Professional Documents
Culture Documents
Idiopathic Fatal Pancytopenia
Uploaded by
Kaye Antonette AntioquiaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Idiopathic Fatal Pancytopenia
Uploaded by
Kaye Antonette AntioquiaCopyright:
Available Formats
DOI: 10.7860/JCDR/2016/19230.
7996
Case Report
Idiopathic Fatal Pancytopenia:
Pathology Section
A Case Report
Hema Goyal1, Vijai Tilak2
ABSTRACT
Pancytopenia is defined as decrease in red blood cells, white blood cells and platelets. Many disease processes involve the bone marrow
primarily or secondarily resulting in pancytopenia. A 55-year-old male presented with generalized body weakness and few episodes of
malena for last one year. Physical and systemic examination was unremarkable. CBC report revealed pancytopenia. Other haematological
parameters were within normal limit. Stool for occult blood was positive. USG and CECT abdomen showed no abnormality. The patient
was evaluated for any evidence of malignancy but no clue was found. Bone marrow examination was done as patient was having
pancytopenia. Bone marrow smears, clot sections and bone marrow biopsy was normal. Immunohistochemistry and cytogenetics study
was unremarkable. Patient was admitted in hospital for 1 month and his condition rapidly deteriorated. The cause of pancytopenia
remained unexplained and therefore it was named as Idiopathic fatal pancytopenia. “Idiopathic Fatal Pancytopenia (IFP)” is an emerging
new entity with a grave prognosis. We wish to sensitize the medical community and the scientists to this rapidly fatal condition.
Keywords: Cytogenetics, Idiopathic cytopenia of undetermined significance (ICUS), Immunohistochemistry
CASE REPORT
A non-diabetic, non-hypertensive 55-year-old male patient pre
sented with generalized body weakness and few episodes of
malena since last one year. Physical examination of the patient
revealed mild pallor, no clubbing, no jaundice, no lymphadenopathy
and no pedal oedema. Informed consent was obtained from the
patient.
Systemic examination was within normal limit. There was no relevant
history of intake of any drugs or previous radiation exposure. CBC
revealed pancytopenia with Hb-9.5g/dl, TLC -3700 cells/cumm,
Platelet count – 89,000 cells/cumm, RBC count – 3.17X106 /UL,
MCH – 29.9pg, MCV – 88.2fl, MCHC – 34g/dl, RDW – 15.9%,
Reticulocyte count was 0.9%. As per the previous records, patient
was having pancytopenia since 8 months. Stool for occult blood
was positive. Renal function test, liver function test, lipid profile was
within normal limit. Clinically urine was straw coloured and urine
routine microscopy was done to rule out microhaematuria. Serum
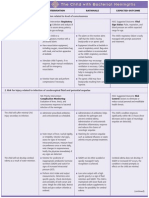
[Table/Fig-1]: Clot Section- section shows normocellular particle (Leishman, 20X).
LDH was 700 IU/L, S.Ferritin – 123.8 mg/dl, S.iron – 109mg/dl and
TIBC – 89µg/dl. Bleeding time, PT(INR), APTT and coagulation
profile was within normal limit. Ultrasound abdomen and KUB was
done to rule any specific pathology but was normal. Viral markers
(HBsAg, HIV, HAV, HCV, EBV), Dengue, paracheck, rk39 and
leptospira (IgG & IgM) test were negative. Contrast enhanced CT
scan was done and no evidence of any pathology was detected. As
the patient had few episodes of malena, endoscopy was performed
but it was within normal limits. Bone marrow examination was done
and smears showed normal distribution of all lineage, no evidence
of dysplasia, no increase in blasts and absence of ringed sideroblast
on perl’s stain. Clot section revealed 5 normocellular particles and
showed normal haematopoiesis [Table/Fig-1]. Bone marrow biopsy
was also done, sections showed normocellular biopsy with normal
distribution of haematopoiesis and no evidence of myelodysplasia
noted [Table/Fig-2]. Immunohistochemistry with CD34 showed
no increase in blast (<1%) [Table/Fig-3]. Cytogenetics was done
on bone marrow aspirate and G banding was done and showed
normal karyotype (46,XY) [Table/Fig-4].
