tone increases, he in turn, increase his satisfaction in place the concave side of the contact
uses a raking grasp with digits 4-5. his occupational performance. faced up on the dorsal side of his R
He has hemiplegia in his RUE and hand.
moves in a flexor synergy pattern. Rehabilitation model:
His PROM in his RUE are WFL, Client wants to be able to put his Once the contact is on his R hand,
however, when he activates his contacts in independently. To be he will use his L index finger and pick
RUE, he can activate 160 degrees able to accomplish this goal, this up the contact so that the concave
of shoulder flexion- but has treatment session will focus on side of the contact is placed in the
difficulty extending his wrist and teaching him a compensatory one- middle of his distal phalanx. Once
fingers to reach for items in high handed technique using his L hand the contact is in this position, the
shelves, 85 degrees of shoulder to place the contacts in his eyes. client will bring his L index finger up
abduction, and 45 degrees of MCP towards the center of his eye, and
flexion. He has some finger Motor Control/Motor Learning use his 3rd digit to pull his lower eye
extension in digits 4-5, about 2-5 model: While learning a one- lid down. He will then look up while
degrees. He has limited finger handed technique with his L hand, his eyelid is pulled down so that his
extension and cannot actively he will incorporate his RUE into the eye is opened wide enough to fit the
open his R hand fully. He activity to increase the use of his size of the contact, and then place
displayed difficulty extending his paretic arm through task specific the contact in his eye with his index
wrist and MCP/finger extension in training in order to strengthen the finger.
digits 1-3. He also displays neglect neuropathways. He will utilize his
of his RUE, proprioception deficits, RUE into the task such as He will practice the motion of this
and no tactile sensation issues. stabilizing the contact container one-handed technique multiple times
while his L hand twists the cap without the contact on his finger so
open to help decrease R neglect. that he can work on pulling his eyelid
down with his 3rd digit, and looking
up at the same time. We will provide
him feedback and verbal cueing to
correct his positioning or if he needs
to pull down his lower eyelid more or
remind him to look up. Once he has
practiced this motion, he will then
practice putting his actual contact in.
Home Program:
-continue practicing one-handed technique to put in contacts
-keep track of how many times you practice every day, and how many times you succeed
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- BSS 3rd Edition Participant Handbook CD FinalDocument75 pagesBSS 3rd Edition Participant Handbook CD FinalUhuebor David100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Piano Junior Lession Book 1Document49 pagesPiano Junior Lession Book 1Thu Trang Vũ100% (1)
- Ot and VisionDocument25 pagesOt and Visionapi-433536062100% (1)
- Ot Program FinalDocument59 pagesOt Program Finalapi-433536062No ratings yet
- Normandy J 2017 Peds Spa Interview Competency Rubric-2Document2 pagesNormandy J 2017 Peds Spa Interview Competency Rubric-2api-433536062No ratings yet
- Discharge NoteDocument4 pagesDischarge Noteapi-433536062No ratings yet
- Power Forearms PDFDocument36 pagesPower Forearms PDFMike100% (2)
- Biligválne Gymnázium Milana Hodžu, Sučany: Investigation Physiology of Sensory OrgansDocument7 pagesBiligválne Gymnázium Milana Hodžu, Sučany: Investigation Physiology of Sensory OrgansPaulína PalčinskáNo ratings yet
- 2006, Vol.24, Issues 3, Nail Disorders and Their ManagementDocument105 pages2006, Vol.24, Issues 3, Nail Disorders and Their ManagementRizweta DestinNo ratings yet
- Growth and Development of FaceDocument12 pagesGrowth and Development of FaceARJUN SreenivasNo ratings yet
- Yoga Massage Therapy BookDocument54 pagesYoga Massage Therapy BookKhadi MadamaNo ratings yet
- Distal Phalangeal Fingertip InjuriesDocument140 pagesDistal Phalangeal Fingertip InjuriesiwanbaongNo ratings yet
- A Low-Cost Open-Source 3-D-Printed Three-Finger Gripper Platform For Research and Educational PurposesDocument10 pagesA Low-Cost Open-Source 3-D-Printed Three-Finger Gripper Platform For Research and Educational PurposesAtakan DelikanNo ratings yet
- Sri Akshobhya Bhairava MahamantraDocument9 pagesSri Akshobhya Bhairava MahamantraSHAILESH PURANIKNo ratings yet
- Neon Anarchist Cookbook Playtest - PegasusDocument51 pagesNeon Anarchist Cookbook Playtest - Pegasuscaroline llewellyn100% (1)
- Master Tong Information Document PDFDocument105 pagesMaster Tong Information Document PDFKimberly100% (2)
- Energy Healing Exercises HandoutDocument1 pageEnergy Healing Exercises HandoutRandall HallNo ratings yet
- Building Machines That Emulate Humans: Lesson Plan and More Resources Are Available At: Aka - Ms/hackingstemDocument34 pagesBuilding Machines That Emulate Humans: Lesson Plan and More Resources Are Available At: Aka - Ms/hackingstemAndré FozzyNo ratings yet
- Sumukhi MantraDocument14 pagesSumukhi MantraRN100% (1)
- Criminalistic SDocument137 pagesCriminalistic SSheila Mae CaballaNo ratings yet
- NYSSH Orthopaedic MCQ Hand QuestionsDocument38 pagesNYSSH Orthopaedic MCQ Hand QuestionsLuisAngelPonceTorresNo ratings yet
- Linck S. R. - Combat Jiu Jitsu PDFDocument64 pagesLinck S. R. - Combat Jiu Jitsu PDFnautilus81100% (2)
- Key Basketball FundamentalsDocument69 pagesKey Basketball FundamentalsKrishan KantNo ratings yet
- Secrets of The Pulse Vasant Lad 09743 1 PDFDocument19 pagesSecrets of The Pulse Vasant Lad 09743 1 PDFdcode workNo ratings yet
- Erotic MassageDocument113 pagesErotic MassageMahmoud El Mohamdy75% (4)
- Closed Gloving: Using The Closed-Gloves Technique Put On The Sterile GlovesDocument2 pagesClosed Gloving: Using The Closed-Gloves Technique Put On The Sterile GlovesCindy Cabales AbellanaNo ratings yet
- 12 Ways To Exercise Hands and FingersDocument6 pages12 Ways To Exercise Hands and FingersAri WidiyantoNo ratings yet
- IP Injection Protocol in MiceDocument3 pagesIP Injection Protocol in Miceadan ranaNo ratings yet
- Clinical Significance of Upper LimbDocument3 pagesClinical Significance of Upper LimbflissxloveNo ratings yet
- Carbon-X Fire Shark GloveDocument1 pageCarbon-X Fire Shark GlovesepehrccNo ratings yet
- The Contents of Anatomical Snuff Box AreDocument3 pagesThe Contents of Anatomical Snuff Box AreZimam ZamriNo ratings yet
- Horgoláshoz Kéz BemelegítésDocument1 pageHorgoláshoz Kéz BemelegítésKrisztaNo ratings yet
- How To Play CastanetsDocument1 pageHow To Play CastanetsAlesya CalinNo ratings yet
- Wrist and Finger SeminarDocument40 pagesWrist and Finger SeminarMisoNo ratings yet