Professional Documents
Culture Documents
Laparoscopic Appendicectomy in All Trimesters of Pregnancy
Uploaded by
Jason CalvinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Laparoscopic Appendicectomy in All Trimesters of Pregnancy
Uploaded by
Jason CalvinCopyright:
Available Formats
SCIENTIFIC PAPER
Laparoscopic Appendicectomy in all Trimesters
of Pregnancy
Norman Oneil Machado, MBBS, MS, FRCSEd, Christopher S. Grant, FRCS
ABSTRACT INTRODUCTION
Background: The laparoscopic approach for appen- Appendicectomy is the most common nonobstetric oper-
dicectomy in pregnancy was not considered the preferred ation during pregnancy.1,2 Pregnancy was a relative con-
procedure until recently. The aim of this study was to traindication to laparoscopy until recently because of the
examine our experience with laparoscopic appendicec- belief that the procedure would decrease uterine and fetal
tomy in pregnancy and review the scientific evidence blood flow and result in abortion or possibly influence
available in the medical literature. fetal development. Several reports of successful laparo-
scopic procedures in pregnancy have indicated the safety
Method: The clinical data of all patients who underwent
of laparoscopy in pregnancy.3–30 However, a recent re-
laparoscopic appendicectomy during pregnancy at our
view of laparoscopic appendicectomy in pregnancy re-
hospital between 1999 and 2007 were collected and ret-
ported a significantly higher fetal loss rate compared with
rospectively analyzed. A Medline literature search re-
open appendicectomy and has raised some concerns.31
stricted to English language articles on laparoscopic ap-
Our experience is presented here, and the available liter-
pendicectomy in pregnancy was carried out.
ature is reviewed, regarding the present status of laparo-
Result: Twenty patients underwent laparoscopic appen- scopic appendicectomy in pregnancy.
dicectomy during pregnancy. Of these, 8 were in the first
trimester, 9 in the second trimester, and 3 in the third METHODS
trimester. Fifteen patients had histologically confirmed
appendicitis. The mean operating time was 45 minutes, The data for all patients undergoing laparoscopic appen-
and the average postoperative stay in the hospital was 1.5 dicectomy during pregnancy in our hospital from January
days. All patients except one had a full-term normal de- 1999 to January 2007 were analyzed. The data studied
livery. Literature search: An additional 637 patients from included presentation, estimated weeks of gestation at
the English literature were reviewed and summarized. presentation, procedures, intraoperative findings, compli-
cations, and the outcome of laparoscopic appendicec-
Conclusion: Our results demonstrate that laparoscopic tomy. The birth records were also reviewed for outcome,
appendicectomy can be safely performed during all tri- including gestational age at delivery, birth weight, and
mesters of pregnancy. The literature search suggests that Apgar score.
although laparoscopic appendicectomy in pregnancy is
associated with a low rate of intraoperative complications Operative Technique
in all trimesters it may be associated with a significantly
higher rate of fetal loss compared with open appendicec- The procedure was carried out with the patient under
tomy. general anesthesia with end tidal carbon dioxide monitor-
ing that was maintained within the physiological range (30
Key Words: Laparoscopic appendectomy, Pregnancy, mm Hg to 40 mm Hg). A Foley catheter was inserted in all
Abortion. patients and removed at the end of the surgery. Patients
were tilted to the left to displace the uterus from the IVC.
In the initial 3 cases, pneumoperitoneum was carried out
using a Veress needle. In all the later cases, pneumoperi-
Senior Consultant, Department of Surgery, Sultan Qaboos University Hospital
Muscat/Sultanate of Oman (Dr Machado)., Professor & Chairman, Department of
toneum was carried out using an open (Hasson) tech-
Surgery, Sultan Qaboos University Hospital, Muscat/Sultanate of Oman (Dr Grant). nique. The pneumoperitoneum pressure was maintained
Address reprint requests to: Dr. Norman Machado, Senior Consultant, Department between 10mm Hg to 12mm Hg. Fetal heart rate was
of Surgery, Sultan Qaboos University Hospital, PO Box 38, Postal Code 123, recorded immediately before and after surgery.
Muscat/Sultanate of Oman. E-mail: norman@omantel.net.om
© 2009 by JSLS, Journal of the Society of Laparoendoscopic Surgeons. Published by The procedure was always performed using 3 ports, and
the Society of Laparoendoscopic Surgeons, Inc. their placement was modified in accordance with gesta-
384 JSLS (2009)13:384 –390
tional age. The first port (10 mm) was placed 2 cm ceph- gery within 12 hours of admission, 5 within 24 hours, 4
alad to the gravid uterus in the upper midline between the within 48 hours, and one after 72 hours. A preoperative
umbilicus and xiphoid process. The second port (5 mm) obstetric assessment was carried out in all the patients.
was placed laterally in the right lower quadrant, and the After an informed consent, laparoscopic appendicectomy
third port (10 mm) was placed in the right upper quadrant was performed.
in a more cranial location. The appendix was ligated with
endoloops and extracted after the entire appendix was The details of our patients including the operative findings
placed within the 10-mm port to reduce the possibility of and outcome are outlined in Table 1. The intraoperative
contamination of the port site. Patients were administered findings included inflamed appendix in 12 patients,
antibiotics (cefuroxime and metronidazole), and the du- phlegmonous appendix in 2, appendicular mass in 1, and
ration of antibiotic therapy was 24 hours for acute appen- normal appendix in 5 patients. Fifteen patients had histo-
dicitis and 2 days to 3 days for phlegmonous appendicitis. logically proven appendicitis. Among the 5 patients with a
Oral intake was started on the first postoperative day, and normal appendix, the abnormal findings included omen-
tocolysis in the form of indomethacin 100 mg suppository tal adhesions to the right fallopian tube and cecum (2
was given to 4 patients because of uterine contractility on patients) and an appendicular fecalith and torsion of the
the advice of the obstetrician. ovary in one patient each. The average duration of surgery
was 45 minutes (range, 25 to 90). The hospital stay ranged
Literature Review from 3 days to 8 days (mean, 3.5). A delay in surgery of
A review of the literature was carried out by searching the more than 24 hours after admission was noted in 5 pa-
Medline database selecting only studies published in En- tients. These included those who were primarily admitted
glish that described well-documented cases of laparo- under an obstetrician’s care or had atypical presentation.