[Table/Fig-2]: Bone Marrow Biopsy: Section shows normocellular bone marrow with
During the stay in hospital, patients Hb, TLC and platelet counts normal distribution of all lineages (Leishman, 10X).
were in declining trend shown in [Table/Fig-5].
Journal of Clinical and Diagnostic Research. 2016 Jun, Vol-10(6): ED09-ED11 9
Hema Goyal and Vijai Tilak, Idiopathic Fatal Pancytopenia: A Case Report www.jcdr.net
DISCUSSION
Pancytopenia is defined by reduction of all the three formed
elements of blood below the normal reference range [1]. Variety of
disorders, haematological and non-haematological can affect the
bone marrow primarily or secondarily, resulting in the manifestation
of pancytopenia [2]. In cases where a definite cause of persistent
cytopenia (without dysplasia and without one of the specific
cytogenetic abnormalities) cannot be determined, the condition
is regarded as Idiopathic Cytopenia of Undetermined Significance
(ICUS) and long term follow-up is recommended to assess the
evolution [3].
Idiopathic cytopenia of undetermined significance (ICUS) [3,4] is a
recently proposed, provisional diagnostic category that recognizes
patients who present with cytopenias of undetermined etiology.
The current proposed criteria for diagnosing ICUS include:
(a) Persistent cytopenia (for 6 months): hemoglobin <11 g/dl,
[Table/Fig-3]: IHC (CD34): Normal blood vessels are highlighted by CD34. No neutrophils <1.5×109L, and platelets <100×109/L;
increase in blast is seen.
(b) No morphologic features of myelodysplasia;
(c) Normal chromosome analysis and
(d) A detailed clinical history and investigation that excludes other
secondary causes of cytopenias.
These criteria suggest that there are three major components
for an ICUS diagnosis: morphologic examination, cytogenetic
analysis, and detailed clinical investigation.
The diagnosis of ICUS should only be established when all
potential differential diagnoses (hepatopathy, infectious diseases,
chronic inflammation, mastocytosis, others) have been excluded
ICUS, a term was also proposed by Dr. G. Mufti (8th International
Symposium on MDS, Nagasaki, Japan, 2005) and recommends
long term follow up to assess the evolution [3].
The natural history of patients with ICUS is largely unknown and
appears to be highly variable [5]. Small studies indicate that some
patients will go on to develop frank MDS or a related myeloid
[Table/Fig-4]: Cytogenetics study shows normal karyogram of the patient (46+XY) malignancy such as AML [6]. Others may follow a more indolent
course [7].
At admission In our case, patient presented with persistent pancytopenia
Parameters 1st day 8th day 15th day 20th day 24th day 26th day since 8 months and there is evidence of persistent decrease in
HB(gm/dl) 9.5 8.2 7.7 5.8 4.2 3.1 haematological parameters further leading to death.
TLC 3700 3600 3600 3400 3400 2900 Wimazal F et al., published a series of 10 cases which were
(cells/cumm)
diagnosed as ICUS. All of them were followed up and the period of
Platelet 89,000 85,000 60,000 53,000 50,000 27,000
(cells/cumm)
follow-up ranged from few months to few years [8]. It is pertinent
to mention that all the 10 patients were alive at least for a period
[Table/Fig-5]: Table shows haematological parameters of the patient during the
stay in hospital. of six months. The term ‘undetermined significance’ was used in
ICUS since the cytopenia was stable and the patient were alive for
Initially patient was started on symptomatic management. at least 6 months. In our case ICUS- pancytopenia could not be
Patient was started on haematinic therapy but patient showed offered, as the entity was not of unknown significance but of grave
no improvement. On day 20 patients Hb dropped to 5.8gm/dl, significance as even after an exhaustive clinical and laboratory
then he was given two units of packed RBC transfusion (PRBC). work-up, no cause of pancytopenia was found and the patient
There were no signs of active bleed. Despite the above measures died without a definite diagnosis. We therefore suggest the term
patient did not improve clinically. On 24th day, patient had mild “Idiopathic fatal pancytopenia (IFP)” for such cases.
gum bleeding followed by nasal bleed, bleed through ryles tube
and then several episodes of malena and haemetemesis. A Various international studies reported few cases of pancytopenia
repeat PT INR, APTT, Bleeding time and coagulation profile was with normal marrow which ranged from 3.38% to10.5% [9-12].
