Professional Documents
Culture Documents
Awad 2003
Uploaded by
Jansen ChCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Awad 2003
Uploaded by
Jansen ChCopyright:
Available Formats
Glomerular and Tubular Dysfunction in
Children with Congenital Cyanotic Heart
Disease: Effect of Palliative Surgery
HESHAM AWAD, MD; IBRAHIM EL-SAFTY, PHD; MOUSTAFA ABDEL-GAWAD, MD;
SALWA EL-SAID, MSC
ABSTRACT: Background: Nephropathy has long been mentioned parameters. Results: Results of the present
recognized as a potential complication of congenital work showed that with increasing duration of cyano-
cyanotic heart disease (CCHD). The present study was sis (ie, on going from G2 to G5) among the studied
undertaken to investigate some aspects of glomerular children with CCHD, there was a significant elevation
function by measuring urinary total protein, microalbu- in the urinary excretion of the investigated functional
min, and tubular function by assessing urinary ␣-1- and structural parameters of the glomeruli and proxi-
microglobulin. The structural integrity of the renal prox- mal tubules compared with the control children. The
imal tubules was also studied by measuring urinary data also showed a significant increase in Hct,
activities of the brush-border enzyme leucine-amino- whereas oxygen saturation was significantly de-
peptidase and the lysosomal enzyme N-acetyl--D-glu- creased. Results of G6 after the palliative surgery
cosaminidase. The levels of hematocrit (Hct) and oxygen demonstrated a significant decrease in the urinary
saturation were also investigated as predisposing factors excretion of the investigated parameters of the kidney,
for renal impairment in CCHD. Methods: These investi- with a significant decrease in Hct and increase in
gations were done by recruiting 86 children who were oxygen saturation levels, compared with the results of
grouped as follows: the control group (G1) consisted of the patients of this group before the palliative surgery.
14 children (aged 4 –12 years); the other 72 children Conclusions: These results suggest impairment of both
with CCHD were divided according to age (ie, duration glomerular and tubular functions as well as structure of
of cyanosis) into 4 equal groups, each containing 18 the proximal tubules among children with CCHD and that
patients: G2 (age ⬍1 year), G3 (age ⱖ1 year and ⬍5 the palliative surgery has significantly improved this
years), G4 (age ⱖ5 years and ⬍10 years), and G5 (age impairment. KEY INDEXING TERMS: Congenital cyanotic
ⱖ10 years). In addition, 10 of the 72 patients underwent heart disease (CCHD); Children; Palliative surgery; ␣-1-
a palliative surgery and were included as G6 (regard- microglobulin; Leucine-aminopeptidase; N-acetyl--D-
less of age: 2 from G3, 4 from G4, and 4 from G5) to glucosaminidase; Hematocrit; Oxygen saturation. [Am J
study the effect of the palliative surgery on the above- Med Sci 2003;325(3):110–114.]
functions occur in some patients with CCHD.2 Clin-
N ephropathy has long been recognized as a po-
tential complication in patients with long-
standing CCHD1. The incidence of renal abnormal-
ical studies have reported these functional abnor-
malities, mostly without discriminating between
ities increases with the degree of cyanosis and may glomerular and tubular dysfunction.4 Findings in-
also increase with increasing duration of cyanosis2. cluded normal5 or decreased6 glomerular filtration
Abnormalities of renal structure and function oc- rate (GFR) and decreased renal plasma flow2 as well
cur in some patients with CCHD. The principle as both glomerular and tubular proteinuria7 were
renal structural lesions have been in the glomeru- reported.
lus,3 and tubular changes are rare.4 Abnormal renal Because of the great reserve capacity of the kid-
ney, tests used for assessing the functional integrity
of the kidney (such as serum creatinine or urea and
From the Departments of Pediatrics (HA, SE-S) and Cardiology
(MA-G), Faculty of Medicine, and Section of Biochemistry, Depart- GFR) are not sufficiently sensitive because these
ment of Chemistry, Faculty of Education (IE-S), Ain-Shams Uni- measurements can be in the normal range despite
versity, Cairo, Egypt. considerable impairment of renal function, and they
Submitted July 26, 2002; accepted December 10, 2002.
Correspondence: Ibrahim El-Safty, Ph.D., Department of Bio-
become significantly altered only after considerable
chemistry, Faculty of Science, Makerere University, PO Box 7062, damage to the kidney has occurred with major func-
Kampala, Uganda. tional impairment8. Various urinary parameters of
110 March 2003 Volume 325 Number 3
Awad et al
Table 1. Laboratory Reference Values for the Investigated the kidney functional and structural integrity
Urinary Parameters among 14 Healthy Children (Aged 4 –12
Years)
among such patients was investigated.