scopic appendicectomy in patients with intrauterine preg- The mean postoperative stay in the hospital was 1.5 days
nancy and those in whom the surgical and obstetric (range, 1 to 5). In 2 patients, the postoperative stay was
outcome were clearly linked to the operative approach. longer than 3 days; these include the patient with appen-
Studies with incomplete or confusing data were rejected. dicular mass and the one with hydronephrosis. The pa-
tient with hydronephrosis developed Klebsiella pneumo-
RESULTS nia that was effectively treated with antibiotics and
supportive treatment. This patient was discharged on the
During the period under review, 16 803 deliveries were fifth postoperative day after the fever subsided. The other
conducted by the obstetrical service. Twenty-six appen- patient with appendicular mass had postoperative ileus
dicectomies were performed during pregnancy, an inci- for 2 days and was mildly febrile. These symptoms im-
dence of 0.15%. In 6 cases, an open procedure was cho- proved by the third postoperative day, and the patient was
sen before surgery because of advanced gestational age or discharged a day later. None of these patients developed
patient preference. The data of the remaining 20 patients wound complications, including wound infection in the
who underwent laparoscopic appendicectomy are sum- immediate postoperative period and port-site hernia fol-
marized in Table 1. lowing subsequent follow-up. No other postoperative
Fourteen patients had acute pain located at McBurney’s complications were seen. All patients except one had a
point. In 2 cases, the pain was located in the right flank, full-term normal delivery. The exception was a patient
and 4 had central abdominal pain. The temperature with a past history of recurrent abortion who aborted 3
ranged from 37°C to 38.5°C (mean temperature, 37.5°C), weeks following appendicectomy. No perinatal deaths
and WBC count ranged from 7.1x109/L to 18x109/L (mean, occurred. The birth weights of the infants ranged from
15.7x109/L). Ultrasound of the abdomen was carried out 3050 g to 3400 g (mean, 3200), and the mean Apgar score
in 10 patients in whom the diagnosis was uncertain. The at 5 minutes was 9 (range, 8 to 10). Normal milestones
findings included pericecal fluid collection in 5, thickened were observed in all infants at 1-year follow-up.
edematous appendix in 2, and hydronephrosis in one
patient. Four patients were initially admitted under an The English literature search yielded 28 main reports with
obstetrician’s care and then transferred to the surgical a total of 637 patients who underwent laparoscopic ap-
service once a diagnosis of acute appendicitis was enter- pendicectomy during pregnancy3–31 and matched our in-
tained. The remaining patients were admitted primarily clusion criteria and are included in the review. The data
under the surgical service. Ten patients underwent sur- are summarized in Table 2.
JSLS (2009)13:384 –390 385
Laparoscopic Appendicectomy in all Trimesters of Pregnancy, Machado NO et al.
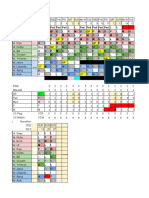
Table 1.
Operative Details and Outcome in Patients Undergoing Laparoscopic Appendectomy in This Series
Patient Age Gestation Abdominal Entry Operative Finding Operative Outcome of Hospital
No. (years) (weeks) (Veress Needle/ Time Pregnancy Stay
Hasson Technique) (min) Delivery (days)
(weeks)
1 26 20 V Acute appendicitis 48 38 3
2 30 13 H Appendicular mass 55 39 7
3 19 22 V Fecalith normal 30 39 4
appendix
4 26 16 V Acute appendicitis 60 40 3
5 27 9 H Acute appendicitis 50 Abortion 3
6 19 25 H Normal appendix 35 38 8
right hydronephrosis
7 23 26 H Acute appendicitis 42 39 3
8 31 12 H Omental adhesions to 40 38 3
right salpinx normal
appendix
9 38 10 H Mucocele of 35 39 3
appendix
10 22 13 H Acute appendicitis 50 38 3
11 24 11 H Acute appendicitis 40 39 3
12 20 15 H Omental adhesions to 45 40 3
caecum / right
salpinx normal
appendix
13 24 12 H Acute appendicitis 40 38 3
14 21 24 H Acute appendicitis 60 40 3
15 26 28 H Acute appendicitis 55 39 3
16 19 13 H Acute appendicitis 40 40 3
17 24 23 H Torsion of right ovary 55 39 4
normal appendix
18 28 10 H Phlegmonous 65 40 4
appendicitis
19 25 24 H Acute appendicitis 55 40 4
20 19 14 H Acute appendicitis 45 38 3
DISCUSSION trimester (69%) compared with the first and second tri-
mester.33 Twenty-five per cent of all pregnant women
Acute appendicitis is the most common cause of nonob- who have acute appendicitis will progress to perfora-
stetric acute abdomen during pregnancy, with a reported tion.34 A 66% perforation incidence has been reported
incidence of 0.05% to 0.1%.1,2,21 Even though the inci- where surgery is delayed by more than 24 hours com-
dence of acute appendicitis in pregnancy has been con- pared with 0% incidence when surgical management is
sidered identical to that in the nonpregnant population, a initiated prior to 24 hours after presentation.35
recent case control study suggested a lower incidence in
pregnant women, with the third trimester being particu- The difficulty in making a clinical diagnosis particularly
larly protective.32 However, it has been noted that perfo- close to term combined with the previously quoted high
ration of the appendix occurs twice as often in the third incidences of fetal and maternal mortality for appendiceal
386 JSLS (2009)13:384 –390
Table 2.
