Professional Documents
Culture Documents
Mechanisms Related To Neuron Injury and Death in Cerebral Hypoxic Ischaemia
Uploaded by
DianOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mechanisms Related To Neuron Injury and Death in Cerebral Hypoxic Ischaemia
Uploaded by
DianCopyright:
Available Formats
Review article
Mechanisms related to neuron injury and death in cerebral
hypoxic ischaemia
Min-Fang Guo, Jie-Zhong Yu, Cun-Gen Ma
Institute of Brain Science, Shanxi Datong University, Datong, Shanxi, China
Folia Neuropathol 2011; 49 (2): 79-87
Abstract
Cerebral hypoxic-ischaemic injury is involved in many central nervous system diseases. The mechanisms of neuron
injury and death in cerebral hypoxic ischaemia remain unclear. There have been many theories on pathogenesis of
neuron injury and death in cerebral hypoxic ischaemia, such as the toxicity of excitatory amino acid, NO, the pro-
duction of oxygen free radicals, chondriosome injury, complement component, injury of immunological inflamma-
tion, matrix metalloproteinase, dopamine, Ca2+ overloading, cell apoptosis and so on. The aim of this review is to
describe recent observations regarding the mechanisms of neuron injury and death in cerebral hypoxic ischaemia.
Key words: neuron, hypoxic ischaemia, excitatory amino acid, NO, free radical, cell apoptosis, immunological inflam-
mation, chondriosome, complement component, matrix metalloproteinase, dopamine, calcium.
Introduction oxidative stress, and followed by prolonged periods
The brain is an important organ of human beings. of delayed cell death or apoptosis, inflammation and
Its weight is about 2% of the whole body weight, so on [13]. The anoxia-induced vulnerability appears
but the brain consumes up to 25% of all the oxygen to be related to the profound rise of the intracellular
the body needs. Most mammalian neurons have concentration of free Ca2+ [48]. A large body of evi-
a low tolerance to brain anoxia because of severe dence suggests that nitric oxide biosynthesis is a key
arterial hypoxia [19,40]. Hypoxic-ischaemic (H-I) factor in the pathophysiological response of the
brain injury is a major cause of acute mortality and brain to H-I [33]. And the generation of nitric oxide
chronic neurological morbidity. The cause of cerebral triggers a cascade of free radical reactions, leading
neuron injury during ischaemic events is an area of to modifications of cerebral plasticity and increasing
major interest to neuroscientists. blood-brain barrier (BBB) permeability, which may
It is now well appreciated that a cerebral H-I be a contributory factor to the progression of H-I
event related to the depletion of tissue energy encephalopathy [27,44]. This short review will focus
reserves is rapidly followed by acidosis, glutamate on the mechanisms of neuron injury and death in
excitotoxicity, production of oxygen free radicals and cerebral H-I.
Communicating author:
Cun-Gen MA, Institute of Brain Science, Medical School, Shanxi Datong University 037009, East Yuhe Bridge, Datong, Shanxi, P.R.China,
phone: +86-352-7158663, mobile: 13803426680, fax: +86-352-6100528, e-mail: macungen2001@yahoo.com.cn
Folia Neuropathologica 2011; 49/2 79
Min-Fang Guo, Jie-Zhong Yu, Cun-Gen Ma
The effect of excitatory amino acids and GLT-1 after rat microsphere embolism and it is
associated with extracellular Glu concentration [20].
Excitatory amino acids (EAAs) are widely distri-
But there is transient enhanced expression of EAATs
buted in the mammalian central nervous system and
in the subcortical white matter early after ischaemia
play an important role in excitatory synaptic trans-
to limit excitotoxicity by means of removing extra-
mission, but are toxic to neurons. Glutamate (Glu) cellular Glu more efficiently and thus generating
and aspartate (Asp) are the main EAAs. Under nor- a refined Glu environment [2]. The study provides
mal conditions, Glu and Asp mainly exist in the vesi- overwhelming evidence that ceftriaxone, a GLT-1
cle of nerve endings. H-I energy metabolic dysfunc- (a major Glu transporter) modulator, caused a signi-
tion has direct inhibitory effects on the activity of ficant upregulation of GLT-1 mRNA and protein and
Na+-K+-ATPase in the cell membranes, and this induced a significant increase in [3H]-glutamate
induces a higher level of extracellular K+ concentra- uptake, which confers neuroprotection in cerebral
tion. EAAs are released into the extracellular space ischaemia/reperfusion injury [53].
when depolarization of neurons occurs. When cere- EAA receptors are the primary excitatory neuro-
bral ischaemia occurs, the inflow of extracellular cal- transmitter receptors in the central nervous system
cium increases, followed by increased intracellular and are divided into two major categories: ion tropic
Ca2+, which might activate phospholipase A2. Phos- receptors and metabotropic receptors. Ion tropic
pholipase A2 acts on membrane phospholipid and receptors contain N-methyl-D-aspartate (NMDA)
changes membrane structure. Thus amino acids dif- receptors, α-amino-3-hydroxy-5-methyl-4-isoxazole-
fuse outside the cell along a concentration gradient propionic acid (AMPA) receptors and kainite recep-
to result in an increase in the efflux of EAAs [39]. tors. The increase of synaptic tyrosine kinase activi-
Benveniste found that the extracellular contents of ty is not only related to the increase in tyrosine
Glu and Asp were increased, respectively, eight- and phosphorylation of the NMDA receptor and the high-
three-fold after a 10-min period of transient com- er level of basal phosphorylation which would con-
plete cerebral ischaemia. The concentration variation tribute to the increased excitability of the NMDA
of EAA in brain was correlated with the degree of receptor supporting normal cerebral development,
brain damage after acute cerebral ischaemia-reper- but also renders the brain more vulnerable to H-I
fusion [25,50]. damage [18]. The results demonstrated that there
Reuptake and absorption by neurocytes is the was enhanced phosphorylation of the NMDAR sub-
only way to inactivate Glu in the nervous system. unit, NR1, by PKC and PKA after ischaemia and which
H-I could result in neuron and glia releasing EAAs and may contribute to alterations in NMDA receptor
reducing the capacity for reabsorption and deactiva- function in the postischaemic brain [8]. The impor-
tion [13]. EAA transporters (EAATs) play a major role tance of metabotropic Glu receptors in brain
in this process. The glutamate transporters EAAT3 ischaemic injury remains uncertain. Glu induces cell
and EAAT4 are expressed in neurons. They contribute death by activating type I metabotropic Glu recep-
to the cellular uptake of Glu and Asp and thus to tors (mGluRs) [21]. mGluR1 after transient focal
the elimination of the excitatory transmitters from ischaemia is involved in the activation of Src and the
the extracellular space. The destruction of the increase in NADPH oxidase activity that is mediated
Na+/K+ transmembrane gradient leads to the reverse by PKCδ. mGluR1 antagonist could modify properties
transportation of EAATs in the membrane when cere- of the NMDA receptor, attenuates infarct size, and
bral ischaemia occurs. Neurons depolarize because reduces NADPH oxidase activity and superoxide pro-
of potassium efflux and energy depletion, by which duction after transient focal cerebral ischaemia
the Glu diffuses outside the cell along the Na+ con- [36,37]. Metabotropic Glu mGlu5 receptor-mediated
centration gradient. Glu uptake was inhibited and serine phosphorylation of NMDA receptor subunit
the release of arachidonic acid was enhanced. And NR1 in the hippocampal CA1 region may be linked to
arachidonic acid could significantly inhibit Glu the pathogenesis of cerebral ischaemia and the
uptake by astrocytes for a long time. Recently Glu mGlu5 receptor antagonist could reduce neuron
transporters have emerged as a potential therapeu- death in this region [49]. But the activation of mGlu4
tic target in a wide range of neurological disorders. receptors limits the development of brain damage
There is downregulation of Glu transporters EAAC1 after permanent or transient focal ischaemia and
80 Folia Neuropathologica 2011; 49/2
Neuron injury in cerebral hypoxic ischaemia
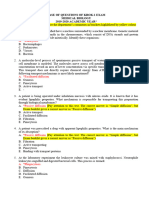
plays a protective role [35]. The early cellular swelling The experiments showed that the protective
occurring during cerebral ischaemia is a result of effects of EAA inhibitors against cerebral ischaemia
massive ionic fluxes mediated by EAAs which are are associated with depressing the extracellular
released by a Ca2+-dependent exocytotic process levels of amino acid transmitters in brain of rats
from the nerve terminals [23]. Glu increases intracel- [57] (Fig. 1).