done and was within normal limit. Patient developed respiratory But no follow-up of the patient was described in these studies. No
distress, tachypnea, tachycardia along with persistent hypotension study has reported the phenomenon of IFP.
and went into haemorrhgic shock. After fluid resuscitation and
blood transfusions, the patient vitals remain unstable. Ionotropes CONCLUSION
were started. Massive blood transfusion was given as per our We report for the first time a new entity “Idiopathic Fatal Pancyto
institutional protocols. Due to persistent haemorrhgic shock, penia (IFP)” for pancytopenic patients in whom a definite etiology
patient developed metabolic acidosis secondary to lactic acidosis cannot be established even after an exhaustive workup and who
and then refractory hyperkalaemia and went into cardiorespiratory eventually succumb to the complication of pancytopenia. Further
arrest. The cause of pancytopenia remained unexplained and research is necessary to elucidate the underlying pathology and
therefore was diagnosed as Idiopathic fatal pancytopenia. potential drugs to halt the inevitable death.
10 Journal of Clinical and Diagnostic Research. 2016 Jun, Vol-10(6): ED09-ED11
www.jcdr.net Hema Goyal and Vijai Tilak, Idiopathic Fatal Pancytopenia: A Case Report
REFERENCES undetermined significance (ICUS): HUMARA unravels clonality in a subgroup of
patients. Ann Oncol. 2010;21(11):2267-71.
[1] Williams DM. Wintrobe’s Clinical Haematology, 10th edition. Baltimore; William
[7] Busque L, Patel JP, Figueroa ME, Vasanthakumar A, Provost S, Hamilou Z, et
and Wilkins; 1993.1449-84.
al. Recurrent somatic TET2 mutations in normal elderly individuals with clonal
[2] Khodke K, Marwah S, Buxi G, Vadav RB, Chaturvedi NK, Bone marrow
haematopoiesis. Nat Genet. 2012;44(11):1179-81.
examination in cases of pancytopenia. J Academy Clin Med. 2001;2:55-59.
[8] Wimazal F, Fonatsch C, Thalhammer R, Schwarzinger I, Müllauer L, Sperr WR,
[3] Valent P, Horny HP, Bennett JM, Fonatsch C, Germing U, Greenberg P, et al.
et al. Idiopathic cytopenia of undetermined significance (ICUS) versus low risk
Definitions and standards in the diagnosis and treatment of the myelodysplastic
MDS: the diagnostic interface. Leuk Res. 2007;31:1461–68.
syndromes: Consensus statements and report from a working conference.
[9] Jha A, Sayami G, Adhikari RC, Patna AD, Jha R. Bone marrow examination in
Leukemia Research. 2007;(31):727–36.
cases of pancytopenia. J Nepal Med Assoc. 2008;47:12-17.
[4] Valent P, Bain BJ, Bennett JM, Wimazal F, Sperr WR, Mufti G, et al. Idiopathic
[10] Pathak R, Jha A, Sayami G. Evaluation of bone marrow in patients with
cytopenia of undetermined significance (ICUS) and idiopathic dysplasia of
pancytopenia. Journal of Pathology of Nepal. 2012;2:265–71.
uncertain significance (IDUS), and their distinction from low risk MDS. Leukemia
[11] Lakhey A, Talwar OP, Singh VK, KC SR. Clinico-haematological study of
Research. 2012;(36):1–5.
pancytopenia. Journal of Pathology of Nepal. 2012;(2):207–10.
[5] Kwok B, Hall JM, Witte J S, Xu Y, Reddy P, Lin K, et al. MDS-associated somatic
[12] Pudasaini S, Prasad KBR, Rauniyar SK, Shrestha R, Gautam K, Pathak R, et al.
mutations and clonal haematopoiesis are common in idiopathic cytopenias of
Interpretation of bone marrow aspiration in haematological disorder. Journal of
undetermined significance. Blood. 2015;126(21):2355-61.
Pathology of Nepal. 2012;2:309-12.
[6] Schroeder T, Ruf L, Bernhardt A, Hildebrandt B, Aivado M, Aul C, et al.
