Professional Documents
Culture Documents
Clinical Effect of Periodontal Pocket Irrigation with H2O2
Uploaded by
Lisa Noor SetyaningrumOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Effect of Periodontal Pocket Irrigation with H2O2
Uploaded by
Lisa Noor SetyaningrumCopyright:
Available Formats
Received: Oct.
2010
Original Article Accepted: Jan. 2010
Clinical Effect of Periodontal Pocket Irrigation with H2O2
Sahebjam Atabaki, M.* Moradi Haghgoo, J.** Khoshhal, M. **Arabi, R. **
Khodadoostan, A.** Gholami, L.***
*Assistant Professor, Department of Priodontology, Faculty of Dentistry, Esfahan University of Medical Sciences,
Esfahan, Iran.
**Assistant Professor, Department of Priodontology, Faculty of Dentistry, Hamadan University of Medical Sciences,
Hamadan, Iran.
** Post graduate student of Periodontology, Faculty of Dentistry, Hamadan University of Medical Sciences,
Hamadan, Iran.
ABSTRACT
Statement of the problem: Subgingival irrigation with an antimicrobial agent after scaling and
root planing (SRP) is assumed to be able to kill the bacteria left behind after mechanical
debridement. 3% H2O2 is used in the treatment of periodontal disease and it has been shown
effective in killing anaerobic pathogens.
Purpose: The aim of this study was to evaluate the clinical effects of subgingival irrigation of
periodontal pockets with 3% H2O2.
Materials and methods: Thirty-five patients with probing depths of 3‒5 mm were selected for the
study. All the oral cavity sites were scored at baseline and on days 21 and 35 for these periodontal
indices: gingival bleeding on probing, probing depth, and attachment level. The pockets in various
quadrants were randomly assigned to professionally performed subgingival irrigation with 3%
H2O2 or saline or to non-irrigation groups on baseline and days 7 and 14 after the first step of
therapy with SRP and oral hygiene instruction.
Results: The results showed that subgingival irrigation with 3% H2O2 produced a significant
reduction in gingival bleeding index compared to the control while there were no significant
differences between the 3 groups in probing depth reduction. Irrigation with H2O2 also resulted in
a significant reduction of attachment levels between the 3 groups on day 21.
Conclusion: The results of the present study indicate that subgingival irrigation with 3% H2O2
plays a potential role in inflammation control and reduction of gingival bleeding.
Keywords: Periodontal pocket, attachment level, gingival bleeding index, scaling and root
planing, therapeutic irrigation.
INTRODUCTION periodontitis is based on destroying the
plaque or altering its structure.(1) The first
In the pathogenesis of the infectious disease
step of the different stages of treatment
of periodontitis bacterial plaque is
consists of scaling and root planing (SRP),
considered the culprit and the treatment of
oral hygiene instruction, and proper plaque
Corresponding Author: J. Moradi Address:
Assisstant Professor, Dept. of Priodontology of
control by the patient. Mechanical
Faculty of Dentistry of Hamadan University of debridement of deep pockets is not usually
Medical Sciences, Fahmideh Blv, Hamadan, Iran. completely possible and there are
Tel: +98 811 8354018 Email: Jmoradi@umsah.ac.ir
subgingival plaque and calculus left
DJH 2011; Vol.3, No.1 53
Moradi et al. Clinical Effect of Periodontal Pocket …
behind.(2,3) Subgingival irrigation using an NaHCO3 can decrease subgingival
antimicrobial agents following SRP is microorganism counts, including
based on the assumption that the remaining spirochetes and motile rods and
bacteria after medical debridement can be significantly enhance the microbiological
destroyed this way.(1) To be effective, this and clinical effects of periodontal scaling
irrigation should be carried out after careful and root planing.(11)
SRP and the irrigation solution should be In 1987 Wennström et al studied the
(4)
able to reach all tooth surfaces. clinical effect of professionally performed
Some researchers believe that compared to periodic subgingival irrigation per se and as
SRP as a solitary therapy subgingival an adjunct to scaling and root planing in
irrigation does not have much further patients suffering from moderate/severe
clinical benefits.(5) periodontal disease. The results revealed
Hydrogen peroxide has been used in that repeated professional irrigation of
dentistry in combination with salts or alone unscaled periodontal pockets with
for over 70 years. Therapeutic delivery of chlorhexidine or hydrogen peroxide
H2O2 to prevent periodontal disease resulted in a temporarily reduced frequency
requires mechanical access to subgingival of bleeding sites, with no clinically
pockets. Furthermore, wound healing significant changes in probing assessments.
