Professional Documents
Culture Documents
Surgical Treatment of Non-Embolized Patients With Nasoangiofibroma
Uploaded by
arief ardaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Surgical Treatment of Non-Embolized Patients With Nasoangiofibroma
Uploaded by
arief ardaCopyright:
Available Formats
Rev Bras Otorrinolaringol
2008;74(4):583-7. original article
Surgical Treatment of Non-
embolized Patients with
Nasoangiofibroma
Adriano Santana Fonseca1, Eriko Vinhaes2, Viviane
Boaventura3, Nilvano Alves de Andrade4, Lislane Keywords: treatment, embolization, juvenile nasopharyngeal
angiofibroma, skull base.
Andrade Dias5, Vyrna Medeiros6, Fernando
Coifman7
Summary
J uvenile nasopharyngeal angiofibroma (JNA) is an
uncommon tumor of the sphenopalatine foramen. Surgery
combined with preoperative embolization has been the
treatment of choice for JNA patients without intracranial
invasion. This study aims to assess the viability of surgically
treating non-embolized patients with JNA (types I-III according
to Fisch). Materials And Method: This is a retrospective,
descriptive study based on the medical records of 15 patients
with histologically confirmed JNA (Fisch’s types I- III), who
underwent surgical treatment without pre-op embolization
in our institution between 2000 and 2005. Results: Seven of
the fifteen patients were approached endoscopically, four
through the transantral approach, three were treated with the
combined transmaxillary and endoscopic approach, and one
with the combined transmaxillary and transpalatal approach.
Six patients required intraoperatory blood transfusion,
averaging volumes of 1.3 unit/patient. There were no cases
of death or significant morbidity. Eleven of the fifteen patients
were followed for an average of twelve months and 27% of
them relapsed. Four patients did not comply with the follow-
up scheme. Conclusion: Resection of JNF types I-III was
safely completed in non-embolized patients. The observed
levels of intraoperative bleeding, occurrence of complications,
and rates of recurrence were close to those seen in embolized
patients as found in the literature.
1
Specialist in ENT and head and neck surgery by the HC/ UNICAMP. Specialist in Forensic Medicine at SSP/BA, Adjunct Professor of head and neck surgery at Santa
Casa de Misericórdia da Bahia - Hospital Santa Izabel. Specialist in swallowing disorders and head and neck surgery at the Núcleo de Otorrinolaringologia e Estudos da
Voz/Hospital da Bahia /Hospital Português.
2
Specialist in ENT, otorhinolaryngologist, Adjunct Professor of rhinology at the ENT Department of the Santa Casa de Misericórdia da Bahia, Hospital Santa Izabel.
3
MSc in pathology at FIOCRUZ/ UFBA, PhD student at FIOCRUZ UFBA, Adjunct Professor of ENT at Santa Casa de Misericórdia da Bahia, Hospital Santa Izabel.
4
PhD in ENT at USP, Head of the ENT and Head and Neck Department at Santa Casa de Misericórdia da Bahia, Hospital Santa Izabel.
5
MD, Resident at the ENT and Head and Neck Surgery Department at Santa Casa de Misericórdia da Bahia, Hospital Santa Izabel.
6
MD, Resident at the ENT and Head and Neck Surgery Department at Santa Casa de Misericórdia da Bahia, Hospital Santa Izabel.
7
MD, Resident at the ENT and Head and Neck Surgery Department at Santa Casa de Misericórdia da Bahia, Hospital Santa Izabel.
Santa Casa de Misericórdia da Bahia, Hospital Santa Izabel.
Send correspondence to: Adriano Santana Fonseca - Unidade de Otorrinolaringologia e Cirurgia Cérvico-Facial do Hospital Santa Izabel. Praça Almeida Couto 500
Nazaré Salvador BA 40050-410.
This paper was submitted to the RBORL-SGP (Publishing Manager System) on 5 April 2007. Code 4411.
The article was accepted on 12 September 2007.
Brazilian Journal of Otorhinolaryngology 74 (4) July/August 2008
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
583
INTRODUCTION Patients with previous history of JNA surgery were
excluded. This study was approved by the Hospital Ethics
Juvenile nasopharyngeal angiofibroma (JNA) is an and Research Committee under permit FR - 67401 and
uncommon tumor that develops almost exclusively in CAAE (CAAE - 0022.0.057.000-05).
young men. It accounts for 0.05% of all head and neck Fentanyl (3Mcg/Kg), propofol (2.5mg/Kg), cisa-
tumors1,2. Although it is considered a benign neoplasm, this tracurium (0.15mg/Kg) were used in general anesthesia
tumor is not encapsulated, may lead to local destruction and dexamethasone (10mg) in anesthetic induction; and
and has high relapse rates1. This vascular tumor emerges sevoflurane (2%) with remifentanil (0.2 to 0.5mg/Kg/min)
mainly from the sphenopalatine foramen and may extend in sustaining anesthesia. Blood pressure was kept at an
all the way to the middle cranial fossa3,4. average 60mmHg intraoperatively, and tranexamic acid
According to the scheme proposed by Fisch5, these (10mg/Kg) was administered as a prophylactic measure
tumors may be contained within the nasal cavity and against bleeding. Volemic replacement was done with
nasopharynx (I), invade the face sinuses or the pterygopa- crystalloids and blood transfusion was indicated whenever
latine fossa (II), expand towards the infratemporal fossa, hemoglobin was under 7g/dl.