lular Na+ concentration of neural cells by acting on
AMPA receptors on the cell membrane. Meanwhile Nitric oxide and free radicals
Cl– enters cells along the potential difference.
The entry of Cl– and positive ion leads to the influx Nitric oxide (NO) is closely correlated with H-I
of a large amount of water that causes acute oede- neuron apoptosis since NO biosynthesis is a key fac-
ma of neurons. The over-activation of NMDA recep- tor in the pathophysiological response of the brain to
tor and excessive stimulation of NMDA receptor can H-I (Fig. 1). But the role of NO in H-I injury is actual-
activate another signalling molecule, nNOS, which is ly far more complex than conceived. A study showed
mediated by PSD-95 and is crucial for neuronal that NO mediated the neurotoxicity of Glu, abnor-
injury after cerebral ischaemia [55,62]. NMDA or mality of mitochondrial energy metabolism and
AMPA could worsen the BBB disruption. Any insult impairment of antioxidant status, which may
increasing the release of EAAs could further aggra- account for Glu-mediated neurotoxicity via a mecha-
vate the BBB disruption and brain oedema in the nism involving NO biosynthesis in rat neurons in pri-
focal cerebral ischaemic period [9]. mary culture [5]. Superoxide and NO are able to form
Brain ischemia and/or reperfusion
Mitochondrial respiratory dysfunction ATP ↓
Depolarization of cell membrane
Intracellular and
mitochondrial calcium
overload
AD EAAs ↑
Lipid protein AD AD
enzyme dysfunction
and nucleic
Mitochondrial
acids Free radicals
destroyed NOS activation
Immune
inflammatory NO ↑
Complement AD
component injury
Oxidative stress
Failure of energy
AD metabolism
BBB
destroyed MMPs↑
Cell apoptosis and death
Fig. 1. Pathways leading to cell death in ischaemia-reperfusion.
Folia Neuropathologica 2011; 49/2 81
Min-Fang Guo, Jie-Zhong Yu, Cun-Gen Ma
peroxynitrite, which can be decomposed to produce load and generation of great amounts of free radi-
the powerful and cytotoxic oxidant hydroxyl and cals. As the subcellular target, mitochondria were in-
nitrogen dioxide. These oxidants are highly diffusible jured. Mitochondrial respiratory dysfunction results
and can easily cross the BBB to exert their destruc- in decrease of ATP synthesis, thus affecting the ener-
tive action on brain tissue [52]. NO may modulate gy supply to brain cells and leading to mtDNA disor-
the balance between glucose consumption through der. The animal experiments indicated that there
the glycolytic pathway and the pentose phosphate was decreased expression of mtDNA in CA1 pyrami-
pathway in neurons. This may relate to the mecha- dal neurons during initial H-I. Meanwhile, there was
nisms of neurodegeneration and enhancement of decreased expression of mtRNA and mtDNA encod-
apoptosis due to oxidative and nitrosative stress [4]. ed protein in the period of reperfusion. All of these
The study indicated that activation of the NO/NOS factors seriously affected the function of the respira-
signalling system could trigger amyloid-β (Aβ) pro- tory chain, leading to energy exhaustion and meta-
duction through the beta-site APP-cleaving enzyme 1 bolism level decrease of neurons, which was the
(BACE1) pathway during and after acute focal cere- major cause of neuron delayed death [17]. After cere-
bral ischaemia in aged rats. Then, Aβ stimulates bral ischaemia, mitochondria overproduce reactive
reactive oxygen species production and changes oxygen species (ROS), which activate various mole-
mitochondria activity, leading to apoptosis both in cular signalling pathways. Apoptosis-related signals
vitro and in vivo [29]. Progressively higher levels of return to mitochondria, and then mitochondria
malondialdehyde indicated that free radical causes induce cell death through the release of pro-apop-
severe injury in H-I encephalopathy, which is asso- totic proteins such as cytochrome c or apoptosis-
ciated with the increased concentration of NO [27]. inducing factor [38]. But Yin et al. identified that, for
Free radicals are produced during ischaemia, the first time, increased mitochondrial mass would
which can strengthen activity of lipid peroxidation, clearly improve the overall oxidative function and
induce lesions of the cell and cellular barrier, and fur- energy state of the H-I brain, which may be an endo-
ther result in necrosis or apoptosis of neurons. Free genous neuroprotective response against H-I injury
radicals can reduce the vasoconstrictor response to [59] (Fig. 2).
arterial hypocapnia, damage the vascular endothelial
cells, increase the BBB permeability, interfere with Complement component
and inhibit protein synthesis, and damage the struc-
Permeability of the BBB was increased after
ture of DNA [46]. Endogenous neurotrophin-3 (NT-3)
ischaemia-reperfusion injury, resulting in macromo-
enhanced neuronal injury by increasing oxygen
lecule complement component in blood permeating
radical mediated cell death, accelerated the dissolu-
into brain tissue. And astrocytes in brain possess the
tion of neurons by promoting the release of EAAs,
potential ability of complement synthesis. Astrocytes
cracked the cytolysosome to result in the release of
can synthesize complete complement under stimula-
numerous lysosomes, and damaged mitochondria to
tion of cytokine and regulate the synthesis of com-
result in energy dyspoiesis [3].
plete complement when the brain is injured by H-I.
Two days after hypoxia-reoxygenation, nNOS and
Complement activation is a pathological mechanism
iNOS expression remained high. The study supports
of injury in the post-H-I neonatal brain (Fig. 1).
the intriguing possibility that induction of iNOS and
A role of complements in ischaemia-reperfusion
nNOS after brain hypoxic insult would enhance the
injury was first described by Ward [43]. C3a and C5a
susceptibility of brain to a subsequent excitotoxic
could induce histamine release from inflammatory
insult [14]. Edaravone, a free radical scavenger, had
cells that resulted in a further increase of vascular
a novel neuroprotective mechanism in cerebral
permeability. C5a stimulated vascular smooth mus-
infarction by abrogating the release of high-mobility
cle to lead to exaggeration of brain ischaemia. Fur-
group box-1 in neuronal cells [24].
thermore, complements, such as leukocyte chemo-
tactic factor (LCF), attract leukocyte accumulation
Mitochondrial dysfunction and make the inflammatory reaction more severe.
