Professional Documents
Culture Documents
Ang LW Et Al. Epidemiology and Control of Hand, Foot and Mouth Disease in Singapore, 2001-2007. Ann Acad Med Singapore 2009 38 106-12
Uploaded by
chaer assofiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ang LW Et Al. Epidemiology and Control of Hand, Foot and Mouth Disease in Singapore, 2001-2007. Ann Acad Med Singapore 2009 38 106-12
Uploaded by
chaer assofiCopyright:
Available Formats
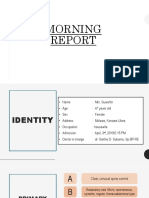
106 Epidemiology and Control of HFMD in Singapore, 2001-2007—Li Wei Ang et al
Original Article
Epidemiology and Control of Hand, Foot and Mouth Disease in Singapore,
2001-2007
Li Wei Ang,1Msc (Statistics), Benjamin KW Koh,2MBBS, MPH, Kwai Peng Chan,3MBBS, Dip Bact, FRCPA, Lian Tee Chua,1BSc (Nursing),
Lyn James,1MBBS, MMed, FAMS, Kee Tai Goh,4MSc (PH), MD, FAMS
Abstract
Introduction: We reviewed the epidemiology of hand, foot and mouth disease (HFMD) in
Singapore after the 2000 epidemic caused by Enterovirus 71 (EV71), with particular reference
to the cyclical pattern, predominant circulating enteroviruses and impact of prevention and
control measures in preschool centres. Materials and Methods: We analysed the epidemiological
data from all clinical cases and deaths of HFMD diagnosed by medical practitioners and notified
to the Ministry of Health, as well as laboratory data on enteroviruses detected among HFMD
patients maintained by the Department of Pathology, Singapore General Hospital, and the
Microbiology Laboratory, KK Women’s and Children’s Hospital from 2001 to 2007. Results:
The incidence rate was highest in the 0 to 4 years old age group, with males being predominant.
Three deaths were reported between January and February 2001. Nationwide epidemics
occurred periodically; the predominating circulating virus was Coxsackievirus A16 (CA16) in
the 2002, 2005 and 2007 epidemics, and EV71 in the 2006 epidemic. During the epidemic years
between 2005 and 2007, 2 peaks were observed. The number of institutional outbreaks had
increased 10-fold from 167 in 2001 to 1723 in 2007, although most of these outbreaks were rapidly
brought under control with an attack rate of less than 10%. Conclusion: HFMD remains an
important public health problem in Singapore with the annual incidence rate per 100,000
population increasing from 125.5 in 2001 to 435.9 in 2007, despite stringent measures taken in
preschool centres to prevent the transmission of infection. A high degree of vigilance should be
maintained over the disease situation, in particular, surveillance of EV 71 which continues to
cause severe complications and deaths in the region.
Ann Acad Med Singapore 2009;38:106-12
Key words: Coxsackievirus A16, Enterovirus 71, Epidemic, Preschools
Introduction In Singapore, the first outbreak of HFMD was reported
Hand, foot and mouth disease (HFMD) is a common in June to July 1970, but the aetiological agent was
childhood viral infection, which is typically mild and self- unknown.2 Two other outbreaks associated with CA16
limiting. It is characterised by a brief prodromal fever, were reported during the period between September 1972
followed by pharyngitis, mouth ulcers and rash on the and January 1973, and between September and December
hands and feet. The disease is caused by numerous members 1981.3 The largest epidemic of HFMD caused by EV71
of the Enterovirus genus of the family Picornaviridae e.g. with 3790 cases and 4 deaths occurred in Singapore between
Coxsackievirus type A (CA) and Enterovirus 71 (EV71), September and December 2000. The main pathological
and the clinical features are indistinguishable. Transmission findings at autopsy were interstitial pneumonitis,
occurs from person to person through direct contact with myocarditis and encephalitis.4
saliva, faeces, vesicular fluid or respiratory droplets of an The purpose of this study was to review the epidemiology
infected person and indirectly by contaminated articles.1 of HFMD after the 2000 epidemic in Singapore, with
1
Communicable Diseases Division, Ministry of Health, Singapore
2
Hospital Services Division, Ministry of Health, Singapore
3
Department of Pathology, Singapore General Hospital, Singapore
4
Office of the Director of Medical Services, Ministry of Health, Singapore
Address for Correspondence: Ang Li Wei, Communicable Diseases Division, Ministry of Health, Singapore, College of Medicine Building, 16 College Road,
Singapore 169854.
Email: ang_li_wei@moh.gov.sg
Annals Academy of Medicine
Epidemiology and Control of HFMD in Singapore, 2001-2007—Li Wei Ang et al 107
particular reference to determine the seasonality or cyclical for categorical data. Differences between the age-gender-
pattern, the predominant circulating enteroviruses and the standardised incidence rates of the ethnic groups based on
impact of prevention and control measures in preschools. direct method were computed and tested for statistical
significance using the Z-test.8 A P value less than 0.05 was
Materials and Methods considered statistically significant.
We reviewed the records of all cases of HFMD notified
Results
to the Ministry of Health (MOH) by medical practitioners
between 2001 and 2007. The clinical criteria for diagnosis Morbidity
and notification of HFMD are provided in a guidebook that Nationwide epidemics were reported in 2002, 2005,
is made available to all medical practitioners.1 2006 and 2007 with 16,228 cases, 15,256 cases, 15,282
Childcare centres, preschools and primary schools are cases and 20,003 cases, respectively, compared with 5,187
also required to notify MOH via facsimile of any HFMD cases in 2001, 5,603 cases in 2003 and 6,411 cases in 2004.
outbreaks in their institutions. An outbreak is defined as 2 The incidence rates ranged from 125.5 per 100,000 in 2001
or more cases of HFMD with onset of illness occurring to 435.9 per 100,000 in 2007 (Table 1).
within 10 days in the same institution for investigation and The incidence rate was highest in the 0 to 4 years old age
management by MOH. group, and this had increased steeply from 1460.5 per
Laboratory notifications of enteroviruses identified in 100,000 population in 2001 to 5975.5 per 100,000
stool samples, throat and rectal swabs and swabs from population in 2007 (Table 1). A gradual decline in the
vesicular fluid and oral ulcers randomly collected from proportion of cases in this age group was observed during
outpatient and inpatient cases of HFMD at KK Women’s the period of review. It constituted 74.5% of the reported
and Children’s Hospital (KKH) and tested at the Virology cases in 2001, but dropped to 62.2% in 2007. There was a
Laboratory of the Department of Pathology, Singapore corresponding shift in the age distribution of the HFMD
General Hospital, were collated. Samples included those cases in older children aged 5 to 9 years old. The proportion
obtained from HFMD cases at childcare centres, of cases in this age group increased significantly from
kindergartens and schools with parental consent. 17.0% in 2001 to 26.2% in 2007 (P <0.05, χ2 test for trend).