orbit, and parasellar region (III) or present intracranial When approaching patients endonasally, the surge-
invasion (IV). on used 0, 30 and 45 degree endoscopes (Comeg, Storz),
Surgery is considered to be the best treatment nasal vasoconstriction with cotton swabs drenched in
option for JNA6 and many are the isolated and combined lidocaine and adrenalin solution (1:3000), and irrigation
procedures and approaches to resect the tumor, such as with saline solution at 0.9% and 4ºC. Patients were then
the endoscopic, transmaxillary and transpalatine7. Intra- submitted to a partial medial turbinectomy to expose the
operative bleeding may occur in any of the approaches sphenoethmoidal recess and the sphenopalatine foramen
and has been one of the main perioperative complications. region, defining the superior border of the tumor in the
Preoperative arterial embolization has been used syste- cases where it involved the tail or body of the concha.
matically to reduce the amount of bleeding and the use Sphenoidal sinusotomy was done via the sphenoethmoi-
of blood byproducts during surgery with good results4,7. dal recess and ethmoidectomy with inferior and posterior
However, there is no consensus as to the routine use of traction of the tumor when the neoplasm involved the
preoperative embolization, given its high cost and incon- posterior-superior portion of the nasal fossa. Maxillary
sistent availability of the procedure in care centers. antrostomy, with detachment of the posterior fontanel
This paper aims to assess the possibilities of sur- to expose the sphenopalatine foramen, was indicated to
gically treating patients for JNA without preoperative determine the lateral borders of the tumor, in the pterygo-
embolization looking at surgery time, volume of red cell palatine fossa or the infratemporal fossa. The tumor’s
packs, intra and postoperative complications, and tumor arterial pedicles (mainly the often numerous terminal
relapse rates. branches of the internal maxillary artery) that surround it
inferiorly and superiorly were dissected and ligated with
MATERIALS AND METHOD a monopolar electrocautery. A bipolar cautery was used
in the vessels close to the meninges and the optic nerve,
This descriptive, retrospective study used data from
whereas neurosurgery 200 clips were placed in the larger
the medical records of fifteen patients who underwent
diameter vessels.
JNA resection surgery without preoperative tumor embo-
In type-I patients, after vascular ligation, the tumor
lization between 2000 and 2005. All patients underwent
was pulled towards the rhinopharynx until it was complete-
nasofibroscopy with a flexible 3.2mm Machida scope and
ly detached. In type II and III patients, part of the palatine
had sinus CT images taken.
bone vertical lamina and of the maxillary sinus posterior
Diagnostic criteria comprehended history of epis-
wall were removed endoscopically, thus exposing the
taxis and/or nasal obstruction, presence of angiomatous
pterygopalatine fossa and part of the infratemporal fossa.
tumor under endoscopy, and CT image showing expansive
The transeptal approach as described by Wormald8 was
formations in the nasal cavity with or without invasion into
preferred in patients operated on more recently. Vascular
the sinuses, rhinopharynx, pterygomaxillary fossa, infra-
ligation was conducted after the lateral borders of the
temporal fossa, orbit, and intracranial area, after contrast
tumor were identified as described above. The tumor was
uptake. Tumors were rated based on the criteria developed
then detached up to its posterior borders, in the inferior
by Fisch. Clinical diagnosis was confirmed postoperatively
orbital fissure and the venous pterygoid plexus.
through histology exams done on the surgical specimens.
When the lateral border could not be reached en-
All patients were operated on by the same surgeon.
doscopically, the transmaxillary approach was used in a
None of the patients received adjuvant treatment
medial labial rhinotomy or in a facial medial degloving
such as hormone therapy, chemotherapy, or radiotherapy
procedure, as described by Denker and Caldwell-Luc
perioperatively.
Brazilian Journal of Otorhinolaryngology 74 (4) July/August 2008
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
584
respectively. The transpalatine approach with microsco- three groups of patients. Surgery took slightly longer for
pe assisted dissection combined with the transmaxillary type II tumors, but no statistically significant difference
approach was used in one case where a bulky tumor was was found between the three groups. Average surgery
adhered posteriorly. length was 140 minutes. Six of the fifteen patients had
Isolated transmaxillary approach was used in tumors intraoperative bleeding requiring blood transfusion. They
invading the entire nasal fossa, regardless of type, that ren- averaged 1.3 units of red cell pack per patient.
dered impossible the use of the endoscopic approach. Three patients had postoperative bleeding, two from
All patients stayed in intensive care units for 24-48 group II and one from group III. Bleeding episodes were
hours after surgery. controlled by ligating the maxillary artery. All patients were
Nasal packing, when required, was removed after discharged without requiring nasal packing. There were
48-72 hours. Nasal irrigation with hypertonic saline solution no postoperative complications.
was indicated after hospital discharge and follow-up was All fifteen patients who underwent surgery were
conducted for nasofibroscopy exams at the institution’s followed up for 12-63 months.
outpatient ward. Endoscopic CT face scans were taken Three of the patients (27%) had relapsing tumors
whenever relapsing tumors were suspected. and were referred to tumor resection. None had relapsing
tumors after the second procedure.