Parameter Range (mean ⫾ SD) Subjects and Methods
U.TP/U.Cr mg/g Cr 29.1–80.95 (49.96 ⫾ 14.59) Subjects. Fourteen healthy children aged 4 to 12 years served
U.Malb/U.Cr g/mg Cr 1.86–5.75 (3.47 ⫾ 1.10) as control group (G1). Patients of the present study were recruited
U.␣1M/U.Cr g/mg Cr 2.35–11.67 (6.93 ⫾ 4.14) over a period of 6 months (June–December 1999) from those
U.LAP/U.Cr U/mg Cr 1.44–15.86 (9.74 ⫾ 4.57) attending Ain-Shams University Childrens’ Hospital and Insti-
U.NAG/U.Cr nmol/mg Cr 0.99–24.73 (8.94 ⫾ 7.63) tute of Cardiology, Cairo, Egypt. The study was approved by the
hospital review board. Patients were subjected to full medical
TP, total protein; U.Cr, urinary creatinine. history, clinical examination, and echocardiology. Patients with
coarctation of the aorta, associated renovascular or structural
malformations, urinary tract infection, or receiving antibiotics of
aminoglycoside family were excluded. After application of these
the kidney, such as microalbumin (Malb) and ␣-1- exclusion criteria, 72 patient children suffering from CCHD were
microglobulin (␣1M) have proved useful to assess included in the present study. They were divided into 4 equal
functional integrity of glomerulus and proximal tu- groups (each obtained 18 cases) according to age: G2 (⬍1 year), G3
bules, respectively, whereas urinary kidney-specific (ⱖ1 year and ⬍5 years), G4 (ⱖ5 years and ⬍10 years) and G5 (ⱖ10
years). In addition, 10 of the 72 cases (2 from G3, 4 from G4, and
enzymes such as brush-border leucine-aminopepti- 4 from G5) underwent palliative surgery and were investigated as
dase (LAP) and lysosomal N-acetyl--D-glucosamini- G6.
dase (NAG) are indicators for structural integrity of Sampling and Methods. Parents of each child (patient and
proximal tubules.9 control) participating in the investigation gave their oral permis-
sion to get the urine sample and perform the renal function tests.
The purpose of this study was to evaluate some Morning urine sample was suggested as the best sample for
aspects of glomerular and proximal tubular func- detecting early kidney abnormalities.10 A random morning urine
tions as well as structural integrity of the proximal sample was collected at home between 8 and 9 AM from each
tubules in children with CCHD. The study also participant child (control and case subjects) in a sterilized con-
aimed to investigate the role of both hematocrit and tainer and centrifuged at 4500 rpm for 5 minutes, and the top 5
mL of the supernatant were stored frozen at ⫺20°C in aliquots
oxygen saturation as predisposing factors of renal without preservatives until analyzed within 2 weeks for the
impairment among such patients. The effect of pal- assessment of:
liative surgery on the above-mentioned factors and 1. Glomerular function by estimation of total protein by dye-
Table 2. Values (mean ⫾ SD) of the Investigated Parameters among the Control Group and the Different Groups of CCHD
Children
Control Different Groups of CCHD Children
G1 (n ⫽ 14) G2 (n ⫽ 18) G3 (n ⫽ 18) G4 (n ⫽ 18) G5 (n ⫽ 18)
Parameters Age 4–12 years Age ⬍1 years Age ⱖ1 year to ⬍5 years Age ⱖ5 years to ⬍10 years Age ⱖ10 years
Hct 0.35.11 ⫾ 0.274 0.3833 ⫾ 0.327* 0.4433 ⫾ 0.512*a 0.5505 ⫾ 0.445*bd 0.6235 ⫾ 0.751*cef
Oxygen saturation 95.21 ⫾ 3.11 66.22 ⫾ 6.83* 61.27 ⫾ 6.47* 61.83 ⫾ 7.53* 59.41 ⫾ 7.70*c
(%)
Glomerular function
U.TP/ 49.96 ⫾ 14.59 91.11 ⫾ 112.92* 80.95 ⫾ 93.18* 133.76 ⫾ 79.37*bd 189.30 ⫾ 95.34*ce
U.Cr (mg/g)
U.Malb/ 3.47 ⫾ 1.10 2.62 ⫾ 1.73* 14.49 ⫾ 17.74*a 73.66 ⫾ 70.74*bd 224.42 ⫾ 208.03*cef
U.Cr (g/mg)
Tubular function
U.␣1M/ 6.93 ⫾ 4.14 22.34 ⫾ 20.59* 36.91 ⫾ 48.01* 55.33 ⫾ 19.97*bd 83.12 ⫾ 82.63*cef
U.Cr (g/mg)
Tubular structure
U.LAP/ 9.74 ⫾ 4.57 12.40 ⫾ 18.31* 35.99 ⫾ 38.45*a 45.25 ⫾ 44.55*b 103.47 ⫾ 157.06*c
U.Cr (U/mg)
U.NAG/ 8.94 ⫾ 7.63 31.68 ⫾ 26.11* 75.56 ⫾ 84.58*a 201.73 ⫾ 149.86*bd 244.77 ⫾ 101.96*ce
U.Cr (nmol/mg)
*P ⬍ 0.05 compared with control group (G1).
a
G2:3, P ⬍ 0.05.
b
G2:4, P ⬍ 0.05.
c
G2:5, P ⬍ 0.05.
d
G3:4, P ⬍ 0.05.
e
G3:5, P ⬍ 0.05.
f
G4:5, P ⬍ 0.05.
