Professional Documents
Culture Documents
Interpretare Eucast CLSI Yeasts
Uploaded by
Geoemilia1Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Interpretare Eucast CLSI Yeasts
Uploaded by
Geoemilia1Copyright:
Available Formats
EUCAST-and CLSI potency Page 1 / 4 - Document: 3.15.
0
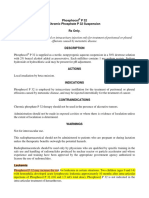
NEO-SENSITABS™
Interpretation Zones and MIC Yeasts (CLSI's M44-A2 Method of Diffusion
Breakpoints according to CLSI on Agar)
Only Fluconazole and Voriconazole are included in the M44-A guideline from CLSI (formerly NCCLS)(1)
and interpretation zones are only available for Fluconazole so far. When MIC breakpoints are available
from CLSI (2) they are used in the table below.
Table 13.5-1 Interpretation for Yeasts
Mueller-Hinton Glucose Methylene Blue agar. Inoculum McFarland 0.5 undiluted. Incubation at 35 °C 2
°C ambient air for 20-24 hours. MICs according to M27-S3 (2007).
Zone diameter Break-points
in mm MIC µg/ml
NEO-SENSITABS POTENCY CODE S I R S R
Amphotericin B 10 µg AMPHO 15 14-10 < 10 1 2
Caspofungin *) (24) 5 µg CASP5
C. albicans, C. tropicalis 17 16-15 14 0.25 1
C. parapsilosis,* C. guilliermondii 13 12-11 10 2 >2
C. glabrata, C. krusei 16 - - 0.5 -
Fluconazole **) (27) 25 µg FLUCZ
C. albicans, C. tropicalis, C. parapsilosis 17 16-14 13 2 8
C. glabrata - 15 14 32 64
(SDD) (SDD)
Itraconazole (11) 10 µg ITRAC 23 22-14 13 0.12 > 0.5
(SDD)
Ketoconazole 15 µg KETOC 28 27-21 20 0.12 0.5
Posaconazole (9,12) 5 µg POSAC 17 16-14 13 1 >2
(SDD)
Voriconazole (23) 1 µg VOR.1
C. albicans, C. tropicalis, C. parapsilosis 17 16-15 14 0.12 1
C. krusei 15 14-13 12 0.5 2
C. glabrata 16 - 15 0.5 > 0.5
*) Tentative. There is cross-resistance between Caspofungin and the other echinocandins:
Anidulafungin and Micafungin (19).
**) C. krusei should be reported as resistant to Fluconazole (no matter the zone).
For further information on Susceptibility Testing of Yeasts, see Neo-Sensitabs User's Guide.
Table 13.5-2 Mold Disk Diffusion Testing (14, 17,21)
Mueller-Hinton Plain. Incubation for 16-24 hours (zygomycetes), 24 hours (Aspergillus),
48 hours (other spp.). Temperature: 35-37°C
Inoculum:
Prepare a suspension of sporulating colonies in 0.85% saline, add 1 drop of Tween 20. Allow heavy
particles to settle for 3-5 minutes and the upper suspension is treated for 15 seconds in a vortex mixer.
The density of the suspension is read on a spectrophotometer at 530 mm wave length and the optical
density adjusted at 0.09 to 0.13 for Aspergillus.
Revision date: 03.12.13 Establish date: 01.08.07
Rev./Appr. by: tp / TP Establish by: JBC
Replaces date: 24.01.13 Revision no.: 12
EUCAST-and CLSI potency Page 2 / 4 - Document: 3.15.0
NEO-SENSITABS™
Interpretation Zones and MIC Yeasts (CLSI's M44-A2 Method of Diffusion
Breakpoints according to CLSI on Agar)
Zone diameter Break-points
in mm MIC µg/ml
NEO-SENSITABS POTENCY CODE S I R S R
Amphotericin B 10 µg AMPHO 15 - - 1 -
(zygomycetes only)
Caspofungin 5 µg CASP5 17 - - 1 -
Itraconazole 10 µg ITRAC 17 - - 1 ≥2
Posaconazole 5 µg POSAC 23 - - 0.25 ≥ 0.5
Voriconazole 1 µg VOR.1 17 - - 1 ≥2
Note: The base medium should not be supplemented with neither 2% glucose nor 0.5% methylene blue
dye.