Laparoscopic Appendectomy During Pregnancy Literature Review
Study n Trimester V / H* MP* MOT* (min) Tocolysis Introp Postop Preterm Fetal
(1; 2; 3) (mmHg) Complications Complications Delivery Loss
Present study 20 8; 9; 3 3/17 10–12 45 4 — — — 1
12
Andreoli 5 0; 5; 0 NI 12 40 — — — — —
Affleck3 19 6; 9; 4 NI NI 54.5 4 — NI 3 —
14
Amos 3 0; 3; 0 -/3 12 NI — NI NI 1
Barnes20 2 0; 0; 2 -/2 12 60 1 NI — —
22
Buser 1 0; 1; 0 NI NI NI NI — — — —
Carver9 17 5; 12; 0 NI NI NI — — — — 2
Curet 21 4 0; 4; 0 -/6 10–15 82 — — — — —
dePerrot11 6 2; 2; 2 1/5 12 51.6 3 — — 1 2
23
Friedman 1 0; 1; 0 1/- NI NI — 1 1 1 1
Geisler24 2 0; 2; 0 2/- 15 NI — — — — —
Gurbuz13 5 2; 0; 3 -/5 12 64 — — — — —
Halkic6 11 0; 11; 0 0/11 10–12 45 — — — — —
25
Hee 7 NI NI NI NI NI — — — —
Lemaire18 4 1; 3; 0 4/- 12 33.7 1 — — — —
Lyass10 11 5; 4; 2 0/1 12 46 11 — — — —
McGory31 454 NI; NI; NI — — — — — — 1 31
Moreno-Sanz4 6 4; 2; — 0/6 12 46 0 — — 1 —
Palanivelu7 7 0; 7; 0 6/1 NI NI NI 0 0 0 0
16
Posta 1 0; 1; 0 -/1 12 70 — — — — —
Radwan26 1 1 NI 10–12 — — — — — —
27
Rizzo 4 0; 4; 0 -/4 10 25–90 — — — 2 —
Rollins5 28 6; 13; 9 17/11 15 46.3 6 — NI 6 —
19
Schreiber 6 2; 4; 0 6/- NI NI 1 — — NI —
Schwartzberg15 1 1; 0; 0 -/1 15 NI — — — — —
Spirtos28 13 NI — — — 1 —
Thomas29 2 2; 0; 0 -/2 NI NI NI — — 1 —
30
Tracey 3 1; 2; — — — — — — — — —
Wu8 11 4; 6; 1 0/11 NI 50.5 3 — 1 — 1
*V ⫽ Veress needle; H ⫽ Hasson technique; MP ⫽ mean pneumoperitoneum pressure; MOT ⫽ mean operative time; NI ⫽ not
indicated.
perforation has led to a traditionally low threshold for Use of laparoscopic procedures has rapidly gained accep-
surgical intervention. This has resulted in a higher nega- tance in the treatment of patients with appendicitis. In a
tive appendicectomy rate, ranging from 23% to 55% in study of 3133 pregnant patients who underwent appen-
pregnant women compared with 18% in nonpregnant dicectomy,31 the laparoscopic approach was used in 14%
women (P⬍0.05).4,25,29,31,32,36 However, of concern was of pregnant women compared with 23% of nonpregnant
the finding in the systematic review by Walsh et al36 who women. This change in approach stems from the fact that
noted that fetal loss rates in the group with no evidence of laparoscopic appendicectomy, in addition to its general
appendicitis were as high as for those with simple appen- advantage of a smaller incision, less postoperative pain,
dicitis. and earlier return to normal activity, offers other potential
JSLS (2009)13:384 –390 387
Laparoscopic Appendicectomy in all Trimesters of Pregnancy, Machado NO et al.
advantages for pregnant women.3– 6,10 Laparoscopy can nant patients in accordance with SAGES recommenda-
result in less manipulation of the uterus while obtaining tions.38 The remaining trocars can be positioned accord-
optimum exposure of the surgical field and could reduce ing to the preferences of the surgical team but always
delays in diagnosis and treatment. It affords easier visual- displaced cephalad to avoid the uterine fundus. It is rec-
ization and treatment of ectopically located appendix or ommended that the patient be placed on her left side after
helps in detecting other unexpected sources of pain as in the second term of pregnancy to prevent uterine compres-
4 of our patients.10,11 Lower rates of dehiscence or herni- sion of the vena cava and to facilitate access to the ap-
ation during labor are another potential benefit. Rapid pendix.4,37 This can be achieved by tilting the operating
return to full activity could reduce the frequency of ma- table to the left; it is unnecessary to place the patient in a
ternal thrombosis and embolic events, which can be a strict lateral decubitus position.4 In a recent review,36 the
major source of maternal mortality in some patients.4,11,21 mode of laparoscopic entry was documented in 116 cases;
the open (Hasson) technique was used in 68% of cases
The major concerns, however, have been the potential compared with the use of the Veress needle in 32% cases.
effects of pneumoperitoneum on fetal physiology and the
possibility of injury to the uterus during the operation. The Tocolytic agents are used in patients either prophylacti-
effects of laparoscopic appendicectomy due to increased cally or following the development of postoperative uter-
intraabdominal pressure and fetal acidosis during CO2 ine contractions. However, a recent review revealed no
pneumoperitoneum have been looked into in clinical or statistical difference in the rate of preterm delivery among
experimental studies, and no substantial adverse effects the prophylactic tocolysis group (0/15) and the nontoco-
for the fetus have been found when the maximal pneu- lysis group (3/79; P⫽0.59).36 Hence, the use of prophy-
moperitoneum pressure was limited to 10mm Hg to 12mm lactic tocolytic agents is not indicated but can be appro-
Hg for a duration of ⬍60 minutes.21,37 Although studies priate if there are obstetric criteria as evidenced by uterine
have demonstrated that laparoscopy can be performed contractions and risk of premature birth.4,36,37 This has
safely during any trimester with good fetal and maternal been the practice in our unit.
