Professional Documents
Culture Documents
The Prediction of Difficult Intubation in Obese Pa
Uploaded by
anindita fauziahCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Prediction of Difficult Intubation in Obese Pa
Uploaded by
anindita fauziahCopyright:
Available Formats
[Downloaded free from http://www.joacp.org on Wednesday, September 28, 2016, IP: 82.54.195.
219]
Original Article
The prediction of difficult intubation in obese patients using
mirror indirect laryngoscopy: A prospective pilot study
Arne O Budde, Matthew Desciak1, Venugopal Reddy, Octavio A Falcucci, Sonia J Vaida,
Leonard M Pott
Department of Anesthesiology, 1Geisinger Health System, Wilkes-Barre, PA; Penn State University College of Medicine, Hershey,
PA, United States
Abstract
Background: The incidence of difficult laryngoscopy and intubation in obese patients is higher than in the general population.
Classical predictors of difficult laryngoscopy and intubation have been shown to be unreliable. We prospectively evaluated
indirect mirror laryngoscopy as a predictor of difficult laryngoscopy in obese patients.
Materials and Methods: 60 patients with a body mass index (BMI) greater than 30, scheduled to undergo general anesthesia,
were enrolled. Indirect mirror laryngoscopy was performed and was graded 1‑4 according to Cormack and Lehane. A view of
grade 3‑4 was classified as predicting difficult laryngoscopy. Additional assessments for comparison were the Samsoon and Young
modification of the Mallampati airway classification, Wilson Risk Sum Score, neck circumference, and BMI. The view obtained
upon direct laryngoscopy after induction of general anesthesia was classified according to Cormack and Lehane as grade 1-4.
Results: Sixty patients met the inclusion criteria; however, 8 (13.3%) patients had an excessive gag reflex, and examination
of the larynx was not possible. 15.4% of patients who underwent direct laryngoscopy had a Cormack and Lehane grade 3 or 4
view and were classified as difficult. Mirror laryngoscopy had a tendency toward statistical significance in predicting difficult
laryngoscopy in these patients.
Conclusions: This study is consistent with previous studies, which have demonstrated that no one individual traditional
test has proven to be adequate in predicting difficult airways in the obese population. However, the new application of an old
test ‑ indirect mirror laryngoscopy ‑ could be a useful additional test to predict difficult laryngoscopy in obese patients.
Key words: Difficult airway, mirror indirect laryngoscopy, obesity, prediction
Introduction patients present the anesthesiologist with additional challenges,
such as redundant neck soft tissue, impaired neck mobility, and
Assessment of the airway and anticipation of the “difficult large chest and breasts. The incidence of difficult intubation in
airway” are fundamental skills for an anesthesiologist. Although the obese population with a BMI of greater than 30 has been
the traditional methods of assessing the airway by Mallampati reported in a large meta‑analysis to be 15.8% compared to
score[1] and Wilson risk sum score[2] are widely accepted, these 5.8% in the general population.[5] Unfortunately, the classical
tests suffer from poor sensitivity with only moderate specificity and predictors of difficult intubation have been shown to be even less
have a limited positive predictive value.[3,4] The airways of obese reliable in the obese with only increasing neck circumference of
more than 43 cm measured at the level of the thyroid cartilage[6]
Address for correspondence: Dr. Arne O. Budde, and Mallampati score being reproducible risk factors in the obese
Department of Anesthesiology, Penn State Milton S. Hershey Medical population[7,8] and not BMI.[4,8,9] Rosenblatt et al. demonstrated
Center, 500 University Drive, United States.
that additional examination of the upper airway anatomy can
E‑mail: abudde@hmc.psu.edu
change a previously established airway management plan in
Access this article online up to one fourth of patients with potential difficult airways.[10]
Quick Response Code:
Website:
Using a simpler method than Rosenblatt, Yamamoto et al.[11]
www.joacp.org demonstrated the usefulness of an additional airway examination.