following gingival surgery is enhanced due A similar improvement in bleeding scores
to the antimicrobial effects of topically was observed in the saline-irrigated control
administered hydrogen peroxide. For most group. The study failed to demonstrate that
subjects, beneficial effects have been seen professionally performed periodic
(6)
seen with H2O2 levels above 1%. subgingival irrigation with chlorhexidine or
Hydrogen peroxide has been shown to hydrogen peroxide used alone or in
possess a wide spectrum of antimicrobial combination with thorough mechanical
activity in that it is active against bacteria, debridement, has a significant therapeutic
yeasts, fungi, viruses and spores.(7‒9) effect.(12)
In 1982 Wolff et al studied the effect of 3% Subgingival irrigation with a suitable agent
H2O2 on gingival inflammation and currently constitutes an effective adjunct to
concluded that 3% H2O2 is effective in the simplified oral hygiene regimen that
reducing pocket depth of more than 4 mm does not require unrealistic levels of
but it showed no effect on bleeding and interdental or subgingival home-care
(10) (13)
other gingival indices. cleaning by the patient. In a recent study
Rosling et al reported in 1983 that subgingival irrigation with high
professional and personal subgingival concentrations of tetracycline was found to
application of a mixture of H2O2-NaCl and play a beneficial role in the management of
54 DJH 2011; Vol.3, No.1
Moradi et al. Clinical Effect of Periodontal Pocket …
patients with chronic periodontitis.(14) gingival sulcus bleeding using a probe, the
Targeted lavage and subgingival delivery of probe is gently moved through the margins
effective antimicrobial agents show around a tooth; after 10 seconds presence or
potential as supplemental office procedures absence of bleeding is evaluated.
or as a component of a home oral hygiene The first phase of treatment, consisting of
regime. Additional research is needed to OHI and full-mouth SRP, was
develop more efficacious chemotherapeutic carefully performed on each patient. SRP
substances than are currently available and was carried out using a piezoelectric
to further define the optimum application of ultrasonic device (Cavitron EM, Dentsply).
15
each. Considering the role of anaerobic Each quadrant in each patient’s mouth was
bacteria in periodontal diseases and the randomly treated with 3% H2O2 subgingival
ecosystem in periodontal pockets that irrigation in one quadrant and normal saline
allows microbial growth we decided to was used for irrigation in the other quadrant
investigate the effect of subgingival and the two other quadrants were treated
irrigation with H2O2 and the destructive with SRP alone. Subgingival irrigation was
effects of its free oxygen radicals. performed at baseline and after 1 and 2
MATERIALS AND METHODS weeks. The clinical parameters were
Thirty-five patients who had been referred recorded at baseline at the end of week 3
to the Department of Periodontics, Isfahan and at the end of week 5.
Dental, School, signed informed consent Data was analyzed with SPSS 11. T-test
forms and were enrolled in this study. was used to compare mean probing depths,
Patients' dental and medical histories were attachment levels, and gingival bleedings
obtained. The patients had no systematic before and after treatment. The mean
diseases such as diabetes, blood pressure, clinical parameters of the 3 groups in the
and hematologic, cardiovascular or renal different stages of the study were also
disorders. None of them had taken any compared using ANOVA.