outcomes, the long-term effects on the child after delivery The need for continuous fetal monitoring by ultrasonog-
have not been well studied. However, one recent study27 raphy scans has been reported previously.17,38 Despite
evaluating 11 children from 1 year to 8 years whose being SAGES recommendations, this measure has been
mothers underwent surgery during pregnancy found no abandoned because it is difficult to carry out and has a
growth or developmental delay in these children. low efficacy.4 Most of the recent recommendations con-
Guidelines for laparoscopic procedures during pregnancy sider it essential to have uterine and fetal monitoring
have previously been published by the Society of Ameri- before and after operations rather than intraoperatively,
can Gastrointestinal and Endoscopic Surgeons38 and mod- and some would repeat this just before the discharge of
ifications have been proposed by Moreno-Sanz et al.4 A their patients.3–5,11
pneumoperitoneum pressure of ⬍12 mm Hg is recom- Operative times were reported in 110 cases (mean 51⫾13
mended, because previous animal studies have demon- min)(median, 46). The mean operative times were 45, 51,
strated fetal hypercapnia and acidosis secondary to CO2 and 59 minutes for procedures in the first, second, and
pneumoperitoneum in pregnant ewes.39 However, sub- third trimesters, respectively.36 This has been quicker than
stantial adverse effects to the fetus with pneumoperito- the recently reported median operating time for laparo-
neum limited to 10 mm Hg to 12 mm Hg have not been scopic appendicectomy (LA) in a nonpregnant population
demonstrated.21,39 (median 60 min) and may reflect the fact that the laparo-
scopic procedure in pregnancy is usually performed by
Some controversy exists about the best approach to access
experienced surgeons.36,40 This is supported by the low
the abdomen and to create the pneumoperitoneum. Com-
(1%) rate of conversion to laparotomy that is better than
plications have been described for all techniques, but
most published rates of nonpregnant patients.36 The mean
accidental puncture of the uterus with a Veress needle is
stay was 5⫾3.8 days. Information on the use of intraop-
the most serious.21,23 Open access to the abdomen was the
erative antibiotics was sparse, with antibiotic administra-
most common approach reported in the literature re-
tion routinely in 29/36 cases.36
viewed,6,8,9,11,13,15,17,20,27,29 but the Veress needle was only
routinely used in 3 studies.18,19,24 The correct use of the Advanced pregnancy was initially considered a relative
Hasson technique is completely safe and reproducible contraindication by authors who suggested the gestational
and is recommended as the standard technique in preg- age limit for successful completion for laparoscopic sur-
388 JSLS (2009)13:384 –390
gery during pregnancy should be 26 weeks to 28 who underwent appendectomy via a laparoscopic approach
weeks.14,17 However, there are several reports of success- despite a higher rate of nonappendicitis in this group.31
ful laparoscopic appendicectomy carried out in patients Hence, it appears that negative appendectomy is not entirely
beyond the estimated gestational age of 26 weeks.3,5,20 a benign intervention in a pregnant woman, and the risk of
Review of the literature reveals gestational age being re- misdiagnosis needs to be carefully balanced against the risks
corded in 155 cases. Of these, 52, 77, and 26 women of perforation from a delay in diagnosis.
underwent LA in the first, second, and third trimesters of
pregnancy, respectively. The mean (standard deviation) CONCLUSION
gestational age at the time of LA was 17.9 weeks
(SD⫾5.7). Among the patients in the third trimester, 8 Laparoscopic appendicectomy is technically feasible in all
were in advanced pregnancy with the gestational age trimesters of pregnancy and is associated with the same
above 30 weeks.3,5,20 Even though successful LA has been benefits of laparoscopic surgery experienced in nonpreg-
carried out in advanced pregnancy, some feel that the size nant patients, provided the specific recommendations for
of the gravid uterus in the third trimester may interfere these types of patients are strictly followed. Although the
with adequate visualization and instrumentation,20 and laparoscopic approach to appendectomy in pregnancy is
these procedures that are technically demanding should associated with a low rate of intraoperative complications
be carried out by experienced laparoscopic surgeons. in all trimesters, the rate of fetal loss following LA is almost
However, there was no significant difference reported in 6%, which is significantly higher than that following open
the rates of intraoperative complications, fetal loss, or appendectomy. Rates of preterm delivery appear to be
preterm delivery between the first and among the 26 equal or slightly better in the LA group. The data available
patients in third trimesters.36,37 at present on LA in pregnancy are derived from case
reports and retrospective case series rather than random-
The overall rate of preterm delivery following LA in preg- ized controlled trials. However, given the surgical exper-
nancy was 2.1% (13/624), which is significantly lower than tise needed to confidently perform laparoscopic proce-
that reported following open appendectomy (OA) (8.1%, dures in pregnant women, a large randomized trial to
346/4193; P⬍0.0001).36 No fetal deaths were recorded address the optimal surgical approach to appendicitis in
among the cases of preterm delivery following LA although pregnancy, though desirable, seems less likely.
other neonatal outcomes are not reported. Data are insuffi-
cient to examine the effect of appendectomy on subsequent
birth weight.36 An increased tendency toward obstetric com- References:
plications following perforated appendicitis in pregnancy 1. Kammerer WS. Nonobstetric surgery during pregnancy. Med
has been previously demonstrated. Rates of fetal loss were Clin North Am. 1979;63:1157–1164.