The classical diagnostic method was adopted; There was a male predominance of HFMD cases, with a
enteroviruses cultured from the samples were typed by male-to-female ratio between 1.3:1 and 1.6:1 (Table 2).
micro-neutralisation tests using Lim-Benyesh-Melnick A- Males had a significantly higher incidence rate of HFMD
H equine antiserum pools (World Health Organization, compared to females, with the relative risk ranging from
Statens Serum Institut, Copenhagen, Denmark), equine 1.2 in 2006 to 1.6 in 2003.
antiserum pools (Rijksinstituut voor Volksgesondheid en Among the 3 major ethnic groups, the incidence rate
Milieuhygiene, Bilthoven, the Netherlands), rabbit 385JS among the Chinese was significantly higher than that of
HEV71-specific polyclonal antiserum (Victorian Infectious Indians (Table 2). The incidence rate of HFMD cases
Diseases Reference Laboratory, Melbourne, Australia), among Malays was higher than that of Chinese in the last
and rabbit or monkey antisera specific for CA serotypes 2 years, and the difference between the age-gender-
(National Institutes of Health, Bethesda, MD).4 Rapid standardised incidence rates was statistically significant.
diagnosis for enterovirus polymerase chain reaction (PCR) During the epidemic year in 2002 when CA16 was the
was performed on nasopharyngeal aspirate/throat swab.1 predominant circulating enterovirus, there was only 1
The molecular methods used have been described single peak in May, whereas in the other epidemic years, 2
previously.5,6 Since April 2006, selected stool samples, peaks were observed in March and October 2005, March
vesicle and throat swabs were also tested at the Microbiology and August 2006, and May and August 2007, with the first
Laboratory, KKH, using the reverse transcriptase-PCR peak consistently higher than the second (Fig. 1). There
method for specific identification of EV71.7 were 2 seasonal troughs, one occurring during the school
For the calculation of age-specific and ethnic-specific holidays around the middle of the year and the other at the
incidence rates, the denominators used were the estimated end of the year.
mid-year population of the corresponding years from the During the EV71-associated HFMD epidemic between
Singapore Department of Statistics. The attack rates of March and April 2006, 1.8% of the cases were hospitalised.
institutional outbreaks were calculated based on the This was more than twice higher than those epidemics
population of students and staff provided by the affected caused by CA16 (0.8% of the cases were hospitalised
institutions. Statistical analyses were performed using SPSS between March and April 2005, and 0.7% between April
Software Version 15.0 (SPSS Chicago, IL). We used χ2 test and May 2007).
February 2009, Vol. 38 No. 2
108 Epidemiology and Control of HFMD in Singapore, 2001-2007—Li Wei Ang et al
Table 1. Age-Specific Incidence Rates (Per 100,000 Population) of Reported HFMD Cases, 2001-2007
Age group (y) 2001 2002 2003 2004 2005 2006 2007
0–4 1640.5 (74.5) 5256.8 (74.7) 1830.2 (72.3) 2111.6 (71.1) 4807.7 (66.7) 4649.0 (63.1) 5975.5 (62.2)
5–9 330.3 (17.0) 1127.5 (18.5) 447.1 (20.7) 541.4 (21.3) 1485.8 (24.4) 1474.1 (24.0) 2140.8 (26.2)
10 – 14 47.1 (2.4) 165.3 (2.8) 44.7 (2.2) 70.8 (3.0) 194.8 (3.5) 269.5 (4.8) 347.4 (4.7)
15 – 24 13.0 (1.6) 33.7 (1.3) 9.0 (1.0) 13.9 (1.3) 33.4 (1.4) 50.8 (2.3) 58.2 (2.1)
25 – 34 15.7 (2.7) 31.5 (1.7) 15.5 (2.3) 14.2 (1.9) 43.8 (2.5) 60.8 (3.6) 60.6 (2.9)
35 – 44 10.2 (1.5) 19.3 (0.9) 9.6 (1.3) 9.0 (1.1) 26.9 (1.3) 38.0 (1.9) 43.0 (1.7)
45 – 54 2.6 (0.3) 3.8 (0.1) 1.8 (0.2) 1.7 (0.2) 3.8 (0.2) 5.7 (0.2) 4.9 (0.2)
55+ 0.4 (0.04) 0.9 (0.03) 0.3 (0.04) 1.0 (0.1) 1.1 (0.05) 1.9 (0.1) 1.1 (0.04)
Total 125.5 (100.0) 388.6 (100.0) 136.2 (100.0) 153.9 (100.0) 357.6 (100.0) 347.2 (100.0) 435.9 (100.0)
Figures in brackets refer to percentage of total cases in the corresponding year.
Table 2. Gender and Ethnic-Specific Incidence Rates (Per 100,000 Population) of Reported HFMD Cases, 2001-2007
Residents 2001 2002 2003 2004 2005 2006 2007
Chinese
Male 182.5 583.8 212.4 221.1 518.2 464.1 595.2
Female 129.1 393.0 124.7 162.4 391.5 360.1 453.6
Malay
Male 136.6 578.9 166.4 209.5 439.3 549.8 733.5
Female 104.0 392.2 108.0 170.9 332.1 442.8 562.3
Indian
Male 37.4 181.8 51.9 64.4 137.7 173.8 270.0
Female 32.4 127.3 38.1 42.1 105.3 144.0 215.3
Others
Male 316.0 1545.8 961.4 722.8 876.9 759.7 902.9
Female 230.8 810.7 585.4 419.9 619.4 535.9 723.8
Foreigners
Male 58.1 40.2 16.2 6.1 75.9 93.4 124.3
Female 47.6 31.3 7.9 5.2 75.4 91.2 125.1
Total
Male 142.5 454.5 167.4 174.2 399.3 383.2 476.8
Female 107.3 320.1 104.2 133.1 315.0 310.0 392.7
Mortality aetiology. EV (untypable) was isolated from the intestine.