Mitochondria are the cell’s energy converter. Complement activation results in the production of
Cerebral H-I damage induced intracellular Ca2+ over- inflammatory C3a and C5a, the opsonization of cells
82 Folia Neuropathologica 2011; 49/2
Neuron injury in cerebral hypoxic ischaemia
K+ Ca2+
Na+ mitochondrial
H+ Na+ Na+ Ca2+ respiratory
Ca2+ ATP ↓
Ischaemia dysfunction
O2 ↑
PH ↓ Membrane
lactate damage
Calpain ↑
and rupture
ATP
Cyto Ca2+ ↑ Caspasa ↑
glycolysis
Δψ
Ca2+ ↑ ROS ↑
ATP ADP
O2 ↑
Calpain ↑
Reperfusion +
Na + 2+
H+ Na Ca
Death
Fig. 2. Mitochondrial dysfunction and calcium leading to cell death in ischaemia-reperfusion.
with component C3b and iC3b for recognition and response involving the adherence, accumulation and
phagocytosis by macrophages, and the formation of infiltration of leucocytes produced much proteolytic
lethal membrane attack complexes (MAC) (C5b-9) on enzymes, oxygen free radicals and other factors,
target cell membranes. All these effects finally cause causing the destruction of capillary endothelium and
oedema and death of neurons [1], which demon- basal membrane, and increasing the permeability of
strated that complements are acutely activated in the BBB [11]. Compared with controls, there was
H-I brain. Another study showed that complement a significant increase in the proinflammatory
component C1q can exacerbate cerebral H-I injury by cytokine nuclear factor kB (NFkB) with concomitant
potentiating the severity of mitochondria-mediated upregulation of cell adhesion molecules. Therefore,
oxidative stress [51]. The complement depletion NFkB plays an important role in hypoxia-induced
reduces H-I-induced complement activation and transvascular leakage and cerebral oedema in brain
injury [10]. of rats [42]. Mice with NOX2 subunit gp91 (phox)
knockout (gp91 KO) exhibited less severe post-
Inflammatory and immune mechanisms ischaemic inflammation, demonstrating that NADPH
oxidase is involved in post-ischaemic neuroinflam-
The central nervous system produces inflamma- mation, as evidenced by reduced microglial activa-
tory responses to many injuries. Acute inflammation tion and decreased upregulation of inflammation
plays a key role in secondary brain injury induced by mediators, including IL-1, TNF, iNOS, CC-chemokine
H-I (Fig. 1). The release of oxygen free radicals, ligand 2, and CC-chemokine ligand 3 [7].
inflammatory cytokines, chemotactic factors and the During cerebral ischaemia-reperfusion, astrocytes
upregulation of leucocyte adhesion molecule expres- and gitter cells could secrete many cytokines, such
sion are involved in the event of cerebral ischaemia- as TNF, IL-1, IL-2, IL-8 and so on [47]. TNF is a kind of
reperfusion injury. Thus, local leukocyte accumula- multi-functional proinflammatory cytokine. It aggra-
tion and the increased secretion of cytokines vated the injury of cerebral ischaemia-reperfusion
appeared in cerebral ischaemia-reperfusion injury in through promoting coagulation, increasing endothe-
the acute stage [54]. Inflammation and immune lial cell permeability and inducing adhesion molecule
Folia Neuropathologica 2011; 49/2 83
Min-Fang Guo, Jie-Zhong Yu, Cun-Gen Ma
expression. TNFα and IL-6 may destroy brain choles- neuronal excitation (Fig. 1). DA has two forms, cal-
terol homeostasis by insulting oligodendrocytes, cium-dependent and calcium-independent, when it
which might be important in the molecular patholo- is released in cerebral ischaemia-reperfusion injury.
gy of H-I white matter injury [61]. IL-1 and adhesion Intracellular calcium overload caused by many fac-
molecules facilitate the adherence of leucocytes and tors can promote the release of DA after ischaemia.
endothelial cells, which promotes the inflammatory Meanwhile, there is a decrease of Na+-K+-ATPase
reaction. activity and a decline in the levels of cellular Na+ due
to energy exhaustion, which promotes reverse DA
Hydrolysis of matrix metalloproteinase transport in a Ca2+-independent way and partici-
Leukocytes release many toxic products and pates in the release of DA. DA and its metabolites all
destructive proteinases in the process of activation induce neuronal damage. The toxicity of DA mainly
and adhesion. Among them, matrix metalloprotei- includes: DA own toxicity, the toxicity of its metabo-
nases (MMPs) possess very strong destructiveness lites, increasing the toxicity of EAAs, inducing neu-
to the vascular basement membrane, increase blood ronal apoptosis and so on [6]. Yoshimoto et al. [60]
vessel permeability, and induce cerebral oedema [45] examined the effects of stimulations of ischaemia
(Fig. 1). MMP-2 and MMP-9 are crucial for the degra- and/or potassium on the release of DA and sero-
dation of various components of the extracellular tonin (5-HT) in the nucleus accumbens (ACC) of
matrix and the basement membrane, and can anaesthetized rats and found after ischaemia for
hydrolyze type IV and type V collagen, fibronectin, 10 min increased DA and 5-HT release in the ACC
elastin and metamorphic matrix collagen to aggra- 200-fold and 15-fold in the first experiment, respec-
vate the vasogenic brain oedema [12]. Previous stud- tively. This research suggested different brain vulner-
ies have proved that basement membrane as the ability in the dopaminergic and serotonergic neu-
second barrier is important to maintain the integrity rons in the same area of the ACC. And there are
of the BBB. After cerebral ischaemia-reperfusion higher levels of DA and its metabolites in the extra-
injury, TNF induces the expression of C-jun and C-fos cellular fluid of the striatum in acute cerebral
proto-oncogene through a series of transcription fac- ischaemia-reperfusion injury. Electroacupuncture can
tors and facilitates MMP gene transcription. MMPs decrease the accumulation of DA and its metabo-
promote the degradation of extracellular matrix and lites, which may contribute to its effect in protecting
basement membrane to result in brain oedema [34]. the brain from ischaemia-reperfusion injury [56,60].
During H-I, abnormal expression and activation of
MMP result in the opening of the BBB, prevent nor- Intracellular calcium overload and cell
mal cell signalling, and eventually lead to cell death. apoptosis
Neuroprotection after inhibition of MMP (MMP-2 Under normal conditions, intracellular calcium is
and -9) activation has been previously demonstrated mainly stored in mitochondria and sarcoplasmic
in the adult brain after focal cerebral acute and reticulum. In acute cerebral ischaemia-reperfusion, it
chronic ischaemia in both mouse and rat [15,28]. has been found that there was abnormality of
The data showed that there was increased activity Na+/Ca2+ exchange, which is mainly due to metabo-
of MMP-2 and -9 in the ischaemic neuronal nuclei lic acidosis. Furthermore, a lot of free radicals dam-
at 3 h and it significantly attenuated ischaemia- age biofilm, leading to significantly increased per-
induced PARP-1 cleavage, degradation of XRCC1 and meability of the membrane and mitochondrial
elevation of oxidized DNA. This suggested that dysfunction, thus resulting in intracellular calcium
intranuclear MMP activity cleaves PARP-1 and XRCC1, overload [41]. It is well known that there is a Ca2+
and interferes with oxidative DNA repair. This novel overload in destined death neurons in the period of
role for MMPs could contribute to neuronal apopto- ischaemia and immediate reperfusion. Under these
sis in ischaemic injuries [58]. conditions, the mitochondrial Ca2+ pump was sti-
mulated to take up Ca2+, and excessive Ca2+ binds
Toxicity of dopamine with mixtures containing phosphatidate to form
Dopamine (DA) is distributed mainly in the insoluble calcium acid phosphate that could inter-
nigrostriatal system, presents in vesicles when it is fere with mitochondrial oxidative phosphorization
synthesized, and is released by exocytosis during and reduce the production of ATP. On the other hand,
84 Folia Neuropathologica 2011; 49/2
Neuron injury in cerebral hypoxic ischaemia
the free Ca2+ increase in cells can activate many Conclusions
Ca2+-dependent degrading enzymes to result in
H-I is a complicated pathological process which
matrix degradation and cell injury. Meanwhile, the
involves primary injury during the ischaemic period
elevation of cytoplasmic Ca2+ impairs the encoding
and secondary injury during the reperfusion stage.