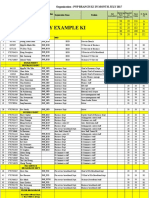
RESULTS The data above is described on the chart below.
All fifteen patients operated for JNA resection wi- DISCUSSION
thout embolization were staged based on the model pro-
posed by Fisch. Eight patients (53%) had type II disease, Some authors believe embolization is indispen-
followed by four (27%) with type III, and three (20%) with sable when resecting nasopharyngeal angiofibromas
type I tumors. None of the patients had type IV disease. endoscopically8,9. Most papers in the literature comparing
The endonasal and transmaxillary approaches were elected surgical treatment with and without embolization have
for patients with disease types I and II. Combined transma- demonstrated reduced intraoperative blood loss and fewer
xillary and endonasal or transmaxillary and transpalatine blood transfusions when embolization is done10,12. Blood
approaches were reserved for type III tumors. loss is reduced by 836 to 1200 ml per non-embolized pa-
Age averaged between 17 and 19 years within the tient; and by 400 to 600 ml per embolized patient10-26.
Chart
Follow-
Stage Intraop Blood Surgery
Patient # Age (years) Approach Postop Bleeding Relapse up (mon-
(Fisch) Transfusion Duration
ths)
1 24 Endonasal Not 02:40 Not Not 46
I 2 15 Transmaxillary 1 unit 02:10 Not Not 45
3 19 Endonasal Not 02:20 Not Not 42
4 15 Endonasal Not 02:20 Not Not 12
5 24 Endonasal 6 units 02:50 Not Not 48
6 19 Endonasal 3 units 03:20 Yes Yes 63
7 19 Transmaxillary 2 units 03:25 Yes Not 58
II
8 12 Transmaxillary Not 02:00 Not Not 47
9 16 Transmaxillary Not 02:45 Not Not 23
10 24 Endonasal 5 units 03:20 Not Not 24
11 24 Endonasal Not 02:40 Not Not 12
Endonasal +
12 16 3 units 02:05 Not Yes 22
Transmaxillary
Transmaxillary +
13 24 Not 03:10 Yes Yes 29
Transpalatine
III
Endonasal +
14 23 Not 02:45 Not Not 25
Transmaxillary
Endonasal +
15 08 Not 01:30 Not Not 36
transmaxilar
Brazilian Journal of Otorhinolaryngology 74 (4) July/August 2008
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
585
In terms of blood transfusion, the values ranged CONCLUSION
between 3 and 4.4 units of red cell pack per patient in the
non-embolized group, when compared to 0 to 2 units in This study presents a review of fifteen JNA patients
the group of embolized patients11-26. who underwent surgery without preoperative embolization
This study comprehended patients with disease within a five-year span. Intraoperative and postoperative
types I to III according to Fisch. Intraoperative blood complication rates and blood loss levels were similar to
transfusion volumes were comparable to those found by those found in the literature for patients submitted to pre-
other authors looking at preoperative embolization - 0 to operative embolization, thus indicating that the procedure
2 units per patient11-26 against 1.3 units per patient in this without preoperative embolization can be safely offered to
study. Bleeding was reduced as a result of the adopted selected patients. Additional comparative studies must be
surgical tactic, which included systematic tumor vascular conducted so that a treatment routine can be developed
ligation in the beginning of the procedure, approaching for these patients.
not only the maxillary artery branch, but also all other
arterial branches irrigating the neoplasm. By maintaining REFERENCES
the patients’ blood pressure at a lower level (60mmHg) 1. Pryor S, Moore E, Kasperbauer J. Endoscopic versus Traditional
until the tumor has been removed and tranexamic acid Approaches for Excision of Juvenile Nasopharyngeal Angiofibroma.
applied, it is believed that intraoperative bleeding was Laryngoscope 2005;115:1201-7.
significantly reduced. 2. Brieger J, Wierzbicka M, Sokolov M, Roth Y, Szyfter W, Mann WJ.
Vessel Density, Proliferation, and Immuno localization of Vascular
Moulin et al. do not indicate embolization as a Endothelial Growth Factor in Juvenile Nasopharyngeal Angiofibromas.
routine preoperative procedure. Considering the blood Arch Otolaryngol Head Neck Surg 2004;130:727-31.
losses of embolized and non-embolized patients, the 3. Onerci TM, Yucel OT, Ogretmenoglu O. Endoscopic surgery in
authors concluded that the procedure should only be treatment of juvenile nasopharyngeal angiobroma. Int J Ped Otorhi-
nolaryngol 2003;67:1219-25.
offered to patients with larger tumors12. Petruson et al., 4. Hosseini SM, Borghei P, Borghei SH, Ashtiani MT, Shirkhoda A. An-
looking at intraoperative bleeding, did not encounter sta- giofibroma: an outcome review of conventional surgical approaches.
tistically significant differences between embolized and Eur Arch Otorhinolaryngol 2005;262:807-12.
non-embolized patients13. The authors found higher JNA 5. Fisch U. The infratemporal fossa approach for nasopharyngeal tumors.
