Professional Documents
Culture Documents
Cervical Cancer Screening PDF
Uploaded by
fahmiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cervical Cancer Screening PDF
Uploaded by
fahmiCopyright:
Available Formats
QEYGYN051
Cervical Cancer Screening
Clinical Practice Guidelines for Average Risk Women
For Approval of the Provincial Medical Affairs Committee
October 2013
Table of Contents
Page
Background Information & Contributors 3-5
Process for Guideline Review
Average Risk Women
Primary Testing
PEI Cervical Cancer Incidence Rates
PEI Revised Screening Guidelines & Rationale 6-8
Initiation
Interval
Cessation
Screening Women with Special Circumstances 9
Management of Abnormal Cytology 10
HPV Testing 11
Conclusion 12
Appendix A:
Clinician Reference Tool
DRAFT For Approval (October 2013)
Background
The last review of the PEI Cervical Cancer Screening Clinical Practice Guidelines was done in 2009. Since that
time advancements in testing and screening practices have evolved to improve cervical cancer prevention. In
response to the updated guidelines in other provinces and updated cervical cancer screening recommendations
by the Canadian Task Force on Preventative Health Care (CTFPHC), a working group was struck to begin the
revision of screening guidelines in PEI using the latest evidence.
The goals of the working group were to:
draft, revise and finalize the PEI Cervical Cancer Screening Clinical Practice Guidelines according to
current evidence and within available resources,
develop an implementation and communications plan to ensure clinicians, stakeholders and public are
aware of the revised guidelines in PEI,
And recommend next steps including a monitoring and review process.
The working group was formed to ensure a balance of expertise with contributions from the across continuum
of care from prevention to detection and treatment. Members of the working group included:
Role Name Business Area
Chair Dr. Krista Cassell Gynecology (QEH)
Past-Chair Dr. Ruth Sellers Acting Director of Medical Affairs
Member Dr. David I. Stewart Cornwall Pap Screening Clinic
Member Dr. Lamont Sweet Chief Public Health Officer
Member Dr. Carol McClure Epidemiologist, Chief Public Health Office
Member Dr. Kristen Mead Pathology/Laboratory Services
Member Dr. Elizabeth Barbrick-Crozier Gynecology (PCH)
Member Dr. Jennifer Zelin Family Physician (Queens)
Member Dr. Gil Grimes Family Physician (Prince)
Member Dr. Philip Hansen Family Physician (Prince)
Member Sherri McKinnon Nurse Practitioner, Primary Care Network East
Member Christina Phillips Registered Nurse, Primary Care Network West
Member Pat Charlton Manager, Chronic Disease Prevention & Management Unit
Coordinator Marla Delaney Cancer Screening Programs
DRAFT For Approval (October 2013)
Review Process:
To undertake this review, a process was developed and timelines were determined by the working group with
the intention to launch the revisions by October 2013.
This process included gathering up-to-date evidence from research and any available provincial data, face-to-
face meetings of the working group, an ad hoc review of the draft guidelines, and work to garner support and
endorsement from the Provincial Medical Affairs Committee, administration and professional and community
stakeholders. All of these processes culminated with a consensus on proposed changes to the current guidelines
to be supported by a plan for implementation, communication and monitoring to ensure every effort is made to
engage clinicians and the public.
DRAFT For Approval (October 2013)
Screening & Early Detection for Average Risk Women:
A woman’s risk of developing cervical cancer can increase based on age, personal and family history of cancer,
ethnicity, a history of early or multiple pregnancies, and a history of abnormal cervical tests or the presence of
the human papillomavirus (HPV).
The following Clinical Practice Guidelines (CPG’s) for cervical cancer screening are intended for women of
average risk, where the primary risk factor is age. Women who have had a subtotal hysterectomy and retain
their cervix, who have a history of dysplasia, or who are pregnant require different attention. Screening
practices for such situations would be individualized. (See section below “Screening for Women with Special
Circumstances” or refer to Appendix A: Clinician Reference Tool)
Primary Screening Test in PEI:
These revised CPG’s were developed based on the current practice of conventional cytology collection using a
Pap smear.
Progress in Cervical Cancer Prevention:
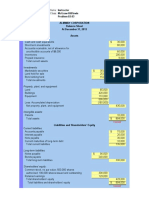
PEI cervical cancer trends for the past 30 years (1982-2012) have shown a decrease in the incidence rate of
cervical cancers. (Figure 2)
Figure 2: PEI Cancer Trends Report (2012)
DRAFT For Approval (October 2013)
Age of Cervical Screening Initiation
PEI Guidelines 2009
All Women age 18 and over or within three years of first sexual activity should be screened for
cervical cancer by a Pap screening test.
PEI Guideline Revision 2013
All women aged 21 and over should be screened for cervical cancer using a Pap test.
- Women who are not sexually active by age 21 should delay cervical cancer screening until
sexually active.
- Women who have never been sexually active do not require cervical cancer screening
“Sexually active” includes intercourse, as well as digital or oral sexual activity involving the genital area
with a partner of either sex.