Three HFMD-associated deaths were reported in January The last fatal case was an 11-month-old Chinese boy whose
and February 2001 when there was no nationwide epidemic condition deteriorated rapidly with poor appetite and
of HFMD.9 The first death involved a 4-year-old Chinese lethargy. He vomited and developed a fit on the way to
boy who collapsed suddenly at home and died on arrival at hospital. Clinically, he died of pulmonary and cerebral
the Emergency Department. Postmortem examination oedema. No postmortem was done. Since then, no further
showed brainstem encephalitis. EV71 was isolated from deaths from HFMD had been reported to MOH.
the tracheal swab, brain and intestine. The second death
was an 11-month-old Malay boy who vomited and suddenly Institutional Outbreaks
collapsed at home. The main postmortem findings were The number of institutional HFMD outbreaks reported in
myocarditis and pneumonitis consistent with a viral childcare centres, kindergartens and schools increased
Annals Academy of Medicine
Epidemiology and Control of HFMD in Singapore, 2001-2007—Li Wei Ang et al 109
100 1800
90 1600
80 1400 x
70
1200
Number of outbreaks
Attack rate (%)
60
1000
50
800
40
600
30
20 400
10 200
0 0
2001 2002 2003 2004 2005 2006 2007
Attack rate (%) < 10 10 - 20 21 - 30 31 - 40 41 - 50 >50
Fig. 1. Monthly distribution of reported cases of HFMD, 2001-2007.
Fig. 2. Institutional outbreaks of HFMD by attack rate (%), 2001-2007.
25
20
EV71
Number of isolates
15
10
0
r l r l r l
05 eb a pr a y un Ju Aug Sep Oct ov Dec 006 Feb Ma Apr a y Jun Ju Aug Sep Oct ov Dec 007 Feb Ma Apr a y Jun Ju Aug Sep Oct ov Dec
20 F M A M J N 2 M N 2 M N
n- n- n-
Ja Ja Ja
25
20
CA16
Number of isolates
15
10
5 Fig. 3. Monthly isolation/detection of CA16 and
EV71, January 2005 to December 2007.
0
r l r l r l
0 05 Feb Ma Apr a y Jun Ju Aug Sep Oct ov Dec 006 Feb Ma Apr a y Jun Ju Aug Sep Oct ov Dec 007 Feb Ma Apr a y Jun Ju Aug Sep Oct ov Dec
-2 M N 2 M N 2 M N
n n- n-
Ja Ja Ja
from 167 in 2001 to 539 in 2002, then declined to 169 in and both CA6 and EV71 were also in almost similar
2003, and thereafter increased rapidly to 1723 in 2007 (Fig. proportions in 2006. In fact, EV71 was detected only in the
2). Overall, the number of institutional outbreaks increased second half of 2005 and continued into 2006. Other
10-fold since 2001. enteroviruses isolated were CA10, CA2, CA4, CA5, CA9,
echoviruses, CB3, CB4 and CB5.
Most of the outbreaks occurred in childcare centres
where children aged between 2 and 6 years old congregate Monthly isolation showed that the 2 peaks during the last
(44.8% to 86.4% of the reported cases), followed by 3 epidemic years were associated with the same enterovirus;
kindergartens attended by children aged between 5 and 6 CA16 in 2005 (EV71 came into circulation after the second
years old (13.0% to 34.1%). While the number of peak was over), EV71 in 2006 and CA16 in 2007 (Fig. 3).
institutional outbreaks had been increasing, the majority
Discussion
had an attack rate of less than 10%.
The 2 main enteroviruses causing nationwide epidemics
Viral Detection of HFMD in Singapore were CA16 and EV71. CA16 was
The majority of the enteroviruses detected from the the predominant strain circulating during the epidemic in
HFMD cases were CA16 in 2002, 2004 and 2007, while 2002. It re-emerged in 2004 to cause another epidemic in
EV71 was predominant in 2001 and 2003 (Table 3). Both 2005 and 2007. In the case of EV71, although it was the
CA16 and EV71 were almost equally distributed in 2005, predominant strain detected in 2001, 2003 and 2005/6, it
February 2009, Vol. 38 No. 2
110 Epidemiology and Control of HFMD in Singapore, 2001-2007—Li Wei Ang et al
Table 3. Percent Distribution of Non-polio Enteroviruses Among Positive Isolates from HFMD Cases, 2001-2007
2001 2002 2003 2004 2005 2006 2007
No. tested 305 255 469 66 183 339 328
No. positive 178 210 50 21 76 145 94
Enteroviruses
CA2 2.2 0.0 0.0 14.3 0.0 3.5 4.3
CA4 10.7 0.0 6.0 4.7 0.0 2.8 0.0
CA5 0.0 0.0 0.0 0.0 0.0 0.7 0.0
CA6 18.5 11.9 0.0 0.0 0.0 35.8 10.6
CA9 0.0 0.5 0.0 0.0 0.0 1.4 0.0
CA10 4.5 6.7 16.0 9.5 2.6 2.8 9.6
CA16 15.7 76.2 10.0 66.8 43.4 5.5 64.9
CB3, CB4 & CB5 0.6 0.0 0.0 0.0 0.0 0.0 0.0
EV71 45.6 3.8 68.0 4.7 52.7 45.5 8.5
Echoviruses 2.2 0.9 0.0 0.0 1.3 2.0 2.1
CA: coxsackie A virus; CB: coxsackie B virus; EV: enterovirus
Table 4. Triggers for Voluntary and Mandatory Closure of Preschools During Epidemic Phase*
Trigger level Criteria for trigger MCYS registered MOE registered institutions Other non-MCYS/MOE
institutions (kindergartens and preschools) registered institutions
1 No. of cases ≥2 MOH to alert institution(s)
2 No. of cases >7 or MCYS to conduct field visit MOE to conduct field MOH to conduct field visit
Attack rate > 9% or and provide feedback visit and provide
Transmission period >9 days to MOH feedback to MOH
3a No. of cases >13 or MOH to conduct investigations and highlight
Attack rate >18% or serious hygiene irregularities for actions by NEA
Transmission period >15 days
3b Transmission period >15 days MCYS to implement MOE to implement PA/MOH to implement
voluntary closure voluntary closure voluntary closure
4 Transmission period >15 days and MCYS to implement MOE to implement PA/MOH to implement
(No. of cases >13 or mandatory closure mandatory closure mandatory closure
Attack rate >18%)
* Revised April 2008
MOH: Ministry of Health; MOE: Ministry of Education; MCYS: Ministry of Community Development Youth and Sports; NEA: National Environment
Agency; PA: People’s Association
did not cause another epidemic until 2006. A longer time EV71 conducted in 1996/7 at the National University
series would be needed to ascertain whether EV71 epidemic Hospital in Singapore, the infection was largely acquired in
occurs on a 2- to 3-year cycle in Singapore. A 2- to 3-year the preschool years with an annual infection rate of 12%.13
cyclical epidemic of HFMD was noted in the United The increasing size of the epidemics seen in recent years
Kingdom.10 A 3-year epidemic cycle in 1997, 2000, 2003, could be partly attributed to better reporting from preschool
and 2006 caused by EV71 with co-circulation of CA16 was centres, as a result of parental concerns and wide media
observed in Sarawak, Malaysia.11 In Japan, EV71 re- publicity.