Laryngoscope 1983;93:36-44.
relapse rates among embolized patients. Mc Combe et al. 6. Tseng HZ, Chao WY. Transnasal endoscopic approach for juvenile
suggested that preoperative embolization may compromise nasopharyngeal angiofibroma. Am J Otolaryngol 1997;18:151-4.
the identification of surgical margins as it reduces tumor 7. Gruber B, Kron TK, Goldman ME. Nasopharyngeal angiofibroma
size, consequently increasing chances of relapse14. in two young children. Case reports. Otolaryngol Head Neck Surg
1985;93:803-6.
Many papers also point out the benefits of preope- 8. Wormald PJ. Endoscopic medial maxillectomy for maxillary and
rative arterial embolization in controlling intraoperative pterygopalatine fossa tumors. In: Wormald PJ, editor: Endoscopic
bleeding8,9,15,17, reducing it by as much as fifty percent15, Sinus Surgery: anatomy, three dimensional reconstruction, and sur-
thus allowing the full excision of the tumor16, lower relap- gical technique, 1st ed. New York: Thieme; 2005. p. 125-34.
9. Nicolai P, Berlucchi M, Tomenzoli D, Cappiello J, Trimarchi
se rates and neurological complications9,17, and reduced M, Maroldi R, Battaglia G, Antonelli AR. Endoscopic surgery
surgery duration when associated with the endoscopic for juvenile angiofibroma: when and how. Laryngoscope 2003;
approach alone18. Nevertheless, the most important prog- 113(5):775-82.
nostic factor for relapse is early staging and knowing the 10. Li JR, Qian J, Shah XZ, et al: Evaluation of the effectiveness of preo-
perative embolization in surgery for nasopharyngeal angiofibroma.
extension of the tumor19. Eur Arch Otorhinolaryngol 1998;255:430-2.
Maxillary artery embolization is a relatively safe 11. Siniluoto TM, Luotonen JP, Tikkakoski TA, et al: Value of preoperative
invasive procedure. Complication rates may be as high embolization in surgery for nasopharyngeal angiofibroma. J Laryngol
as 27%20, most of which are temporary21 in spite of the Otol 1993;107:514-21.
12. Moulin G, Chagnaud C, Gras R, Gueguen E, Dessi P, Gaubert JY,
few (2%) severe ones22. Such complications may include Bartoly JM, Zanaret M, Botti G, Cannoni M. Juvenile nasopharyngeal
occlusion of the central retinal artery and consequent tem- angiofibroma: comparison of blood loss during removal in embolized
porary blindness23, oronasal fistula due to tissue necrosis24, group versus nonembolized group. Cardiovasc Intervent Radiol 1995
occlusion of the middle cerebral artery followed by stroke, May,Jun;18(3):158-61.
13. Petruson K, Rodriguez Catarino M, Petrusin B, Finizia C. Juvenile
and occlusion of the ophthalmic artery25. nasopharyngeal angiofibroma: long-term results in preoperative
Preoperative embolization may cost between USD embolized and nonembolized patients. Acta Otolaryngol 2002
2,000 and USD 11,00020,21,27, being therefore a procedure Jan;122(1):96-100.
that most public and non-profit hospitals in Brazil cannot 1. McCombe A, Lund VJ, Howard DJ. Recurrence in juvenile angiofibroma.
Rhinology 1990;28:97-102.
afford. We could not find indexed papers discussing the 14. Pletcher JD, Newton TH, Dedo HH, Norman D. Preoperative em-
costs of this procedure in Brazil. bolization of juvenile angiofibromas of the nasopharynx. Ann Otol
Rhinol Laryngol 1975 Nov/Dec;84(6):740-6.
Brazilian Journal of Otorhinolaryngology 74 (4) July/August 2008
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
586
15. Katsiotis P, Tzortzis G, Karaminis C. Transcatheter arterial em- 21. Tseng EY, Narducci CA, Willing SJ, Sillers MJ. Angiographic em-
bolization in nasopharyngeal angiofibroma. Acta Radiol Diagn bolization for epistaxis: a review of 114 cases. Laryngoscope 1998
(Stockh)1979;20(3):433-8. Apr;108(4 Pt 1):61-9.
16. Wilms G, Peene P, Baert AL, Dewit A, Ostyn F, Plets C. Preoperative 22. Onerci M, Gumus K, Cil B, Eldem B. A rare complication of em-
embolization of juvenile nasopharyngeal angiofibromas. J Belge bolization in juvenile nasopharyngeal angiofibroma. Int J Pediatr
Radiol 1989 Dec;72(6):465-70. Otorhinolaryngol 2005 Mar;69(3):423-8.
17. Roger G, Tran Ba Huy P, Froehlich P, Van Den Abbeele T, Klossek 23. Gay I, Elidan J, Gordon R. Oronasal fistula a possible complication
JM, Serrano E, Garabedian EM, Herman P. Exclusively endoscopic of preoperative embolization in the management of juvenile naso-
removal of juvenile nasopharyngeal angiofibroma: trends and limits. pharyngeal angiofibroma. J Laryngol Otol 1983 Jul;97(7):651-6.
Arch Otolaryngol Head Neck Surg 2002 Aug;128(8):928-35. 24. Casasco A, Houdart E, Biondi A, Jhaveri HS, Herbreteau D, Aymard
18. Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT. Angiofibroma. A, Merland JJ. Major complications of percutaneous embolization of
Changes in staging and treatment. Arch Otolaryngol Head Neck Surg skullbase tumors. Am J Neuroradiol 1999 Jan;20(1):179-81.