Distinguishing myelodysplastic syndromes (MDS) from idiopathic cytopenia of
PARTICULARS OF CONTRIBUTORS:
1. Junior Resident, Department of Pathology, IMS, BHU, Varanasi, India.
2. Professor, Department of Pathology, IMS, BHU, Varanasi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:
Dr. Hema Goyal, Date of Submission: Feb 04, 2016
SE-357, Shastri Nagar, Ghaziabad-201002, India. Date of Peer Review: Feb 23, 2016
E-mail: hemagoyal88@gmail.com
Date of Acceptance: Apr 09, 2016
Financial OR OTHER COMPETING INTERESTS: None. Date of Publishing: Jun 01, 2016
Journal of Clinical and Diagnostic Research. 2016 Jun, Vol-10(6): ED09-ED11 11
You might also like
- Diagnosis of Blood and Bone Marrow DisordersFrom EverandDiagnosis of Blood and Bone Marrow DisordersSa A. WangNo ratings yet
- A Case Report of Malignant Hypertension in A YoungDocument7 pagesA Case Report of Malignant Hypertension in A YoungMega AnggarNo ratings yet
- Sandaletal UpdateonITPDocument18 pagesSandaletal UpdateonITPMarcellia AngelinaNo ratings yet
- 14 Nisal EtalDocument5 pages14 Nisal EtaleditorijmrhsNo ratings yet
- Low Blood Counts: Immune Mediated, Idiopathic, or MyelodysplasiaDocument7 pagesLow Blood Counts: Immune Mediated, Idiopathic, or MyelodysplasiaaaaaNo ratings yet
- Sfaa 142Document11 pagesSfaa 142Eduardo AdameNo ratings yet
- Urinary Incontinence As A Possible Signal of Neuromuscular Toxicity During Immune Checkpoint Inhibitor Treatment - Case Report and Retrospective Pharmacovigilance StudyDocument10 pagesUrinary Incontinence As A Possible Signal of Neuromuscular Toxicity During Immune Checkpoint Inhibitor Treatment - Case Report and Retrospective Pharmacovigilance StudyRA Tri Retno WulanNo ratings yet
- Tau 10 11 4100Document10 pagesTau 10 11 4100marcelloNo ratings yet
- Maiden2008 Article ABlindedPilotComparisonOfCapsuDocument4 pagesMaiden2008 Article ABlindedPilotComparisonOfCapsuRecep Taha ErdoganNo ratings yet
- Pancytopenia A Clinico Hematological StudyDocument6 pagesPancytopenia A Clinico Hematological StudyUci Rahmadhani MNo ratings yet
- 2016 Article 291Document6 pages2016 Article 291Yunika ArumNo ratings yet
- Cureus 0014 00000022733Document6 pagesCureus 0014 00000022733Dede IskandarNo ratings yet
- Etiological Causes of Pancytopenia: A Report of 137 Cases: ArticleDocument4 pagesEtiological Causes of Pancytopenia: A Report of 137 Cases: ArticleGabriella HardikasariNo ratings yet
- Chilaiditi Syndrome: Rare Bowel AbnormalityDocument4 pagesChilaiditi Syndrome: Rare Bowel AbnormalityZoraya Febriana SyahnazNo ratings yet
- Risk Factors and Management of Primary Choledocholithiasis: A Systematic ReviewDocument8 pagesRisk Factors and Management of Primary Choledocholithiasis: A Systematic ReviewKAREN LUCERO VASQUEZ NORIEGANo ratings yet
- Hivan Ucla PDFDocument29 pagesHivan Ucla PDFAndrés David Calles UrdanetaNo ratings yet
- Fulminant Hepatitis Revealing Complicated Crohn S Disease of Budd Chiari Syndrome About A CaseDocument6 pagesFulminant Hepatitis Revealing Complicated Crohn S Disease of Budd Chiari Syndrome About A CaseHerald Scholarly Open AccessNo ratings yet
- 2Document6 pages2Srinath M VNo ratings yet
- Jurnal SOFADocument11 pagesJurnal SOFAMekar PalupiNo ratings yet
- Algoritmo Diagnóstico Trombocitopénia Japão 2024Document13 pagesAlgoritmo Diagnóstico Trombocitopénia Japão 2024nigel farageNo ratings yet