For women under the age of 21, interaction with healthcare providers is encouraged for STI
screening, HPV vaccination and for necessary contraception.
Rationale and Evidence for Revision:
Based on current evidence and expert opinion, age 21 was determined as the optimal time to initiate cervical
screening to be most effective for the prevention of cervical cancer, especially when looking at the ages of
existing precancerous cases of Island women.
The recommendation of a start age of 25 years published in 2013 by the Canadian Task Force on Preventative
Health Care (CTFPHC)1 was considered, however, this was labeled as a weak recommendation with only
moderate quality evidence by the CTFPHC. There was however a strong recommendation and high quality
evidence to determine that there was no benefit of screening women any younger than age 20.
In response to the Task Force recommendations, a joint position statement was released by The Society of
Obstetricians and Gynaecologists of Canada (SOGC), The Society of Gynecologic Oncology of Cancer (SGOC), and
the Society of Canadian Colposcopists (SCC)2. This group agreed that the age to start screening can be
controversial and that evidence varies amongst international studies. Key to this position is the written
statement, “We should remember that screening 21-25 year old women for precursors has the potential to
prevent cancer in women in their 30’s, when cervical cancer rates start to rise.”
The group also turned to the Epidemiological and Cytology information for PEI women. The information
examined by the group demonstrated to best detect abnormal cells at the pre-cancerous stage, initiation would
need to be prior to age 25. There were no cases of squamous cell cervical carcinoma in women aged 20-24 years
of age in the past decade, though there were cases detected between ages 25-29, supporting that screening to
prevent should take place prior to age 25.
1
Canadian Task Force on Preventative Health Care: Recommendations on screening for cervical cancer. CMAJ, January 8,
2013, 185 (1). http://canadiantaskforce.ca/guidelines/screening-for-cervical-cancer
2
Joint Position Statement regarding recommendations on screening for cervical cancer. http://sogc.org/wp-
content/uploads/2013/04/medCervicalCancerScreeningENG130220.pdf
6
DRAFT For Approval (October 2013)
Cervical Screening Interval
PEI Guidelines 2009
Most women should be screened for cervical cancer every 2 years, after three consecutive annual
negative tests have been documented.
If abnormalities are detected, the schedule for repeat examinations is dictated by clinical
requirements.
PEI Guideline Revision 2013
Pap testing for cervical cancer screening of average risk women should be done every 2 years.
If abnormalities are detected, follow related recommendation in the “Management of Cytology
Abnormalities”.
Rationale and Evidence for Revision:
The rate of Island women completing a pap test within a three year period was examined and found that there is
high uptake in those between 20-29 years (89%) of age and a continuous decline in screening rates of women
between 40-69 years of age (47%). Figure 1: Pap Screening Participation in PEI 2009-11.
Figure 1: Percentage of Women who have successfully completed a Pap test, between 2009 and 2011, compared
to overall female population in PEI (Census 2011)
The CTFPHC recommendation of a 3 year interval was considered, however reaching under-screened and never
screened women with an extended interval without an organized screening program structure on PEI was a
concern of the working group. The Joint Position Statement by the SOGC, SGOC and SCC also reflected on the
fact that 50% of cervical cancers are found in women who had never screened or lapsed in their screening
routine. They caution that without a tracking and recall program a move to the three year interval could mean
more women never or under-screened.
Increased uptake of regular cervical screening for women in Canada, especially those over the age of 40, would
have a significant impact on the incidence and mortality of cervical cancers. To best engage the population, the
working group felt it was important to maintain a 2 year screening interval, providing consistency with other
population-based cancer screening recommendations in PEI.
It was acknowledged that a recommendation for a 3 year interval would be better supported by the group if PEI
had an organized screening program where women were supported by correspondence and recalls.
DRAFT For Approval (October 2013)
Age of Cervical Screening Cessation
PEI Guidelines 2009
In most women, Pap screening should be discontinued after age 75, if they have had two negative
tests, at the recommended screening interval.
Pap screening may be discontinued in women who have had a total hysterectomy, in the absence of a
cervical malignancy or pre-malignancy.
PEI Guideline Revision 2013
Women of average risk should cease Pap testing at age 65, provided that they have had an adequate
history of normal tests in the previous ten years (i.e. three or more negative Pap tests)
Abnormalities are to be managed as clinically indicated based on the revised “Managing of Cytology
Abnormalities” recommendations.
Rationale and Evidence for Revision:
There was limited evidence found that screening over age 70 prevented cervical cancers in all published
materials, including the CTFPHC. The group in turn reviewed the guidelines of other provinces and territories as
well as the local data on incidence, mortality and screening history where available. As each province updates
their guidelines for cervical cancer screening, there is a definite shift to lower the age of screening cessation as
more information becomes available and the science of HPV advances. Cancer Care Ontario’s Program in
Evidence-Based Care released an updated report in 2011 on Cervical Screening3. The discussion and evidence in
this document supports the move to age 65 from age 70 as a phased in approach in Ontario. This
recommendation is the consensus of the authors, taking into account the low rate of cervical cancer in this age
group among women who have previously been adequately screened, the potential discomfort of the
procedure, and difficulties with visualization of the squamocolumnar junction in older women.