emerged 3-yearly as the predominant strain after 1994.12 It The incidence rate of HFMD was highest in preschool
is postulated that this cyclical pattern could have been due children below 5 years of age which comprised 62% to 75%
to the accumulation of immunologically naive preschool of the reported cases. This is consistent with the findings in
children between epidemics until a critical threshold level other outbreaks.11,14 Transmission occurred rapidly in
is breached.11 Based on a seroepidemiological study on preschools with attack rates exceeding 40% in some of the
Annals Academy of Medicine
Epidemiology and Control of HFMD in Singapore, 2001-2007—Li Wei Ang et al 111
institutions. There was a male predominance with since 2001, a high degree of vigilance is maintained on the
differences in ethnic-specific incidence rates. The reason clinical severity and prevalence of this specific enterovirus
for the differences observed in gender and ethnic specific through routine laboratory surveillance. MOH together
incidence rates is not known. with other relevant agencies have instituted a number of
The number of childcare centres and their capacity has measures to curb the HFMD problem. Public health
increased over the years. There were 739 childcare centres measures, in particular, personal and environmental hygiene,
providing almost 63,000 places as at end 2007, compared continue to target childcare centres, kindergartens and
to 653 childcare centres providing about 54,000 places in preschools where highly susceptible children congregate.
2003.15,16 Correspondingly, a larger cohort of 23% of These institutions are required to report clusters of 2 or
preschool children currently attends childcare centres, up more cases of HFMD and to take appropriate steps to
from 16% in 2003. With the emphasis on centre-based interrupt transmission of infection. Depending on the level
care, in the form of infant care, childcare and student care of trigger for outbreak management involving cluster
centres as an important continuum of care and development notifications, actions taken range from issuing alert letters
for children, supply and enrollment of childcare centres are to the relevant institutions, field investigation including
expected to rise over the next few years. More children implementation of control measures, to mobilisation of
would be congregating in a limited space, which provides multi-agency efforts to contain further spread. To stem the
a readily available reservoir for rapid circulation of the spread of infection, preschools where transmission persists
virus, which could then be transmitted to their families and for more than 2 incubation periods, are recommended for
the rest of the population. Thus, the incidence of HFMD in closure with additional trigger criteria for voluntary closure
preschool population is expected to increase further. instituted in April 2008 (Table 4). During closure, operators
are to thoroughly clean the centres before they are allowed
Poor feeding and loss of appetite due to mouth ulcers
to reopen. In addition, parents are advised to ensure that
rather than neurological and cardiac complications
their children adopt a high standard of personal hygiene
accounted for admissions to hospital requiring intravenous
and to keep the infected child at home until full recovery.
drip. Of 131 non-fatal cases admitted to KKH during the
2000 epidemic, there were only 2 cases of aseptic Despite the stringent measures taken to prevent
meningitis. 17 A higher proportion of children was transmission of HFMD in institutions where young children
hospitalised during EV71-associated epidemics of HFMD congregate, outbreaks in these institutions increased 10-
compared to those due to CA16. In Taiwan, where several fold from 2001 to 2007. However, due to the high degree
enteroviruses have also been circulating in the community, of vigilance, institutional outbreaks were recognised early
EV71 was found to be more prevalent among the severely and rapidly brought under control with the majority of
ill and hospitalised cases with HFMD.14,18 In Japan, these outbreaks having an attack rate of less than 10%.
hospitalised cases also increased when EV71 was the main Moreover, there had been a significant decline in the
circulating strain in 2000.12 proportion of HFMD cases among preschool children aged
between 0 and 4 years old over the years compared to older
The case fatality rate in 2001 was very low at 0.06% (3/
children aged between 5 and 9 years old. This suggests that
5210 cases) and the 3 deaths in January and February were
control measures could have delayed the onset of infection.
probably related to the EV71 which caused the 2000
epidemic with 4 deaths between September and October. The main limitation of the study was the small number of
Based on the genetic sequence of 2 representative EV71 samples tested for enteroviruses. Therefore, virological
strains isolated from a fatal case and a surviving patient in surveillance data should be interpreted with caution.
the 2000 epidemic, the outbreak strains were classified Moreover, if more EV71 isolated were to be routinely
under genogroup B, similar with those previously isolated sequenced, we could have a better understanding on the
in Singapore, Malaysia and Japan. It is believed that evolution of the virus from one genotype to another and its
epidemics of EV71 were caused by closely related genetic epidemiological linkage with viruses isolated from other
variants of the enterovirus giving rise to a wide spectrum of countries in the region.20 Nevertheless, based on limited
clinical disease severity. There was no evidence to show data, the predominant EV71 genotype during the 2000
that these epidemics were due to the emergence of EV71 epidemic was B4, and it was B5 during the 2006 epidemic.
strains with increased virulence.19 Another study on
Acknowledgements
molecular epidemiology of EV71 strains isolated during
The authors wish to acknowledge with thanks the support of Communicable
large epidemics in Sarawak, Singapore and Taiwan in 2000 Diseases Division of Ministry of Health, Singapore, Virology Laboratory of
also confirmed that the viruses were from genotype B4.20 the Department of Pathology in Singapore General Hospital and the
Microbiology Laboratory of KK Women’s and Children’s Hospital.