Itraconazole susceptible strains should be reported as susceptible to both, Posaconazole and
Voriconazole.
Interpretation table for Local treatment
In local treatment of fungal infections, a high concentration of antifungal is placed at site of the infection. Consequently
other MIC breakpoints and zone interpretations should be used in those cases.
Local Treatment
MH Glucose Methylene Blue Agar or Shadomy
McFarland 0.5 inoculum
Susceptible 20 mm 15 mm 10 mm
Intermediate 12-19 mm 10-14 mm -
Resistant 11 mm no zone no zone
Ciclopirox Natamycin Griseofulvin
Clotrimazole Nystatin
Econazole Itraconazole
Fluconazole
Isoconazole
Ketoconazole
Miconazole
Tioconazole
Terbinafine
Fluorocytosine cannot be tested on MH-agar (antagonists), but has to be tested on Shadomy agar or
similar.
Revision date: 03.12.13 Establish date: 01.08.07
Rev./Appr. by: tp / TP Establish by: JBC
Replaces date: 24.01.13 Revision no.: 12
EUCAST-and CLSI potency Page 3 / 4 - Document: 3.15.0
NEO-SENSITABS™
Interpretation Zones and MIC Yeasts (CLSI's M44-A2 Method of Diffusion
Breakpoints according to CLSI on Agar)
Table 13.5-3 Quality Control Zone Diameters (mm) Ranges
Mueller-Hinton Glucose Methylene Blue agar. Inoculum McFarland 0.5 undiluted. Incubation
at 35 °C 2 °C for 20-24 hours.
Zone diameter in mm
C. albicans C. parapsilosis C. krusei
NEO-SENSITABS POTENCY CODE ATCC 90028 ATCC 22019 ATCC 6258
Amphotericin B 10 µg AMPHO 20-27 22-29 18-25
Fluconazole 25 µg FLUCZ 28-39 22-33 -
Itraconazole 10 µg ITRAC 21-30 19-26 16-22
Ketoconazole 15 µg KETOC 31-42 35-45 22-29
Voriconazole 1 µg VOR.1 31-42 28-37 23-31
Caspofungin 5 µg CASP5 15-22 13-23 16-22
Posaconazole 5 µg POSAC 24-34 25-36 23-31
Carrillo-Munoz et al (30) determined Posaconazole susceptibility of clinical yeast isolates with Neo-
Sensitabs and a microdilution method. Complete agreement between Posaconazole Neo-Sensitabs and
the microdilution was 92.3 % after 24 hours incubation. The authors conclude that the Agar Diffusion
with Posaconazole Neo-sensitabs can improve Posaconazole susceptibility testing due to its excellent
correlation and reduced percentage of disagreements in comparison with microdilution testing.
References:
1) NCCLS. Methods for Antifungal Disk Diffusion Susceptibility Testing on Yeasts. Approved Guideline
M44-A2, 2008.
2) NCCLS. Reference Methods for Broth Dilution Antifungal Susceptibility Testing of yeasts. Approved
Standard,
2nd Ed. M27-A2, 2002.
3) Vandenbossche I. et al: Susceptibility testing of Fluconazole by the NCCLS broth macrodilution
method. E-Test and Disk diffusion for application in the routine laboratory. J. Clin. Microbiol, 40,
918-921, 2002.
4) Pfaller M.A. et al: Evaluation of the NCCLS M44-P Disk diffusion method for determining Fluconazole
susceptibility of 276 clinical isolates of Cryptococcus neoformans. ICAAC 2003, presentation M-
1204.
5) Barry A. et al: Quality Control for Fluconazole disk susceptibility tests on Mueller-Hinton Agar with
glucose and methylene blue. J.Clin.Microbiol., 41, 3410-12, 2003.
6) Rementeria A. et al: Utility of Neo-S. tablets of Fluconazole and Voriconazole for in vitro
susceptibility testing of Candida spp. with the NCCLS M44-P method of diffusion on agar. VII
Congress Mycology. Salamanca, July 2004 (Spanish).