The PEI Cancer Registry and laboratory cytology records show that there were less than 5 cases of cervical
cancer in the past 5 years of women aged 65 and over. Due to confidentiality of the patients, sharing the data is
not permitted. However, it was demonstrated that the cases of squamous cell carcinomas of the cervix reported
were of women who had not followed the recommended screening guidelines.
3
Murphy J, Kennedy E, Dunn S, Fung Kee Fung M, Gzik D, McLachlin CM, et al. Cervical Screening. Toronto
(ON): Cancer Care Ontario; 2011 Oct 5. Program in Evidence-based Care Evidence-based Series No.: 15-9.
http://www.cancercare.on.ca/toolbox/qualityguidelines/clin-program/screening-ebs/
DRAFT For Approval (October 2013)
Screening Women with Special Circumstances4: (all in Appendix A)
These guidelines do not apply to women who have been previously treated for dysplasia. Screening
intervals should be individualized and should likely be annual.
Immunocompromised women should receive annual screening.
Women who have undergone subtotal hysterectomy and retained their cervix should continue screening
according to the guidelines.
Pregnant women should be screened according to the guidelines; however, care should be taken not to
over-screen. Only conduct Pap tests during pre-natal and post-natal visits if the woman is otherwise due
for screening.
Women who have sex with women should follow the same cervical screening regimen as women who
have sex with men.
Women who have received the HPV vaccine should continue with screening.
Women who have had previous positive HPV test but have a negative cytology test during
routine screening require repeat testing (both HPV and Pap) twelve months after the negative
cytology test. For more information on managing this please refer to the SOGC Joint Clinical
Practice Guidelines.
4
Cancer Care Ontario: Ontario Cervical Screening Cytology Guidelines Summary (2012).
www.cancercare.on.ca/screenforlife
DRAFT For Approval (October 2013)
Management of Cytology Abnormalities
PEI Guidelines 2009
Repeat Pap test in 3 months if “UNSAT” (Unsatisfactory).
Repeat Pap test twice at 6 month intervals, 2 abnormal tests (ASC-US, LSIL) within 2 year period
warrants colposcopy.
Colposcopy if ASC-H, HSIL, malignant
PEI Guideline Revision 2013
Cytology Result: Follow-up:
UNSAT (unsatisfactory) Repeat Pap in 3 months.
ASCUS Repeat Pap in 6 months. If abnormality is
persistent, refer to colposcopy.
If HPV Testing is used in women 30 years or older
and the results is negative, repeat cytology in 12
months. If the HPV test result is positive, then
refer to colposcopy.
LSIL Repeat Pap in 6 months. If abnormality is
persistent, refer to colposcopy.
ASC-H, AGUS, HSIL+ or Malignancy Refer to colposcopy.
Rationale and Evidence for Revision:
The group turned to the Journal of Obstetrics and Gynaecology Canada (JOGC) and reviewed the clinical practice
guideline for Colposcopic Management of Abnormal Cervical Cytology and Histology5. Developing these guidelines
was a major endeavor with the input of many contributing experts. Having a Canadian consensus and standardizing
practices demonstrates a significant advancement in practice. These guidelines should support and provide
consistency in practice of the abnormal management from primary care providers and in gynecologic intervention by
specialists and align with any reporting from laboratory services.
It was noted by the group that the implementation of HPV Testing would change the recommended follow-up of
abnormalities. The working group recommends that HPV testing only be considered for women age 30 or over
following the primary screening cytology result of Atypical Squamous Cells of Undetermined Significance (ASCUS).
The management plan of a HPV positive test requires clinicians to consider if the abnormal was high or low grade,
patient history, any risk factors and age. This would improve management of abnormalities with an HPV confirmation,
especially in the younger population, and would allow of more appropriate colposcopy referral.
For more information on HPV testing in PEI see the HPV discussion below and Appendix A: Clinician Reference Tool.
5
Colposcopic Management of Abnormal Cervical Cytology and Histology. J Obstet Gynaecol Can 2012;34(12):1188–1202
10
DRAFT For Approval (October 2013)
HPV Testing
PEI Guidelines 2009
Nothing stated at that time.
PEI Guideline Revision 2013
Recommendation on HPV testing as a primary cervical screening tool will be developed based on
ongoing monitoring of evidence as it develops; will require local planning and the allocation of
resources.
HPV Testing can be used for women aged 30 and over with the presence of ASCUS. See “Clinician
Reference Tool: Recommendations for Follow-up of Abnormal Cytology” (Appendix A)
Rationale and Evidence:
The review done by the CTFPHC did not provide sufficient evidence for the Task Force to confidently make any
recommendations at this time. Currently, each province and territory is examining their resources, any
developing evidence and considering HPV testing as a population-based screen for cervical cancers.