3.4% (11/324), 12.1% (11/91), and 7.3% (11/150) in simple, 2. Kort B, Katz VL, Watson WJ. The effect of nonobstetric
complicated, and negative appendicitis, respectively.36 Com- operation during pregnancy. Surg Gynecol Obstet. 1993;177:371–
plicated appendicitis was defined as appendicitis with evi- 376.
dence of perforation, appendiceal abscess, or generalized
peritonitis. Fetal loss was statistically more likely following 3. Affleck DG, Handrahan DL, Egger MJ, Price PR. The laparo-
scopic management of appendicitis and cholelithiasis during
LA for complicated appendicitis compared with LA for sim-
pregnancy. Am J Surg. 1999;178:523–529.
ple appendicitis in pregnancy (P⫽0.0027). There was no
statistically significant difference in fetal loss in the simple 4. Moreno-Sanz C, Pascual-Pedreno A, Picazo-Yeste JS, Seo-
appendicitis group compared with those who had a negative ane-Gonzalez JB. Laparoscopic appendectomy during pregnan-
LA (P⫽0.0641).36 cy: between personal experiences and scientific evidence. J Am
Coll Surg. 2007;205(1):37– 42.
The overall rate of interrupted pregnancy (premature deliv-
5. Rollins MD, Chan KJ, Price RR. Laparoscopy for appendicitis
ery and fetal loss) following LA in pregnancy has been
and cholelithiasis during pregnancy: a new standard of care.
reported to be 7.7%, which is significantly less than 11.3% Surg Endosc. 2004;18:237–241.
following OA.36 However McGory et al31 who examined
appendectomy in 3133 pregnant women over an 8-year 6. Halkic N, Tempia-Caliera AA, Ksontini R, Suter M, Delaloye
period in California noted an overall fetal loss rate of 5.6% JF, Vuilleumier H. Laparoscopic management of appendicitis
(35/624) in the LA group, which was significantly higher than and symptomatic cholelithiasis during pregnancy. Langenbecks
Arch Surg. 2006;391:467– 471.
that reported following OA (3.1%, 128/4193; P⫽0.001). The
rate of fetal loss was significantly higher in those women 7. Palanivelu C, Rangarajan M, Parathasarathi R. Laparoscopic
JSLS (2009)13:384 –390 389
Laparoscopic Appendicectomy in all Trimesters of Pregnancy, Machado NO et al.
appendectomy in pregnancy: a case series of 7 patients. JSLS. gynecologic laparoscopy in second and third trimester preg-
2006;10:321–325. nancy: obstetric implications. JSLS. 1998;2(3):235–238.
8. Wu JM, Chen KH, Lin HF, Tseng LM, Tseng SH, Huang SH. 25. Hee P, Viktrup L. The diagnosis of appendicitis during preg-
Laparoscopic appendectomy in pregnancy. J Laparoendosc Adv nancy and maternal and fetal outcome after appendectomy. Int
Surg Tech A. 2005;15(5):447– 450. J Gynecol Obstet. 1999;65:129 –135.
9. Carver TW, Antevil J, Egan JC, Brown CV. Appendectomy 26. Radwan M, Maciolek-Blewniewska G, Malinowski A. Spon-
during early pregnancy: What is the preferred surgical approach? taneous heterotopic pregnancy and acute appendicitis treated by
Am Surg. 2005;71:809 – 812. laparoscopy. Int J Gynaecol Obstet. 2007;96:129.
10. Lyass S, Pikarsky A, Eisenberg VH, Elchalal U, Schenker JG, 27. Rizzo AG. Laparoscopic surgery in pregnancy: long-term
Reissman P. Is laparoscopic appendicectomy safe in pregnant follow-up. J Laparoendosc Adv Surg Tech A. 2003;13(1):11–15.
women? Surg Endosc. 2001;15:377–379.
28. Spirtos NM, Eisenkop SM, Spirtos TW, Poliakin RI, Hibbard
11. de Perrot MD, Jenny A, Morales M, Kohlik M, Morel P. LT. Laparoscopy -a diagnostic aid in cases of suspected appen-
Laparoscopic appendicectomy during pregnancy. Surg Laparosc dicitis. Its use in women of reproductive age. Am J Obstet Gy-
Endosc Percutan Tech. 2000;10(6):368 –371. necol. 1987;156:90 –94.
12. Andreoli M, Servakov M, Meyers P, Mann WJ. Laparoscopic 29. Thomas SJ, Brisson P. Laparoscopic appendectomy and cho-
surgery during pregnancy. J Am Assoc Gynecol Laparosc. 1999; lecystectomy during pregnancy: six case reports. JSLS. 1998;2:
6(2):229 –233. 41– 46.
13. Gurbuz AT, Peetz ME. The acute abdomen in the pregnant 30. Tracey M, Fletcher HS. Appendicitis in pregnancy. Am Surg.
patient. Is there a role for laparoscopy? Surg Endosc. 1997;11: 2000;66:555–559.
98 –102.
31. McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer
14. Amos JD, Schorr SJ, Norman PF, et al. Laparoscopic surgery HM. Negative appendectomy in pregnant women is associated
during pregnancy. Am J Surg. 1996;171:435– 437. with a substantial risk of fetal loss. J Am Coll Surg. 2007;205:
534 –540.
15. Schwartzberg BS, Conyers JA, Moore JA. First trimester of preg-
nancy laparoscopic procedures. Surg Endosc. 1997;11:1216 –1217. 32. Andersson RE, Lambe M. Incidence of appendicitis during
pregnancy. Int J Epidemiol. 2001;30:1281–1285.
16. Posta CG. Laparoscopic surgery in pregnancy: report on two
cases. J Laparoendosc Surg. 1995;5:203–205. 33. Weingold AB. Appendicitis in pregnancy. Clin Obstet Gy-
necol. 1983;26:801– 809.