antibiotics or used any kind of mouthrinses RESULTS
in the previous 3 months and had mild to
According to the results of comparison of
moderate chronic periodontitis with pocket
the mean probing depths before and after
depths of 3‒5 mm
treatment (before the first treatment phase
The clinical indices of patients were
or baseline (0), 3 weeks after
recorded at baseline: attachment level,
first treatment phase (after-1) and 5 weeks
pocket depth (by William’s probe)
after treatment (after-2), a statistically
and gingival bleeding (Ainano and Bay's
significant difference observed (P<0.001)
method).(1)
(Table 1)
In this simple method for investigating
In addition, there were significant
DJH 2011; Vol.3, No.1 55
Moradi et al. Clinical Effect of Periodontal Pocket …
differences between (0) and after-1 and difference was not significant in after-2
after-2 and between after-2 and after-1 in (Table 4)
the mean attachment levels (Table 2). The mean gingival bleeding index showed a
There was also a significant difference difference that was statistically significant
between mean attachment levels between between (0) and after-1 and (0) and after- 2
the 3 study groups in (0) and after-1 but the (Table 3)
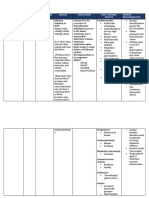
Table 1. Comparison of mean probing depths before and after the initial treatment phase
Treatment stages Mean ± δ p
0 2.62±0.42
After-1 2.02±0.37
0 2.62±0.42
P<0.001
After-2 1.79±0.34
After-1 2.02±0.37
After-2 1.79±0.34
Table 2. Comparison of attachment levels before and after treatment
Treatment stages Mean ± δ P
0 1.57±0.41
After-1 1.28 ±0.26
0 1.57±0.41
P<0.001
After-2 1.21±0.21
After-1 1.28 ±0.26
After-2 1.21±0.21
Table 3. Comparison of the mean gingival bleeding index
Treatment stages Mean ± δ P
0 27.08±13.42
After-1 6.9 ±6.95
0 27.08±13.42 P<0.001
After-2 6.57±6.68
After-1 6.9 ±6.95
After-2 6.57±6.68
56 DJH 2011; Vol.3, No.1
Moradi et al. Clinical Effect of Periodontal Pocket …
Table 4: Comparing mean attachment levels in the three different treatment groups
First Phase of
Treatment Normal Saline Hydrogen Peroxide
P P Treatment (SRP) P
stages Mean ± δ Mean ± δ
Mean ± δ
(0) 1.43±0.36 1.76±0.42 25
0.4
After-1 1.22±0.23 0.002 1.38±0.29 0.0271 1.98±0.23
2
After-2 1.19±0.21 1.25±0.22 1.20±0.19
DISCUSSION In Wolff’s study % H2O2 had a positive
This study was conducted to evaluate the effect on depth reduction in pockets more
clinical effect of subgingival irrigation with than 4 mm deep. A study by Wolff et al
20 mL of 3% H2O2. The results showed showed that an oxidizing agent containing
significant reduction in gingival bleeding H2O2 had a positive effect on probing depth
compared to normal saline and SRP alone, compared with SRP alone.(16)
reaching from 28.95±14.02 to 1.11±6.98 in The results of the present study showed that
the H2 O2 group but from 24.95±13.3 to in the 3% H2 O2 group 3 weeks after the first
9.11±6.98 by normal saline and from phase of treatment there was a greater gain
27.34±12.99 to 9.5±5.47 by SRP alone, in attachment level, reaching from
which is different from what Wolff reported 1.76±0.42 to 1.38±0.4 mm in the H2O2
in 1982.(10) group in week 3 and from 1.43±0.36 to
Many studies have considered gingival 1.22±0.23 in the normal saline group and
bleeding as a sensitive index of evaluating from 1.51±0.39 to 1.25±0.23 with SRP
primary gingival inflammation. BOP is alone but in week 5 there were no
considered a good marker for periodontal significant differences between the 3 groups
health.(1) regarding attachment gain. Wolff's study
According to the results, 3% H2O2 had no also showed that H2O2 was more effective
significant effect on probing depth in attachment gain than SRP alone.(16)
compared to the other two groups. In the Since these results were significantly
H2O2 group mean probing depth changed different between the 3 groups at week 3
from 2.77±0.44 to 1.72±0.36 mm and in the but not week 5 it can be concluded that
normal saline group it decreased from attachment gain in the H2O2 group was
2.54±0.37 mm to 1.8±0.37 mm and from faster than the other groups. Changes in
2.56±0.41 to 1.85±0.31 for the SRP group. attachment level are a result of losing or
DJH 2011; Vol.3, No.1 57
Moradi et al. Clinical Effect of Periodontal Pocket …
building an attachment, which better consider when comparing probing depths
correspond to the amount of periodontal before and after treatment; reduction in
destruction. probing depth might be more as a result of
Clinical attachment level shows the amount remission of inflammation rather than
of root surface without PDL whereas the attachment gain.