Their study showed that indirect mirror laryngoscopy is superior
DOI:
to both the Mallampati score and Wilson risk sum score in
10.4103/0970-9185.111685 regards to positive predictive value and specificity in predicting
difficult intubation (defined as Cormack and Lehane grade III or
Journal of Anaesthesiology Clinical Pharmacology | April-June 2013 | Vol 29 | Issue 2 183
[Downloaded free from http://www.joacp.org on Wednesday, September 28, 2016, IP: 82.54.195.219]
Budde, et al.: Mirror indirect laryngoscopy
IV view).[11] The patient population in their study group had an Table 1: Wilson risk sum score 2
average weight of 55 kg; therefore, it is unknown if this method Parameter Parameter risk score
of assessing the airway is applicable to the obese population with Weight 0<90 kg
potentially difficult airways. 190-110 kg
2>110 kg
Head/Neck movement 0 above 90°
We prospectively evaluated indirect mirror laryngoscopy as 1 approx. 90° (±10°)
a predictor of difficult intubation defined as Cormack and 2 below 90°
Lehane[12] score of 3 or 4 in the obese population compared Jaw movement 0 IG* ≥5 cm; or
SLux**>0
to Samsoon and Young’s modification of the Mallampati 1 IG<5 cm and SLux=0
score,[13] Wilson risk sum score, neck circumference, and 2 IG<5 cm and SLux<0
BMI. Our hypothesis was that indirect mirror laryngoscopy Receding mandible 0 normal
1 moderate
would be superior to the traditional methods. 2 severe
Prominent incisors 0 normal
Materials and Methods 1 moderate
2 severe
*IG=Incisor gap,**SLux=Mandibular subluxation, SLux>0 demonstrates ability
The study protocol was approved by the institutional internal to sublux mandible past upper incisors, SLux=0 implies that patient can bring
review board, and written informed consent was obtained mandibular incisors equal to upper incisors, SLux<0 implies that the patient
from all participating patients. Inclusion criteria were patients cannot sublux the mandibular incisors equal to or past the upper incisors
scheduled to undergo general anesthesia with endotracheal
intubation for elective surgery, age greater than 18 years, Neck circumference was measured in the upright and
and BMI greater than 30. Exclusion criteria included seated position at the level of the thyroid cartilage using a
patients with known distortion of anatomy (such as head and standard tape measure. Neck circumference of 43 cm or
neck cancer), use of a cervical collar, obstetrical patients, greater was classified as predicting a difficult intubation.
age < 18 years, inability to sit up, and patient refusal. The Indirect mirror laryngoscopy was performed with the
indirect mirror laryngoscope used was the Welch Allyn 3.5v patient in sitting position and leaning slightly forward with
Larynx Illuminator (Welch Allyn Inc., Skaneateles Falls, slight neck extension and protrude his/her tongue. The
examiner used a 4 × 4 gauze to gently grasp the patients
NY). Measurements of neck circumference and inter‑incisor
tongue with his left hand and introduced the indirect mirror
gap were made with a standard tape measure. 60 patients were
laryngoscope into the patient’s mouth. The laryngoscope
enrolled. The authors indentified patients presenting on the day
was used to elevate the soft palate and visualize the glottis.
of surgery in the pre‑operative holding area. All pre‑operative
The view obtained from indirect mirror laryngoscopy
airway assessments were made by a single author (MD). After
was recorded as grade 1‑4 as follows: Grade 1‑ view
obtaining an informed consent, the patient was asked to sit up,
of vocal cords; grade 2‑ view of posterior commissure
and the Samsoon and Young modification of the Mallampati
only; grade 3‑ view of epiglottis only; grade 4‑ no glottis
airway classification assessment was made by instructing the structures visible. A view of grade 3‑4 was classified as
patient to maximally open their mouth and protrude their predicting difficult intubation. The primary anesthesia
tongue without phonation while the observer stood in front team performed a separate airway examination but was
of the patient. The Samsoon and Young modification of the blinded to the results of the pre‑operative examination
Mallampati airway score was recorded as follows: Grade I conducted by the investigators. Induction and intubation
for view of soft palate, uvula, and tonsillar pillars; grade II for methods were at the discretion of the primary anesthesia
view of soft palate and uvula; grade III for view of soft palate team. The view obtained upon laryngoscopy was classified
and base of the uvula; grade IV for no view of soft palate at according to Cormack and Lehane as follows: Grade 1‑ full
all. Grade III and IV were classified as predicting difficult view of glottis; grade 2‑ only posterior commissure visible;
intubation (defined as grade III or IV view by Cormack and grade 3‑ only epiglottis visible; grade 4‑ no glottic structure
Lehane classification). The components of the Wilson risk visible. Grade 3‑4 were classified as difficult laryngoscopy.