of action potentials and the dynamics of sodium
Its initial factor is cerebral H-I, but the inducing dam-
channels and function in GABAergic neurons to lead
age after reperfusion consists of many factors. These
to neural excitotoxicity [22].
may be reciprocal causation or influence each other,
Ca2+ overload triggers the elevation of superoxide and finally cause brain oedema and neuronal injury,
radicals and other oxygen radicals. But Ca2+ overload apoptosis, and necrosis. So far, the majority of stud-
in the period of ischaemia and immediate reperfu- ies on cerebral H-I injury come from animal experi-
sion is only a trigger. The later persistent downregu- ments, and some are even from neonatal brain.
lation of L-type calcium channels may be one of the However, although age-dependent differences do
executors of delayed neuronal death [30] (Fig. 2). exist, these experimental data provided important
Apoptosis is an important way of neuronal death enlightenment and reference for clinical therapy, and
after cerebral ischaemia-reperfusion injury, especial- the theoretical basis for clinical study.
ly delayed neuron death. Neuronal apoptosis is relat-
ed to ischaemia type, severity and the time of reper- Acknowledgment
fusion. Immediate early gene is a class of rapid and
Supported by Natural Science Foundation of China
transient expression and takes part in intercellular
(81070957), Natural Science Foundation of Shanxi
signal transmission, growth, differentiation and da-
(2008011082-1).
mage repair, such as c-fos, c-jun, krox-24, jun-B, jun-D
and so on. After 5 min of ischaemia and 2 h of reper- References
fusion, the expression of c-fos, c-jun, and krox-24
1. Anthony L, David J, Sander E. The role of the complement cas-
was higher in the hippocampal CA1 region, which cade in ischemic/ reperfusion injury: implications for neuro-
suggested that they may relate to cell apoptosis in protection. Mol Med 2001; 7: 367-382.
these positions [26]. 2. Arranz AM, Gottlieb M, Pérez-Cerdá F, Matute C. Increased
Caspases are the major executioners of apopto- expression of glutamate transporters in subcortical white
sis. Zhu et al. found that the total level of Bcl-2 matter after transient focal cerebral ischemia. Neurobiol Dis
2010; 37: 156-165.
decreased after H-I in vivo and after ionophore chal-
3. Bates B, Hirt L, Thomas SS, Akbarian S, Le D, Amin-Hanjani S,
lenge in cultured human neuroblastoma (IMR-32) Whalen M, Jaenisch R, Moskowitz MA. Neurotrophin-3 pro-
cells in vitro, which suggested cross-talk between motes cell death induced in cerebral ischemia, oxygen-glucose
excitotoxicity and apoptosis [63]. Cerebral ischaemia deprivation, and oxidative stress: possible involvement of oxy-
significantly upregulated the expression of Fas, FasL gen free radicals. Neurobiol Dis 2002; 9: 24-37.
~
and caspase-3, which induced neurocyte apoptosis. 4. Bolanos JP, Herrero-Mendez A, Fernandez-Fernandez S, Almei-
da A. Linking glycolysis with oxidative stress in neural cells:
Moreover, IL-10 treatment significantly inhibited
a regulatory role for nitric oxide. Biochem Soc Trans 2007; 35
neurocyte apoptosis and the mechanisms seemed (Pt 5): 1224-1227.
related to inhibition of the expression of proapopto- 5. Brown GC. Nitric oxide and neuronal death. Nitric Oxide 2010;
tic gene FasL and caspase-3 [31]. Increased levels of 23: 153-165.
ROS are a major cause of tissue injury after cerebral 6. Büyükuysal RL, Mete B. Anoxia-induced dopamine release
from rat striatal slices: involvement of reverse transport me-
ischaemia, in which ROS can react with cellular
chanism. J Neurochem 1999; 72: 1507-1515.
macromolecules through oxidation and cause the 7. Chen H, Kim GS, Okami N, Narasimhan P, Chan PH. NADPH
cells to undergo necrosis or apoptosis [32]. A flux oxidase is involved in post-ischemic brain inflammation.
enhanced autophagy may be related to apoptosis Neurobiol Dis 2011; 42: 341-348.
since some neurons presenting a high level of 8. Cheung HH, Teves L, Wallace MC, Gurd JW. Increased phos-
autophagy also expressed apoptotic features. These phorylation of the NR1 subunit of the NMDA receptor follow-
ing cerebral ischemia. J Neurochem 2001; 78: 1179-1182.
results suggest that the role of enhanced autophagy
9. Chi OZ, Hunter C, Liu X, Weiss HR. Effects of exogenous exci-
in delayed neuronal death after severe H-I is diffe- tatory amino acid neurotransmitters on blood-brain barrier
rentially linked to apoptosis according to the cerebral disruption in focal cerebral ischemia. Neurochem Res 2009; 34:
region [16]. 1249-1254.
Folia Neuropathologica 2011; 49/2 85
Min-Fang Guo, Jie-Zhong Yu, Cun-Gen Ma
10. Cowell RM, Plane JM, Silverstein FS. Complement activation scavenger edaravone rescues rats from cerebral infarction by
contributes to hypoxic-ischemic brain injury in neonatal rats. attenuating the release of high-mobility group box-1 in neu-
J Neurosci 2003; 23: 9459-9468. ronal cells. J Pharmacol Exp Ther 2009; 329: 865-874.
11. Del Zoppo G, Ginis I, Hallenbeck JM, Iadecola C, Wang X, Feuer- 25. Kimelberg HK, Nestor NB, Feustel PJ. Inhibition of release of
stein GZ. Inflammation and stroke: putative role for cytokines, taurine and excitatory amino acids in ischemia and neuropro-
adhesion molecules and iNOS in brain response to ischemia. tection. Neurochem Res 2004; 29: 267-274.
Brain Pathol 2000; 10: 95-112. 26. Kokubo Y, Matson GB, Liu J, Mancuso A, Kayama T, Sharp FR,
12. Dijkhuizen RM, Asahi M, Wu O, Rosen BR, Lo EH. Rapid break- Weinstein PR. Correlation between changes in apparent diffu-
down of microvascular barriers and subsequent hemorrhagic sion coefficient and induction of heat shock protein, cell-spe-
transformation after delayed recombinant tissue plasminogen cific injury marker expression, and protein synthesis reduction
activator treatment in a rat embolic stroke model. Stroke 2002; on diffusion-weighted magnetic resonance images after tem-
33: 2100-2104. porary focal cerebral ischemia in rats. J Neurosurg 2002; 96:
13. Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischae- 1084-1093.
mic stroke: an integrated view. Trends Neurosci 1999; 22: 27. Kumar A, Mittal R, Khanna HD, Basu S. Free radical injury and
391-397. blood-brain barrier permeability in hypoxic-ischemic ence-
14. Ezquer ME, Valdez SR, Seltzer AM. Inflammatory responses of phalopathy. Pediatrics 2008; 122: e722-727.
the substantia nigra after acute hypoxia in neonatal rats. Exp 28. Li Q, Zhang R, Ge YL, Mei YW, Guo YL. Effects of neuregulin
Neurol 2006; 197: 391-398. on expression of MMP-9 and NSE in brain of ischemia/reper-
15. Fujimoto M, Takagi Y, Aoki T, Hayase M, Marumo T, Gomi M, fusion rat. J Mol Neurosci 2009; 38: 207-215.
Nishimura M, Kataoka H, Hashimoto N, Nozaki K. Tissue 29. Li S, Wang W, Wang C, Tang YY. Possible involvement of
inhibitor of metalloproteinases protect blood-brain barrier dis- NO/NOS signaling in hippocampal amyloid-beta production
ruption in focal cerebral ischemia. J Cereb Blood Flow Metab
induced by transient focal cerebral ischemia in aged rats.