THE AMERICAN JOURNAL OF THE MEDICAL SCIENCES 111
Palliative Surgery in Congenital Cyanotic Heart Disease
Table 3. Percentage of CCHD Patients with Abnormal Level of Table 5. Correlation Coefficient (r) between Measured Urinary
the Measured Parameters in Each Investigated Group Glomerular and Tubular Markers among CCHD Children as 1
Group of Patients
Parameter G2 G3 G4 G5
Urinary Tubular Markers
Hct 11 27 44 83 Urinary Glomerular
U.TP/U.Cr 27 27 66 88 Markers U.␣1M/U.Cr U.LAP/U.Cr U.NAG/U.Cr
U.Malb/U.Cr 0 72 100 100
U.␣1M/U.Cr 73 89 95 100 U.TP/U.Cr 0.55* 0.26* 0.29*
U.LAP/U.Cr 11 61 61 70 U.Malb/U.Cr 0.53* 0.44* 0.62*
U.NAG/U.Cr 44 88 100 100
* P ⬍ 0.05.
binding method11 and microalbumin (U.Malb) by enzyme-linked levels of each investigated parameter increased (Ta-
immunosorbent assay (ELISA) technique using a kit from OR-
Gentec-Germany (Mainz, Germany).
ble 3). There was a significant correlation between
2. Tubular function by measuring ␣1-microglobulin (U.␣1M) by age and Hct, and each was significantly correlated
ELISA technique using a kit from ORGentec-Germany. with urinary parameters of the glomeruli and the
3. Tubular structural integrity by estimation of leucine- tubules (Table 4).
aminopeptidase (U.LAP)12 and N-acetyl--D-glucosaminidase
Both TP and Malb (glomerular urinary markers)
(U.NAG).13
4. Urine creatinine (U.Cr) concentration by Jaffe kinetic were significantly correlated with both ␣1M and
method.14 LAP as well as NAG (proximal tubular urinary
In addition, oxyhemoglobin saturation was assessed using markers) (Table 5). Data for the effect of palliative
pulse oximetry, and Hct was estimated using microcapillary tube surgery (Table 6) showed that the levels of Hct and
centrifugation after obtaining a blood sample by pin-prick
method.
urinary parameters of glomeruli and tubules were
Spot urine measurements were used because it has been shown significantly decreased, whereas oxygen saturation
that urinary protein/creatinine ratio15 and albumin/creatinine was significantly increased after the surgery com-
ratio16 as well as dividing the urinary enzyme activity by urinary pared with levels before the surgery.
creatinine concentration17 in a random urine sample correlate
with 24-hour urinary excretion and eliminate variations caused
by changing rates of urine output and provide a measure inde- Discussion
pendent of urine concentration.
Statistical Analysis. Results were tabulated as mean ⫾ SD Results for Hct in the present study (Tables 2, 3,
and analyzed using paired t test for parametric data, whereas the and 4) are in agreement with the findings of others
nonparametric data were analyzed using the Mann-Whitney that Hct was significantly elevated among CCHD
U–Wilcoxon Rank Sum W test and sign test. Spearman’s Corre- patients4,6,7 and that Hct was correlated with the
lation Coefficients were used and level of significance was con-
sidered at P ⬍ 0.05. age of patients (ie, duration of cyanosis).7,18 Data of
oxygen saturation in the present work (Table 4)
Results confirms the report of others4 that oxygen satura-
tion at rest was related neither to Hct elevation nor
Data from the present study (Table 2) showed, to renal injury (both at the glomerular and proximal
compared with control subjects (G1), a significant tubular levels).
increase in Hct and urinary parameters of the glo- Results of the glomerular function in the present
meruli (except U.Malb/U.Cr in G2, which showed investigation (Tables 2 and 3) support the work of
significant decrease in the mean value) and tubules others4,6,7 who reported increased proteinuria and
with increasing duration of cyanosis (on going from microalbuminuria among CCHD patients, indicat-
G2 to G5), whereas oxygen saturation was signifi- ing glomerular dysfunction. This elevation of pro-
cantly decreased. As duration of cyanosis increased, teinuria and microalbuminuria may be attributable
the percentage of CCHD patients with abnormal to 1 of 2 possibilities or to both. First, renal histo-
Table 4. Correlation Coefficient (r) between the Investigated Predisposing Factors for Renal Impairment and Urinary Parameters of
Kidney Function among CCHD Children as 1 Group of Patients
Predisposing Factors for Urinary Parameters for
Renal Impairment Glomerular Function Urinary Parameters for Tubular Integrity
Age Hct Oxygen-Saturation U.TP/U.Cr U.Malb/U.Cr U.␣1M/U.Cr U.LAP/U.Cr U.NAG/U.Cr
Age 1 0.86* 0.13 0.38* 0.57* 0.38* 0.33* 0.63*
Hct 1 0.21 0.42* 0.53* 0.24* 0.24* 0.55*
Oxygen saturation 1 0.22 0.14 0.20 0.20 0.15
* P ⬍ 0.05.