sum score were then measured with the patient in the sitting
position. Wilson risk sum score consists of measurements of Demographical data is expressed as mean and standard
head and neck movement, jaw movement, presence and degree deviation (SD) or median and range as appropriate. Each
of receding mandible, the presence of prominent maxillary method was analyzed with the Wilcoxon Ranks Sum
incisors, and body weight. Each variable received a score of Test, and Receiver Operator Characteristics (ROC)
0‑2 [Table 1] for a possible sum score of 0-10. A total score curves were constructed for each predicting method. All
of two or greater is classified as predicting difficult intubation. ROC curves were compared to the indirect laryngoscopy
184 Journal of Anaesthesiology Clinical Pharmacology | April-June 2013 | Vol 29 | Issue 2
[Downloaded free from http://www.joacp.org on Wednesday, September 28, 2016, IP: 82.54.195.219]
Budde, et al.: Mirror indirect laryngoscopy
ROC curve for statistical significance; alpha was set at
0.05. The statistical analysis was done using JMP 9.0
(SAS Institute Inc. Cary, NC), the power analysis with
PASS 11 (NCSS, Kaysville, UT), and the ROC curves
comparison with Medcalc 12.2.1.0 (Medcalc Software,
Mariakerke, Belgium).
Results
Indirect mirror laryngoscopy was attempted in all 60 patients;
however, 8 (13.3%) patients had an excessive gag reflex,
making examination of the larynx impossible and were
excluded from the study. Direct laryngoscopy was performed
with a Macintosh blade in all but three patients. In all of these Figure 1: Scatterplot: Direct laryngoscopy vs. predicting methodologies
three patients, a Miller blade was used resulting in a good view
of the larynx with subsequent easy intubation. Eight out of the Table 2: Patient characteristics–mean (Standard
52 patients (15.4%) who underwent direct laryngoscopy had Deviation) or median (Range) by laryngoscopy difficulty
a Cormack and Lehane grade 3 or 4 view and were classified using the cormack lehane scale
as “difficult.” Patient characteristics can be seen in Table 2. Patient All (n=52) “Easy” “Difficult”
characteristics (n=44) (n=8)
grade 1, 2 grade 3, 4
When analyzed independently, no method showed that view view
it could predict a difficult airway at the P < 0.05 level. Weight 115.5 kg 114.5 kg 121.1 kg
Indirect mirror laryngoscopy was the closest, with a (27.0) (27.4) (25.4)
Height 170.2 cm 168.8 cm 178.0 cm
P value = 0.0503 [Table 3].
(10.4) (10.2) (9.4)
BMI 39.4 kg/m2 39.8 kg/m2 37.2 kg/m2
We also constructed ROC curves for all methods and calculated (8.2) (8.7) (5.0)
their respective areas under the curve. Again, the best method Neck circumference 43.5 cm (5.0) 43.1 cm (5.0) 45.8 cm
was indirect mirror laryngoscopy, followed by the Mallampati (4.5)
Wilson risk score 2 (0,5) 2 (0,5) 2.5 (1,5)
score and the neck circumference measurement [Table 3].
Mallampati score 2 (1,4) 2 (1,4) 3 (2,3)
When we compared indirect mirror laryngoscopy against Mirror laryngoscopy 2 (1,4) 2 (1,4) 2.5 (1,4)
all the other methods using AUC [Table 4], we determined view
that there were no statistically significant differences between BMI=Body mass index
them, although the largest difference (indirect Laryngoscopy
vs. BMI at 0.15) showed a tendency towards significance.
Table 3: Relationship between methodology and
Results are also displayed in a scatterbox [Figure 1].