Cancer Care Ontario’s revised cervical screening guidelines were released in 2011 with a phased in approach to
move from cytology testing to HPV testing. This shift will influence the age of initiation and cessation as well as
extending the screening interval. It is recommended that PEI monitor the experience in such jurisdictions as
Ontario and any other evidence that arises that would strengthen a recommendation for HPV testing as a form
of cervical cancer screening.
The best way to test for HPV, and the follow-up to diagnosis, is not definitively known at this time. When
examining other jurisdictions, a variety of ways of testing, implementation and guidelines of HPV testing are
being piloted or are only newly adopted and not yet evaluated. Based on experiences in other jurisdictions and
evidence, future consideration for feasibility in PEI is required.
The working group recognizes that HPV testing in women age 30 and over following the primary cytology screen
resulting in a finding of ASCUS can be used as a triage to better determine the management plan. This aligns
with the recommendations in the SOGC Joint Clinical Guidelines for Colposcopic Management of Abnormal
Cervical Cytology and Histology. However, it is important to acknowledge that at this time that HPV testing is not
covered by PEI Medicare so the cost of HPV testing would be the responsibility of the woman. With this in mind,
management of ASCUS can be done with either cytology or HPV testing, depending on which test is used. (Health care
providers can request the HPV test through PEI Laboratory Services)
The group recommends that Health PEI begin planning for HPV testing, as this is on the horizon as evidence
grows, and will require decisions and investments in cervical cancer screening on PEI. With this planning it a cost
benefit analysis is needed to determine the optimal primary screening tool for population-based cervical cancer
screening.
11
DRAFT For Approval (October 2013)
Conclusion:
The practice of regular screening for cervical cancer has made a significant impact on the incidence and
mortality rates in Canada and PEI over the past three decades. To maintain effective practice, it is important the
guidelines be reviewed and revised as new evidence emerges. This revised version of the PEI Cervical Cancer
Screening Clinical Practice Guidelines demonstrates an alignment with the recommendations of other
jurisdictions in Canada and where information is available, is guided by actual data of precancerous and cancer
cases of women in PEI.
The review process is ongoing and should remain supported by experts who can best advise on advancing
practices. Monitoring the implementation of these revisions is vital to ensure that clinical practices are up to
date, appropriate and are making the most positive impact in preventing cervical cancers.
Health PEI is committed to providing effective, efficient and high quality evidence-based services to Islanders.
These values were maintained throughout the development process. The working group acknowledged that
clinical practice guidelines, when implemented fully, can greatly impact services; improve patient care, and
health outcomes. It is anticipated that the guidelines be reviewed every three years unless major evidence
becomes available that would require immediate alignment of practice for the safety of patients.
Thanks are extended to all those who contributed to this work.
12
DRAFT For Approval (October 2013)
Appendix A PEI Cervical Cancer Screening Clinical Practice Guidelines
Clinician Reference Tool
Updated October 2013
These guidelines are for screening average risk, asymptomatic women.
A symptomatic woman with a visibly abnormal cervix or abnormal bleeding should be tested and/or referred appropriately.
Screening Initiation Women aged 21 and over should be screened for cervical cancer using a Pap test.
- Women who are not sexually active by age 21 should delay cervical cancer screening
until sexually active.
- Women who have never been sexually active do not require cervical cancer screening.
“Sexually active” includes intercourse, as well as digital or oral sexual activity involving the genital
area with a partner of either gender.
For women under the age of 21, interaction with healthcare providers is encouraged for STI
screening, HPV vaccination and for necessary contraception.
Screening Interval Pap screening of average risk women should be done every 2 years.
Women older than 65 years who have had an adequate negative cytology screening history in
Screening Cessation the previous 10 years can discontinue screening (i.e. three or more negative Pap tests).
Optimal Screening The conventional Pap smear is the tool used in PEI for cervical screening.
Tool
There is emerging interest in the use of HPV testing as a primary screening tool; however,
there is currently not enough evidence to recommend it for this purpose in PEI. HPV testing
has been well established for use in triaging ASCUS results and may play a role in the
management of these patients. At this time, HPV testing is not covered by PEI Medicare and
the cost of HPV testing would be the responsibility of the patient.
Women with Special Circumstances:
Hysterectomy Women who have undergone subtotal hysterectomy and retained their cervix
should continue screening according to guidelines.
Women who have had a total hysterectomy with the cervix removed for BENIGN
DISEASE may discontinue screening as long as there is a adequate pathological
documentation that the cervix has been removed completely and there is not history
of high grade lesions. If Pap tests results or hysterectomy pathology is unavailable,
continue screening until 2 negative vaginal vault tests are obtained.
Pregnant Women Pregnant women should be screened according to the guidelines, however care
should be taken not to over-screen. Only conduct Pap tests during pre-natal and
post-partum visits if the woman is otherwise due for screening.
Pregnant women who have an ASCUS or LSIL test result should have a repeat Pap
test 3 months after delivery. Those with an HSIL, ASC-H or AGC test result should be
referred for colposcopy during pregnancy, ideally within 4 weeks.
Immunosuppressed Because of the increased risks associated with immunosuppression, these women
Women should be screened annually.