7) Espinel-Ingroff A. et al: Correlation between Neo-S. tablets on 3 media, NCCLS reference disk
diffusion and broth microdilution methods for testing Candida spp. and Cryptococcus neoformans
with Fluconazole and Voriconazole. Abstract, ECCMID 2005.
8) Espinel-Ingroff A, Canton E.: Comparison of 3 antifungal susceptibility methods for testing Candida
spp. & Cryptococcus neoformans with Caspofungin (CAS) and Amphotericin B (AMB). Abstract,
presentation M-1604, 45th ICAAC 2005.
9) Sims C.R. et al: Correlation between microdilution, E-test and disk diffusion methods for antifungal
susceptibility testing of Posaconazole against Candida spp. J. Clin. Microbiol., 44, 2105-08, 2006.
10) Brown S. et al: Q.C. limits for Posaconazole disk susceptibility tests on MH agar with glucose and
methylene blue. J. Clin. Microbiol., 45, 222-23, 2007.
11) Espinel-Ingroff A. et al: Correlation of Neo-Sensitabs tablet diffusion assay results on 3 different
agar media with CLSI broth microdilution M27-A2 and disk diffusion M44-A results for testing
Revision date: 03.12.13 Establish date: 01.08.07
Rev./Appr. by: tp / TP Establish by: JBC
Replaces date: 24.01.13 Revision no.: 12
EUCAST-and CLSI potency Page 4 / 4 - Document: 3.15.0
NEO-SENSITABS™
Interpretation Zones and MIC Yeasts (CLSI's M44-A2 Method of Diffusion
Breakpoints according to CLSI on Agar)
susceptibilities of Candida spp. and Cryptococcus neoformans to Amphothericin B, Caspofungin,
Fluconazole, Itraconazole and Voriconazole. J. Clin. Microbiol, 45, 858-64, 2007.
12) Diekema D.J. et al: Evaluation of E-test and disk diffusion methods with broth microdilution
antifungal susceptibility testing of Posaconazole against clinical isolates of Candida. J. Clin.
Microbiol., 2007 (in press).
13) Carrillo-Muñoz A.J. et al: Acitivity of Caspofungin and Voriconazole against clinical isolates of
Candida and other medically important yeasts by the CLSI M44A disk diffusion method with Neo-
Sensitabs tablets. Chemotherapy, 54 (1) 38-42, 2008.
14) Espinel-Ingroff A. et al: Multicenter evaluation of a new disk agar diffusion method for susceptibility
testing of filamentous fungi with Voriconazole, Posaconazole, Itraconazole, Amphothericin B and
Caspofungin. J. Clin. Microbiol., 45, 1811-20, 2007.
15) Espinel-Ingroff A.: Standardized disk diffusion method for yeasts. Clin. Microbiol. Newsl., 29, 97-
100, 2007.
16) Carrillo-Muñoz A. J. et al: Antifungal activity in vitro of Posaconazole. Method of diffusion on agar
(Neo-Sensitabs) based on document M44-A, against yeast. III. Forum Micologico, Dec 15 th 2007,
Alicante, Spain (spanish).
17) Espinel Ingroff A. et al: Comparison of Neo-S tablet diffusion assay with CLSI broth microdilution
M38-A and disk diffusion methods for testing susceptibility filamentous fungi with Ampothericin B,
Caspofungin, Itraconazole, Posaconazole and Voriconazole. J. Clin. Microbial. 46, 1793-1803, 2008.
18) Duran-Valle M T et al: Resistance to Voriconazole and/or Fluconazole in yeast isolated in a Madrid
hospital (2005-2007) etc. XII Congress SEIMC, presentation 33, Madrid, May 2008.
19) Pfaller M. A. et al: Correlation of MIC with outcome for Candida spp. tested against Caspofungin,
Amidulafungin and Micafungin: analysis and proposal for interpretative MIC breakpoints. JCM 46,
2620-2629, 2008.
20) Pfaller M. A. et al: Wild-type MIC distribution and epidemiological cutoff values for Aspergillus
fumigatus and 3 triazoles as determined by the CLSI both microdilution methods. J. Clin. Microbiol.