laryngoscopic view by wilcoxon ranks sum test (Chi2
approximation)
Discussion Source Chi2 P Value AUC 95% CI
BMI 0.3565 0.5504 0.51 0.37, 0.66
Wilson 2.7555 0.0969 0.59 0.45, 0.72
The literature is rich with studies and meta‑analyses attempting
Neck 2.7752 0.0957 0.64 0.49, 0.76
to determine the best single method or combination of methods
Mallampati 2.7837 0.0952 0.64 0.50, 0.77
to aid the anesthesiologist in predicting difficult intubation. The Indirect Laryngoscopy 3.8324 0.0503 0.67 0.53, 0.79
rate of difficult laryngoscopy (Cormack and Lehanegrade 3 AUC= Area Under the Curve; CI= Confidence Interval
or 4 view) in patients with apparently normal airways was
determined by two recent meta‑analysis to be 5.8%.[14] It was Table 4: Comparison between AUC. Differences with
shown that tests such as Mallampati score, Wilson Risk score, respect to indirect laryngoscopy
thyromental distance, sternomental distance, and mouth opening Method Difference 95% CI Difference Z Value P Value
offered poor to moderate sensitivity (20‑62%) and moderate BMI 0.15 ‑0.18, 0.44 1.92 0.055
to fair specificity (82‑97%). The rate of difficult laryngoscopy Wilson 0.08 ‑0.23, 0.39 0.57 0.570
in the obese population has been well documented to be much Neck 0.03 ‑0.28, 0.34 0.21 0.837
higher than the non‑obese, ranging from 12‑15.8%,[4,5,8] although Mallampati 0.03 ‑0.28, 0.34 0.19 0.852
multiple studies[5,8,9] have demonstrated that BMI per se does CI= Confidence interval
Journal of Anaesthesiology Clinical Pharmacology | April-June 2013 | Vol 29 | Issue 2 185
[Downloaded free from http://www.joacp.org on Wednesday, September 28, 2016, IP: 82.54.195.219]
Budde, et al.: Mirror indirect laryngoscopy
not offer any predictive value for difficult intubation. High Acknowledgement
Mallampati score and large neck circumference have probably
been the best single risk factor for difficult intubation in the Funding through departmental research starter grant.
obese.,[5,7,8] Ezri et al.[15] used ultrasound to quantify neck soft
tissue at the level of the vocal cords and suprasternal notch and References
demonstrated that, in an obese population, the best predictor of
difficult intubation was distribution of fat in these areas. While 1. Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B,
clearly a useful technique, the availability and time required Freiberger D, et al. A clinical sign to predict difficult
tracheal intubation: A prospective study. Can Anaesth Soc J
performing this examination may be prohibitive to many
1985;32:429‑34.
anesthesiologists. Rosenblatt et al. performed pre‑operative 2. Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting
endoscopic airway examination (PEAE) with a fiberoptic difficult intubation. Br J Anaesth 1988;61:211‑6.
bronchoscope in patients with potentially difficult airways due 3. Yentis SM. Predicting difficult intubation‑worthwhile exercise or
pointless itual? Anaesthesia 2002;57:105‑9.
to anatomical abnormalities.[10] PEAE resulted in change of
4. Ezri T, Medalion B, Weisenberg M, Szmuk P, Warters RD, Charuzi I.
a previously established airway management plan in 26% Increased body mass index per se is not a predictor of difficult
of the study patients. While a change in plan in one of four laryngoscopy. Can J Anaesth 2003;50:179‑83.
patients is an impressive result, PEAE is a relatively complex 5. Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult
intubation in apparently normal patients: A meta‑analysis of bedside
and costly method requiring the utilization of a fiberoptic
screening test performance. Anesthesiology 2005;103:429‑37.
bronchoscope for every patient. Indirect laryngoscopy is a 6. Gonzalez H, Minville V, Delanoue K, Mazerolles M, Concina D,
simple technique used frequently in otolaryngology to assess Fourcade O. The importance of increased neck circumference
the larynx and upper airway. Yamamoto et al. demonstrated to intubation difficulties in obese patients. Anesth Analg
2008;106:1132‑6.
the applicability of this technique in the pre‑operative airway
7. Brodsky JB, Lemmens HJ, Brock‑Utne JG, Vierra M, Saidman LJ.
assessment.[11] Our experience is that the technique can Morbid obesity and tracheal intubation. Anesth Analg
be learned rather quickly, and comfort with the device was 2002;94:732‑6.
obtained after approximately 10‑15 uses of the device. The 8. Juvin P, Lavaut E, Dupont H, Lefevre P, Demetriou M, Dumoulin JL,
et al. Difficult tracheal intubation is more common in obese than
examination takes less than 30 seconds, and the device can be
in lean patients. Anesth Analg 2003;97:595‑600.
quickly cleaned in the same way as the laryngoscope blades. 9. Lundstrøm LH, Møller AM, Rosenstock C, Astrup G, Wetterslev J.