1996 Feb;122(2):122-9. 25. Glad H, Vainer B, Buchwald C, Petersen BL, Theilgaard SA, Bonvin
19. Strong EB, Bell DA, Johnson LP, Jacobs JM. Intractable epistaxis: P, Lajer C, Jakobsen J. Juvenile nasopharyngeal angiofibromas in
transantral ligation vs. embolization efficacy review and cost analysis. Denmark 1981-2003: diagnosis, incidence, and treatment. Acta Oto-
Otolaryngol Head Neck Surg 1995;113(6):674-8. laryngol 2007 Mar;127(3):292-9.
20. Garcia Cervigon E, Bien S, Rufenacht D, Thurel C, Reizine D, Tran 26. Christensen NP, Smith DS, Barnwell SL, Wax MK. Arterial embolization
Ba Huy P, Merland JJ. Preoperative embolization of nasopharyngeal in the management of posterior epistaxis. Otolaryngol Head Neck
angiofibromas. Report of 58 cases. Neuroradiology 1988;30(6):556- Surg 2005 Nov;133(5):748-53.
60.
Brazilian Journal of Otorhinolaryngology 74 (4) July/August 2008
http://www.rborl.org.br / e-mail: revista@aborlccf.org.br
587
You might also like
- Applied Peritoneal Dialysis: Improving Patient OutcomesFrom EverandApplied Peritoneal Dialysis: Improving Patient OutcomesAnjay RastogiNo ratings yet
- Anorectal Malformation With Long Perineal Fistula: One of A Special TypeDocument6 pagesAnorectal Malformation With Long Perineal Fistula: One of A Special Typepunzell eonnieNo ratings yet
- Intracranial Aneurysms in Childhood - 27 - Year Sigle Institution ExperienceDocument10 pagesIntracranial Aneurysms in Childhood - 27 - Year Sigle Institution ExperienceRony EvangelistaNo ratings yet
- 2013 - BoghaniDocument11 pages2013 - Boghanialejandra gonzalezNo ratings yet
- JurnalDocument5 pagesJurnalFuchsia ZeinNo ratings yet
- Incidence of Developing Contralateral M Enie're's Disease in Patients Undergoing Transmastoid Labyrinthectomy For Unilateral M Enie're's DiseaseDocument4 pagesIncidence of Developing Contralateral M Enie're's Disease in Patients Undergoing Transmastoid Labyrinthectomy For Unilateral M Enie're's DiseaseNoviTrianaNo ratings yet
- Pediatric Inguinal Hernia PDFDocument5 pagesPediatric Inguinal Hernia PDFade-djufrieNo ratings yet
- Intracranial Aneurysms in Childhood: 27-Year Single-Institution ExperienceDocument10 pagesIntracranial Aneurysms in Childhood: 27-Year Single-Institution Experiencezrated786No ratings yet
- Wright 2011Document3 pagesWright 2011diana.miron.mNo ratings yet
- Comparative Study of Laparoscopic Congenital Inguinal Hernia Repair VS Open Congenital Inguinal Hernia Repair PDFDocument3 pagesComparative Study of Laparoscopic Congenital Inguinal Hernia Repair VS Open Congenital Inguinal Hernia Repair PDFrhmathidayatNo ratings yet
- Original Research PaperDocument2 pagesOriginal Research Paperيحيى الجبليNo ratings yet
- Pi Is 0022346814003935Document5 pagesPi Is 0022346814003935wibizzzNo ratings yet
- Endoscopic Polipectomy With Middle Meatal Antrostomy For Antrochoanal Polyp TreatmentDocument4 pagesEndoscopic Polipectomy With Middle Meatal Antrostomy For Antrochoanal Polyp TreatmentCut Nanda FitriNo ratings yet
- En V34n4a04Document7 pagesEn V34n4a04Diego AndradeNo ratings yet
- Fistula in AnoDocument5 pagesFistula in AnoIoannis ValioulisNo ratings yet
- Lumbar Laminectomy TIVA With Propofol Versus InhalDocument6 pagesLumbar Laminectomy TIVA With Propofol Versus InhalDhannyNo ratings yet
- Treatment of Basicervical Femoral Neck Fractures With Proximal Femoral Nail AntirotationDocument11 pagesTreatment of Basicervical Femoral Neck Fractures With Proximal Femoral Nail AntirotationOrto MespNo ratings yet
- Possible Involvement of Hyperactive Internal Anal Sphincter in Adult MegacolonDocument4 pagesPossible Involvement of Hyperactive Internal Anal Sphincter in Adult MegacolonHans Steven KurniawanNo ratings yet
- Abdomen: International Abstracts of Pediatric Surgery 593Document1 pageAbdomen: International Abstracts of Pediatric Surgery 593Yohanes WilliamNo ratings yet
- Topical Steroids in Rhinosinusitis and Intraoperative Bleeding: More Harm Than Good?Document7 pagesTopical Steroids in Rhinosinusitis and Intraoperative Bleeding: More Harm Than Good?lala poNo ratings yet
- 20waqar PDFDocument4 pages20waqar PDFMelisa ClaireNo ratings yet