pocket depth is less important since it is not It can concluded from this study that
always related to bone level. Periodontal subgingival irrigation with 3% H2O2 is
attachment is also a mechanical barrier effective in reducing gingival bleeding and
against microorganisms and the earlier it is inflammation and also in the speed in
established the more resistance there is gaining an attachment, demonstrating a
against microorganisms and a lower chance positive clinical effect compared to SRP
of periodontal diseases recurrence. alone. Still successful periodontal therapy
An important thing is that in a periodontal will always remain dependent on patient
pocket the probe penetrates approximately compliance to regular professional and
0.3 mm into the JE and connective tissue, home care.
which can be important to have in mind and
REFRENCES 6.Marshall MV, Cancro LP, Fischman SL.
1.Newman MG, Taki HH, Carranza FA, Hydrogen peroxide: a review of its use in
Carranza's Clinical Periodontology: WB dentistry. J Periodontol 1995;Sep;66(9):786‒96.
Saunders Co. Philadelphia: USA, 2002: 96‒100 7.Brudzynski K. Effect of hydrogen peroxide on
2.Albandar JM, Brunelle JA, Kingman A. antibacterial activities of Canadian honeys. Can
Destructive periodontal disease in adults 30 J Microbiol. 2006; 52(12):1228–37.
years of age and older in the united states . J 8.Glockmann E, Wiesner J, Oehring H,
periodontal 1999; 70(1):13‒29. Glockmann I. Antibacterial efficiency and
3.Allbandar JM, Kingman A. Gingival toxicity of hydrogen peroxide and other
Recession, Gingival bleeding and dental antiseptics. Dutsch Stomatol 1990; 40(11):462–
calculus in adults 30 years of age and older in 3.
the United States. J periodontal 1999; 9.Tschernjawskaja MA, Belowa AS.
70(1):30‒43. Antibacterial mechanism of action of hydrogen
4.Douglasss CW, Fox CH, Wilson RF. Cross peroxide preparations. Z Gesamte Hyg 1990;
sectional studies in periodontal disease current 36(2):86–8.
status and implications for dental practice. Adv 10.Wolff LF, Bandt C, Pihlstrom B, Brayer L.
Dent Res 1993; 7(1)25‒31. Phase contrast microscopic evaluation of
5.THE AMERICAN ACADEMY OF subgingival plaque in combination with either
PERIODONTOLOGY. Translating findings of conventional or antimicrobial home treatment of
systematic reviews into consensus statements on patients with periodontal inflammation. J
periodontal therapy. J Am Dent Assoc 2004 Periodontal Res. 1982 Sep; 17(5):537‒40.
Aug; 135(8):1099‒107. 11.Rosling BG, Slots J, Webber RL,
58 DJH 2011; Vol.3, No.1
Moradi et al. Clinical Effect of Periodontal Pocket …
Christersson LA, Genco RJ. Microbiological
and clinical effects of topical subgingival
antimicrobial treatment on human periodontal
disease. J Clin Periodontol 1983; Sep;
10(5):487‒514.
12.Wennström JL, Heijl L, Dahlén G, Gröndahl
K. Periodic subgingival antimicrobial irrigation
of periodontal pockets (I). Clinical observations.
J Clin Periodontol 1987; Oct; 14(9):541‒50.
13.Newman HN. Periodontal pocket irrigation
as adjunctive treatment. Curr Opin Periodontol
1997; 4:41-50.
14.Krishna MK, Ravindran SK, Vivekanandan
G, Navasivayam A, Thiagarajan R, Mohan R.
Effects of a single episode of subgingival
irrigation with tetracycline HCl or
chlorhexidine: A clinical and microbiological
study. J Indian Soc Periodontol 2011 Jul;
15(3):245‒9.