2008; 28: 1674-1685.
Neurosci Lett 2010; 470: 106-110.
16. Ginet V, Puyal J, Clarke PG, Truttmann AC. Enhancement of
30. Li XM, Yang JM, Hu DH, Hou FQ, Zhao M, Zhu XH, Wang Y,
autophagic flux after neonatal cerebral hypoxia-ischemia and
Li JG, Hu P, Chen L, Qin LN, Gao TM. Contribution of downreg-
its region-specific relationship to apoptotic mechanisms. Am
ulation of L-type calcium currents to delayed neuronal death
J Pathol 2009; 175: 1962-1974.
in rat hippocampus after global cerebral ischemia and reperfu-
17. Green DR, Reed JC. Mitochondria and apoptosis. Science 1998;
sion. J Neurosci 2007; 27: 5249-5259.
281: 1309-1312.
31. Liu N, DU HW, Chen RH, Zheng A, Huang HP, Wu ZH. The effect
18. Gurd JW, Bissoon N, Beesley PW, Nakazawa T, Yamamoto T,
of interleukin-10 on neurocyte apoptosis in cerebral ischemia
Vannucci SJ. Differential effects of hypoxia-ischemia on subunit
in rats. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 2007; 23: 498-500.
expression and tyrosine phosphorylation of the NMDA receptor
32. Loh KP, Huang SH, De Silva R, Tan BK, Zhu YZ. Oxidative stress:
in 7- and 21-day-old rats. J Neurochem 2002; 82: 848-856.
apoptosis in neuronal injury. Curr Alzheimer Res 2006; 3:
19. Haddad GG, Jiang C. O2 deprivation in the central nervous sys-
327-337.
tem, on mechanisms of neuronal response, differential sensi-
33. Maiti P, Singh SB, Ilavazhagan G. Nitric oxide system is
tivity and injury. Prog Neurobiol 1993; 40: 277-318.
involved in hypobaric hypoxia-induced oxidative stress in rat
20. Han F, Shioda N, Moriguchi S, Qin ZH, Fukunaga K. Downregu-
brain. Acta Histochem 2010; 112: 222-232.
lation of glutamate transporters is associated with elevation
in extracellular glutamate concentration following rat micros- 34. Montaner J, Molina CA, Monasterio J, Abilleira S, Arenillas JF,
phere embolism. Neurosci Lett 2008; 430: 275-280. Ribó M, Quintana M, Alvarez-Sabín J. Matrix metallopro-
21. Hilton GD, Nunez JL, Bambrick L, Thompson SM, McCarthy MM. teinase-9 pretreatment level predicts intracranial hemorrhagic
Glutamate-mediated excitotoxicity in neonatal hippocampal complications after thrombolysis in human stroke. Circulation
neurons is mediated by mGluR-induced release of Ca++ from 2003; 107: 598-603.
intracellular stores and is prevented by estradiol. Eur J Neurosci 35. Moyanova SG, Mastroiacovo F, Kortenska LV, Mitreva RG,
2006; 24: 3008-3016. Fardone E, Santolini I, Sobrado M, Battaglia G, Bruno V, Nico-
22. Huang L, Chen N, Ge M, Zhu Y, Guan S, Wang JH. Ca2+ and aci- letti F, Ngomba RT. Protective role for type 4 metabotropic glu-
dosis synergistically lead to the dysfunction of cortical tamate receptors against ischemic brain damage. J Cereb
GABAergic neurons during ischemia. Biochem Biophys Res Blood Flow Metab 2011; 31: 1107-1118.
Commun 2010; 394: 709-714. 36. Murotomi K, Takagi N, Mizutani R, Honda TA, Ono M, Takeo S,
23. Katayama Y, Tamura T, Becker DP, Tsubokawa T. Early cellular Tanonaka K. mGluR1 antagonist decreased NADPH oxidase
swelling during cerebral ischemia in vivo is mediated by exci- activity and superoxide production after transient focal cere-
tatory amino acids released from nerve terminals. Brain Res bral ischemia. J Neurochem 2010; 114: 1711-1719.
1992; 577: 121-126. 37. Murotomi K, Takagi N, Takayanagi G, Ono M, Takeo S, Tano-
24. Kikuchi K, Kawahara K, Tancharoen S, Matsuda F, Morimoto Y, naka K. mGluR1 antagonist decreases tyrosine phosphoryla-
Ito T, Biswas KK, Takenouchi K, Miura N, Oyama Y, Nawa Y, tion of NMDA receptor and attenuates infarct size after tran-
Arimura N, Iwata M, Tajima Y, Kuramoto T, Nakayama K, Shige- sient focal cerebral ischemia. J Neurochem 2008; 105:
mori M, Yoshida Y, Hashiguchi T, Maruyama I. The free radical 1625-1634.
86 Folia Neuropathologica 2011; 49/2
Neuron injury in cerebral hypoxic ischaemia
38. Niizuma K, Yoshioka H, Chen H, Kim GS, Jung JE, Katsu M, Oka- 55. Wang WW, Hu SQ, Li C, Zhou C, Qi SH, Zhang GY. Transduced
mi N, Chan PH. Mitochondrial and apoptotic neuronal death PDZ1 domain of PSD-95 decreases Src phosphorylation and
signaling pathways in cerebral ischemia. Biochim Biophys Acta increases nNOS (Ser847) phosphorylation contributing to neu-
2010; 1802: 92-99. roprotection after cerebral ischemia. Brain Res 2010; 1328:
39. Phillis JW, O’Regan MH. Characterization of modes of release 162-170.
of amino acids in the ischemic/reperfused rat cerebral cortex. 56. Xu MS, Fang C, Xu J, Zhang GF, Ge LB. Dynamic changes of
Neurochem Int 2003; 43: 461-467. dopamine and its metabolite levels in the rat striatum after
40. Qin AP, Zhang HL, Qin ZH. Mechanisms of lysosomal proteas- cerebral ischemia-reperfusion and electroacupuncture. Zhen Ci
es participating in cerebral ischemia-induced neuronal death. Yan Jiu 2009; 34: 230-235.
Neurosci Bull 2008; 24: 117-123. 57. Xu XH, Zheng XX, Zhou Q, Li H. Inhibition of excitatory amino
41. Racay P, Tatarkova Z, Chomova M, Hatok J, Kaplan P, Dobro- acid efflux contributes to protective effects of puerarin against
ta D. Mitochondrial calcium transport and mitochondrial dys- cerebral ischemia in rats. Biomed Environ Sci 2007; 20:
function after global brain ischemia in rat hippocampus. 336-342.