- Purpura Trombocitopenica ImunaDocument8 pagesPurpura Trombocitopenica ImunaDenisa Carmen ColiofNo ratings yet
- Villanacci2011the Spectrum of Drug-Related Colitides Important Entities, Though Frequently OverlookedDocument6 pagesVillanacci2011the Spectrum of Drug-Related Colitides Important Entities, Though Frequently OverlookedKito TongHuiNo ratings yet
- 2022 Parathyroid Carcinoma All-In-One, A Rare Life-Threatening Case With Multiple Systemic Manifestations Case Report and Review of The LiteratureDocument12 pages2022 Parathyroid Carcinoma All-In-One, A Rare Life-Threatening Case With Multiple Systemic Manifestations Case Report and Review of The LiteratureCharley WangNo ratings yet
- The Histopathological Evaluation of Drug-Induced Liver InjuryDocument13 pagesThe Histopathological Evaluation of Drug-Induced Liver InjuryAnonymous 01bH8iNo ratings yet
- Acute Kidney Injury Pathology and PathophysiologyDocument11 pagesAcute Kidney Injury Pathology and Pathophysiologyhossein kasiriNo ratings yet
- DefinitionofdicDocument9 pagesDefinitionofdicDwika AudiyanandaNo ratings yet
- JAHA.121.021198Document38 pagesJAHA.121.021198Cut Keumala PutriNo ratings yet
- Diagnosis and Management of PNHDocument12 pagesDiagnosis and Management of PNHapi-26302710No ratings yet
- Pti y MMDocument2 pagesPti y MMClara Espinosa ArnandisNo ratings yet
- Ajprenal 00376 2017Document8 pagesAjprenal 00376 2017Ana-Mihaela BalanuțaNo ratings yet
- Bone Marrow Evaluation of Patients Having Pancytopenia at Tertiary Care Center, M. Y. Hospital, Indore, India: One-Year StudyDocument4 pagesBone Marrow Evaluation of Patients Having Pancytopenia at Tertiary Care Center, M. Y. Hospital, Indore, India: One-Year StudyivanNo ratings yet
- Management of Chronic Liver Diseases And.1Document3 pagesManagement of Chronic Liver Diseases And.1aldyNo ratings yet
- Immune Thrombocytopenic Purpura: 3. DiagnosisDocument3 pagesImmune Thrombocytopenic Purpura: 3. DiagnosisAy'oe Ithyu RezthuNo ratings yet
- Splenectomy - A Therapeutic Option in Splenic Marginal Zone Cell LymphomaDocument11 pagesSplenectomy - A Therapeutic Option in Splenic Marginal Zone Cell LymphomaFlorin IliescuNo ratings yet
- Myelodysplastic Syndromes: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpDocument15 pagesMyelodysplastic Syndromes: ESMO Clinical Practice Guidelines For Diagnosis, Treatment and Follow-UpUmmul HayatiNo ratings yet
- Fine Needle Aspiration Cytology (FNAC) of GISTDocument7 pagesFine Needle Aspiration Cytology (FNAC) of GISTurfriendanshul100% (1)
- sepsis_induced_coagulopathy__a_comprehensive.2 (1)Document16 pagessepsis_induced_coagulopathy__a_comprehensive.2 (1)antoine.dovalNo ratings yet
- Ren 2020 Alteraciones MicrobiotaDocument14 pagesRen 2020 Alteraciones MicrobiotaMartin GomezNo ratings yet
- Journal of Medical Case Reports: Adrenocortical Oncocytic Neoplasm Presenting With Cushing's Syndrome: A Case ReportDocument5 pagesJournal of Medical Case Reports: Adrenocortical Oncocytic Neoplasm Presenting With Cushing's Syndrome: A Case Reportlala_bojaNo ratings yet
- 1717 Manuscript 7426 1 10 20180428Document5 pages1717 Manuscript 7426 1 10 20180428Labnotes LCNo ratings yet
- BiopsyDocument4 pagesBiopsyanirbanmanna88320No ratings yet
- Gastrointestinal Stromal Tumors-A Mini ReviewDocument14 pagesGastrointestinal Stromal Tumors-A Mini ReviewThomas KlebNo ratings yet