Although no EV71-associated deaths have been reported
February 2009, Vol. 38 No. 2
112 Epidemiology and Control of HFMD in Singapore, 2001-2007—Li Wei Ang et al
REFERENCES 10. UK Communicable Disease Surveillance Centre. Hand, Foot and Mouth
1. Goh KT, Ong A, Low J, editors. A Guide on Infectious Diseases of Public Disease. Communicable Disease Report 1980;34:3-4.
Health Importance in Singapore. 6th ed. Singapore: Ministry of Health 11. Podin Y, Gias EL, Ong F, Leong YW, Yee SF, Yusof MA, et al. Sentinel
and Tan Tock Seng Hospital, 2004. surveillance for human enterovirus 71 in Sarawak, Malaysia: Lessons
2. Tay CH, Gaw CYN, Low T, Ong C, Chia KW, Yeo H, et al. Outbreak of from the first 7 years. BMC Public Health 2006;6:180.
hand, foot and mouth disease in Singapore. Singapore Med J 1974;15: 12. Infectious Disease Surveillance Centre (IDSC), National Institute of
174-83. Infectious Diseases (NID), Japan. Hand, foot and mouth disease, 2000-
3. Goh KT, Doraisingham S, Tan JL, Lim GN, Chew SE. An outbreak of 2003, Japan. Infectious Agents Surveillance Report (IASR) 2004;25:
hand, foot and mouth disease in Singapore. Bull World Health Organ 224-5.
1982;60:965-9. 13. Ooi EE, Phoon MC, Ishak B, Chan SH. Seroepidemiology of human
4. Chan KP, Goh KT, Chong CY, Teo ES, Lau G, Ling AE. Epidemic hand enterovirus 71, Singapore. Emerg Infect Dis 2002;8:995-7.
foot and mouth disease caused by human enterovirus 71, Singapore. 14. Chen KT, Chang HL, Wang ST, Cheng YT, Yang JY. Epidemiological
Emerg Infect Dis 2003;9:78-85. features of hand-foot-mouth disease and herpangina caused by enterovirus
71 in Taiwan, 1998-2005. Pediatrics 2007;120:e244-52.
5. Singh S, Chow VT, Phoon MC, Chan KP, Poh CL. Direct detection of
enterovirus 71 (EV71) in clinical specimens from a hand, foot, and 15. Ministry of Community Development, Youth and Sports, Singapore.
mouth disease outbreak in Singapore by reverse transcription-PCR with Media release no. 19/2008, date of issue: 5 March 2008: Better support
universal enterovirus and EV71-specific primers. J Clin Microbiol for parents-centre-based childcare to be of good quality and accessible,
2002;40:2823-7. while remaining affordable. Available at: http://app.mcys.gov.sg/web/
corp_press.asp. Accessed 5 September 2008.
6. Oon L LE, Ling AE. Enterovirus infection: overview and laboratory
diagnosis. In: Lin RVTP, Goh KT, editors. Enterovirus Infection in 16. Ministry of Community Development, Youth and Sports, Singapore.
Singapore – with Particular Reference to the EV71 Outbreak in 2000. Singapore Social Statistics In Brief 2004. Available at: http://
Institute of Environmental Epidemiology, Ministry of Environment, app.mcys.gov.sg/web/GeneralStatistics.asp. Accessed 5 September 2008.
2002:46-65. 17. Chong CY, Chan KP, Shah V A, Ng WYM, Lau G, Teo TES, et al. Hand,
7. Perera D, Podin Y, Akin W, Tan C-S, Cardosa MJ. Incorrect identification foot and. mouth disease in Singapore: a comparison of fatal and non-fatal
of recent Asian strains of Coxsackievirus A16 as human enterovirus 71: cases. Acta Paediatr 2003;92:116-9.
Improved primers for the specific detection of human enterovirus 71 by 18. Lum LC, Wong KT, Lam SK, Chua KB, Goh AY. Neurogenic pulmonary
RT PCR. BMC Infect Dis 2004;4:11. oedema and enterovirus 71 encephalomyelitis. Lancet 1998;352:1391.
8. Armitage P, Berry G. Statistical Methods in Medical Research. 2nd ed. 19. Singh S, Poh CL, Chow VT. Complete sequence analyses of
Oxford: Blackwell Scientific, 1987. enterovirus 71 strains from fatal and non-fatal cases of the hand, foot and
mouth disease outbreak in Singapore (2000). Microbiol Immunol
9. Lai SH, Teo CES, Lau G. Fatalities from enterovirus infection during an
2002;46:801-8.
epidemic of hand, foot and mouth disease in Singapore: postmortem
findings. In: Lin RVTP, Goh KT, editors. Enterovirus Infection in 20. Cardosa MJ, Perera D, Brown BA, Cheon D, Chan HM, Chan KP, et al.
Singapore – with Particular Reference to the EV71 Outbreak in 2000. Molecular epidemiology of human enterovirus 71 strains and recent
Institute of Environmental Epidemiology, Ministry of the Environment, outbreaks in the Asia-Pacific region: Comparative analysis of the VP1
2002:84-103. and VP4 genes. Emerg Infect Dis 2003;9:461-8.