This includes women who are transplant recipients, being treated with
chemotherapy or taking long-term corticosteroids, or who are HIV/AIDS positive.
Women who have The gender of the sexual partner does not change the woman’s risk of cervical
sex with other cancer. These women should be screened according to their other risk factors.
women
Previous high-grade After treatment for dysplasia (biopsy proven NOT abnormal Pap result) or cancer,
lesions or cancer. continue to screen annually.
HPV Vaccinated Continue screening according to the clinical guidelines noted above for average risk
Women women.
13
DRAFT For Approval (October 2013)
Appendix A Recommendations for Follow-up of Abnormal Cytology
October 2013
It is recommended that clinicians turn to the SOGC Joint Clinical Guidelines:
“Colposcopic Management of Abnormal Cervical Cytology and Histology Guidelines”
Cytological Abnormality Recommended Management
Atypical Squamous Cells of For women < 30 years of age (HPV triage not recommended)
Undetermined Significance Repeat cytology in 6 Result: Negative Result: Negative Routine screening
(ASCUS) months Repeat Cytology in 6 in 2 years
months
* HPV Testing is available by Result: ≥ ASCUS Colposcopy
request to Laboratory Result: ≥ ASCUS Colposcopy
Services in PEI but at a cost to
For women ≥ 30 years of age (If HPV Testing is used)
the patient. HPV Testing is
not covered by PEI Medicare. HPV Test* Result: Negative Repeat Cytology in Result: Negative Routine screening in
12 months 2 years
Result: Positive Colposcopy
For women ≥ 30 years of age (If HPV testing is NOT used)
Repeat Result: Negative Repeat Cytology in Result: Routine screening in
Cytology in 6 12 months Negative 2 years
Months Result: ≥ ASCUS Colposcopy
Low-Grade Squamous Repeat Cytology Result: Negative Repeat cytology in Result: Routine Screening in
Intraepithelial Lesion (LSIL) in 6 months 6 months Negative 2 years
Result: ≥ ASCUS Colposcopy
Atypical Glandular Cells (AGC) Colposcopy and endocervical curettage.
Formerly referred to as Women over 35 years of age or with a history of abnormal bleeding should have endometrial
Atypical Glandular Cells of sampling.
Undetermined Significance
(AGUS)
Atypical Squamous Cells,
Cannot Exclude HSIL (ASC-H)
Atypical Glandular Cells of Colposcopy
Undetermined Significance
(AGUS)
High Grade Intraepithelial
Lesion (HSIL)
Carcinoma/Malignancy
Unsatisfactory for Cytology Repeat cytology in 3 months.
Evaluation
Satisfactory but No Routine screening as per screening guidelines; no immediate recall required.
Transformation Zone Present
Benign Endometrial Cells on - Pre-menopausal women who are asymptomatic require no action (follow screening
Pap Test guidelines).
- Post-menopausal women may require investigations, including adequate endometrial tissue
sampling.
- Any woman with abnormal vaginal bleeding requires investigation, which may include
adequate endometrial tissue sampling.
Cytology Negative and HPV Women with negative cytology and positive HPV results should have both tests repeated with
Positive their primary health care provider after 12 months.
12 Month Follow-up Test Result Plan:
Cytology: Negative Return to routine cytology screening every 2
HPV: Negative years.
Cytology: Abnormal Manage as clinically indicated for cytological
abnormality
HPV: Positive 2 times 1 year apart Colposcopy
14
DRAFT For Approval (October 2013)
You might also like
- Fire Resistance UL 1709Document2 pagesFire Resistance UL 1709ednavilod100% (3)
- Entrepreneurship & New Venture Management 6e - Chapter 1Document19 pagesEntrepreneurship & New Venture Management 6e - Chapter 1Hlulani Decision50% (2)
- Uterine ProlapseDocument3 pagesUterine ProlapsefrankyNo ratings yet
- Dissertation - CD 2Document112 pagesDissertation - CD 2pavlov2No ratings yet
- Vancouver Style Referencing SystemDocument20 pagesVancouver Style Referencing SystemKarthik ManoharanNo ratings yet
- Discover Haxeflixel FullDocument182 pagesDiscover Haxeflixel FullKristian Macanga100% (3)
- Online Auction SystemDocument29 pagesOnline Auction SystemDharmendra83% (6)