- Fulltext - Ams v5 Id1040Document4 pagesFulltext - Ams v5 Id1040yaneemayNo ratings yet
- Inflammatory Myofibroblastic TumourDocument4 pagesInflammatory Myofibroblastic TumourThiruNo ratings yet
- SMW 09797 PDFDocument9 pagesSMW 09797 PDFEJ AguilarNo ratings yet
- Disseminated Intravascular Coagulation: A Practical ApproachDocument7 pagesDisseminated Intravascular Coagulation: A Practical Approachoki harisandiNo ratings yet
- Cytology of Bone MarrowDocument62 pagesCytology of Bone MarrowFabrício CamargoNo ratings yet
- Diagnosis of Sepsis Induced DicDocument10 pagesDiagnosis of Sepsis Induced DicDwika AudiyanandaNo ratings yet
- IJPO_3(3)_479-484 (2)Document6 pagesIJPO_3(3)_479-484 (2)Srinath M VNo ratings yet
- Case ConDocument9 pagesCase ConDhine Dhine ArguellesNo ratings yet
- Thyroid-Like Follicular Carcinoma of The Kidney in A Chronic Dialysis Patient: One Case Report and Review of The LiteratureDocument8 pagesThyroid-Like Follicular Carcinoma of The Kidney in A Chronic Dialysis Patient: One Case Report and Review of The LiteratureIJAR JOURNALNo ratings yet
- Review of Systemic Amyloidosis Types and Clinical ManifestationsDocument25 pagesReview of Systemic Amyloidosis Types and Clinical ManifestationsMathew McCarthy100% (1)
- 2011 SuzukiDocument9 pages2011 SuzukiElviraNo ratings yet
- OpenVetJ 13 233Document8 pagesOpenVetJ 13 233Emilia AmmariNo ratings yet
- AKI PathogenesisDocument11 pagesAKI PathogenesisKaren RamNo ratings yet
- Pancytopenia: A Clinico Hematological Study: Gayathri B N, Kadam Satyanarayan RaoDocument6 pagesPancytopenia: A Clinico Hematological Study: Gayathri B N, Kadam Satyanarayan RaoYeni PuspitasariNo ratings yet
- Study of Histopathological Spectrum of GallbladderDocument7 pagesStudy of Histopathological Spectrum of GallbladderleartaNo ratings yet
- Pathology of Kidney in Medicolegal AutopsyDocument6 pagesPathology of Kidney in Medicolegal AutopsyDr. Haricharan ANo ratings yet
- Renal BiopsyDocument4 pagesRenal BiopsyDeshan AdikariNo ratings yet
- Blastoid Mantle Cell LymphomaDocument3 pagesBlastoid Mantle Cell LymphomaAlinaNo ratings yet
- Child - Bacterial MeningitisDocument3 pagesChild - Bacterial MeningitisJessica PhillipsNo ratings yet
- NCP For Impaired Gas ExchangeDocument2 pagesNCP For Impaired Gas ExchangeSweetie Star94% (16)
- DEATHDocument1 pageDEATHKaye Antonette AntioquiaNo ratings yet
- 1Document1 page1Kaye Antonette AntioquiaNo ratings yet
- Peerj 4846 PDFDocument20 pagesPeerj 4846 PDFKaye Antonette AntioquiaNo ratings yet
- Child - Bacterial MeningitisDocument3 pagesChild - Bacterial MeningitisJessica PhillipsNo ratings yet
- Clinico-Hematological Analysis of PancytopeniaDocument4 pagesClinico-Hematological Analysis of PancytopeniaKaye Antonette AntioquiaNo ratings yet
- Idiopathic Fatal PancytopeniaDocument3 pagesIdiopathic Fatal PancytopeniaKaye Antonette AntioquiaNo ratings yet
- Blood Pressure Targets in The Elderly.5Document3 pagesBlood Pressure Targets in The Elderly.5Kaye Antonette AntioquiaNo ratings yet
- Pancytopenia - A Clinicopathological Analysis of 132 CasesDocument11 pagesPancytopenia - A Clinicopathological Analysis of 132 CasesKaye Antonette AntioquiaNo ratings yet
- Acute Myeloid Leukemia Presenting As PancytopeniaDocument3 pagesAcute Myeloid Leukemia Presenting As PancytopeniaKaye Antonette AntioquiaNo ratings yet