15.Stein M. A literature review: oral irrigation
therapy. The adjunctive roles for home and
professional use. Probe.1993; Jan-Feb;
27(1):18‒25.
16.Wolff LF, Pihlstrom BL, Bakdash MB,
Schaffer EM, Aeppli DM, Bandt CL. Four-year
investigation of salt and peroxide regimen
compared with conventional oral hygiene. J Am
Dent Assoc1989; Jan; 118(1):67‒72.
DJH 2011; Vol.3, No.1 59
You might also like
- SPG-Hospital 3rd EditionDocument118 pagesSPG-Hospital 3rd Editionira_blissNo ratings yet
- (Oklahoma Notes) Pamela S. Miles M.D., William F. Rayburn M.D., J. Christopher Carey M.D. (Auth.) - Obstetrics and Gynecology (1994, Springer US)Document224 pages(Oklahoma Notes) Pamela S. Miles M.D., William F. Rayburn M.D., J. Christopher Carey M.D. (Auth.) - Obstetrics and Gynecology (1994, Springer US)Muskan DasNo ratings yet
- Chapter 17 Maxillary Sinus - SlidesDocument40 pagesChapter 17 Maxillary Sinus - SlidesRajat GuptaNo ratings yet
- Parenteral Products: The Preparation and Quality Control of Products for InjectionFrom EverandParenteral Products: The Preparation and Quality Control of Products for InjectionNo ratings yet
- IM ITE D: Reading Sub-TestDocument20 pagesIM ITE D: Reading Sub-TestAlwin BrightNo ratings yet
- Jctres07202105003 EpubDocument18 pagesJctres07202105003 Epubسامر مضحيNo ratings yet
- Comparative Evaluation of Chlorhexidine and Hydrogen Peroxide Mouth Wash Among Patients With GingivitisDocument5 pagesComparative Evaluation of Chlorhexidine and Hydrogen Peroxide Mouth Wash Among Patients With GingivitisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Vol09 2 84-88strDocument5 pagesVol09 2 84-88strJoe Sam AbrahamNo ratings yet
- Periodontal Infection Control: Current Clinical ConceptsDocument10 pagesPeriodontal Infection Control: Current Clinical ConceptsNunoGonçalvesNo ratings yet
- Wjoud 11 221Document5 pagesWjoud 11 221ReshmaaRajendranNo ratings yet
- Mouthash 10daysDocument7 pagesMouthash 10dayssamanvi badriNo ratings yet
- Efectele IrigatieiDocument9 pagesEfectele IrigatieiKlaudynhooq JaudyNo ratings yet
- GJHS 8 211Document6 pagesGJHS 8 211Susi SimangunsongNo ratings yet
- Comparative evaluation of curcumin and chlorhexidine irrigation for chronic periodontitisDocument7 pagesComparative evaluation of curcumin and chlorhexidine irrigation for chronic periodontitissamanvi badriNo ratings yet
- Carranza's Clinical Periodontology 2002Document6 pagesCarranza's Clinical Periodontology 2002Lia Optimeze Alwayz100% (1)
- The Topical Effect of Chlorhexidine and Povidone-Iodine in The Repair of Oral Wounds. A ReviewDocument7 pagesThe Topical Effect of Chlorhexidine and Povidone-Iodine in The Repair of Oral Wounds. A ReviewMario CastroNo ratings yet
- Oral Care in Ventilation MechanicDocument8 pagesOral Care in Ventilation MechanicRusida LiyaniNo ratings yet
- Dehghan IDocument7 pagesDehghan IincisivusNo ratings yet
- LDD in Period On TicsDocument6 pagesLDD in Period On TicsAstridNo ratings yet
- A. Pilloni Et Al. (2021) - Treatment of Residual Periodontal Pockets Using A Hyaluronic GelDocument15 pagesA. Pilloni Et Al. (2021) - Treatment of Residual Periodontal Pockets Using A Hyaluronic Gelvalentin.c.serbanNo ratings yet
- Efficacy of Xanthan Based Chlorhexidine Gel As AnDocument5 pagesEfficacy of Xanthan Based Chlorhexidine Gel As AnMai ThúyNo ratings yet