47, 3142-46, 2009.
21) M51-A Method for antifungal disk diffusion susceptibility testing of filamentous fungi approved
guideline. CLSI 2009.
22) Pfaller M. et al: Clinical breakpoints for the Echinocandins and Candida, revisited. Presentation M-
369, 50th ICAAC, Sept. 2010.
23) Pfaller M. et al: Clinical breakpoints for Voriconazole and Candida spp. revisited: Review of
microbiologic, molecular, pharmacodynamic and clinical data as they pertain to the development of
species–specific interpretative criteria. Diagn. Microbiol. Infect. Dis. 70, 330-343, 2011.
24) Pfaller M. et al: Clinical breakpoints for Echinocandins and Candida revisited: Integration of
molecular, clinical and microbiological data to arrive at species-specific interpretative criteria. Drug
Resistance Updates. 14, 164-176, 2011.
25) Ochiuzzi M. E et al: Correlation of E-test and Neo-Sensitabs diffusion assays on Mueller-Hinton-
methylene blue agar, with broth microdilution reference method (CLSI-M27-A2) for testing
susceptibilities of Cryptococcus neoformans to Amphotericin B and Fluconazole. Med. Mycology. 48,
893-896, 2010.
26) Carrillo-Muñoz A. J. et al: Antifungal activity of Posaconazole against Candida spp. and non-Candida
clinical yeast isolates. Rev. Esp. Quimioter. 23, 122-125, 2010.
27) Nweze E. I et al: Agar-based disk diffusion assay for susceptibility testing of Dermatophytes. J. Clin.
Microbiol. 48, 3750-52, 2010.
28) Pfaller M. A et al: Wild-type MIC distributions, epidemiological cutoff values and species-specific
clinical breakpoints for Fluconazole and Candida: Time for harmonization of CLSI and EUCAST broth
microdilution methods. Drug Resistance Updates. 13, 180-195, 2010.
29) Pfaller M. A et al: Echinocandin and triazole antifungal susceptibility profiles for Candida spp.,
Cryptococcus neoformans and Asp. fumigatus; application of new CLSI clinical breakpoints and
epidemiologic cutoff values to characterize resistance in SENTRY Antimicrobial Surveillance Program
(2009). Diag. Microbiol. Infect. Dis. 69, 45-50, 2011.
30) Carrillo-Munoz AJ et al: Posaconazole susceptibility of clinical yeast isolates determined by an agar
diffusion and microdilution method. Int. J. Antimicr. Agents. 37, 271-273, 2011.
Revision date: 03.12.13 Establish date: 01.08.07
Rev./Appr. by: tp / TP Establish by: JBC
Replaces date: 24.01.13 Revision no.: 12
You might also like
- Music Business Chapter 9 Music PublishingDocument27 pagesMusic Business Chapter 9 Music Publishingcmk97No ratings yet
- EPS: Electric Power Steering Components & ModesDocument9 pagesEPS: Electric Power Steering Components & ModesTilahun Worku100% (1)
- Fungal Cultivation and Identification (Side Notes)Document8 pagesFungal Cultivation and Identification (Side Notes)Reca Marie FRIAS100% (1)
- Bethesda 2001: Ma. Minda Luz M. Manuguid, M.DDocument75 pagesBethesda 2001: Ma. Minda Luz M. Manuguid, M.Djulo_05100% (1)
- Gram-Negative Diplococci Characteristics and Pathogenic SpeciesDocument33 pagesGram-Negative Diplococci Characteristics and Pathogenic SpeciesShuler0071No ratings yet
- Mycology Lab ProjectionDocument7 pagesMycology Lab Projectionapi-3700579100% (3)
- Cortisol ARCDocument7 pagesCortisol ARCilc67123100% (1)