In the current study, mirror indirect laryngoscopy was the only High body mass index is a weak predictor for difficult and failed
method that had a tendency towards predicting whether an tracheal intubation. Anesthesiology 2009;110:266‑74.
10. Rosenblatt W, Ianus AI, Sukhupragarn W, Fickenscher A,
airway will be difficult or not. As had been reported previously,
Sasaki C. Preoperative endoscopic airway examination (PEAE)
BMI had the poorest correlation with difficult intubation and provides superior airway information and may reduce the use of
when compared with indirect laryngoscopy, had a tendency unnecessary awake intubation. Anesth Analg 2011;112:602‑7.
towards being significantly worse. We experienced a 13.3% 11. Yamamoto K, Tsubokawa T, Shibata K, Ohmura S, Nitta S,
Kobayashi T. Predicting difficult intubation with indirect
rate of excessive gag reflex, which is consistent with the 15%
laryngoscopy. Anesthesiology 1997;86:316‑21.
reported by Yamamoto et al.[11] The use of local anesthesia 12. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics.
may have reduced this rate. Anaesthesia 1984;39:1105‑11.
13. Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective
This study was designed as a pilot study to determine study Anaesthesia 1987;42:487‑90.
14. Lundstrøm LH, Vester‑Andersen M, Møller AM, Charuluxananan S,
if indirect laryngoscopy might prove useful in the obese L’hermite J, Wetterslev J. Danish Anaesthesia Database.
population. Our results are consistent with previous Poor prognostic value of the modified Mallampati score:
studies, which have demonstrated that no one of the A meta‑analysis involving177,088 patients. Br J Anaesth
commonly performed tests alone has proven to be adequate 2011;107:659‑67.
15. Ezri T, Gewürtz G, Sessler DI, Medalion B, Szmuk P, Hagberg C,
in predicting difficult intubation in the obese population. et al. Prediction of difficult laryngoscopy in obese patients by
Indirect mirror laryngoscopy is a relatively simple method of ultrasound quantification of anterior neck soft tissue. Anaesthesia
assessing airway anatomy with a tendency towards statistical 2003;58:1111‑4.
significance in predicting difficult laryngoscopy. A larger How to cite this article: Budde AO, Desciak M, Reddy V, Falcucci OA, Vaida
sample size will be required in further investigations to SJ, Pott LM. The prediction of difficult intubation in obese patients using mirror
indirect laryngoscopy: A prospective pilot study. J Anaesthesiol Clin Pharmacol
proof our hypothesis that mirror indirect laryngoscopy 2013;29:183-6.
can be a useful test for pre‑operative airway assessment Source of Support: Departmental research starter grant., Conflict of Interest:
of obese patients. None declared.
186 Journal of Anaesthesiology Clinical Pharmacology | April-June 2013 | Vol 29 | Issue 2
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Amputee Rehabilitation and Preprosthetic CareDocument17 pagesAmputee Rehabilitation and Preprosthetic CareJessica Sepúlveda SalasNo ratings yet
- OET Writing Test 6Document3 pagesOET Writing Test 6LOTSOFTESTS67% (3)
- PK Urine Practicum 1 KBK Sem 6 2016 ManualDocument38 pagesPK Urine Practicum 1 KBK Sem 6 2016 Manualanindita fauziahNo ratings yet
- SW3 007 Excision of Skin Lesions Under Local Anaesthetic 07.21 v6Document8 pagesSW3 007 Excision of Skin Lesions Under Local Anaesthetic 07.21 v6anindita fauziahNo ratings yet
- Endoscopic Excision of Benign Tumors in The Forehead and BrowDocument4 pagesEndoscopic Excision of Benign Tumors in The Forehead and Browanindita fauziahNo ratings yet
- Acute Care 30: Glasgow Coma Scale-Adult, Pediatric, Infant: Eye OpeningDocument2 pagesAcute Care 30: Glasgow Coma Scale-Adult, Pediatric, Infant: Eye OpeningOkdiantoRahmanGastiNo ratings yet