- The Study of Clinico-Aetiological Profile of Pancytopenia in Elderly PDFDocument3 pagesThe Study of Clinico-Aetiological Profile of Pancytopenia in Elderly PDFKaye Antonette AntioquiaNo ratings yet
- Patient Info Wound Care Leaflet PDFDocument2 pagesPatient Info Wound Care Leaflet PDFKaye Antonette AntioquiaNo ratings yet
- An Etiological Reappraisal of Pancytopenia - LargestDocument9 pagesAn Etiological Reappraisal of Pancytopenia - LargestKaye Antonette AntioquiaNo ratings yet
- Journal ReadingDocument8 pagesJournal ReadingKaye Antonette AntioquiaNo ratings yet
- CKD Management in GP Handbook 3rd EditionDocument56 pagesCKD Management in GP Handbook 3rd EditionDesla CitraNo ratings yet
- Evaluation of A Community-Based Program That Integrates Joyful Movement Into Fall Prevention For Older AdultsDocument8 pagesEvaluation of A Community-Based Program That Integrates Joyful Movement Into Fall Prevention For Older AdultsKaye Antonette AntioquiaNo ratings yet
- Travel-Associated Zika Cases in California During Global OutbreakDocument8 pagesTravel-Associated Zika Cases in California During Global OutbreakKaye Antonette AntioquiaNo ratings yet
- International Journal of GerontologyDocument5 pagesInternational Journal of GerontologyKaye Antonette AntioquiaNo ratings yet
- Geriatrics 04 00004Document14 pagesGeriatrics 04 00004Kaye Antonette AntioquiaNo ratings yet
- Travel-Associated Zika Cases in California During Global OutbreakDocument8 pagesTravel-Associated Zika Cases in California During Global OutbreakKaye Antonette AntioquiaNo ratings yet
- Memory and Confusion ComplaintsDocument9 pagesMemory and Confusion ComplaintsKaye Antonette AntioquiaNo ratings yet
- International Journal of Gerontology: Thiago J. Avelino-Silva, Omar JaluulDocument6 pagesInternational Journal of Gerontology: Thiago J. Avelino-Silva, Omar JaluulKaye Antonette AntioquiaNo ratings yet
- International Journal of GerontologyDocument5 pagesInternational Journal of GerontologyKaye Antonette AntioquiaNo ratings yet
- International Journal of GerontologyDocument5 pagesInternational Journal of GerontologyKaye Antonette AntioquiaNo ratings yet
- Geriatrics: Falls in Geriatric Populations and Hydrotherapy As An Intervention: A Brief ReviewDocument8 pagesGeriatrics: Falls in Geriatric Populations and Hydrotherapy As An Intervention: A Brief ReviewKaye Antonette AntioquiaNo ratings yet
- Geriatrics 04 00004Document14 pagesGeriatrics 04 00004Kaye Antonette AntioquiaNo ratings yet
- Adherence To Exercise Programs in Older Adults: Informative ReportDocument10 pagesAdherence To Exercise Programs in Older Adults: Informative ReportKaye Antonette AntioquiaNo ratings yet
- Blood Culture With CAPDocument10 pagesBlood Culture With CAPKaye Antonette AntioquiaNo ratings yet
- (Teach Yourself) David Le Vay, Jenny Stafford-Brown - Anatomy & Physiology - A Complete Introduction-John Murray Learning (2015)Document385 pages(Teach Yourself) David Le Vay, Jenny Stafford-Brown - Anatomy & Physiology - A Complete Introduction-John Murray Learning (2015)Teresa ChaoNo ratings yet
- Science - 2Document130 pagesScience - 2Bhavesh KaleNo ratings yet
- IGCSE Biology: Grade VIII Biochemical TestsDocument26 pagesIGCSE Biology: Grade VIII Biochemical TestsSarveshrau MagentharauNo ratings yet
- Dennett's 4 Levels of Creatures from Darwinian to GregorianDocument3 pagesDennett's 4 Levels of Creatures from Darwinian to GregorianNur Izatie IsmailNo ratings yet