- Hyaluronic AcidDocument7 pagesHyaluronic Acidsamanvi badriNo ratings yet
- 1Document15 pages1محمد ابوالمجدNo ratings yet
- Periodontal Tray Application of Chlorine Dioxide Gel As An Adjunct To Scaling and Root Planing in The Treatment of Chronic PeriodontitisDocument6 pagesPeriodontal Tray Application of Chlorine Dioxide Gel As An Adjunct To Scaling and Root Planing in The Treatment of Chronic PeriodontitisPhuong ThaoNo ratings yet
- JIntClinDentResOrgan62103-2760784 074007Document4 pagesJIntClinDentResOrgan62103-2760784 074007daniel_siitompulNo ratings yet
- Irrigacion Iodo Vs Agua OxigenadaDocument5 pagesIrrigacion Iodo Vs Agua OxigenadaAlanis BuenrostroNo ratings yet
- Influence of Periodontal Treatment On Subgingival and Salivary MicrobiotasDocument9 pagesInfluence of Periodontal Treatment On Subgingival and Salivary MicrobiotasRabiatul AdawiyahNo ratings yet
- Tratamiento de Boca Completa Versussuperficie de La Raíz Del Cuadrante Desbridamiento en El Tratamientode Periodontitis Crónicauna Revisión SisDocument11 pagesTratamiento de Boca Completa Versussuperficie de La Raíz Del Cuadrante Desbridamiento en El Tratamientode Periodontitis Crónicauna Revisión SisNessa Barek VonMillerNo ratings yet
- OzonearticleDocument9 pagesOzonearticleسامر مضحيNo ratings yet
- Nonsurgical Periodontal Therapy DCNADocument12 pagesNonsurgical Periodontal Therapy DCNAdhwanit31No ratings yet
- Rare Case of Odontogenic Infection Extending to Temporal SpaceDocument5 pagesRare Case of Odontogenic Infection Extending to Temporal SpaceAyu SawitriNo ratings yet
- Clinically Proven Herbal Toothpaste in Sri LankaDocument7 pagesClinically Proven Herbal Toothpaste in Sri LankaYoga ChanNo ratings yet
- Hidroxido 1Document5 pagesHidroxido 1Natalia MosqueraNo ratings yet
- A Possible Alternative and Safe Adjunctive Role Forlocally Appliedmangiferinin Periodontal Therapy A Clinical and Microbiological StudyDocument15 pagesA Possible Alternative and Safe Adjunctive Role Forlocally Appliedmangiferinin Periodontal Therapy A Clinical and Microbiological StudyIJAR JOURNALNo ratings yet
- 02 Antimicrobial AgentsDocument10 pages02 Antimicrobial AgentssandipladaniNo ratings yet
- Case Report Treatment of A Periodontic-Endodontic Lesion in A Patient With Aggressive PeriodontitisDocument10 pagesCase Report Treatment of A Periodontic-Endodontic Lesion in A Patient With Aggressive PeriodontitissulistiyaNo ratings yet
- Effect of Fixed: Orthodontic Treatment On Salivary Flow, PH and Microbial CountDocument5 pagesEffect of Fixed: Orthodontic Treatment On Salivary Flow, PH and Microbial CountAndré FonsecaNo ratings yet
- 11th JC - SINDHUDocument22 pages11th JC - SINDHUDadi SindhuNo ratings yet
- Bacteriologic-Conditions-of-the-Apical-Root-Canal-Document10 pagesBacteriologic-Conditions-of-the-Apical-Root-Canal-channadrasmaNo ratings yet
- Management of Chronic Gingivitis PDFDocument5 pagesManagement of Chronic Gingivitis PDFliaamNo ratings yet
- The Clinical Effect of Diode Laser in The Treatment of The Periodontal Pockets in Comparison With The Use of Photodynamic TherapyDocument18 pagesThe Clinical Effect of Diode Laser in The Treatment of The Periodontal Pockets in Comparison With The Use of Photodynamic TherapyAthenaeum Scientific PublishersNo ratings yet