- Questions Answers: Legarda vs. Saleeby: The Real Purpose of The Torrens System Is To Quiet Title To Land To Put A StopDocument19 pagesQuestions Answers: Legarda vs. Saleeby: The Real Purpose of The Torrens System Is To Quiet Title To Land To Put A StopNico RoaNo ratings yet
- Immunofluorescence Handbook 1601971Document80 pagesImmunofluorescence Handbook 1601971Ray KuoNo ratings yet
- SpermogramaDocument13 pagesSpermogramaGeoemilia1No ratings yet
- CHAPTER 8 The Rise of Instrumental Music - 141-152Document8 pagesCHAPTER 8 The Rise of Instrumental Music - 141-152Aleksandre Roderick-LorenzNo ratings yet
- Camera de Numarat Improved NeubauerDocument4 pagesCamera de Numarat Improved NeubauerGeoemilia1No ratings yet
- Interpretive standards and control zone diameters for antimicrobial susceptibility testingDocument16 pagesInterpretive standards and control zone diameters for antimicrobial susceptibility testingGeoemilia180% (5)
- Distinguishing Reference Intervals and Clinical Decision LimitsDocument13 pagesDistinguishing Reference Intervals and Clinical Decision LimitsJoana BarbosaNo ratings yet
- Body in Movement - WorkshopDocument8 pagesBody in Movement - WorkshopAndrew CareyNo ratings yet
- Jurnal SinusitisDocument49 pagesJurnal SinusitisAramanda Dian100% (1)
- Co2 LDocument3 pagesCo2 LARIF AHAMMED P100% (1)
- Sediment UrinarDocument69 pagesSediment UrinarGeorge CîciuNo ratings yet
- Unit DNI Candidate Guidance v51612018191423Document14 pagesUnit DNI Candidate Guidance v51612018191423Carla Baraybar100% (1)
- CLSI Antifungical Susceptibility Test UpdatedDocument34 pagesCLSI Antifungical Susceptibility Test UpdatedSofiaMarmolejoNo ratings yet
- Microbiologie Curs FrotiuriDocument17 pagesMicrobiologie Curs FrotiuriIoana Manole100% (2)
- Cerebrospinal Fluid: By: Raynhier G. Constantino, RMTDocument53 pagesCerebrospinal Fluid: By: Raynhier G. Constantino, RMTJaellah MatawaNo ratings yet
- IMMUNOHISTOCHEMISTRY STEPSDocument96 pagesIMMUNOHISTOCHEMISTRY STEPSAdarshBijapurNo ratings yet
- 5 Part CBC ReportDocument1 page5 Part CBC Reportalagom2001No ratings yet
- GUM/HIV Microscopy Stains and FindingsDocument2 pagesGUM/HIV Microscopy Stains and Findingswavezone113No ratings yet
- The Urinary Sediment by UriSed Technology G.B. Fogazzi - G. GarigaliDocument123 pagesThe Urinary Sediment by UriSed Technology G.B. Fogazzi - G. GarigaliALMA ROSA PEREZ MORALES100% (2)
- VitekDocument35 pagesVitektamrinNo ratings yet
- 1 Cervical and Vaginal CytologyDocument63 pages1 Cervical and Vaginal Cytologynanxtoyah100% (1)
- Hands-On Learning Active ProcessDocument3 pagesHands-On Learning Active Processjackielyn75% (8)
- Acinetobacter baumannii: An Update on an Emerging Multidrug Resistant PathogenDocument12 pagesAcinetobacter baumannii: An Update on an Emerging Multidrug Resistant PathogenGIST (Gujarat Institute of Science & Technology)No ratings yet
- EsblDocument159 pagesEsblArunagiri Subramanian100% (2)
- Contributions To The Anatomy of Ruscus Aculeatus L Liliaceaecontributii To The PDFDocument5 pagesContributions To The Anatomy of Ruscus Aculeatus L Liliaceaecontributii To The PDFArdian SyahputraNo ratings yet