112 March 2003 Volume 325 Number 3
Awad et al
Table 6. Effect of Palliative Surgery on the Investigated which is similar to ␣1M in that it is filtered through
Parameters among CCHD Children the glomeruli and reabsorbed almost totally by prox-
imal tubules, suggesting proximal tubular reabsorp-
G6 (Before) G6 (After)
Parameters (Mean ⫾ SD) (Mean ⫾ SD) P tion dysfunction among CCHD patients. This sug-
gestion receives support from the results of the
Hct 0.5160 ⫾ 0.105 0.4370 ⫾ 0.764 S present study (Tables 2 and 3) and a report of other
Oxygen saturation (%) 63.90 ⫾ 5.56 92.60 ⫾ 1.57 S researchers6 that demonstrated damage to proximal
Glomerular function tubular cells as evidenced by elevated urinary activ-
U.TP/U.Cr (mg/g) 194.00 ⫾ 93.69 47.05 ⫾ 40.70 S
U.Malb/U.Cr (g/mg) 147.90 ⫾ 220.70 27.80 ⫾ 27.48 S ities of LAP and NAG. This damage resulted in
Tubular function leakage of these enzymes into urine as well as ex-
U.␣1M/U.Cr (g/mg) 46.30 ⫾ 18.49 27.05 ⫾ 12.90 S cessive loss of ␣1M through failure of reabsorption
Tubular structure by the damaged proximal tubular cells. Another
U.LAP/U.Cr (U/mg) 152.30 ⫾ 149.42 70.36 ⫾ 41.14 S
U.NAG/U.Cr (nmol/mg) 187.53 ⫾ 146.23 37.78 ⫾ 27.39 S
evidence for the damage and reabsorption dysfunc-
tion of proximal tubules is that the increased levels
S, significant (P ⬍ 0.05). of proteins filtered through the glomerulus because
of its dysfunction may exceed the reabsorption ca-
pacity of the proximal tubules, leading to increased
logical studies revealed that glomerulomegaly is as- urinary microalbumin and total proteinuria concen-
sociated with CCHD.19 In glomerulomegaly, there is trations (Table 2). This evidence is supported by
a selective dilation of afferent arterioles20 that in- results of the present study, which demonstrated
creases the glomerular hydrostatic pressure,21 that as duration of cyanosis increased, the percent-
which in turn causes glomerular capillary dilation22 age of CCHD patients with abnormal levels of prox-
and increasing GFR.21 Thus, it would seem most imal tubular urinary markers was elevated (Table
likely that the increase in the glomerular size prob- 3), and a significant correlation between glomerular
ably transiently alters the size and/or the charge- and tubular dysfunction was present (Table 5), sup-
selective permeability of the glomerular basement porting the observations that proteinuria is related
membrane to protein, allowing an increase in the to decreased tubular function4,6.
protein filtered through the glomerulus. Second, in Among CCHD patients of G2 (duration of cyanosis
patients with CCHD, blood hyperviscosity causes an is ⬍1 year), it was observed that of 11 patients with
overall increase in renal vascular resistance,5 which normal glomerular function (as evidenced by normal
reduces the renal blood flow21 with a rise in intra- urinary excretion of both total protein and mi-
glomerular blood pressure5. Thus, as a greater frac- croalbumin), 9 cases demonstrated elevation of ei-
tion of the plasma flow becomes ultrafiltrate, the ther urinary ␣1M level or urinary NAG activity,
average protein concentration of the plasma remain- suggesting that proximal tubules may be affected
ing within the capillary would rise, accounting in before the glomeruli. This suggestion receives sup-
part for the enhanced proteinuria seen in such cir- port from the work of others,6 who reported that
cumstances. Therefore, hemodynamic changes in urinary NAG activity was elevated among some
the glomerulus may enhance proteinuria, both by CCHD patients without proteinuria. Furthermore,
their effect on the properties of the glomerular wall among CCHD patients of G2, of 5 cases with normal
and by altering the concentration during protein urinary excretion of ␣1M, 3 cases (60%) showed
movement from capillary to the Bowman space. elevated urinary NAG activity, suggesting that
It was observed that results of U.Malb/U.Cr in G2 proximal tubular damage may precede proximal tu-
showed significant decrease in the mean value than bular reabsorption dysfunction.