- Current Treatment of Oral Candidiasis A Literature ReviewDocument8 pagesCurrent Treatment of Oral Candidiasis A Literature ReviewRonaldo PutraNo ratings yet
- Expert Consensus On Irrigation and Intracanal Medication in Root Canal TherapyDocument10 pagesExpert Consensus On Irrigation and Intracanal Medication in Root Canal Therapydocbsg21No ratings yet
- BJMP 2012 5 1 A512Document5 pagesBJMP 2012 5 1 A512maslikanNo ratings yet
- Analysis of Oral Microbiome on TADs Under Different Hygiene ConditionsDocument19 pagesAnalysis of Oral Microbiome on TADs Under Different Hygiene Conditionsshyama pramodNo ratings yet
- New Tendencies in Non-Surgical Periodontal TherapyDocument18 pagesNew Tendencies in Non-Surgical Periodontal TherapyGustavo MoreraNo ratings yet
- Int J Dental Hygiene - 2023 - Tahery - Microbiological Status at Intake in Relation To Clinical Periodontal Status atDocument12 pagesInt J Dental Hygiene - 2023 - Tahery - Microbiological Status at Intake in Relation To Clinical Periodontal Status atmisulica2010No ratings yet
- Analyze The Clinical Effect of YAG Laser CombinedDocument9 pagesAnalyze The Clinical Effect of YAG Laser CombinedJose Luis AnayaNo ratings yet
- Taneja2011 PDFDocument5 pagesTaneja2011 PDFمعتزعليNo ratings yet
- Ocr 12237Document11 pagesOcr 12237André FonsecaNo ratings yet
- 2794Document11 pages2794RodolfoDamásioNunesNo ratings yet
- JR PerioDocument11 pagesJR PerioPutra ZulhamNo ratings yet
- 12 Sequel To Renal Transplant An Oral Physician's PerspectiveDocument5 pages12 Sequel To Renal Transplant An Oral Physician's PerspectivevinhannyNo ratings yet
- Sjournal Homepage: - : Manuscript HistoryDocument5 pagesSjournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- 22826Document9 pages22826Ghina Mukti LuthfiaNo ratings yet
- JCDR 9 ZC29Document5 pagesJCDR 9 ZC29سامر مضحيNo ratings yet
- Chen 2012Document8 pagesChen 2012Hamza GaaloulNo ratings yet
- Porphyromonas Gingivalis in Infected Root CanalsDocument7 pagesPorphyromonas Gingivalis in Infected Root CanalsJanneth ValdiviesoNo ratings yet
- Periodontology 2000 - 2022 - Schwarz - Surgical therapy of peri‐implantitisDocument37 pagesPeriodontology 2000 - 2022 - Schwarz - Surgical therapy of peri‐implantitisISABEL ESCOBAR MINOTASNo ratings yet
- The Effect of Listerine Mouthwash On Dental Plaque Gingival Inflammation and C Reactive Protein CRP 2161 1122.1000191Document5 pagesThe Effect of Listerine Mouthwash On Dental Plaque Gingival Inflammation and C Reactive Protein CRP 2161 1122.1000191Bagus RahmawanNo ratings yet
- Residual Antibacterial Effects of A Mixture of Silver Nanoparticles/calcium Hydroxide and Other Root Canal Medicaments Against Enterococcus FaecalisDocument6 pagesResidual Antibacterial Effects of A Mixture of Silver Nanoparticles/calcium Hydroxide and Other Root Canal Medicaments Against Enterococcus FaecalisYunda RagilNo ratings yet
- Chapter 03 Positioning Errors in Panoramic Radiography PDFDocument11 pagesChapter 03 Positioning Errors in Panoramic Radiography PDFLisa Noor SetyaningrumNo ratings yet
- Normal Radiographic Dental AnatomyDocument117 pagesNormal Radiographic Dental AnatomyKamal ShantoNo ratings yet
- Journal of Oral RehabilitationDocument8 pagesJournal of Oral RehabilitationLisa Noor SetyaningrumNo ratings yet