- VIRUSOLOGIE: CARACTERE GENERALE ALE VIRUSURILORDocument24 pagesVIRUSOLOGIE: CARACTERE GENERALE ALE VIRUSURILORMonzer AchtarNo ratings yet
- MM Ous Microscan Eucast Gram Pos Ds 11 2013-01349656 PDFDocument2 pagesMM Ous Microscan Eucast Gram Pos Ds 11 2013-01349656 PDFsazunaxNo ratings yet
- Microbiology: Pathogenic Gram-Positive Cocci (Streptococcus)Document26 pagesMicrobiology: Pathogenic Gram-Positive Cocci (Streptococcus)Shuler0071No ratings yet
- Bergy's Manual Identification Flow ChartDocument8 pagesBergy's Manual Identification Flow ChartOmid Nilchi Zadeh RahbarNo ratings yet
- Wiley - Roitt's Essential Immunology, 12th Edition - 978!1!118-23287-3Document3 pagesWiley - Roitt's Essential Immunology, 12th Edition - 978!1!118-23287-3Muhammad RameezNo ratings yet
- Diagnostic CarmenDocument67 pagesDiagnostic CarmenCattleya KlfNo ratings yet
- Monolisa HCV Ag-Ac UltraDocument4 pagesMonolisa HCV Ag-Ac UltraSantiagoAFNo ratings yet
- EnterobacteriaceaeDocument107 pagesEnterobacteriaceaeClaire Gonzales100% (1)
- Fisa Control Intern AntibioticeDocument1 pageFisa Control Intern AntibioticeGeoemilia1No ratings yet
- Non-Fermentative Gram-Negative Bacteria IdentificationDocument56 pagesNon-Fermentative Gram-Negative Bacteria IdentificationAbiola Olumuyiwa OlaitanNo ratings yet
- PreciControl HbA1c Path.05854237001.V4.EnDocument2 pagesPreciControl HbA1c Path.05854237001.V4.EnARIF AHAMMED PNo ratings yet
- Laceanu Rodica CAb, CAf, My, UDocument2 pagesLaceanu Rodica CAb, CAf, My, UrlaceanuNo ratings yet
- FlowcitometrieDocument49 pagesFlowcitometrieelenaelena96No ratings yet
- Lab Examination Parasitology UnibrawDocument40 pagesLab Examination Parasitology UnibrawFaiz Fort Knox80% (5)
- Complete Blood Count Analyzer Maintenance and CalibrationDocument3 pagesComplete Blood Count Analyzer Maintenance and CalibrationMary Grace CuevaNo ratings yet
- VIRUSOLOGY: KEY ASPECTS OF VIRUS STRUCTURE AND REPLICATIONDocument27 pagesVIRUSOLOGY: KEY ASPECTS OF VIRUS STRUCTURE AND REPLICATIONSanzianaGoga100% (1)
- CURS DE PROTEOMICA FUNCTIONALA SI CLINICADocument424 pagesCURS DE PROTEOMICA FUNCTIONALA SI CLINICAElena AsaveiNo ratings yet
- CitologieDocument14 pagesCitologieAlexandra CrisanNo ratings yet
- CholestaticDocument191 pagesCholestaticDunareanu Ana-alexandraNo ratings yet
- 3 PracticalDocument47 pages3 PracticalT NNo ratings yet
- ABO subgroups Bombay group phenotypesDocument15 pagesABO subgroups Bombay group phenotypeshamaadaNo ratings yet
- ChemiluminiscentaDocument9 pagesChemiluminiscentaLucia CristinaNo ratings yet
- Hymenolepis Nana Vs Hymenolepis DimunotaDocument4 pagesHymenolepis Nana Vs Hymenolepis DimunotaangelNo ratings yet
- Metastaze MedulareDocument40 pagesMetastaze MedulareIrina StamateNo ratings yet
- IMUNOLOGIE - Coloratii imunohistologice si separarea populatiilor celulare de anticorpiDocument6 pagesIMUNOLOGIE - Coloratii imunohistologice si separarea populatiilor celulare de anticorpiRaduta CosminNo ratings yet
- Overview of the Complement System: Activation Pathways, Regulation, Functions and Roles in DiseaseDocument9 pagesOverview of the Complement System: Activation Pathways, Regulation, Functions and Roles in DiseaseAxel RamírezNo ratings yet