17. Curet MJ, Allen D, Josloff RK, et al. Laparoscopy during
pregnancy. Arch Surg. 1996;131:546 –550. 34. Cappell MS, Friedel D. Abdominal pain during pregnancy.
Gastroenterol Clin North Am. 2003;32:1–58.
18. Lemaire BM, van Erp WF. Laparoscopic surgery during preg-
nancy. Surg Endosc. 1997;11:15–18. 35. Tamir IL, Bongard FS, Klein SR. Acute appendicitis in the
pregnant patient. Am J Surg. 1990;160:571–575.
19. Schreiber JH. Laparoscopic appendicectomy during preg-
nancy. Surg Endosc. 1990;4:100 –102. 36. Walsh CA, Tang T, Walsh SR. Laparoscopic versus open
appendectomy in pregnancy: a systematic review. Int J Surg.
20. Barnes SL, Shane MD, Schoemann MB, Bernard AC, Bou-
20086:339 –344. Epub 2008 Feb1.
langer BR. Laparoscopic appendectomy after 30 weeks preg-
nancy: report of two cases and description of technique. Am 37. Jackson H, Granger S, Price R, et al. Diagnosis and laparo-
Surg. 2004;70:733–736. scopic treatment of surgical diseases during pregnancy: an evi-
dence based review. Surg Endosc. 2008;22:1917–1927.
21. Curet MJ. Special problems in laparoscopic surgery. Previ-
ous abdominal surgery, obesity and pregnancy. Surg Clin North 38. Society of American Gastrointestinal Endoscopic Surgeons
Am. 2000;80:1093–1110. (SAGES). Guidelines for laparoscopic surgery during pregnancy.
Surg Endosc. 1998;12:189 –190.
22. Buser KB. Laparoscopic surgery in the pregnant patient-one
surgeons experience in a small rural hospital. JSLS. 2002;6(2): 39. Curet MJ, Vogt DA, Schob O, Qualls C, Izquierdo LA, Zucker
121–124. KA. Effects of CO2 pneumoperitoneum in ewes. J Surg Res.
1996;63:339 –344.
23. Friedman JD, Ramsey PS, Ramin KD, Berry C. Pnuemoam-
nion and pregnancy loss after second trimester laparoscopic 40. Pedersen AG, Petersen OB, Wara P, Ronning H, Qvist N,
surgery. Obstet Gynecol. 2002;99:512–513. Laurberg S. Randomized clinical trial of laparoscopic versus
open appendicectomy. Br J Surg. 2001;88:200 –205.
24. Geisler JP, Rose SL, Mernitz CS, Warner JL, Hiett AK. Non-
390 JSLS (2009)13:384 –390
You might also like
- Laparoscopic Versus Open Appendectomy During Pregnancy: Original Research ArticleDocument5 pagesLaparoscopic Versus Open Appendectomy During Pregnancy: Original Research ArticleJason CalvinNo ratings yet
- Laparoscopic Appendectomy During PregnancyDocument4 pagesLaparoscopic Appendectomy During PregnancypsychobillNo ratings yet
- Comparison of Laparoscopy and Laparotomy in The Surgical Management of Ectopic PregnancyDocument5 pagesComparison of Laparoscopy and Laparotomy in The Surgical Management of Ectopic PregnancyFitri Maya AnggrainiNo ratings yet
- Complicated AppendicitisDocument4 pagesComplicated AppendicitisMedardo ApoloNo ratings yet
- Lap vs Open Appendectomy: Which is BetterDocument22 pagesLap vs Open Appendectomy: Which is Betterfahryzal_noteNo ratings yet
- Placenta AccretaDocument5 pagesPlacenta AccretaF3rcitaNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleHazbullah AisyNo ratings yet
- Lateral ColposuspentionDocument24 pagesLateral ColposuspentionMohammad QuayyumNo ratings yet
- Conventional Versus Laparoscopic Surgery For Acute AppendicitisDocument4 pagesConventional Versus Laparoscopic Surgery For Acute AppendicitisAna Luiza MatosNo ratings yet
- Management of AUB in A Bicornuate Uterus - Endometrial Ablation in A CompDocument1 pageManagement of AUB in A Bicornuate Uterus - Endometrial Ablation in A Comptipu42No ratings yet
- Alborzi2014Document5 pagesAlborzi2014dw21541No ratings yet
- TAPP HernioplastyDocument5 pagesTAPP HernioplastyMaryam Alam KhanNo ratings yet
- Ijcem0007 1366Document4 pagesIjcem0007 1366Ratih Kusuma DewiNo ratings yet
- Could Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProceduresDocument9 pagesCould Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProcedurespingusNo ratings yet
- 10 - Vaginal Agenesis - A Systematic ReviewDocument41 pages10 - Vaginal Agenesis - A Systematic ReviewNunuh SulaemanNo ratings yet
- 3 PBDocument6 pages3 PBAulia Rizqi MulyaniNo ratings yet
- Outcome of Total Laparoscopic HysterectomyDocument4 pagesOutcome of Total Laparoscopic HysterectomyDanica SavićNo ratings yet
- Bun V34N3p223Document6 pagesBun V34N3p223pingusNo ratings yet
- Acute Abdomen in PregnancyDocument6 pagesAcute Abdomen in PregnancydkasisNo ratings yet
- Laparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Document5 pagesLaparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Juan Carlos SantamariaNo ratings yet
- Laparoscopic Appendectomy PostoperativeDocument6 pagesLaparoscopic Appendectomy PostoperativeDamal An NasherNo ratings yet
- 10 1016@j Ijscr 2020 01 020Document4 pages10 1016@j Ijscr 2020 01 020ari naNo ratings yet