Neurochem Res 2009; 34: 1469-1478. 58. Yang Y, Candelario-Jalil E, Thompson JF, Cuadrado E, Estrada EY,
42. Ridder DA, Schwaninger M. NF-kappaB signaling in cerebral Rosell A, Montaner J, Rosenberg GA. Increased intranuclear
ischemia. Neuroscience 2009; 158: 995-1006. matrix metalloproteinase activity in neurons interferes with
43. Riedemann NC, Ward PA. Complement in ischemia reperfusion oxidative DNA repair in focal cerebral ischemia. J Neurochem
injury. Am J Pathol 2003; 162: 363-367. 2010; 112: 134-149.
44. Rodrigo J, Fernández AP, Serrano J, Peinado MA, Martínez 59. Yin W, Signore AP, Iwai M, Cao G, Gao Y, Chen J. Rapidly
A. The role of free radicals in cerebral hypoxia and ischemia. increased neuronal mitochondrial biogenesis after hypoxic-
Free Radic Biol Med 2005; 39: 26-50. ischemic brain injury. Stroke 2008; 39: 3057-3063.
45. Sandoval KE, Witt KA. Blood-brain barrier tight junction 60. Yoshimoto K, Hori M, Shinmen N, Kakiuchi K, Kato H, Sa-
permeability and ischemic stroke. Neurobiol Dis 2008; 32: kabe M, Ikegaya H. Forensic studies of brain vulnerability and
200-219. resistance: ischemia-induced dopamine and serotonin releas-
46. Srivastava AK, Kalita J, Dohare P, Ray M, Misra UK. Studies of es in the rat nucleus accumbens. Leg Med (Tokyo) 2009; 11
free radical generation by neurons in a rat model of cerebral (Suppl 1): S279-281.
venous sinus thrombosis. Neurosci Lett 2009; 450: 127-131. 61. Yu Z, Li S, Lv SH, Piao H, Zhang YH, Zhang YM, Ma H, Zhang J,
47. Szaflarski J, Burtrum D, Silverstein FS. Cerebral hypoxia- Sun CK, Li AP. Hypoxia-ischemia brain damage disrupts brain
ischemia stimulates cytokine gene expression in perinatal cholesterol homeostasis in neonatal rats. Neuropediatrics
rats. Stroke 1995; 26: 1093-1100. 2009; 40: 179-185.
48. Szydlowska K, Tymianski M. Calcium, ischemia and excito- 62. Zhou L, Li F, Xu HB, Luo CX, Wu HY, Zhu MM, Lu W, Ji X,
toxicity. Cell Calcium 2010; 47: 122-129. Zhou QG, Zhu DY. Treatment of cerebral ischemia by disrupting
49. Takagi N, Besshoh S, Morita H, Terao M, Takeo S, Tanonaka K. ischemia-induced interaction of nNOS with PSD-95. Nat Med
Metabotropic glutamate mGlu5 receptor-mediated serine 2010; 16: 1439-1443.
phosphorylation of NMDA receptor subunit NR1 in hippocam- 63. Zhu C, Hallin U, Ozaki Y, Grandér R, Gatzinsky K, Bahr BA,
pal CA1 region after transient global ischemia in rats. Eur Karlsson JO, Shibasaki F, Hagberg H, Blomgren K. Nuclear
J Pharmacol 2010; 644: 96-100. translocation and calpain-dependent reduction of Bcl-2 after
50. Takeuchi H, Jin S, Suzuki H, Doi Y, Liang J, Kawanokuchi J, neonatal cerebral hypoxia-ischemia. Brain Behav Immun 2010;
Mizuno T, Sawada M, Suzumura A. Blockade of microglial glu- 24: 822-830.
tamate release protects against ischemic brain injury. Exp
Neurol 2008; 214: 144-146.
51. Ten VS, Yao J, Ratner V, Sosunov S, Fraser DA, Botto M,
Sivasankar B, Morgan BP, Silverstein S, Stark R, Polin R, Van-
nucci SJ, Pinsky D, Starkov AA. Complement component c1q
mediates mitochondria-driven oxidative stress in neonatal
hypoxic-ischemic brain injury. J Neurosci 2010; 30: 2077-2087.
52. Van der Vliet A, Smith D, O’Neill CA, Kaur H, Darley-Usmar V,
Cross CE, Halliwell B. Interactions of peroxynitrite with human
plasma and its constituents: oxidative damage and antioxi-
dant depletion. Biochem J 1994; 303: 295-301.
53. Verma R, Mishra V, Sasmal D, Raghubir R. Pharmacological
evaluation of glutamate transporter 1 (GLT-1) mediated neuro-
protection following cerebral ischemia/reperfusion injury. Eur
J Pharmacol 2010; 638: 65-71.
54. Wang CX, Shuaib A. Involve of inflammatory cytokines in cen-
tral nervous system injury. Prog Neurobiol 2002; 67: 161-172.
Folia Neuropathologica 2011; 49/2 87
You might also like
- Pathophysiology of Epilepsy: An Updated Review: International Journal of Medical and Health ResearchDocument5 pagesPathophysiology of Epilepsy: An Updated Review: International Journal of Medical and Health ResearchGayathiri GovindarajuNo ratings yet
- Ischemic StrokeDocument8 pagesIschemic StrokeRinavi Adrin RirinNo ratings yet
- B Signaling in Cerebral Ischemia: Review NFDocument12 pagesB Signaling in Cerebral Ischemia: Review NFDefi DestyawenyNo ratings yet
- Neuroprotection by Alpha 2-Adrenergic Agonists inDocument8 pagesNeuroprotection by Alpha 2-Adrenergic Agonists inB AuNo ratings yet
- Lau 2010Document18 pagesLau 2010Oris WicaksonoNo ratings yet
- Novel Strategies for Neuro-Protection after Traumatic Brain InjuryDocument26 pagesNovel Strategies for Neuro-Protection after Traumatic Brain InjuryErlin IrawatiNo ratings yet
- TFAMDocument12 pagesTFAMKurtisNo ratings yet
- Intensive Care Treatment in Traumatic Brain Injury: The Epidemiology of Head TraumaDocument6 pagesIntensive Care Treatment in Traumatic Brain Injury: The Epidemiology of Head TraumaDwi Utari JNo ratings yet
- Glutamate, Calcium and Magnesium Roles in Secondary Brain InjuryDocument16 pagesGlutamate, Calcium and Magnesium Roles in Secondary Brain InjuryAndrea Guzman BotiaNo ratings yet
- Jurnal PDFDocument9 pagesJurnal PDFFerdy Arif FadhilahNo ratings yet
- Khoshnam2017 Article PathogenicMechanismsFollowingIDocument20 pagesKhoshnam2017 Article PathogenicMechanismsFollowingILovin BiancaNo ratings yet
- Pathophysiology of EpilepsyDocument16 pagesPathophysiology of EpilepsyYexalen Zazil100% (1)
- Molecular Pathophysiology of StrokeDocument10 pagesMolecular Pathophysiology of StrokeKahubbi Fatimah Wa'aliyNo ratings yet
- Post-Ischemic in Ammation in The Brain: Takashi Shichita, Ryota Sakaguchi, Mayu Suzuki and Akihiko YoshimuraDocument7 pagesPost-Ischemic in Ammation in The Brain: Takashi Shichita, Ryota Sakaguchi, Mayu Suzuki and Akihiko YoshimuraAlex GasnasNo ratings yet
- Neurorestoration StrokeDocument11 pagesNeurorestoration StrokeHastrina MailaniNo ratings yet