- Nonsurgical Treatment of Appendiceal Abscess or Phlegmon: A Systematic Review and Meta-AnalysisDocument8 pagesNonsurgical Treatment of Appendiceal Abscess or Phlegmon: A Systematic Review and Meta-AnalysisOscar VillacresNo ratings yet
- Recurrent Ureteropelvic Junction Obstruction Following Primary Treatment: Prevalence, Associated Factors, and Laparoscopic TreatmentDocument9 pagesRecurrent Ureteropelvic Junction Obstruction Following Primary Treatment: Prevalence, Associated Factors, and Laparoscopic TreatmentPatricio G.No ratings yet
- Main PDFDocument6 pagesMain PDFEdison HernandezNo ratings yet
- 631-Article Text-2378-1-10-20180830Document6 pages631-Article Text-2378-1-10-20180830azizhamoudNo ratings yet
- Journal of Pediatric SurgeryDocument4 pagesJournal of Pediatric SurgeryAde Triansyah EmsilNo ratings yet
- Incisional HerniaDocument4 pagesIncisional HerniaRini YolandaNo ratings yet
- 1 s2.0 S1079210401433336 MainDocument4 pages1 s2.0 S1079210401433336 Mainوليد محمد ابوعليNo ratings yet
- Characteristics and Outcome of Patients With Ganglioneuroblastoma, Nodular Subtype: A Report From The INRG ProjectDocument7 pagesCharacteristics and Outcome of Patients With Ganglioneuroblastoma, Nodular Subtype: A Report From The INRG ProjectWahyudhy SajaNo ratings yet
- Superior Laryngeal Nerve Neuralgia: Case Series and Review of Anterior Neck Pain SyndromesDocument4 pagesSuperior Laryngeal Nerve Neuralgia: Case Series and Review of Anterior Neck Pain SyndromesjtbattaNo ratings yet
- Neck Abcess in ChildrenDocument6 pagesNeck Abcess in ChildrenNandaNo ratings yet
- Tabrizi An 2009Document4 pagesTabrizi An 2009Dung Tran HoangNo ratings yet
- Anestesia Regional en PediatriaDocument10 pagesAnestesia Regional en PediatriaAnnie MCHNo ratings yet
- Journal PeatriaDocument4 pagesJournal PeatriaDavidArChambaNo ratings yet
- Histological Analysis of Tonsillectomy and Adenoidectomy Specimens - January 2001 To May 2003Document5 pagesHistological Analysis of Tonsillectomy and Adenoidectomy Specimens - January 2001 To May 2003holly theressaNo ratings yet
- Bjorl: Surgical Treatment of Severe Laryngomalacia: A Retrospective Study of 11 CasesDocument5 pagesBjorl: Surgical Treatment of Severe Laryngomalacia: A Retrospective Study of 11 CasesPutri HakimNo ratings yet
- Avaliação Ultra-Sonográfica Das Técnicas de Punção Da Veia Jugular Interna em CriançasDocument4 pagesAvaliação Ultra-Sonográfica Das Técnicas de Punção Da Veia Jugular Interna em CriançasJing CruzNo ratings yet
- Amedee 2001Document7 pagesAmedee 2001Hakim naufaldiNo ratings yet
- Endovascular Treatment of Intracranial Aneurysms: Initial Experience in A Low-Volume CenterDocument5 pagesEndovascular Treatment of Intracranial Aneurysms: Initial Experience in A Low-Volume CenterAswin ChristantoNo ratings yet
- Laparoscopic Versus Open Inguinal Hernia Repair in Children 3: A Randomized Controlled TrialDocument10 pagesLaparoscopic Versus Open Inguinal Hernia Repair in Children 3: A Randomized Controlled TrialRhandy SeptiantoNo ratings yet
- Lazaroni 16Document4 pagesLazaroni 16adiNo ratings yet
- LIS Open Vs ClosedDocument6 pagesLIS Open Vs CloseddoctortareqNo ratings yet
- Long-Term Outcome After Thrombolysis For Acute Lower Limb IschaemiaDocument9 pagesLong-Term Outcome After Thrombolysis For Acute Lower Limb IschaemiaIdham Adyasa Manggala PutraNo ratings yet
- Tto VasoespasmoDocument6 pagesTto VasoespasmoHernando CastrillónNo ratings yet
- 1 s2.0 S2214751921001584 MainDocument7 pages1 s2.0 S2214751921001584 MainfitriNo ratings yet
- Grand Case Presentation EntryDocument51 pagesGrand Case Presentation EntryDon'tAsK TheStupidOnesNo ratings yet
- Juvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyDocument3 pagesJuvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyGiiszs AlvarezNo ratings yet
- Berkhemer PDFDocument158 pagesBerkhemer PDFFariz Eka SetiawanNo ratings yet
- Endoscopic Treatment of Choanal Atresia and Use of Balloon Dilation: Our ExperienceDocument6 pagesEndoscopic Treatment of Choanal Atresia and Use of Balloon Dilation: Our Experiencefarah maulida martaNo ratings yet
- Chichom2013 PDFDocument5 pagesChichom2013 PDFMuhaimin EfendiNo ratings yet
- Early Use of TIPS in Cirrhosis and Variceal BleedingDocument10 pagesEarly Use of TIPS in Cirrhosis and Variceal Bleedingray liNo ratings yet