- Dte 03 121Document5 pagesDte 03 121Buntoro Indra DNo ratings yet
- Success Factors For Bakri Balloon Usage Secondary To Uterine Atony: A Retrospective, Multicentre StudyDocument6 pagesSuccess Factors For Bakri Balloon Usage Secondary To Uterine Atony: A Retrospective, Multicentre StudyMajo MelchiadeNo ratings yet
- Placenta Previa 1Document2 pagesPlacenta Previa 1Gunther MirandaNo ratings yet
- Surgical Treatment of Cesarean Scar Ectopic PregnancyDocument7 pagesSurgical Treatment of Cesarean Scar Ectopic PregnancyIndRa KaBhuomNo ratings yet
- Total Laparoscopic HysterectomyDocument8 pagesTotal Laparoscopic HysterectomySamir CastilloNo ratings yet
- Wind2007 PDFDocument5 pagesWind2007 PDFanatolioNo ratings yet
- Main PDFDocument4 pagesMain PDFhhNo ratings yet
- J of Obstet and Gynaecol - 2022 - Salman - Uterine Preserving Technique in The Treatment of Pelvic Organ ProlapseDocument7 pagesJ of Obstet and Gynaecol - 2022 - Salman - Uterine Preserving Technique in The Treatment of Pelvic Organ ProlapseYo MeNo ratings yet
- Anesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaDocument4 pagesAnesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaHanayuki VizureiNo ratings yet
- RCT Compares Caesarean Section Surgical TechniquesDocument11 pagesRCT Compares Caesarean Section Surgical TechniquesWahab RopekNo ratings yet
- 1 s2.0 S2211419X13000578 MainDocument4 pages1 s2.0 S2211419X13000578 Mainindra040293No ratings yet
- 43 Iajps43052018 PDFDocument6 pages43 Iajps43052018 PDFiajpsNo ratings yet
- Adenomyosis Excision Followed by Successful Live Birth After Three Consecutive IVFDocument5 pagesAdenomyosis Excision Followed by Successful Live Birth After Three Consecutive IVFPyuzz RemakeNo ratings yet
- Therapeutic efficacy of hysterosalpingography with hydrostatic pressureDocument5 pagesTherapeutic efficacy of hysterosalpingography with hydrostatic pressurefishalNo ratings yet
- Intraoperative Complications After Total Laparoscopic Hysterectomy: A Retrospective Study in Training Institute Richa Patel, Arun MorayDocument5 pagesIntraoperative Complications After Total Laparoscopic Hysterectomy: A Retrospective Study in Training Institute Richa Patel, Arun MorayArun MorayNo ratings yet
- PIIS0015028219304844Document2 pagesPIIS0015028219304844nighshift serialsleeperNo ratings yet
- Isj-5899 oDocument5 pagesIsj-5899 oAbhiram MundleNo ratings yet
- Day Case Vaginal Pomeroy Tubectomy A Simplified TechniqueDocument11 pagesDay Case Vaginal Pomeroy Tubectomy A Simplified TechniqueedelinNo ratings yet
- Ojog 2013020415273326Document6 pagesOjog 2013020415273326Achmad Safi'iNo ratings yet
- Pi Is 0020729214001040Document5 pagesPi Is 0020729214001040Nurul AiniNo ratings yet
- Histeroctomy PDFDocument6 pagesHisteroctomy PDFsanta_pangaribuan_1No ratings yet
- Urinary Retention in The Post-Partum PeriodDocument6 pagesUrinary Retention in The Post-Partum PeriodSinggih Nisyah PrasetyoNo ratings yet
- Better Orchiopexy and High Ligation 2016Document4 pagesBetter Orchiopexy and High Ligation 2016Richard QiuNo ratings yet
- Hysterosalpingography 2009Document7 pagesHysterosalpingography 2009Niko MontgomeryNo ratings yet
- Closure Vs Nonclosure of PeritoneumDocument6 pagesClosure Vs Nonclosure of PeritoneumFrancisco Xavier Beltrán Vallejo100% (1)
- 4 Kuratani2008Document5 pages4 Kuratani2008M RidwanNo ratings yet
- En V34n4a04Document7 pagesEn V34n4a04Diego AndradeNo ratings yet
- Ovarian Endometriomas and IVF: A Retrospective Case-Control StudyDocument6 pagesOvarian Endometriomas and IVF: A Retrospective Case-Control Studydr.pravitasari23No ratings yet
- 1 s2.0 S0090825804003610 Main PDFDocument3 pages1 s2.0 S0090825804003610 Main PDFRirin WahyuniNo ratings yet
- 2014 179 0 Successful Treatment of Cervical Incompetence Using A Modified Laparoscopic Cervical Cerclage Technique A Cohort StudyDocument5 pages2014 179 0 Successful Treatment of Cervical Incompetence Using A Modified Laparoscopic Cervical Cerclage Technique A Cohort Studyalifiah nabillaNo ratings yet
- Paper AbdAllah RefaatDocument13 pagesPaper AbdAllah RefaatAbdAllah A. RefaatNo ratings yet
- Use Only: Intracorporeal Hybrid Single Port Conventional Laparoscopic Appendectomy in ChildrenDocument4 pagesUse Only: Intracorporeal Hybrid Single Port Conventional Laparoscopic Appendectomy in ChildrenYelisa PatandiananNo ratings yet
- Trends in Female Sterilization MethodsDocument4 pagesTrends in Female Sterilization MethodsJer KelNo ratings yet
- Laparoscopic Hysterectomy and Decision When and WH PDFDocument5 pagesLaparoscopic Hysterectomy and Decision When and WH PDFDian SiregarNo ratings yet
- Chen 2017Document5 pagesChen 2017Hermus Espiritu MaturranoNo ratings yet