- The Digestive System ExplainedDocument33 pagesThe Digestive System ExplainedGulAwezNo ratings yet
- Protein-Benefits-Infographic Arms100214-04Document2 pagesProtein-Benefits-Infographic Arms100214-04api-226153893No ratings yet
- Eukaryotic DNA Polymerases: Sue Cotterill, Stephen KearseyDocument6 pagesEukaryotic DNA Polymerases: Sue Cotterill, Stephen KearseyOphy FirmansyahNo ratings yet
- Paramecium Homeostasis SeDocument4 pagesParamecium Homeostasis SePofukSilvestar0% (2)
- AML WHO IncludedDocument79 pagesAML WHO IncludedErika Nicole DoradoNo ratings yet
- Yeast DisplayDocument7 pagesYeast DisplayAnnisa Pratiwi GunawanNo ratings yet
- 14 Ways Plants Benefit Humans & EarthDocument6 pages14 Ways Plants Benefit Humans & EarthdeepakatoliaNo ratings yet
- Soal-Soal Bu Ganies PDFDocument2 pagesSoal-Soal Bu Ganies PDFNur Qamar Rahmah100% (1)
- Edexcel GCE Biology Unit-4 June 2013 Question PaperDocument20 pagesEdexcel GCE Biology Unit-4 June 2013 Question PaperAvrinox100% (1)
- Science Class 4 HabitatsDocument6 pagesScience Class 4 HabitatsCatherine JeaneNo ratings yet
- 5grade 10 October QE 2018-2019Document21 pages5grade 10 October QE 2018-2019Lucille Gacutan AramburoNo ratings yet
- Hiv Associated Hematological Malignasis - Marcus HentrichDocument239 pagesHiv Associated Hematological Malignasis - Marcus HentrichJaronjer1No ratings yet
- Domain Eukarya Kingdom ProtistaDocument23 pagesDomain Eukarya Kingdom Protistaanis azizNo ratings yet
- Gbre 2Document259 pagesGbre 2Rommel Bauza86% (7)
- LncRNAs in Neurodegenerative DiseasesDocument12 pagesLncRNAs in Neurodegenerative DiseasesProsenjit PalNo ratings yet
- Embryology Study GuideDocument255 pagesEmbryology Study GuideSiddharth KatyalNo ratings yet
- Molecular Biology: Louise Kamona Kabwe 1616713: 1001839253:::: / 784199656856434: 100821ASTJ0035Document1 pageMolecular Biology: Louise Kamona Kabwe 1616713: 1001839253:::: / 784199656856434: 100821ASTJ0035Louise KamonaNo ratings yet
- Comparing species identification methods for garfish in Muara Angke fish marketDocument8 pagesComparing species identification methods for garfish in Muara Angke fish marketFAKHRI HUSAINI NASUTION 1No ratings yet
- Entamoeba histolytica parasites summaryDocument16 pagesEntamoeba histolytica parasites summaryMarielle Katherine E. EgamNo ratings yet
- 2011 Semifinal Exam QuestionsDocument42 pages2011 Semifinal Exam Questionsmartynapet100% (1)
- Revision Sexual Repro Updated - 015735Document5 pagesRevision Sexual Repro Updated - 015735George SkariahNo ratings yet
- Meiosis and Tetrad AnalysisDocument10 pagesMeiosis and Tetrad Analysishuangc17No ratings yet
- Goljan Audio TranscriptsDocument201 pagesGoljan Audio Transcriptsendocrinology101No ratings yet
- Preparation of BAP and CHOCDocument5 pagesPreparation of BAP and CHOCKenneth Jake BatiduanNo ratings yet
- A Non Beta Cell Tumor Located in The Abdomen of A Patient With Hypoglycaemia Secreting High Levels of "Big" Insulin-Like Growth Factor (IGF) - II and IGF-binding Protein-6.Document8 pagesA Non Beta Cell Tumor Located in The Abdomen of A Patient With Hypoglycaemia Secreting High Levels of "Big" Insulin-Like Growth Factor (IGF) - II and IGF-binding Protein-6.Wouter van de HoefNo ratings yet
- NucleusDocument11 pagesNucleusKaysean MielNo ratings yet