- New Insights Into Migraine Pathophysiology: Margarita Sanchez-del-Rio, Uwe Reuter and Michael A. MoskowitzDocument5 pagesNew Insights Into Migraine Pathophysiology: Margarita Sanchez-del-Rio, Uwe Reuter and Michael A. MoskowitzΖέτα ΤσίρκαNo ratings yet
- α‐lipoic acid protects against cerebral ischemia - reperfusion‐induced injury in ratsDocument7 pagesα‐lipoic acid protects against cerebral ischemia - reperfusion‐induced injury in ratsranu anggaraNo ratings yet
- Pathophysiology of Encephalopathy: N. G.F. ADocument7 pagesPathophysiology of Encephalopathy: N. G.F. Adoğancan uzunNo ratings yet
- Pathophysiology, Bioelectricidad, Review Stroke TINS99Document7 pagesPathophysiology, Bioelectricidad, Review Stroke TINS99Carla Saramy MachillandaNo ratings yet
- Pa Tho Physiology of Traumatic Brain Injury2Document22 pagesPa Tho Physiology of Traumatic Brain Injury2n2s_nqNo ratings yet
- Current Concepts in The Biochemical Mechanisms of Glaucomatous NeurodegenerationDocument0 pagesCurrent Concepts in The Biochemical Mechanisms of Glaucomatous NeurodegenerationlovehopeNo ratings yet
- Acupuncture and Neuroregeneration in Ischemic StrokeDocument11 pagesAcupuncture and Neuroregeneration in Ischemic Strokemartin_salineNo ratings yet
- Kynurenine pathway inhibition as a therapeutic strategy for neuroprotectionDocument35 pagesKynurenine pathway inhibition as a therapeutic strategy for neuroprotectionMészáros - Molnár KingaNo ratings yet
- Alzheimer PDFDocument8 pagesAlzheimer PDFRoberto SunkelNo ratings yet
- Differences: Biological Between Ischemia, Hypoglycemia, EpilepsyDocument9 pagesDifferences: Biological Between Ischemia, Hypoglycemia, EpilepsyAyie JayaNo ratings yet
- Excitotoxicity and neuronal death mechanisms in epilepsyDocument8 pagesExcitotoxicity and neuronal death mechanisms in epilepsyKhrîîz Ëvïi BïbiBüûNo ratings yet
- Epilepsy AssignmentDocument58 pagesEpilepsy Assignmentnasir khanNo ratings yet
- Zhang 2019Document12 pagesZhang 2019McShadiq ZikryNo ratings yet
- Encefalopatia Neomnatal en PotrosDocument10 pagesEncefalopatia Neomnatal en PotrosAndrea Roman chavezNo ratings yet
- 2010 11 E184-E193 Maria Delivoria-Papadopoulos and Peter J. MarroDocument12 pages2010 11 E184-E193 Maria Delivoria-Papadopoulos and Peter J. MarroAle JimenezNo ratings yet
- Trauma Encefalico IDocument7 pagesTrauma Encefalico IMarNo ratings yet
- Neuroprotective Mechanisms of S-allyl-L-cysteine in Neurological Disease (Review)Document5 pagesNeuroprotective Mechanisms of S-allyl-L-cysteine in Neurological Disease (Review)ravajo9581No ratings yet
- Temporal Lobe Epilepsy - Pathophysiology and Mechanisms: EditorialDocument2 pagesTemporal Lobe Epilepsy - Pathophysiology and Mechanisms: EditorialMahesa Kurnianti PutriNo ratings yet
- 97 312 PDFDocument5 pages97 312 PDFdupuytrenNo ratings yet
- Brain Energy RescueDocument25 pagesBrain Energy RescueMaria Vitória Cota de AbreuNo ratings yet
- Review ArticleDocument16 pagesReview ArticleJessica M González CoronaNo ratings yet
- Neurometabolic CascadeDocument8 pagesNeurometabolic CascadeTim BonineNo ratings yet
- Alpha7 Nicotinic Acetylcholine Receptor Is A Target in Pharmacology and ToxicologyDocument20 pagesAlpha7 Nicotinic Acetylcholine Receptor Is A Target in Pharmacology and ToxicologyJean Pierre Chastre LuzaNo ratings yet
- Perspective of Synaptic Protection After Post-Infarction Treatment With StatinsDocument9 pagesPerspective of Synaptic Protection After Post-Infarction Treatment With StatinsDrGasnasNo ratings yet
- Journal of Neurochemistry Doi: 10.1111/j.1471-4159.2009.06433.xDocument16 pagesJournal of Neurochemistry Doi: 10.1111/j.1471-4159.2009.06433.xJulie Susan SamNo ratings yet
- Melatonina Como Neuroprotector PDFDocument17 pagesMelatonina Como Neuroprotector PDFCiarol BorbonNo ratings yet
- 119 - Perinatal AsphyxiaDocument10 pages119 - Perinatal Asphyxiaramla abdiNo ratings yet
- Lithium Enhances Post Stroke Blood Brain Barrier Integrity Act - 2020 - NeurophDocument14 pagesLithium Enhances Post Stroke Blood Brain Barrier Integrity Act - 2020 - NeurophClaudiaNo ratings yet
- 10 Terapie S-NODocument10 pages10 Terapie S-NOdodutaNo ratings yet
- Cerebral EdemaDocument5 pagesCerebral EdemaAdilah AdeebNo ratings yet
- Magnesium Ion Influx Reduces Neuroinflammation in Ab Precursor Protein/presenilin 1 Transgenic Mice by Suppressing The Expression of Interleukin-1bDocument14 pagesMagnesium Ion Influx Reduces Neuroinflammation in Ab Precursor Protein/presenilin 1 Transgenic Mice by Suppressing The Expression of Interleukin-1bkleberttoscanoNo ratings yet
- Department of Physiology Master of Science in PhysiologyDocument77 pagesDepartment of Physiology Master of Science in Physiologyrichardmd2100% (1)
- Current Status and Challenges of Stem Cell Treatment For Alzheimer's DiseaseDocument19 pagesCurrent Status and Challenges of Stem Cell Treatment For Alzheimer's DiseaseHelical Nail FemurNo ratings yet
- Dhami Et Al-2019-Journal of Neurochemistry PDFDocument18 pagesDhami Et Al-2019-Journal of Neurochemistry PDFJawad A. KhanNo ratings yet
- 2010 Hypoxic Ischemic Brain Injury Pathophysiology Neuropathology and Mechanisms KM Busl PDFDocument9 pages2010 Hypoxic Ischemic Brain Injury Pathophysiology Neuropathology and Mechanisms KM Busl PDFDaniel OUNo ratings yet
- Vannucci 1997Document13 pagesVannucci 1997ale marilNo ratings yet
- Curcumin Provides Neuroprotection After Spinal Cord Injury: Ó 2009 Elsevier Inc. All Rights ReservedDocument10 pagesCurcumin Provides Neuroprotection After Spinal Cord Injury: Ó 2009 Elsevier Inc. All Rights ReservedanthonyjoelleeNo ratings yet
- RETRACTED DUSP1 Alleviates Cerebral Ischaemia Reperfusion Injur - 2018 - Life SDocument12 pagesRETRACTED DUSP1 Alleviates Cerebral Ischaemia Reperfusion Injur - 2018 - Life Sronaldquezada038No ratings yet
- Modulation of Brain Hyperexcitability: Potential New Therapeutic Approaches in Alzheimer's DiseaseDocument37 pagesModulation of Brain Hyperexcitability: Potential New Therapeutic Approaches in Alzheimer's DiseaseVicko SuswidiantoroNo ratings yet