the controlled group G1. This may be because pa- Data on the effect of palliative surgery in the
tients in G2 are much younger than children in the present study (Table 6) support the finding that
control group C1. acute changes in Hct are accompanied by acute and
Data on the percentage of CCHD patients with reversible changes in renal hemodynamics,22,23 indi-
abnormal levels of glomerular urinary markers (Ta- cating that the extent of Hct elevation plays an
ble 3) and the correlations between the measured important role in the pathogenesis of CCHD-related
parameters in the present study (Table 4) coincide kidney disease. The present results (Table 6) dem-
with the reports of others who found that glomerular onstrated a significant improving effect of palliative
damage is related to both the duration of cyanosis surgery on oxygen saturation and glomerular func-
and the extent to which Hct is elevated4 and that tion (as indicated by decreasing urinary excretion of
glomerular-type proteinuria (microalbuminuria) is both total protein and microalbumin) as well as
correlated with the patient age.6,7 proximal tubular reabsorption function (as revealed
Results of proximal tubular reabsorption function by a significant decrease in urinary ␣1M level) and
in the present study (Table 2) receive support from structural integrity of proximal tubules (as shown
the work of others who reported tubular-type pro- by a significant decrease in urinary activities of LAP
teinuria4 and elevated urinary 2-microglobulin,6 and NAG).
THE AMERICAN JOURNAL OF THE MEDICAL SCIENCES 113
Palliative Surgery in Congenital Cyanotic Heart Disease
In conclusion, both glomerular and proximal tu- tional exposure to nephrotoxins. I. Categories of tests for
bular dysfunction as well as proximal tubular dam- detecting effects of nephrotoxins. Ren Fail 1997;19:505–21.
age occurs in CCHD patients. In addition, the integ- 10. Zuppi C, Baroni S, Scribano D, et al. Choice of time for
rity of proximal tubules may be affected before that urine collection for detecting early kidney abnormalities in
hypertensives. Ann Clin Biochem 1995;32:373– 8.
of the glomeruli. The extent and duration of hypox-
11. Watanabe N, Kamei S, Ohkubo A, et al. Urinary protein
emia as well as elevated Hct are important factors as measured with a pyrogallol red-molybdata complex, man-
predisposing CCHD patients to renal impairment ually and in a Hitachi 726 automated analyzer. Clin Chem
through hemodynamic changes in the glomerulus. 1986;32:1551– 4.
Finally, palliative surgery has a significant improv- 12. Josch W, Dubach DU. Urine-arylamidase. Z Klin Chem
ing effect on Hct and oxygen saturation level as well 1967;5:59 – 63.
as renal glomerular and tubular integrity. There- 13. Thomas GH. -D-Galactosidase in human urine: deficiency
fore, operative correction of the cardiac malforma- in generalized gangliosidosis. J Lab Clin Med 1969;74:725–
tion could improve renal deterioration in CCHD 31.
patients. 14. Bartels H, Bohmer M, Heieli C. Serum kreatininebestim-
mung ohne enteiweissen. Clin Chim Acta 1972;37:193–7.
15. Lemann J Jr., Dowmans BT. Proteinuria in health and
References disease assessed by measuring the urinary protein/creatinine
1. Burke JR, Glasgow EF, McCredie DA, et al. Nephropathy ratio. Clin Chem 1987;33:297–9.
in congenital cyanotic heart disease. Clin Nephrol 1977;7:38 – 16. Woolerton J, Jary DR, Dunn PJ, et al. Urine albumin/
42. creatinine ration and clinical correlates in a diabetic popula-
2. Flanagan MF, Hourihan M, Keane JF. Incidence of renal tion. N Z Med J 1987;100:130 – 4.
dysfunction in adults with cyanotic congenital heart disease. 17. Jung K. Enzyme activities in urine. How should we express
Am J Cardiol 1991;68:403– 6. their excretion? Eur J Clin Chem Clin Biochem 1991;29:
3. Dittrich S, Kurschat K, Dahnert I, et al. Cyanotic ne- 725–9.
phropathy and use of non-ionic contrast agents during car- 18. Perloff JK. Systemic complications of cyanosis in adults
diac catheterization in patients with congenital cyanotic with congenital heart disease. Hematologic derangements,
heart disease. Cardiol Young 2000;10:8 –14. renal function, and urate metabolism. Cardiol Clin 1993;11:
4. Dittrich S, Haas NA, Buhrer C, et al. Renal impairment in 689 –9.
patients with long-standing congenital cyanotic heart dis- 19. Hagley MT, Murphy DP, Mullins D, et al. Decline in
ease. Acta Pediatr 1998;87:949 –54. creatinine clearance in a patient with glomerulomegaly asso-
5. Burlet A, Drukker A, Guignard JP. Renal function in
ciated with a congenital cyanotic heart disease. Am J Kidney
congenital cyanotic heart disease. Nephron 1999;81:296 –300.
6. Akita H, Matsuoa S, Kuroda Y. Nephropathy in patients Dis 1992;20:177–9.
20. Meessen H, Litton MD. Morphology of the kidney in mor-
with cyanotic congenital heart disease. Tokushima J Exp
Med 1993;40:47–53. bus caeruleus. Arch Pathol 1953;56:480 –7.