Annals Academy of Medicine
You might also like
- Living on the Frontline of COVID-19 in MCO And CMCOFrom EverandLiving on the Frontline of COVID-19 in MCO And CMCONo ratings yet
- Etiologic and Epidemiologic Analysis of Hand FootDocument9 pagesEtiologic and Epidemiologic Analysis of Hand FootAisah AisahNo ratings yet
- Epidemiologi of HFMDDocument16 pagesEpidemiologi of HFMDJimmy AmbaritaNo ratings yet
- 1331907497-Montasseretal 2011BJMMR1038Document12 pages1331907497-Montasseretal 2011BJMMR1038puppyhandaNo ratings yet
- Epidemiology of Recurrent Hand, Foot and Mouth Disease, China, 2008-2015Document11 pagesEpidemiology of Recurrent Hand, Foot and Mouth Disease, China, 2008-2015Catherine BasinNo ratings yet
- HFMD Deaths in VN 2011Document7 pagesHFMD Deaths in VN 2011Pham Van HauNo ratings yet
- Pone 0217474Document12 pagesPone 0217474Breixo HarguindeyNo ratings yet
- Karakteristik Penderita Demam Tifoid Yang Di Rawat Inap Di Rumah Sakit Umum Daerah Dr. Rm. Djoelham Kota Binjai Tahun 2016Document9 pagesKarakteristik Penderita Demam Tifoid Yang Di Rawat Inap Di Rumah Sakit Umum Daerah Dr. Rm. Djoelham Kota Binjai Tahun 2016Lilis Suryani PNo ratings yet
- A Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsDocument28 pagesA Comparative-Descriptive Analysis of Clinical Characteristics in 2019-Coronavirus-Infected Children and AdultsPatrick NunsioNo ratings yet
- Pediatric Oncology Fungal InfectionsDocument6 pagesPediatric Oncology Fungal InfectionserickmattosNo ratings yet
- Effects of One-Dose Varicella Vaccination On Disease Severity in Children During Outbreaks in Seoul, KoreaDocument5 pagesEffects of One-Dose Varicella Vaccination On Disease Severity in Children During Outbreaks in Seoul, KoreaNur WahyuningsihNo ratings yet
- Hand, Foot and Mouth Disease: Spatiotemporal Transmission and ClimateDocument10 pagesHand, Foot and Mouth Disease: Spatiotemporal Transmission and ClimateAisah AisahNo ratings yet
- Clinical and Epidemiological Features of Hymenolepidosis and Teniarichosis in ChildrenDocument6 pagesClinical and Epidemiological Features of Hymenolepidosis and Teniarichosis in ChildrenCentral Asian StudiesNo ratings yet
- 838 3348 1 PBDocument7 pages838 3348 1 PBararapiaNo ratings yet
- Spatial Epidemiology and Climatic Predictors of Paediatric Dengue Infections Captured Via Sentinel Site Surveillance, Phnom Penh Cambodia 2011 - 2012Document8 pagesSpatial Epidemiology and Climatic Predictors of Paediatric Dengue Infections Captured Via Sentinel Site Surveillance, Phnom Penh Cambodia 2011 - 2012Andrew HukomNo ratings yet
- Risk Predictors of Progression To Severe Disease of DengueDocument13 pagesRisk Predictors of Progression To Severe Disease of DengueTaufiqurrokhman RofiiNo ratings yet
- A Review of Dengue Research in MalaysiaDocument9 pagesA Review of Dengue Research in MalaysiaAriff RazakNo ratings yet
- Acute Rheumatic Fever Clinical Profile in Children in Western UkraineDocument5 pagesAcute Rheumatic Fever Clinical Profile in Children in Western UkraineraniaulfahNo ratings yet
- Typhoid fever disease burden and antimicrobial resistance in five Asian countriesDocument4 pagesTyphoid fever disease burden and antimicrobial resistance in five Asian countriesPutu SuartiniNo ratings yet
- HHS Public AccessDocument22 pagesHHS Public AccessZakirNo ratings yet
- Research Article: Viral Agents of Diarrhea in Young Children in Two Primary Health Centers in Edo State, NigeriaDocument6 pagesResearch Article: Viral Agents of Diarrhea in Young Children in Two Primary Health Centers in Edo State, NigeriariniNo ratings yet
- To The Editor:: Sars-Cov-2 Infection in ChildrenDocument2 pagesTo The Editor:: Sars-Cov-2 Infection in ChildrenBogdan BerenghiaNo ratings yet
- 1 s2.0 S0929664621003892 MainDocument8 pages1 s2.0 S0929664621003892 Mainrheynamaulidar rumoninNo ratings yet
- 1 s2.0 S0929664616302480 MainDocument9 pages1 s2.0 S0929664616302480 MainEniola JayeolaNo ratings yet
- Dengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaDocument3 pagesDengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaReju VijayandranNo ratings yet
- fcimb-11-694093Document12 pagesfcimb-11-694093Marketable StudioNo ratings yet
- Bacteremia in Children-JTPDocument5 pagesBacteremia in Children-JTPRomica MarcanNo ratings yet
- MHSRJ 27 (2) 83-87Document5 pagesMHSRJ 27 (2) 83-87Hein Myat HtutNo ratings yet
- Risk Factors for Suppurative Complications in Children with PneumoniaDocument6 pagesRisk Factors for Suppurative Complications in Children with PneumoniaWilson LeccaNo ratings yet
- 2016 Article 1849 PDFDocument8 pages2016 Article 1849 PDFdydy_7193No ratings yet
- Dengue Hemorrhagic Fever in Infants: A Study of Clinical and Cytokine ProfilesDocument12 pagesDengue Hemorrhagic Fever in Infants: A Study of Clinical and Cytokine ProfilesYono FabiandiNo ratings yet
- Diabetes With Hypertension As Risk Factors For Adult Dengue Hemorrhagic Fever in A Predominantly Dengue Serotype 2 Epidemic: A Case Control StudyDocument12 pagesDiabetes With Hypertension As Risk Factors For Adult Dengue Hemorrhagic Fever in A Predominantly Dengue Serotype 2 Epidemic: A Case Control StudyDwitari Novalia HaraziNo ratings yet
- Sepsis Proposal1Document34 pagesSepsis Proposal1Appiah Peter OforiNo ratings yet