- Esposito 2006Document4 pagesEsposito 2006Fernando GarciaNo ratings yet
- Esophageal Preservation and Replacement in ChildrenFrom EverandEsophageal Preservation and Replacement in ChildrenAshwin PimpalwarNo ratings yet
- CV - Jason CalvinDocument2 pagesCV - Jason CalvinJason CalvinNo ratings yet
- November 2022 duty rosterDocument3 pagesNovember 2022 duty rosterJason CalvinNo ratings yet
- Dapus ReferatDocument3 pagesDapus ReferatJason CalvinNo ratings yet
- International Journal of Surgery: Humphrey G.M. Walker, Ahmad Al Samaraee, Sarah J. Mills, M. Reza KalbassiDocument7 pagesInternational Journal of Surgery: Humphrey G.M. Walker, Ahmad Al Samaraee, Sarah J. Mills, M. Reza KalbassiJason CalvinNo ratings yet
- GI BleedDocument48 pagesGI BleedJason CalvinNo ratings yet
- Smoking Cessation Eustella 00000000167Document18 pagesSmoking Cessation Eustella 00000000167Jason CalvinNo ratings yet
- Clinical Skill - Advance History TakingDocument20 pagesClinical Skill - Advance History TakingJason CalvinNo ratings yet
- Soap KasusDocument81 pagesSoap KasusJason CalvinNo ratings yet
- Acute Transverse Myelitis: Elinore Kaufman MS IIIDocument27 pagesAcute Transverse Myelitis: Elinore Kaufman MS IIIParag DashatwarNo ratings yet
- Spare Order 28.03Document27 pagesSpare Order 28.03Ankit AgarwalNo ratings yet
- Biochemistry of InflamationDocument45 pagesBiochemistry of Inflamationmichot feleguNo ratings yet
- Cognitive Neuroscience of MusicDocument13 pagesCognitive Neuroscience of MusicMitkoNo ratings yet
- O & M of DC & UPS SystemsDocument65 pagesO & M of DC & UPS SystemshajimakNo ratings yet
- The Irrefutable Laws of Leadership SummaryDocument6 pagesThe Irrefutable Laws of Leadership Summarycoachersland100% (3)
- Professional EthicsDocument2 pagesProfessional EthicsKoushik MeduriNo ratings yet
- Introduction to Machine LearningDocument30 pagesIntroduction to Machine LearningHafisIzranNo ratings yet
- Assignment Article 2Document14 pagesAssignment Article 2Trend on Time0% (1)
- Carte Tehnica Panou Solar Cu Celule Monocristaline SunPower 345 WDocument4 pagesCarte Tehnica Panou Solar Cu Celule Monocristaline SunPower 345 WphatdoggNo ratings yet
- GEC 107 - Art Appreciation Research Worksheet On Identifying ArtDocument4 pagesGEC 107 - Art Appreciation Research Worksheet On Identifying ArtJustine SicanNo ratings yet
- UConn Criminal Information SummaryDocument2 pagesUConn Criminal Information SummaryEllyn SantiagoNo ratings yet
- HRM - Final Project PresentationDocument9 pagesHRM - Final Project PresentationJeenifer SteavenNo ratings yet
- Youth Stroke Education: 60min & 40min Lesson PlansDocument18 pagesYouth Stroke Education: 60min & 40min Lesson PlansShrishail ShreeNo ratings yet
- US vs. HernandezDocument7 pagesUS vs. HernandezJnhNo ratings yet
- Classwork Natural Selection WorksheetDocument2 pagesClasswork Natural Selection WorksheetGarnetNo ratings yet
- The Beginners Bible Coloring Book by JPR504Document37 pagesThe Beginners Bible Coloring Book by JPR504Ernesto Carmona Parra100% (1)
- ACT1110: Governance, Ethics, Risk and ControlDocument21 pagesACT1110: Governance, Ethics, Risk and ControlDong WestNo ratings yet
- Thesis Jur ErbrinkDocument245 pagesThesis Jur Erbrinkgmb09140No ratings yet
- Sourcing Rules in PurchasingDocument21 pagesSourcing Rules in Purchasingpradhan.neeladriNo ratings yet
- On The Metres of Poetry and Related Matters According To AristotleDocument61 pagesOn The Metres of Poetry and Related Matters According To AristotleBart MazzettiNo ratings yet
- 1 11857 AnatomyDocument5 pages1 11857 Anatomykalyan2k5No ratings yet
- Indosat AR10 ENGDocument564 pagesIndosat AR10 ENGHerry Abu DanishNo ratings yet
- The Multi-Objective Decision Making Methods Based On MULTIMOORA and MOOSRA For The Laptop Selection ProblemDocument9 pagesThe Multi-Objective Decision Making Methods Based On MULTIMOORA and MOOSRA For The Laptop Selection ProblemAnkushNo ratings yet
- SafeNet Ikey4000 PB (En) WebDocument2 pagesSafeNet Ikey4000 PB (En) WebbasharaccountNo ratings yet
- BS NursingDocument5 pagesBS NursingDenise Louise PoNo ratings yet
- Đề Thi và Đáp ÁnDocument19 pagesĐề Thi và Đáp ÁnTruong Quoc TaiNo ratings yet
- AtropineDocument6 pagesAtropineNiluh Komang Putri PurnamantiNo ratings yet
- ChatGpt For AccountantsDocument29 pagesChatGpt For Accountantssamreen khanNo ratings yet
- Sources of Strength For Mental Wellness by Sheryl Boswell, Youth Mental Health Canada (YMHC)Document11 pagesSources of Strength For Mental Wellness by Sheryl Boswell, Youth Mental Health Canada (YMHC)Youth Mental Health CanadaNo ratings yet
- Organisational BehaviourDocument6 pagesOrganisational BehaviourShivam Shreshtha100% (1)