- Pharmacological Strategies For The Prevention of Perinatal Brain DamageDocument15 pagesPharmacological Strategies For The Prevention of Perinatal Brain DamageconstantinoploqweNo ratings yet
- FlavonoidsDocument9 pagesFlavonoidspaulo saNo ratings yet
- Bayazid 2021Document11 pagesBayazid 2021Jocilene Dantas Torres NascimentoNo ratings yet
- Neurotransmission: Proceedings of the Sixth International Congress of PharmacologyFrom EverandNeurotransmission: Proceedings of the Sixth International Congress of PharmacologyLiisa AhteeNo ratings yet
- Basic Neurochemistry: Principles of Molecular, Cellular, and Medical NeurobiologyFrom EverandBasic Neurochemistry: Principles of Molecular, Cellular, and Medical NeurobiologyNo ratings yet
- Biochemical and Pharmacological Roles of Adenosylmethionine and the Central Nervous System: Proceedings of an International Round Table on Adenosylmethionine and the Central Nervous System, Naples, Italy, May 1978From EverandBiochemical and Pharmacological Roles of Adenosylmethionine and the Central Nervous System: Proceedings of an International Round Table on Adenosylmethionine and the Central Nervous System, Naples, Italy, May 1978Vincenzo ZappiaNo ratings yet
- Grafik CDCDocument10 pagesGrafik CDCArief Budi LesmanaNo ratings yet
- 2 To 20 Years: Girls Body Mass Index-For-Age Percentiles: Date Age Weight Stature Bmi CommentsDocument1 page2 To 20 Years: Girls Body Mass Index-For-Age Percentiles: Date Age Weight Stature Bmi CommentsRahayu AgustiaNo ratings yet
- Status Epilepticus: Beyond Guidelines: Helen Basu, Finbar O'CallaghanDocument9 pagesStatus Epilepticus: Beyond Guidelines: Helen Basu, Finbar O'CallaghanDian100% (1)
- Laparoscopic Tissue: Approxima TionDocument4 pagesLaparoscopic Tissue: Approxima TionDianNo ratings yet
- Tem Cell Ther in HDDocument5 pagesTem Cell Ther in HDDianNo ratings yet
- Brown (2010)Document14 pagesBrown (2010)DianNo ratings yet
- Hirschsprung 1socaDocument34 pagesHirschsprung 1socaDianNo ratings yet
- High-Risk Newborn Necrotizing Enterocolitis GuideDocument3 pagesHigh-Risk Newborn Necrotizing Enterocolitis GuideDianNo ratings yet
- Yu (2003)Document3 pagesYu (2003)DianNo ratings yet
- Penting Pge2 Pada AnakDocument6 pagesPenting Pge2 Pada AnakDianNo ratings yet
- BODIPY 493/503 Staining of Neutral Lipid Droplets For Microscopy and Quantification by Flow CytometryDocument5 pagesBODIPY 493/503 Staining of Neutral Lipid Droplets For Microscopy and Quantification by Flow CytometryCong Trang MaiNo ratings yet
- Cell Culture TechnologyDocument174 pagesCell Culture TechnologySabina HajizadaNo ratings yet
- Encyclopedia of Molecular Pharmacology 3rd Ed 2021Document1,625 pagesEncyclopedia of Molecular Pharmacology 3rd Ed 2021Josemar Sena BatistaNo ratings yet
- Free Radicals and AntioxidantsDocument16 pagesFree Radicals and AntioxidantsPRIYANGA. PNo ratings yet
- Lec-3-Dna Replication, Transcription, and TranslationDocument11 pagesLec-3-Dna Replication, Transcription, and TranslationGreatel Elijah TorregosaNo ratings yet
- EritropoesisDocument15 pagesEritropoesisFitriyani Dewi SuwandhiNo ratings yet
- GPCR Mediated Control of Calcium Dynamics A Systems PerspectiveDocument13 pagesGPCR Mediated Control of Calcium Dynamics A Systems PerspectiveLeonel LedezmaNo ratings yet
- Biology EOC: 50 Key Facts to Ace the ExamDocument3 pagesBiology EOC: 50 Key Facts to Ace the ExamThefryboioNo ratings yet
- Structure and Functions of HaemoglobinDocument2 pagesStructure and Functions of HaemoglobinKrissy KayNo ratings yet
- Chapter Seven The Behavior of Proteins: Enzymes, Mechanisms, and ControlDocument25 pagesChapter Seven The Behavior of Proteins: Enzymes, Mechanisms, and ControlCalapati, Jhon Rovic R.100% (1)
- Fonc 13 1226289Document19 pagesFonc 13 1226289Shady tantawyNo ratings yet
- Edtpa Lesson Plans 1Document16 pagesEdtpa Lesson Plans 1api-455073563No ratings yet
- Science 7 Chapter 1 - Cells 1.3-1.4Document13 pagesScience 7 Chapter 1 - Cells 1.3-1.4Hương Minh Phạm QuinnNo ratings yet
- IB Biology D.3 Liver NotesDocument7 pagesIB Biology D.3 Liver NotesDilip Pandurang PattilNo ratings yet
- NK Cells MemoryDocument8 pagesNK Cells MemoryDanielaNo ratings yet
- MCQs On Respiration in PlantsDocument7 pagesMCQs On Respiration in PlantsSriramulu JaichandarNo ratings yet
- Bioenergetics of Exercise and TrainingDocument62 pagesBioenergetics of Exercise and Trainingswordplay716No ratings yet
- MEDBIO KROK-1 English 2019-2020Document65 pagesMEDBIO KROK-1 English 2019-2020Катерина КабишNo ratings yet
- ATP Student PDFDocument5 pagesATP Student PDFtvuongpham0% (1)
- CH 18 Lecture PresentationDocument127 pagesCH 18 Lecture PresentationMaski03No ratings yet
- Genetic Code ExplainedDocument15 pagesGenetic Code ExplainedGe'sh Na'shy TyneNo ratings yet
- Problem Sheet Module 1 QuestionsDocument5 pagesProblem Sheet Module 1 QuestionsJui-Chi ChenNo ratings yet
- EDEXCEL- BIOLOGY- IAL Stem Cells: Natural Reservoir and Unique AbilitiesDocument12 pagesEDEXCEL- BIOLOGY- IAL Stem Cells: Natural Reservoir and Unique AbilitiesSwarnapaliliyanageNo ratings yet
- Tissue Types and FunctionsDocument30 pagesTissue Types and FunctionsEspinosa Mary Dianne V.No ratings yet
- Biology A2 NotesDocument38 pagesBiology A2 NotesMohamed Muawwiz Kamil100% (1)
- Chapter 28 AdrenocorticoidsDocument36 pagesChapter 28 AdrenocorticoidsCapuNo ratings yet
- Biology PosterDocument1 pageBiology PosterNoobmaster666No ratings yet
- 2017 OL Cell Cycle Exam ReviewDocument3 pages2017 OL Cell Cycle Exam ReviewAnne Romo50% (8)
- Cytogenetics and Molecular Cytogenetics - Medical Genomics and Proteomics - Thomas Liehr - CRC Press (2022)Document383 pagesCytogenetics and Molecular Cytogenetics - Medical Genomics and Proteomics - Thomas Liehr - CRC Press (2022)julio castilloNo ratings yet
- Histology of Nervous TissueDocument40 pagesHistology of Nervous TissueSHARON MARIA SUNNYNo ratings yet