- DapusDocument3 pagesDapusanindita fauziahNo ratings yet
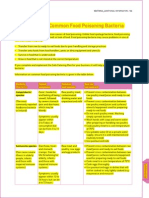
- Common Food Poisoning BacteriaDocument3 pagesCommon Food Poisoning BacteriaYani NyiikNo ratings yet
- Fraktur MandibulaDocument3 pagesFraktur Mandibulaanindita fauziahNo ratings yet
- 1 2018Document48 pages1 2018Lizz22No ratings yet
- Literature ReviewDocument4 pagesLiterature Reviewapi-548908089No ratings yet
- Multiple PregnancyDocument21 pagesMultiple PregnancyMazlina Maidin100% (1)
- English Books BibliotekaDocument10 pagesEnglish Books BibliotekahazeemmegahedNo ratings yet
- Nursing Care Plan EndocarditisDocument2 pagesNursing Care Plan EndocarditisSam TullyNo ratings yet
- Physical Inactivity: Aging Men Hypertension Smoker ObesityDocument1 pagePhysical Inactivity: Aging Men Hypertension Smoker ObesityKEn PilapilNo ratings yet
- Patient EducationDocument5 pagesPatient EducationRS Sentra Medika CisalakNo ratings yet
- Week 7Document33 pagesWeek 7Jakmensar Dewantara Siagian0% (2)
- Rawatan: Kecelaruan Tingkah Laku. Kuala Lumpur: PTS Profesional PublisherDocument2 pagesRawatan: Kecelaruan Tingkah Laku. Kuala Lumpur: PTS Profesional PublisherNeng Azreen ZGNo ratings yet
- Diabetes Foot Examination FormDocument17 pagesDiabetes Foot Examination FormJANUAR RIZQINo ratings yet
- Timely Filing Limit Guide Part 2Document12 pagesTimely Filing Limit Guide Part 2NandhaNo ratings yet
- Survival Guide 08Document172 pagesSurvival Guide 08Kavirm35No ratings yet
- What Hartmann'S Solution Is and What It Is Used For?Document4 pagesWhat Hartmann'S Solution Is and What It Is Used For?YudhaNo ratings yet
- Priority Research Questions For TB/HIV in HIV-prevalent and Resource-Limited SettingsDocument64 pagesPriority Research Questions For TB/HIV in HIV-prevalent and Resource-Limited SettingsGideon IraborNo ratings yet
- Pathophysiology of Varicose Vein - Chronic Venous InsufficiencyDocument31 pagesPathophysiology of Varicose Vein - Chronic Venous InsufficiencyDavid Christian100% (1)
- Why I Want To Become A PhysiotherapistDocument8 pagesWhy I Want To Become A PhysiotherapistgggghcNo ratings yet
- Author: Tuazon, Josefina A. RN, BSN, MN, DRPH: Learning Objective 1: Appreciate OneDocument6 pagesAuthor: Tuazon, Josefina A. RN, BSN, MN, DRPH: Learning Objective 1: Appreciate OneJohn Robert PescadorNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleShahrukh ali khanNo ratings yet
- 1 Lecture 1Document75 pages1 Lecture 1Hoven MacasinagNo ratings yet
- CotrimozaxoleDocument3 pagesCotrimozaxoleDane CunananNo ratings yet
- List of Accredited Ambulatory Surgical Clinics As of September 30, 2020Document11 pagesList of Accredited Ambulatory Surgical Clinics As of September 30, 2020Glomarie Alyssa RacelisNo ratings yet
- Copd 8 439Document13 pagesCopd 8 439alNo ratings yet
- Fortune Magazine Article On Cancer 2004Document12 pagesFortune Magazine Article On Cancer 2004Azaz QureshiNo ratings yet
- DocDocument19 pagesDocapi-325122079No ratings yet
- Telangana State Paramedical Board: Top Priority ExaminationsDocument21 pagesTelangana State Paramedical Board: Top Priority ExaminationsManojNo ratings yet
- Burning Mouth Disease A Guide For Patients (Isaäc Van Der Waal)Document50 pagesBurning Mouth Disease A Guide For Patients (Isaäc Van Der Waal)x9mg58srbyNo ratings yet
- The Prevalence and Risk Factors of DysmenorrheaDocument10 pagesThe Prevalence and Risk Factors of DysmenorrheaMaesaNo ratings yet
- Typology of Nursing Problems in Family Nursing PracticeDocument4 pagesTypology of Nursing Problems in Family Nursing PracticeLeah Abdul KabibNo ratings yet