- Journal Oral MedicineDocument3 pagesJournal Oral MedicineLisa Noor SetyaningrumNo ratings yet
- Office of The Dean / Chief Executive: Medical Teaching Institution GKMC/BKMC SwabiDocument11 pagesOffice of The Dean / Chief Executive: Medical Teaching Institution GKMC/BKMC SwabiRubeenaNo ratings yet
- Clinico-Aetiological Profile of Pancytopenia in Paediatric PracticeDocument4 pagesClinico-Aetiological Profile of Pancytopenia in Paediatric PracticeDesi AdiyatiNo ratings yet
- 1 SMDocument7 pages1 SMPiaggio PIAGGIONo ratings yet
- Femto-Lasik laser eye surgery explainedDocument4 pagesFemto-Lasik laser eye surgery explainedvrlftrNo ratings yet
- Full download book Connectomic Deep Brain Stimulation Pdf pdfDocument41 pagesFull download book Connectomic Deep Brain Stimulation Pdf pdfgeorge.redfield696100% (12)
- Executive Rule For CME - PD - SCFHSDocument14 pagesExecutive Rule For CME - PD - SCFHSsevattapillaiNo ratings yet
- Tata Memorial Centre Final Add V 020513Document6 pagesTata Memorial Centre Final Add V 020513Rupal SojitraNo ratings yet
- Diagnosis-Pedrosa, Joan ADocument27 pagesDiagnosis-Pedrosa, Joan AJoan Alde PedrosaNo ratings yet
- Blueprint of Hospital 20Document25 pagesBlueprint of Hospital 20Muralis MuralisNo ratings yet
- The Long and Short of The Issue of Counsellors - The Star OnlineDocument2 pagesThe Long and Short of The Issue of Counsellors - The Star OnlinefareedhashimNo ratings yet
- Stree Roga Vigyan-Mallikarjuna With MCQs PDFDocument20 pagesStree Roga Vigyan-Mallikarjuna With MCQs PDFCHAUKHAMBHA PRAKASHAKNo ratings yet
- Understanding the Basic Mechanisms of PathophysiologyDocument59 pagesUnderstanding the Basic Mechanisms of PathophysiologyAldous FajardoNo ratings yet
- Female SterilizationDocument40 pagesFemale SterilizationdrrajeshgoudNo ratings yet
- DulcolaxDocument1 pageDulcolaxKatie McPeekNo ratings yet
- Clinical Approach To Isolated Splenomegaly: M M, P M, R KDocument5 pagesClinical Approach To Isolated Splenomegaly: M M, P M, R KlilisNo ratings yet
- Helicure - Google SearchDocument1 pageHelicure - Google Searchalijan deparNo ratings yet
- Patient Medication SheetDocument1 pagePatient Medication SheetYang YangNo ratings yet
- Peptic Ulcer Dse PathophysiologyDocument19 pagesPeptic Ulcer Dse PathophysiologySymone Jay Lapiz100% (1)
- Drug Name Brand Name Classification Dosage Indications Side/ Adverse Effects Nursing ResponsibilitiesDocument2 pagesDrug Name Brand Name Classification Dosage Indications Side/ Adverse Effects Nursing ResponsibilitiesRonald BurkeNo ratings yet
- History TakingDocument55 pagesHistory TakingDeepika MahajanNo ratings yet
- EBM TerapiDocument23 pagesEBM TerapidyahayulestariNo ratings yet
- Endopore Insert eDocument20 pagesEndopore Insert eMery MerryNo ratings yet
- Jurnal AnestesiDocument5 pagesJurnal AnestesiridwanNo ratings yet
- Drug Study On Certain DrugsDocument10 pagesDrug Study On Certain DrugsMelvin D. RamosNo ratings yet
- Expert in BGM & PoCT TechnologiesDocument16 pagesExpert in BGM & PoCT TechnologiesMalik AlnabhaniNo ratings yet
- 1 +Theresia+Jamini+1-9Document9 pages1 +Theresia+Jamini+1-9Florentina yohana ngeluNo ratings yet
- Breathing Control: Pistol@tenrings - Co.ukDocument1 pageBreathing Control: Pistol@tenrings - Co.ukmanfromgladNo ratings yet