- Singer and Monaghan's Cervical and Lower Genital Tract Precancer: Diagnosis and TreatmentFrom EverandSinger and Monaghan's Cervical and Lower Genital Tract Precancer: Diagnosis and TreatmentRating: 5 out of 5 stars5/5 (1)
- Role of Midwifery NurseDocument6 pagesRole of Midwifery NurseLokeshwari KatreNo ratings yet
- Clinical Presentation of FibroidsDocument12 pagesClinical Presentation of FibroidsErwin YanthoNo ratings yet
- Pap Smear - Overview, Indications, PreparationDocument11 pagesPap Smear - Overview, Indications, PreparationBayu Surya DanaNo ratings yet
- Deep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateDocument26 pagesDeep Vein Thrombosis in Pregnancy - Epidemiology, Pathogenesis, and Diagnosis - UpToDateCristinaCaprosNo ratings yet
- MCH Epidemiology Issues MagnitudeDocument25 pagesMCH Epidemiology Issues MagnitudeRatna KumariNo ratings yet
- Dubai Obstetrics and Gynaecology Residency Training ProgrammeDocument48 pagesDubai Obstetrics and Gynaecology Residency Training ProgrammeAloah122346No ratings yet
- Breast Cancer Awareness Among Pregnant Women at Hoima Regional Referral Hospital, Western UgandaDocument12 pagesBreast Cancer Awareness Among Pregnant Women at Hoima Regional Referral Hospital, Western UgandaKIU PUBLICATION AND EXTENSIONNo ratings yet
- Imaging Safety in PregnancyDocument8 pagesImaging Safety in PregnancyKeeranmayeeishraNo ratings yet
- Gandhi University of Health Sciences, Karnataka Synopsis For Registration of Subject For DissertationDocument16 pagesGandhi University of Health Sciences, Karnataka Synopsis For Registration of Subject For DissertationNaman MishraNo ratings yet
- Journal Homepage: - : IntroductionDocument4 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- The Role of Nursing in Cervical Cancer Prevention and TreatmentDocument5 pagesThe Role of Nursing in Cervical Cancer Prevention and TreatmentLytiana WilliamsNo ratings yet
- Signs and Symptoms of PregnancyDocument9 pagesSigns and Symptoms of PregnancyTrina Joy DomantayNo ratings yet
- 05 N141 31673Document21 pages05 N141 31673priya thakurNo ratings yet
- Family Life EducationDocument6 pagesFamily Life EducationKALAI AKSHAYANo ratings yet
- Ob/Gyn Instruments: Done byDocument30 pagesOb/Gyn Instruments: Done byDrHassan Ahmed ShaikhNo ratings yet
- Breastfeeding Issues, RX If Mother N Baby in HivDocument82 pagesBreastfeeding Issues, RX If Mother N Baby in HivMallika JoonNo ratings yet
- Nursing As A Profession: by Jeelani SaimaDocument53 pagesNursing As A Profession: by Jeelani Saimajeelani saimaNo ratings yet
- OBG MnuemonicsDocument9 pagesOBG MnuemonicskhNo ratings yet
- The Five Practices Standards of Midwifery Care: Practice Standard 1Document5 pagesThe Five Practices Standards of Midwifery Care: Practice Standard 1Mahenur100% (1)
- Assessment of Knowledge On Cervical Cancer Among Bangladeshi Women A Hospital Based Cross Sectional StudyDocument6 pagesAssessment of Knowledge On Cervical Cancer Among Bangladeshi Women A Hospital Based Cross Sectional StudySrideviRaviNo ratings yet
- Assessing Nurses' Knowledge on Using Partographs During LaborDocument22 pagesAssessing Nurses' Knowledge on Using Partographs During Laborrevathidadam55555No ratings yet
- Myoma UteriDocument8 pagesMyoma UteriFaraida Arvilla100% (1)
- Cervical Cancer Prevention StrategiesDocument27 pagesCervical Cancer Prevention StrategiesLalita Eka Pervita Sari100% (1)
- OBG ARTICLES ANUM NooriDocument22 pagesOBG ARTICLES ANUM NooriVaishali SinghNo ratings yet
- Menstrual CycleDocument19 pagesMenstrual Cycleraghuram reddyNo ratings yet
- Abnormal Uterine BleedingDocument5 pagesAbnormal Uterine Bleedingwuryan dewiNo ratings yet
- Ambulatory HysterosDocument8 pagesAmbulatory Hysteroskomlanihou_890233161100% (1)
- Rajiv Gandhi University of Health Sciences, Bangalore, Karnataka, Annexure-Ii Proforma For Registration of Subjects For DissertationDocument14 pagesRajiv Gandhi University of Health Sciences, Bangalore, Karnataka, Annexure-Ii Proforma For Registration of Subjects For DissertationJyotiNo ratings yet