7. Krull F, Ehrich JHH, Wurster U, et al. Renal involvement 21. Guyton AR, Hall JE. Textbook of medical physiology, 9th
in patients with cyanotic congenital heart disease. Acta Pe- ed. Philadelphia: WB Saunders; 1996. p. 324 –5.
diatr Scand 1991;80:1214 –9. 22. DeJong PE, Weening JJ, Donker AJM, et al. The effect of
8. Rebel W, Bertsch T, Bode G, et al. Enzymuria as indicator phlebotomy on renal function and proteinuria in a patient
of renal pathomorphology. In: Jung K, Mattenheimer H, with congenital cyanotic heart disease. Nephron 1983;33:
Burchardt U, editors. Urinary enzymes in clinical and exper- 225– 6.
imental medicine. Berlin: Springer-Verlag; 1992. p. 43–72. 23. Wilcox CS, Payne J, Harrison DW. Renal function in
9. Mueller PW, Lash LH, Price RG, et al. Urinary biomark- patients with chronic hypoxemia and cor pulmonale following
ers to detect significant effects of environmental and occupa- reversal of polycythemia. Nephron 1982;30:173–7.
114 March 2003 Volume 325 Number 3
You might also like
- Biological ChemistryDocument28 pagesBiological ChemistryArsilan Aziz LoneNo ratings yet
- ABIM Quick Hits For MDsDocument7 pagesABIM Quick Hits For MDscinosure1100% (2)
- Placental AbnormalitiesDocument3 pagesPlacental AbnormalitiesThakoon TtsNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Musculoskeletal RadiologyDocument5 pagesMusculoskeletal Radiologyapi-3743483No ratings yet
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderFrom EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderNo ratings yet
- 2004 FRACP Written Examination Paediatrics & ChildDocument32 pages2004 FRACP Written Examination Paediatrics & ChildMedicEd100% (1)
- Summer Training Guide For Pharmacy Students-1Document132 pagesSummer Training Guide For Pharmacy Students-1Rania T. Sabri100% (2)
- Drug StudyDocument9 pagesDrug StudyJeanette Leigh BravoNo ratings yet
- All Previous Krok ExamsDocument224 pagesAll Previous Krok ExamsOnur KoyuncuNo ratings yet
- Dr. Herbert Situmorang, SpOG - (K) FER - Hyperemesis GravidarumDocument16 pagesDr. Herbert Situmorang, SpOG - (K) FER - Hyperemesis GravidarumDonutz RiNo ratings yet
- Renal PhysiologyDocument7 pagesRenal PhysiologyLucas TheotonioNo ratings yet
- Metabolic Acidosis - An Underestimated Problem After Kidney Transplantation?Document6 pagesMetabolic Acidosis - An Underestimated Problem After Kidney Transplantation?Daphne HernaezNo ratings yet
- Manuscript 1Document4 pagesManuscript 1maryNo ratings yet
- 1 s2.0 S168719792100040X MainDocument4 pages1 s2.0 S168719792100040X MainfelipetheNo ratings yet
- ACPN AbstractsDocument21 pagesACPN AbstractsPediatric NephrologyNo ratings yet
- Circadian Rhythms of Diuresis, Proteinuria and Natriuresis in Children With Chronic Glomerular DiseaseDocument9 pagesCircadian Rhythms of Diuresis, Proteinuria and Natriuresis in Children With Chronic Glomerular DiseaseAulia Arief RhdNo ratings yet
- 10 1093@ndt@gfy270Document8 pages10 1093@ndt@gfy270Luis Mauricio Mozo MeléndezNo ratings yet
- Subjective Global Assessment in Chronic Kidney Disease - A ReviewDocument10 pagesSubjective Global Assessment in Chronic Kidney Disease - A ReviewDiana Laura MtzNo ratings yet
- 11 134 v12n4 2013 PredictingPortalDocument11 pages11 134 v12n4 2013 PredictingPortalDevy Widiya GrafitasariNo ratings yet
- Hyperuricemia Is Associated With Hypertension, Obesity, and Albuminuria in Children With Chronic Kidney DiseaseDocument5 pagesHyperuricemia Is Associated With Hypertension, Obesity, and Albuminuria in Children With Chronic Kidney DiseaseMuh Husni RifaiNo ratings yet
- Ref 14 PDFDocument9 pagesRef 14 PDFFausiah Ulva MNo ratings yet
- Jurnal Thalassemia 4Document10 pagesJurnal Thalassemia 4Lina AnisaNo ratings yet
- Adler 2015Document7 pagesAdler 2015nathaliepichardoNo ratings yet
- Low Alt CKDDocument5 pagesLow Alt CKDFebianti RukmanaNo ratings yet
- A Rare Cause of AA Amyloidosis and End-Stage Kidney Failure: QuestionsDocument3 pagesA Rare Cause of AA Amyloidosis and End-Stage Kidney Failure: QuestionsSezen YılmazNo ratings yet