- A Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesDocument4 pagesA Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesSake Cinema21No ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofAram Dumnoen-ngamNo ratings yet
- Juvenile Nasopharyngeal Angiofibroma With Intracranial Extension - A Review of 29 CasesDocument6 pagesJuvenile Nasopharyngeal Angiofibroma With Intracranial Extension - A Review of 29 CasesSatya WangsaNo ratings yet
- Safety and Outcomes of Preoperative Embolization of Intracranial Hemangioblastomas A Systematic ReviewDocument9 pagesSafety and Outcomes of Preoperative Embolization of Intracranial Hemangioblastomas A Systematic ReviewDavid Camilo GomezNo ratings yet
- Nejmoa 1010650Document10 pagesNejmoa 1010650Luis socrates Quispe toledoNo ratings yet
- 12-Article Text-77-1-10-20201031Document8 pages12-Article Text-77-1-10-20201031genesis loayzaNo ratings yet
- International Journal of Surgery Open: Sedigheh Nadri, Arash Karimi, Farzad Mohammadi, Hormoz MahmoudvandDocument7 pagesInternational Journal of Surgery Open: Sedigheh Nadri, Arash Karimi, Farzad Mohammadi, Hormoz MahmoudvandLuis ReynaNo ratings yet
- The Long Term Outcome After Resection Of.20 PDFDocument9 pagesThe Long Term Outcome After Resection Of.20 PDFDragos IftimieNo ratings yet
- Testicular Torsion in Undescended TestisDocument5 pagesTesticular Torsion in Undescended TestisjimNo ratings yet
- Paragangliomas of The Head and Neck: A Pictorial EssayDocument25 pagesParagangliomas of The Head and Neck: A Pictorial Essayarief ardaNo ratings yet
- Refereat Treatment of Mandibular FractureDocument2 pagesRefereat Treatment of Mandibular Fracturearief ardaNo ratings yet
- Diagnosis Manage Rhinosinusitis WaldDocument39 pagesDiagnosis Manage Rhinosinusitis WaldLuis De jesus SolanoNo ratings yet
- OTOSCLEROSISDocument16 pagesOTOSCLEROSISarief ardaNo ratings yet
- Case ReportDocument8 pagesCase Reportarief ardaNo ratings yet
- Deep Neck Infection BaileyDocument20 pagesDeep Neck Infection Baileyarief ardaNo ratings yet
- Wer 9231Document4 pagesWer 9231arief ardaNo ratings yet
- WHO SurveillanceVaccinePreventable 04 Diphtheria R2Document15 pagesWHO SurveillanceVaccinePreventable 04 Diphtheria R2arief ardaNo ratings yet
- Branchial Anomalies in ChildrenDocument4 pagesBranchial Anomalies in Childrenarief ardaNo ratings yet
- Main PDFDocument4 pagesMain PDFNadya Dwi PuspitasariNo ratings yet
- Imaging Diagnosis of Benign Lesions of The External AuditoryDocument6 pagesImaging Diagnosis of Benign Lesions of The External Auditoryarief ardaNo ratings yet
- Juvenile Nasopharyngeal Angiofibroma SurgeryDocument18 pagesJuvenile Nasopharyngeal Angiofibroma Surgeryarief ardaNo ratings yet
- Sumber DD IktiosisDocument9 pagesSumber DD IktiosisprajnamitaNo ratings yet
- An Unusual Cause of Bullous MyringitisDocument2 pagesAn Unusual Cause of Bullous Myringitisarief ardaNo ratings yet
- Early Postoperative CT Scanning For JuvenileDocument7 pagesEarly Postoperative CT Scanning For Juvenilearief ardaNo ratings yet
- Clinicopathological Evaluation of Neck MassesDocument4 pagesClinicopathological Evaluation of Neck Massesarief ardaNo ratings yet
- Diphtheria AER 0Document1 pageDiphtheria AER 0arief ardaNo ratings yet
- Cancer of The External Auditory CanalDocument8 pagesCancer of The External Auditory Canalarief ardaNo ratings yet
- 3285 6152 1 SMDocument10 pages3285 6152 1 SMarief ardaNo ratings yet
- Prevalence and Pattern of Neck MassesDocument4 pagesPrevalence and Pattern of Neck Massesarief ardaNo ratings yet
- Adjuvant Therapy With Flutamide For PresurgicalDocument7 pagesAdjuvant Therapy With Flutamide For Presurgicalarief ardaNo ratings yet
- A Clinical, HistopathologicalDocument10 pagesA Clinical, Histopathologicalarief ardaNo ratings yet
- Management Dilemmas in TheDocument6 pagesManagement Dilemmas in Thearief ardaNo ratings yet
- Neck Mass NewDocument9 pagesNeck Mass NewWahyu Permata LisaNo ratings yet
- Causes and Treatment TonsilitisDocument6 pagesCauses and Treatment TonsilitisKhilyatul MufidaNo ratings yet
- Control of Anterior EpistaxisDocument6 pagesControl of Anterior Epistaxisarief ardaNo ratings yet
- s40463 016 0138 2 PDFDocument5 pagess40463 016 0138 2 PDFSelvia LianyNo ratings yet
- Case Report OEDDocument7 pagesCase Report OEDarief ardaNo ratings yet