- AML Immunophenotyping Guide for Diagnosis and ClassificationDocument88 pagesAML Immunophenotyping Guide for Diagnosis and ClassificationKarla Novoa PérezNo ratings yet
- Otagiri, 2016. Albumin in Medicine. EBOOKDocument279 pagesOtagiri, 2016. Albumin in Medicine. EBOOKFinda Istiqomah100% (1)
- Complement Analysis 2016 Clinical Indications Laboratory Diagnostic and Quality ControlDocument12 pagesComplement Analysis 2016 Clinical Indications Laboratory Diagnostic and Quality ControlMARIANA CASTRO DELGADONo ratings yet
- Ast Booklet GB Final PDFDocument19 pagesAst Booklet GB Final PDFAhmed GaberNo ratings yet
- PreciControl HbA1c Norm.05975115001.V4.EnDocument2 pagesPreciControl HbA1c Norm.05975115001.V4.EnARIF AHAMMED PNo ratings yet
- Microbiology Medical MicrobiologyDocument40 pagesMicrobiology Medical MicrobiologyAngelic khanNo ratings yet
- CH50Document88 pagesCH50ABIGAILNo ratings yet
- Applied Microbiology Fall 2015Document56 pagesApplied Microbiology Fall 2015Le HungNo ratings yet
- Tetanus: Ma. Theresa Dj. YumangDocument28 pagesTetanus: Ma. Theresa Dj. YumangJean SarocamNo ratings yet
- M51S1Document2 pagesM51S1Hassab SaeedNo ratings yet
- Analysis of Organophosphorus Pesticides by GC: Key WordsDocument4 pagesAnalysis of Organophosphorus Pesticides by GC: Key WordstalebNo ratings yet
- S 016 LBLDocument5 pagesS 016 LBLmanishbabuNo ratings yet
- Sperm Count ProtocolDocument3 pagesSperm Count ProtocolGeoemilia1No ratings yet
- Bacterii Identificate Cu VITEKDocument4 pagesBacterii Identificate Cu VITEKGeoemilia1No ratings yet
- Reference: 01-592 Technical Data Sheet Product: Bile Esculin Azide AgarDocument2 pagesReference: 01-592 Technical Data Sheet Product: Bile Esculin Azide AgarGeoemilia1No ratings yet
- Bacterii Identificate Cu VITEKDocument4 pagesBacterii Identificate Cu VITEKGeoemilia1No ratings yet
- Tryptone Yeast Extract Agar to Slanetz Bartley Agar BaseDocument1 pageTryptone Yeast Extract Agar to Slanetz Bartley Agar BaseGeoemilia1No ratings yet
- 10Document2 pages10Geoemilia1No ratings yet
- 01-278 TDS enDocument2 pages01-278 TDS enGeoemilia1No ratings yet
- BacteriaDocument1 pageBacteriaGeoemilia1No ratings yet
- 01-579 TDS enDocument2 pages01-579 TDS enGeoemilia1No ratings yet
- Caiet Sumar UrinaDocument1 pageCaiet Sumar UrinaGeoemilia1No ratings yet
- Test Beta-Lizina CAMP Strept Grup B PDFDocument2 pagesTest Beta-Lizina CAMP Strept Grup B PDFGeoemilia1No ratings yet
- Discuri Antibiograma 1: Denumire Produs Nr. CartuseDocument2 pagesDiscuri Antibiograma 1: Denumire Produs Nr. CartuseGeoemilia1No ratings yet
- Cryo InstantDocument1 pageCryo InstantGeoemilia1No ratings yet
- SpermogramDocument286 pagesSpermogramalmutazimNo ratings yet
- Bacterii Identificate Cu VITEKDocument4 pagesBacterii Identificate Cu VITEKGeoemilia1No ratings yet
- Antibiograma Enterobacteriaceae ClsiDocument2 pagesAntibiograma Enterobacteriaceae ClsiGeoemilia1No ratings yet
- 70 2009 1806 1 PDFDocument2 pages70 2009 1806 1 PDFFer FloresNo ratings yet
- Paraziti IntestinaliDocument31 pagesParaziti IntestinaliGalateanu MagdaNo ratings yet
- Ezhawg474 F7ha83772Document1 pageEzhawg474 F7ha83772mlaorrcNo ratings yet
- Model Caiet UroculturiDocument1 pageModel Caiet UroculturiGeoemilia1No ratings yet