- 154-The Frequency and Aetiology of Repeated Kidney Injury Episodes Determine The Degree of Renal DamageDocument2 pages154-The Frequency and Aetiology of Repeated Kidney Injury Episodes Determine The Degree of Renal DamageCarlos Martinez SalgadoNo ratings yet
- Adult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesDocument9 pagesAdult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesMutiara RizkyNo ratings yet
- Resuscitation Fluid Composition in Acute Kidney Injury in Critical IllnessDocument2 pagesResuscitation Fluid Composition in Acute Kidney Injury in Critical IllnessDe Frede EditoreNo ratings yet
- Dickson 1989Document7 pagesDickson 1989Necesito esta cuentaNo ratings yet
- CLN 66 06 991 PDFDocument5 pagesCLN 66 06 991 PDFyenny handayani sihiteNo ratings yet
- AlopurinolDocument10 pagesAlopurinoljoselyne carrascoNo ratings yet
- Nejm ArticleDocument10 pagesNejm ArticlePabloNo ratings yet
- Hypokalemia in CKDDocument9 pagesHypokalemia in CKDGoris HariyadiNo ratings yet
- Reliability of Mini Nutritional Assessment in Hemodialysis Compared With Subjective Global AssessmentDocument6 pagesReliability of Mini Nutritional Assessment in Hemodialysis Compared With Subjective Global AssessmentyafanitaizzatiNo ratings yet
- Giglio 2018Document11 pagesGiglio 2018yafanitaizzatiNo ratings yet
- (03241750 - Acta Medica Bulgarica) The Heparanase Inhibitor (Sulodexide) Decreases Urine Glycosaminoglycan Excretion and Mitigates Functional and Histological Renal Damages in Diabetic RatsDocument6 pages(03241750 - Acta Medica Bulgarica) The Heparanase Inhibitor (Sulodexide) Decreases Urine Glycosaminoglycan Excretion and Mitigates Functional and Histological Renal Damages in Diabetic RatsTeodorNo ratings yet
- Chronic Kidney Disease in Children and AdolescentsDocument16 pagesChronic Kidney Disease in Children and AdolescentsFernanda SierraNo ratings yet
- Stability of Urinary AKI Biomarkers Over TimeDocument6 pagesStability of Urinary AKI Biomarkers Over TimeHervita YeniNo ratings yet
- SC 2015242Document7 pagesSC 2015242resi ciruNo ratings yet
- Single BlindedDocument5 pagesSingle BlindedERNI FORWATYNo ratings yet
- Jurnal AKIDocument7 pagesJurnal AKIAnonymous Vz9teLNo ratings yet
- Nej Mo A 1915833Document10 pagesNej Mo A 1915833Tensa ZangetsuNo ratings yet
- Nejmoa 1813599Document10 pagesNejmoa 1813599Ahmed El RashedyNo ratings yet
- The New Age of Renal Biomarkers - Does SDMA Solve All of Our ProblemsDocument11 pagesThe New Age of Renal Biomarkers - Does SDMA Solve All of Our ProblemsCabinet VeterinarNo ratings yet
- Am J Ophthalmol 2004 - p401Document6 pagesAm J Ophthalmol 2004 - p401Abrilia OctafijayantiNo ratings yet
- Endocrine abnormalities in children with beta thalassemia majorDocument6 pagesEndocrine abnormalities in children with beta thalassemia majorKrisbiyantoroAriesNo ratings yet
- Tgi Erc 3Document10 pagesTgi Erc 3Adrian LaimeNo ratings yet
- Izumita 2020Document5 pagesIzumita 2020AsimaJulianaSiregarNo ratings yet
- Large-Volume Paracentesis in The Management of Ascites in ChildrenDocument5 pagesLarge-Volume Paracentesis in The Management of Ascites in ChildrenMed MorciNo ratings yet
- Dialysis Free Protocol For Some End Stage Renal Disease PatientsDocument7 pagesDialysis Free Protocol For Some End Stage Renal Disease PatientsDannieCiambelliNo ratings yet
- Sharawey2011 PDFDocument7 pagesSharawey2011 PDFIkram DibNo ratings yet
- s11255-018-1819-8Document8 pagess11255-018-1819-8Aaron Paul BernasNo ratings yet
- Nocturnal PD Better For OSA Than CAPDDocument9 pagesNocturnal PD Better For OSA Than CAPDsavvy_as_98No ratings yet
- Lec - S32 Injuria RenalDocument8 pagesLec - S32 Injuria RenalEvelyn EstradaNo ratings yet
- 2018 Article 31727Document11 pages2018 Article 31727Jackson HakimNo ratings yet
- 1899 FullDocument6 pages1899 Fullmelanita_99No ratings yet
- Lipid Profile in CKDDocument4 pagesLipid Profile in CKDAmiyanshu BeheraNo ratings yet
- 2008.clin Chem - RantnerDocument7 pages2008.clin Chem - RantnertwkangNo ratings yet
- Model For End Stage Liver Disease (MELD) and Child-TurcottePugh (CTP) PDFDocument4 pagesModel For End Stage Liver Disease (MELD) and Child-TurcottePugh (CTP) PDFPaulus AnungNo ratings yet