- Physiologicalchangesinpregnancy 170323142156Document69 pagesPhysiologicalchangesinpregnancy 170323142156madhu.B100% (1)
- Following Are The Indications For Medical Termination of PregnancyDocument1 pageFollowing Are The Indications For Medical Termination of PregnancyJayjeet BhattacharjeeNo ratings yet
- Tmbool's Notes in Obstetrics and GynecologyDocument113 pagesTmbool's Notes in Obstetrics and GynecologyFrom HumanNo ratings yet
- Insertion and Removal of Intrauterine Devices-AAFPDocument8 pagesInsertion and Removal of Intrauterine Devices-AAFPnouval_iqbalNo ratings yet
- Thesis ProtocolDocument11 pagesThesis ProtocolSuyajna JoshiNo ratings yet
- IUCD Manual EnglishDocument194 pagesIUCD Manual EnglishHarshaWakodkarNo ratings yet
- Legislations Clinical Rights and Professional ResponsibilityDocument10 pagesLegislations Clinical Rights and Professional ResponsibilityFarheen khanNo ratings yet
- Obstetrics & Gynaecology NursingDocument15 pagesObstetrics & Gynaecology Nursingyola listantiaNo ratings yet
- tmp7DB6 TMPDocument78 pagestmp7DB6 TMPFrontiersNo ratings yet
- Recurrent Pregnancy LossDocument61 pagesRecurrent Pregnancy LossHerman FiraNo ratings yet
- Handout and Questions of HysterosalpingDocument12 pagesHandout and Questions of Hysterosalpingahmad shaltout100% (2)
- Hiv in PregnancyDocument98 pagesHiv in PregnancyAkrit DahalNo ratings yet
- O&G Counselling - TSPDocument6 pagesO&G Counselling - TSPTarran PhagooNo ratings yet
- Understanding HIV and HAART ManagementDocument33 pagesUnderstanding HIV and HAART ManagementWill CheahNo ratings yet
- Effect of A Training Program About Maternal Fetal Attachment Skills On Prenatal Attachment Among Primigravida WomenDocument6 pagesEffect of A Training Program About Maternal Fetal Attachment Skills On Prenatal Attachment Among Primigravida WomenInternational Organization of Scientific Research (IOSR)No ratings yet
- Gynecology Screening ProceduresDocument30 pagesGynecology Screening Proceduresapi-506496190No ratings yet
- Postpartum Care: PuerperiumDocument4 pagesPostpartum Care: PuerperiumBenedict Paul RaguntonNo ratings yet
- Preventive ObstetricsDocument8 pagesPreventive ObstetricsMahima LalNo ratings yet
- د.عبد الزهره THE GYNAECOLOGICAL EXAMINATION-1 (Muhadharaty)Document29 pagesد.عبد الزهره THE GYNAECOLOGICAL EXAMINATION-1 (Muhadharaty)MohammedNo ratings yet
- Presentation (10) 1Document12 pagesPresentation (10) 157 NakshatraNo ratings yet
- Maternal Breastfeeding SatisfactionDocument66 pagesMaternal Breastfeeding SatisfactionALisa ZaharaNo ratings yet
- The Nursing Process: Dr. Abdalkarim RadwanDocument62 pagesThe Nursing Process: Dr. Abdalkarim RadwanAngelique Ramos PascuaNo ratings yet
- Genital Prolapse: Clinical FeaturesDocument29 pagesGenital Prolapse: Clinical FeaturesMerlin AshlyNo ratings yet
- Virginia Henderson's Need TheoryDocument11 pagesVirginia Henderson's Need TheoryjoreyneeNo ratings yet
- Lath ADocument118 pagesLath AManish PandeyNo ratings yet
- Abortion India Lit ReviewDocument48 pagesAbortion India Lit ReviewPrathibha GuruguriNo ratings yet
- 2023 OB/GYN Coding Manual: Components of Correct CodingFrom Everand2023 OB/GYN Coding Manual: Components of Correct CodingNo ratings yet
- Dewhurst's Textbook of Obstetrics & GynaecologyFrom EverandDewhurst's Textbook of Obstetrics & GynaecologyChristoph LeesRating: 2 out of 5 stars2/5 (1)
- Efc EFgffDocument1 pageEfc EFgfffahmiNo ratings yet
- Efc EFgffDocument1 pageEfc EFgfffahmiNo ratings yet
- Efc EFgffDocument1 pageEfc EFgfffahmiNo ratings yet
- Efc EFgffDocument1 pageEfc EFgfffahmiNo ratings yet
- Efc EFgffDocument1 pageEfc EFgfffahmiNo ratings yet
- RR Vwag45Document1 pageRR Vwag45fahmiNo ratings yet
- Ewf/43 TT 4 Edxa 6 DSF 7Document1 pageEwf/43 TT 4 Edxa 6 DSF 7fahmiNo ratings yet
- RR v4vg45Document1 pageRR v4vg45fahmiNo ratings yet
- Efc EFgffDocument1 pageEfc EFgfffahmiNo ratings yet
- RR v4v Ug45Document1 pageRR v4v Ug45fahmiNo ratings yet
- k0td9 FFQWDocument1 pagek0td9 FFQWfahmiNo ratings yet
- RR v4g45Document1 pageRR v4g45fahmiNo ratings yet
- SVSVDocument1 pageSVSVfahmiNo ratings yet
- K 0 S SDQWDocument1 pageK 0 S SDQWfahmiNo ratings yet