- Acute Tonsillitis and Its ComplicationsDocument5 pagesAcute Tonsillitis and Its Complicationsarief ardaNo ratings yet
- Classification of Books Using Python and FlaskDocument5 pagesClassification of Books Using Python and FlaskIJRASETPublicationsNo ratings yet
- Benefits and Limitations of BEPDocument2 pagesBenefits and Limitations of BEPAnishaAppuNo ratings yet
- Riqas Ri RQ9142 11aDocument6 pagesRiqas Ri RQ9142 11aGrescia Ramos VegaNo ratings yet
- Lesser Known Homoeopathic Medicines of Alopecia Areata.20200718115446Document9 pagesLesser Known Homoeopathic Medicines of Alopecia Areata.20200718115446BruntNo ratings yet
- Paul Wade - The Ultimate Isometrics Manual - Building Maximum Strength and Conditioning With Static Training-Dragon Door Publications (2020) - 120-146Document27 pagesPaul Wade - The Ultimate Isometrics Manual - Building Maximum Strength and Conditioning With Static Training-Dragon Door Publications (2020) - 120-146usman azharNo ratings yet
- Aero Ebook - Choosing The Design of Your Aircraft - Chris Heintz PDFDocument6 pagesAero Ebook - Choosing The Design of Your Aircraft - Chris Heintz PDFGana tp100% (1)
- Description and Operating Instructions: Multicharger 750 12V/40A 24V/20A 36V/15ADocument34 pagesDescription and Operating Instructions: Multicharger 750 12V/40A 24V/20A 36V/15APablo Barboza0% (1)
- Engineering DrawingDocument1 pageEngineering DrawingDreamtech PressNo ratings yet
- CRISTIAN COLCERIU - PERSONALITATI CLUJENE Prof - Dr.ing - POMPILIU MANEADocument21 pagesCRISTIAN COLCERIU - PERSONALITATI CLUJENE Prof - Dr.ing - POMPILIU MANEAcristian colceriu100% (2)
- 160kW SOFT STARTER - TAP HOLE 1Document20 pages160kW SOFT STARTER - TAP HOLE 1Ankit Uttam0% (1)
- Case 3 SectionC Group 1 (Repaired)Document3 pagesCase 3 SectionC Group 1 (Repaired)SANDEEP AGRAWALNo ratings yet
- DAA UNIT 1 - FinalDocument38 pagesDAA UNIT 1 - FinalkarthickamsecNo ratings yet
- Coal Bottom Ash As Sand Replacement in ConcreteDocument9 pagesCoal Bottom Ash As Sand Replacement in ConcretexxqNo ratings yet
- Crisis of The World Split Apart: Solzhenitsyn On The WestDocument52 pagesCrisis of The World Split Apart: Solzhenitsyn On The WestdodnkaNo ratings yet
- Impact of Government Policies and EthicsDocument24 pagesImpact of Government Policies and EthicsGunveen AbrolNo ratings yet
- Akilas Mebrahtom ResumeDocument1 pageAkilas Mebrahtom ResumeAnonymous lLpBfQNo ratings yet
- Chapter 2.3.3 History of Visual Arts Modernism Post ModernismDocument17 pagesChapter 2.3.3 History of Visual Arts Modernism Post ModernismKim Ashley SarmientoNo ratings yet
- Generalized Class of Sakaguchi Functions in Conic Region: Saritha. G. P, Fuad. S. Al Sarari, S. LathaDocument5 pagesGeneralized Class of Sakaguchi Functions in Conic Region: Saritha. G. P, Fuad. S. Al Sarari, S. LathaerpublicationNo ratings yet
- What You Need To Know About Your Drive TestDocument12 pagesWhat You Need To Know About Your Drive TestMorley MuseNo ratings yet
- Past Simple Vs Past ContinuousDocument3 pagesPast Simple Vs Past ContinuousNatalia SalinasNo ratings yet
- Designing and Drawing PropellerDocument4 pagesDesigning and Drawing Propellercumpio425428100% (1)
- Transparency and Digitalization in The Public Administration of RomaniaDocument8 pagesTransparency and Digitalization in The Public Administration of RomaniaMădălina MarincaşNo ratings yet
- C. Robert Mesle (Auth.) - John Hick's Theodicy - A Process Humanist Critique-Palgrave Macmillan UK (1991)Document168 pagesC. Robert Mesle (Auth.) - John Hick's Theodicy - A Process Humanist Critique-Palgrave Macmillan UK (1991)Nelson100% (3)
- Term Paper Inorganic PolymersDocument24 pagesTerm Paper Inorganic PolymersCasey Karua0% (1)
- EX200Document7 pagesEX200shubbyNo ratings yet
- PNP Ki in July-2017 AdminDocument21 pagesPNP Ki in July-2017 AdminSina NeouNo ratings yet
- Second Conditional Conversation QuestionsDocument2 pagesSecond Conditional Conversation QuestionsEdith Salomé PinosNo ratings yet
- How To Add Attachment Using JAVA MappingDocument4 pagesHow To Add Attachment Using JAVA MappingmvrooyenNo ratings yet
- DR S GurusamyDocument15 pagesDR S Gurusamybhanu.chanduNo ratings yet
- BSH 7005-15Document129 pagesBSH 7005-15Mark InnesNo ratings yet