- Urinary Gamma-Glutamyl Transferase and The Degree of Renal Dysfunction in 75 Bitches With PyometraDocument32 pagesUrinary Gamma-Glutamyl Transferase and The Degree of Renal Dysfunction in 75 Bitches With Pyometraసాయిమహేష్రెడ్డిఆవులNo ratings yet
- 1 Ajaz 2012Document4 pages1 Ajaz 2012Olivia Valentine LekiNo ratings yet
- Güven2015 Article GonadotropinReleasingHormoneAnDocument7 pagesGüven2015 Article GonadotropinReleasingHormoneAnFunnie AdeliaNo ratings yet
- EnalaprilDocument6 pagesEnalaprilEduardo EvangelistaNo ratings yet
- Kocyigit 2012Document8 pagesKocyigit 2012Rengganis PutriNo ratings yet
- The Relation Between Liver Histopathology and GGT Levels in Viral Hepatitis: More Important in Hepatitis BDocument5 pagesThe Relation Between Liver Histopathology and GGT Levels in Viral Hepatitis: More Important in Hepatitis BTanveerNo ratings yet
- Spider Angiomas in Patients With Liver Cirrhosis: Role of Vascular Endothelial Growth Factor and Basic Fibroblast Growth FactorDocument4 pagesSpider Angiomas in Patients With Liver Cirrhosis: Role of Vascular Endothelial Growth Factor and Basic Fibroblast Growth FactorChrizzna HaryantoNo ratings yet
- Sasjs 810 658-662 FTDocument5 pagesSasjs 810 658-662 FTrifa iNo ratings yet
- Albuminuria, Cerebrovascular Disease and Cortical Atrophy: Among Cognitively Normal Elderly IndividualsDocument8 pagesAlbuminuria, Cerebrovascular Disease and Cortical Atrophy: Among Cognitively Normal Elderly IndividualsYuna Rezkya Kartika YuzanNo ratings yet
- Biopsy - An OverviewDocument9 pagesBiopsy - An OverviewNadya AyuNo ratings yet
- Myocardial BridgingDocument13 pagesMyocardial BridgingAsik AliNo ratings yet
- Oxigenoterapia Parte 2 Indicaciones y ToxicidadDocument9 pagesOxigenoterapia Parte 2 Indicaciones y ToxicidadyeseyeseprimisNo ratings yet
- Material 3 - Acute Kidney Injury in Children - Fauziah Rudhiati, MKep., Sp. Kep - An PDFDocument21 pagesMaterial 3 - Acute Kidney Injury in Children - Fauziah Rudhiati, MKep., Sp. Kep - An PDFINTAN MADULARANo ratings yet
- Optic Nerve Damage from High Intracranial PressureDocument31 pagesOptic Nerve Damage from High Intracranial Pressurejeanne_mbNo ratings yet
- Treatment For Subdural HygromaDocument3 pagesTreatment For Subdural HygromaEka NataNo ratings yet
- Bimbingan Muskuloskeletal CoassDocument224 pagesBimbingan Muskuloskeletal CoassMichael AndhitoNo ratings yet
- Peptic Ulcer DiseaseDocument51 pagesPeptic Ulcer DiseasedocsNo ratings yet
- Types of DoctorsDocument29 pagesTypes of DoctorsEduardo Brier VelascoNo ratings yet
- Anemia by Harsha BJDocument23 pagesAnemia by Harsha BJnaveen kumar kushwahaNo ratings yet
- Breast EndocrineDocument124 pagesBreast EndocrineNguyễn Nhật HoàngNo ratings yet
- Evaluation of The Ruminant Complete Blood Dell CountDocument26 pagesEvaluation of The Ruminant Complete Blood Dell CountDirección Científica Laboratorio VitalabNo ratings yet
- DiphenhydrAMINE Monograph For ProfessionalsDocument12 pagesDiphenhydrAMINE Monograph For Professionalsioana teodorescuNo ratings yet
- Mode Selection For Positive Airway Pressure Titration in Adult Patients With Central Sleep Apnea Syndromes - UpToDateDocument16 pagesMode Selection For Positive Airway Pressure Titration in Adult Patients With Central Sleep Apnea Syndromes - UpToDatedavimemNo ratings yet
- CV Europass GB FlorinaMoldovanDocument4 pagesCV Europass GB FlorinaMoldovanmihaicornelNo ratings yet
- Understanding Idiopathic Intracranial HypertensionDocument12 pagesUnderstanding Idiopathic Intracranial HypertensionEBNo ratings yet
- Daftar Pustaka KolelitiasisDocument2 pagesDaftar Pustaka KolelitiasisReni IstiarNo ratings yet
- AIA PCP Eng FA 20140605 HKDocument6 pagesAIA PCP Eng FA 20140605 HKJosephQuentinNo ratings yet
- Enfermedad de AlzheimerDocument10 pagesEnfermedad de AlzheimerJessicaNo ratings yet
- Avascular NecrosisDocument13 pagesAvascular Necrosisnagarajs50No ratings yet
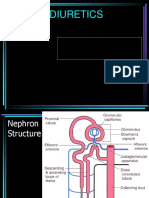
- DIURETICSDocument39 pagesDIURETICSFrancisNo ratings yet