- SVJ 2 RwedjtsvDocument1 pageSVJ 2 RwedjtsvfahmiNo ratings yet
- FecwDocument1 pageFecwfahmiNo ratings yet
- 0416Document6 pages0416fahmiNo ratings yet
- K0okj9 FFQWDocument1 pageK0okj9 FFQWfahmiNo ratings yet
- WR 64 Ryrdwefhdb 2 QWDDocument1 pageWR 64 Ryrdwefhdb 2 QWDfahmiNo ratings yet
- 245 Tsad 7 Erf 6 RTDocument1 page245 Tsad 7 Erf 6 RTfahmiNo ratings yet
- Fec WDocument1 pageFec WfahmiNo ratings yet
- Vanasco 2016Document25 pagesVanasco 2016fahmiNo ratings yet
- Mibgciw 7 Yr 388'''Document1 pageMibgciw 7 Yr 388'''fahmiNo ratings yet
- New Text DocumentDocument1 pageNew Text DocumentfahmiNo ratings yet
- Ringkasan Isi Jurnal: Worksheet PrognosisDocument3 pagesRingkasan Isi Jurnal: Worksheet PrognosisfahmiNo ratings yet
- Perkembangan Fetus Dalam Kondisi Defisiensi Yodium Dan Cukup YodiumDocument13 pagesPerkembangan Fetus Dalam Kondisi Defisiensi Yodium Dan Cukup YodiumLaili ZahirohNo ratings yet
- Asdcfvgbnm NDocument1 pageAsdcfvgbnm NfahmiNo ratings yet
- Ringkasan Isi Jurnal: Worksheet PrognosisDocument3 pagesRingkasan Isi Jurnal: Worksheet PrognosisfahmiNo ratings yet
- Men S Health South Africa - March 2017 PDFDocument132 pagesMen S Health South Africa - March 2017 PDFAbimaelGomesNo ratings yet
- Chapter - 1 NetworksDocument61 pagesChapter - 1 NetworksSummiya JangdaNo ratings yet
- Chapter 4 Duality and Post Optimal AnalysisDocument37 pagesChapter 4 Duality and Post Optimal AnalysisMir Md Mofachel HossainNo ratings yet
- Evolution of Arbitration in IndiaDocument8 pagesEvolution of Arbitration in IndiaPururaj AggarwalNo ratings yet
- AI Story WritermnfyaDocument2 pagesAI Story Writermnfyafrenchrugby98No ratings yet
- Ankur Srivastava Project On Scm. at Purchase Dept (2010)Document59 pagesAnkur Srivastava Project On Scm. at Purchase Dept (2010)ankur_jun100% (1)
- Integral Abutment Bridge Design (Modjeski and Masters) PDFDocument56 pagesIntegral Abutment Bridge Design (Modjeski and Masters) PDFAnderson UrreaNo ratings yet
- Edmonton Report On Flood MitigationDocument6 pagesEdmonton Report On Flood MitigationAnonymous TdomnV9OD4No ratings yet
- Blockchain For IBMers - Eng Model v2.01Document25 pagesBlockchain For IBMers - Eng Model v2.01ayanmukherjee1No ratings yet
- Basic IT Tutorial 2 - No Answer, Candidates Are To Work Out The Answers ThemselveDocument3 pagesBasic IT Tutorial 2 - No Answer, Candidates Are To Work Out The Answers ThemselveTri Le MinhNo ratings yet
- 9 Principles of Income Tax LawsDocument82 pages9 Principles of Income Tax LawsVyankatesh GotalkarNo ratings yet
- Bangladesh Labour Rights ResearchDocument29 pagesBangladesh Labour Rights ResearchMd. Hasan Ali JoyNo ratings yet
- GSV EDU Factbook Apr 13 2012Document127 pagesGSV EDU Factbook Apr 13 2012Innovative Educational Services, CCIUNo ratings yet
- SA-10/20 User ManualDocument31 pagesSA-10/20 User ManualJorgeLuis Anaya NúñezNo ratings yet
- Types of FoundationDocument28 pagesTypes of FoundationraniepaulNo ratings yet
- 07 Safety Culture Informed Just and FairDocument49 pages07 Safety Culture Informed Just and FairDaniel Gaspar SilvaNo ratings yet
- CSC V CADocument2 pagesCSC V CAAllen GrajoNo ratings yet
- North American Free Trade Agreement: Prof. MakhmoorDocument15 pagesNorth American Free Trade Agreement: Prof. MakhmoorShikha ShuklaNo ratings yet
- Assignment 2 QP MPMC - ITDocument1 pageAssignment 2 QP MPMC - ITProjectsNo ratings yet
- Melissa Wanstall March 2016Document2 pagesMelissa Wanstall March 2016api-215567355No ratings yet
- Chapter 3 - Excel SolutionsDocument8 pagesChapter 3 - Excel SolutionsHalt DougNo ratings yet
- DL 57 PDFDocument2 pagesDL 57 PDFmaheshm_erpNo ratings yet
- 78ac PDFDocument7 pages78ac PDFvhgiaoNo ratings yet
- National Power Corporation vs Philipp Brothers Oceanic Ruling on Moral DamagesDocument2 pagesNational Power Corporation vs Philipp Brothers Oceanic Ruling on Moral DamagesRandy SiosonNo ratings yet
- Objective: Ofdm ModulationDocument10 pagesObjective: Ofdm ModulationxxNo ratings yet
- Addition Polymerization: PolymerDocument3 pagesAddition Polymerization: PolymerSVNo ratings yet