- PX Sperma WHODocument56 pagesPX Sperma WHOichtiyaNo ratings yet
- Noutati CLSI 2015Document35 pagesNoutati CLSI 2015Geoemilia1No ratings yet
- Model Caiet ExsudatDocument2 pagesModel Caiet ExsudatGeoemilia1No ratings yet
- Metoda 9308-3Document6 pagesMetoda 9308-3horia96No ratings yet
- Policy # MI/MYC/v01: Procedure Manual Toronto Medical Laboratories / Mount Sinai Hospital Microbiology DepartmentDocument61 pagesPolicy # MI/MYC/v01: Procedure Manual Toronto Medical Laboratories / Mount Sinai Hospital Microbiology DepartmentPalak AgarwalNo ratings yet
- BK Command Line InstallationDocument294 pagesBK Command Line Installation007\\\\No ratings yet
- Quantum Computing CSDocument101 pagesQuantum Computing CSRaghavNo ratings yet
- CCPDocument2 pagesCCPsanojmk2004No ratings yet
- Guided Noteboo Kin GED10 2 (Mathe Matics in The Modern World)Document5 pagesGuided Noteboo Kin GED10 2 (Mathe Matics in The Modern World)Aaronie DeguNo ratings yet
- Knowledge (2) Comprehension (3) Application (4) Analysis (5) Synthesis (6) EvaluationDocument5 pagesKnowledge (2) Comprehension (3) Application (4) Analysis (5) Synthesis (6) EvaluationxtinNo ratings yet
- 2001 Bhuj EarthquakeDocument2 pages2001 Bhuj EarthquakeBhushanRajNo ratings yet
- EOS Web and Multimedia L3Document53 pagesEOS Web and Multimedia L3ብርሃነ ኣፅብሃNo ratings yet
- Insurance - Unit 3&4Document20 pagesInsurance - Unit 3&4Dhruv GandhiNo ratings yet
- CPO Science Foundations of Physics: Unit 7, Chapter 24Document47 pagesCPO Science Foundations of Physics: Unit 7, Chapter 24dheerajbhagwatNo ratings yet
- Compact NSX - Micrologic 5-6-7 - User Guide 11Document1 pageCompact NSX - Micrologic 5-6-7 - User Guide 11amnd amorNo ratings yet
- Chapter 2. COST IDocument8 pagesChapter 2. COST IyebegashetNo ratings yet
- BEETLE /M-II Plus: POS System For The Highest Standards of PerformanceDocument2 pagesBEETLE /M-II Plus: POS System For The Highest Standards of PerformanceHeather JensenNo ratings yet
- PTR 326 Theoretical Lecture 1Document14 pagesPTR 326 Theoretical Lecture 1muhammedariwanNo ratings yet
- Eng. XI, U18 Meaning Into WordsDocument4 pagesEng. XI, U18 Meaning Into Wordssanad BhattaraiNo ratings yet
- Solution:: Ex 3.3 Consider The Following Parallelograms. Find The Values of The Unknowns X, Y, ZDocument9 pagesSolution:: Ex 3.3 Consider The Following Parallelograms. Find The Values of The Unknowns X, Y, ZpadmaNo ratings yet
- MCM SQL PDFDocument8 pagesMCM SQL PDFJeyakumar NarasingamNo ratings yet
- Getting Started With PhotoshopDocument15 pagesGetting Started With PhotoshopJEANIFER BUGARINNo ratings yet
- Chapter OneDocument36 pagesChapter Onepretoria agreement21No ratings yet
- DES-4122 Specialist-Implementation Engineer PowerEdge ExamDocument4 pagesDES-4122 Specialist-Implementation Engineer PowerEdge ExamArnaldo Jonathan Alvarado RuizNo ratings yet
- Icarus & DaedalusDocument2 pagesIcarus & DaedalusIsrael AsinasNo ratings yet
- Post Office Challan - RRB RECRUITMENT PDFDocument1 pagePost Office Challan - RRB RECRUITMENT PDFGaurav KashyapNo ratings yet
- ANR causes and solutionsDocument2 pagesANR causes and solutionsPRAKHAR SRIVASTAVANo ratings yet