- Review Article: The Risk Factors of Acquiring Severe Hand, Foot, and Mouth Disease: A Meta-AnalysisDocument13 pagesReview Article: The Risk Factors of Acquiring Severe Hand, Foot, and Mouth Disease: A Meta-AnalysisFan AccountNo ratings yet
- Characteristics of Gastrointestinal Findings in Children With Sars-Cov-2Document5 pagesCharacteristics of Gastrointestinal Findings in Children With Sars-Cov-2Central Asian StudiesNo ratings yet
- Research Article: The Analysis of Etiology and Risk Factors For 192 Cases of Neonatal SepsisDocument7 pagesResearch Article: The Analysis of Etiology and Risk Factors For 192 Cases of Neonatal Sepsisflorentina lulutNo ratings yet
- DengueDocument5 pagesDengueSam Angelo EstrellaNo ratings yet
- The Rise of Imported Dengue Infections in Victoria, Australia, 2010-2016Document11 pagesThe Rise of Imported Dengue Infections in Victoria, Australia, 2010-2016Satriya WibawaNo ratings yet
- Ensefalitis 9Document4 pagesEnsefalitis 9Asri RachmawatiNo ratings yet
- Ajol File Journals - 494 - Articles - 112516 - Submission - Proof - 112516 5833 312396 1 10 20150204Document6 pagesAjol File Journals - 494 - Articles - 112516 - Submission - Proof - 112516 5833 312396 1 10 20150204ASK De OliveiraNo ratings yet
- Epidemiology of Acute Respiratory Infections in Children in Guangzhou: A Three-Year StudyDocument9 pagesEpidemiology of Acute Respiratory Infections in Children in Guangzhou: A Three-Year Studywina annisaNo ratings yet
- Is Virus Coinfection A Predictor of Severity in Children With Viral Respiratory Infections?Document6 pagesIs Virus Coinfection A Predictor of Severity in Children With Viral Respiratory Infections?castillocavazos09No ratings yet
- Ana 29 492Document6 pagesAna 29 492AdilZyaniNo ratings yet
- Neonatal Infections PerspectiveDocument13 pagesNeonatal Infections PerspectiveYUDY LORENA GIRALDO ALFONSONo ratings yet
- VAP Incidence, Risk Factors and Bacteria in PICUDocument6 pagesVAP Incidence, Risk Factors and Bacteria in PICURabiatul 'raney' AdawiyahNo ratings yet
- Trend and Outcome of Sepsis in ChildrenDocument8 pagesTrend and Outcome of Sepsis in ChildrenGunduz AgaNo ratings yet
- Epidemiology, Clinical Manifestations, and Molecular Typing of Salmonella Typhi in LebanonDocument7 pagesEpidemiology, Clinical Manifestations, and Molecular Typing of Salmonella Typhi in LebanonOmy Ning PratiwiNo ratings yet
- 1 PB PDFDocument7 pages1 PB PDFAndi Prajanita AlisyahbanaNo ratings yet
- Demographic and Clinical Features of Dengue Fever in Pakistan From 2003-2007: A Retrospective Cross-Sectional StudyDocument8 pagesDemographic and Clinical Features of Dengue Fever in Pakistan From 2003-2007: A Retrospective Cross-Sectional Studyann_michelle7No ratings yet
- Epidemiology and Clinical Characteristics of AGE in ChildrenDocument12 pagesEpidemiology and Clinical Characteristics of AGE in ChildrenGusdek AryaNo ratings yet
- Prevalence of Dengue Among Clinically SuDocument5 pagesPrevalence of Dengue Among Clinically SuIshreet ChaddaNo ratings yet
- Dr. Vona 12Document5 pagesDr. Vona 12Agustiawan ImronNo ratings yet
- Hand, Foot and Mouth Disease and VietnamDocument9 pagesHand, Foot and Mouth Disease and VietnamQuỳnh ThưNo ratings yet
- Epidemiology of Tuberculosis and HIV Coinfections in Singapore, 2000 2014Document6 pagesEpidemiology of Tuberculosis and HIV Coinfections in Singapore, 2000 2014jessicaNo ratings yet
- 9219-Article Text-10990-1-10-20220510Document7 pages9219-Article Text-10990-1-10-20220510dosen paNo ratings yet
- H5N1Document7 pagesH5N1miqbal_100No ratings yet
- Gittle R 2017Document4 pagesGittle R 2017Hari 'hardyboy' PurwantoNo ratings yet
- Clinical Characteristics of Children With Coronavirus Disease 2019 in Hubei, ChinaDocument6 pagesClinical Characteristics of Children With Coronavirus Disease 2019 in Hubei, ChinaBobanBisercicNo ratings yet
- 1 s2.0 S1198743X21002846 MainDocument8 pages1 s2.0 S1198743X21002846 MaindrkhengkiNo ratings yet
- Practiva No 3 Anova Serrano 2017Document7 pagesPractiva No 3 Anova Serrano 2017CARLOS DIONEY MOLINA CLEMENTENo ratings yet
- TRANSLATEjdjfjDocument4 pagesTRANSLATEjdjfjchaer assofiNo ratings yet
- Premiere Pro CS4 and After Effects CS4 Read MeDocument8 pagesPremiere Pro CS4 and After Effects CS4 Read MeRadu BogdanNo ratings yet
- Mr. HardIman, 35 Yo, Combustio GR II A-B 41,5%, DPJP Dr. Saktrio D.subarno, SP - Bp-ReDocument45 pagesMr. HardIman, 35 Yo, Combustio GR II A-B 41,5%, DPJP Dr. Saktrio D.subarno, SP - Bp-Rechaer assofiNo ratings yet
- Marur2014 PDFDocument7 pagesMarur2014 PDFchaer assofiNo ratings yet
- 3-4-2019 Mrs. Suwartin 47 Yo, Combutio Grade II AB 5% Ec. Flash Injury, DDocument14 pages3-4-2019 Mrs. Suwartin 47 Yo, Combutio Grade II AB 5% Ec. Flash Injury, Dchaer assofiNo ratings yet
- 10-9-2019. (18.50) Mrs. Waode Konsilo, 67 TH, Ischialgia, DR Tuti, SP - OtDocument13 pages10-9-2019. (18.50) Mrs. Waode Konsilo, 67 TH, Ischialgia, DR Tuti, SP - Otchaer assofiNo ratings yet
- Tetanus Prevention and TreatmentDocument6 pagesTetanus Prevention and TreatmentDwi ApriliaNo ratings yet
- Right Lower Quadrant Pain DiagnosisDocument13 pagesRight Lower Quadrant Pain Diagnosischaer assofiNo ratings yet
- 2-4-2019, Mrs. Puput, 16 Yo, Localized Peritonitis Ec. Susp. Perforated Appendicitis, Dr. Wayan Eka Winarka, SP.BDocument13 pages2-4-2019, Mrs. Puput, 16 Yo, Localized Peritonitis Ec. Susp. Perforated Appendicitis, Dr. Wayan Eka Winarka, SP.Bchaer assofiNo ratings yet
- Scanned With CamscannerDocument15 pagesScanned With Camscannerchaer assofiNo ratings yet
- Knowledge, Attitudes, Beliefs and Practices ofDocument10 pagesKnowledge, Attitudes, Beliefs and Practices ofchaer assofiNo ratings yet
- 10-9-2019. (18.50) Mrs. Waode Konsilo, 67 TH, Ischialgia, DR Tuti, SP - OtDocument13 pages10-9-2019. (18.50) Mrs. Waode Konsilo, 67 TH, Ischialgia, DR Tuti, SP - Otchaer assofiNo ratings yet
- Evaluation of Beneficial Effects of Addition of Intramuscular HumanDocument6 pagesEvaluation of Beneficial Effects of Addition of Intramuscular Humanchaer assofiNo ratings yet
- Wong TY Mitchell P Editors 2004 Current Concept Hypertensive RetinopathyDocument8 pagesWong TY Mitchell P Editors 2004 Current Concept Hypertensive Retinopathychaer assofiNo ratings yet
- 7Document7 pages7Ersya MuslihNo ratings yet
- Abstark InggrisDocument1 pageAbstark Inggrischaer assofiNo ratings yet
- Lapsus Hiperbilirubinemia 20181218162653Document4 pagesLapsus Hiperbilirubinemia 20181218162653chaer assofiNo ratings yet
- Osteomyelitis PDFDocument10 pagesOsteomyelitis PDFchaer assofiNo ratings yet
- Radiation Effects and Sources-2016Document68 pagesRadiation Effects and Sources-2016chaer assofiNo ratings yet
- GHFSDFFDocument11 pagesGHFSDFFchaer assofiNo ratings yet
- Emerging and Re-emerging Diseases: Leptospirosis, Meningococcemia, AH1N1, HFMD, SARS, Chikungunya, Avian Flu, COVID-19Document11 pagesEmerging and Re-emerging Diseases: Leptospirosis, Meningococcemia, AH1N1, HFMD, SARS, Chikungunya, Avian Flu, COVID-19Josielyn Valladolid0% (1)
- Hand Foot and Mouth DiseaseDocument14 pagesHand Foot and Mouth DiseaseE=MC2No ratings yet
- Clinical Features of Viral Exanthems: Sarajane Ting, Rosemary NixonDocument6 pagesClinical Features of Viral Exanthems: Sarajane Ting, Rosemary NixonJustine Frances CabalayNo ratings yet
- 8 Childhood Viral Skin Rashes: Chickenpox, Measles and MoreDocument9 pages8 Childhood Viral Skin Rashes: Chickenpox, Measles and MoreErik OrtegaNo ratings yet
- Protocol For Management of Hand, Foot and Mouth Disease (HFMD) and Herpangina at Clinics and Hospitals in SarawakDocument17 pagesProtocol For Management of Hand, Foot and Mouth Disease (HFMD) and Herpangina at Clinics and Hospitals in SarawakbabytwelveNo ratings yet
- HFMD (Hand-Foot-Mouth Disease) An Emerging DiseaseDocument76 pagesHFMD (Hand-Foot-Mouth Disease) An Emerging DiseaseAn Zheng100% (7)
- Hand Foot and Mouth DiseaseDocument16 pagesHand Foot and Mouth DiseaseCaroline TecsonNo ratings yet
- Assess The Knowledge Regarding Hand Foot Mouth Disease Among Mothers of Under Five Children in Selected CommunityDocument4 pagesAssess The Knowledge Regarding Hand Foot Mouth Disease Among Mothers of Under Five Children in Selected CommunityEditor IJTSRDNo ratings yet
- HFMD Outcomes MainDocument11 pagesHFMD Outcomes Mainberliana mNo ratings yet
- Enteroviral InfectionsDocument32 pagesEnteroviral InfectionsTarik PlojovicNo ratings yet
- PI Virus (Enterovirus and Rhinovirus Groups)Document34 pagesPI Virus (Enterovirus and Rhinovirus Groups)Lovryan Tadena AmilingNo ratings yet
- Rash Diagnosis Cheat Sheet: EmergencyDocument1 pageRash Diagnosis Cheat Sheet: Emergencykdlsfk kajjksolsNo ratings yet
- Hand, Foot and Mouth Disease (HFMDDocument19 pagesHand, Foot and Mouth Disease (HFMDukhtijuNo ratings yet
- HFMD: Clinical Features, Complications, Diagnosis and ManagementDocument27 pagesHFMD: Clinical Features, Complications, Diagnosis and ManagementNur IzzahNo ratings yet
- HFMD FINAL - AzaniDocument8 pagesHFMD FINAL - AzaniGrace BlaiseNo ratings yet
- HFMDDocument1 pageHFMDapi-350983586No ratings yet
- Management of Herpangina: Denta, Jurnal Kedokteran GigiDocument5 pagesManagement of Herpangina: Denta, Jurnal Kedokteran GigirizadNo ratings yet
- Hand Foot and Mouth DiseaseDocument39 pagesHand Foot and Mouth DiseaseSulochan LohaniNo ratings yet
- 403 Hand - Foot.mouthDocument2 pages403 Hand - Foot.mouthAlice MinNo ratings yet
- Fever with Rash: Measles or RoseolaDocument78 pagesFever with Rash: Measles or RoseolaRiyan AgusNo ratings yet
- Alopecia Totalis Following HFMDDocument3 pagesAlopecia Totalis Following HFMDVilt VilNo ratings yet
- Case Study HFMD :)Document15 pagesCase Study HFMD :)Princess CavestaniNo ratings yet
- Viral ExanthemsDocument67 pagesViral ExanthemsKay HanNo ratings yet
- HerpanginaDocument8 pagesHerpanginaWendy Nadya Vitasani HalohoNo ratings yet
- Hand Foot and Mouth DiseaseDocument3 pagesHand Foot and Mouth DiseaseAisah AisahNo ratings yet
- Common Viral Infections in The Oral Cavity: 1. Acute Herpetic Gingivostomatitis DNA VirusDocument6 pagesCommon Viral Infections in The Oral Cavity: 1. Acute Herpetic Gingivostomatitis DNA VirusChristineMartinNo ratings yet
- Sample ReflectionDocument2 pagesSample ReflectionRhiza Joy HiposNo ratings yet
- HFMD Parent Orientation Narrative ReportDocument7 pagesHFMD Parent Orientation Narrative ReportGerald CiudadNo ratings yet
- The Lancet Respiratory MedicineDocument2 pagesThe Lancet Respiratory MedicineNgopibareng.idNo ratings yet