Professional Documents
Culture Documents
Initial Care of Newborn & Newborn Screening Group 5 (Joy Marie Pillado's Conflicted Copy 2013-06-25)
Uploaded by
Doc Prince Caballero0 ratings0% found this document useful (0 votes)
9 views4 pagesNew
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentNew
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views4 pagesInitial Care of Newborn & Newborn Screening Group 5 (Joy Marie Pillado's Conflicted Copy 2013-06-25)
Uploaded by
Doc Prince CaballeroNew
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
Initial Care of Newborn Other persons needed to prepare medication doses and record
Dr. E. Posecion interventions and times
June 18, 2013
Group 5 Equipment
Equipment and supplies must be available at every delivery
Perinatologist – keeps the baby healthy inside All delivery settings should have equipment for O2 administration,
Neonatologist – concerns with high risk pregnancy bag and mask ventilation and ET intubation
CS delivery rooms should be stocked with supplies for vascular
Successful Approach to Neonatal Resuscitation access, volume expanders and medications as well as respiratory
Anticipation equipment
- Personnel Low risk labor-delivery-recovery rooms may be served by ER charts
- Equipment Correct size respiratory equipment should be unpacked, prepared
Recognition and tested
Techniques in resuscitation Responsibility for restocking of supplies and routine maintenance
of equipment must be clearly designated
Risk Factors Associated with the Need for Resuscitation
Maternal Recognition
PROM – high risk for infection Three key steps
Bleeding in 2nd or 3rd trimester – hypotensive mother, no blood o Evaluate infant
supply for the baby o Decide on the correct action
Severe PIH – blood vessels are narrowed o Take that action
- Premature baby Three basic signs forms basis for evaluation
Chronic HPN o Respirations
Previous fetal or neonatal death o Heart rate
Pharmacologic Therapy o Color
Chronic illness Techniques in resuscitation
Maternal infection A - Establish an Airway
Heavy Sedation Positioning
No prenatal care Suctioning
Substance abuse B - Initiate Breathing
Diabetes Mellitus Tactile stimulation
Positive-pressure ventilation
Fetal C - Maintain Circulation
Multiple gestation – 2nd baby is preterm Chest compressions
Preterm gestation (<35 wks) and Post-term gestation (>42wks) Medications and volume expanders
Size-date discrepancy
Congenital abnormalities
Physical Examination of the Newborn
Rh isoimmunisation/hydrops fetalis
Polyhydramnios and oligohydramnios
Thorough physical examination is essential within the first 24 hours
Reduced fetal movement before onset of labor
of life to identify problems and institute early intervention
Intrauterine infection
Any major abnormalities should be discussed with the parents as
IUGR
soon as feasible
Normal newborn should also be examined by the physician within
Intrapartum
24 hours before discharge
Fetal distress
High risk infants should be assessed immediately by the nursing
Prolapsed cord
staff and the physician
Prolonged labor
Precipitous labor Vital Signs
Forceps delivery Nursing personnel should measure the following within the 1st hour
CS delivery of life
Narcotic administration to mother within 4 hours of delivery o Temperature
Abnormal presentation o Respiratory rate
Prolonged rupture of membranes o Heart rate
Antepartum haemorrhage
Thick meconium staining Gestational Age Assessment
Nonreassuring FHR patterns Physicians perform gestational age assessment as part of their
Vacuum-assisted delivery evaluation
Compare with maternal estimated date of confinement (by UTZ
Successful Approach to Neonatal Resuscitation and LMP)
Personnel
There should be one person solely responsible for the baby who is Body Measurements
capable of initiating resuscitation Nursing staff should record the infant’s
A second person with complementary skills should be available o Weight (in Kg)
o Length (in cm) - Congenital hypothyroidism
o Head circumference (in cm) - Congenital adrenal hyperplasia
These should be plotted on the growth chart - Galactosemia
This facilitates identification of infants who are small or large for - G6PD deficiency
gestational age, or microcephalic or macrocephalic
Management of the High Risk Infant During Transition
Routine Evaluation During Transition
Respiratory Areas
o Is there any evidence of increasing respiratory distress? Monitoring
o Is there tachypnea without grunting? o Cardiorespiratory monitor
o Is the infant pink and well saturated? o Blood pressure readings
o Mild grunting during the first few minutes of life is normal o Arterial pressure if with arterial catheter
o Increasing grunting at 15 to 30 min of age and associated with o Pulse oximeter
other signs of respiratory distress is abnormal (pneumonia, Vascular access
RDS, pneumothorax) Oxygen and ventilator support
o Tachypnea with grunting – TTN Evaluation of suspected sepsis
o All infants with any signs of respiratory distress should be
placed on a pulse oximeter to assess O2 saturation
Cardiovascular NEWBORN SCREENING
o Is the infant well perfused? What is the Newborn Screening Test?
o Does the infant have a murmur? Has been an important part of routing newborn care in
o Hypoperfusion often accompanies either sepsis or significant developed countries
asphyxia Introduced in the Philippines in 1996
o Murmurs maybe present in healthy newborns but in the A series of tests used to detect a group of silent disease
presence of cyanosis, poor perfusion or pulses, consider the present at birth which if undetected late could lead to
presence of cardiac disease development delay or death
Neurologic Newborn Screening
o Is the infant lethargic and hypotonic or is the infant jittery? A public health program for the early identification of disorders
o Lethargy and hypotonia are associated with both sepsis and that can lead to mental retardation or death
asphyxia An integral part of routine newborn care in most developed
o Jitteriness may indicate early drug withdrawal or countries
hypoglycaemia As routine as Vit K injection or cord care
o Coarse high-amplitude jitteriness is sometimes seen in infants In the Philippines, it is recognized as part of the standard newborn
with hypoxic-ischemic encephalopathy care
Temperature
o Temperature must be followed closely in preterm infants Why is it important?
o Because of a larger surface to volume ratio, they are more Babies with these metabolic disorders look normal at birth
likely to quickly become hypothermic One will never know that the baby has the disorder until the onset
Laboratory evaluation of signs and symptoms which may already be irreversible such as
o Blood glucose mental retardation and death.
- Prematurity
- Respiratory distress Newborn screening is ideally done on the 48th hour or at least 24
- Suspected sepsis hours from birth.
- Hypovolemia/hypotension Sick and premature babies must be screened by the 7th day of life
- Maternal diabetes – administered insulin passes to the regardless of weight and age of gestation.
placenta
- Baby is hypoglycaemic which leads to poor Landmarks in the History of Newborn Screening
mental performance 1961 Birth of Newborn Screening in US
- LGA/SGA 1996 24 MM Hospitals in the Philippines form the NBS Study Group
- Asphyxia 1999 DOH adopts NBS as a program
- Jitteriness/lethargy 2000 DOH AO No 1 s2000; creation of NTWG – NBS
- Hyperviscosity syndrome 2003 NBS Bill filed in congress and senate
o Hemoglobin/hematocrit 2004 Newborn Screening Act of 2004
- Prematurity 2008 1753 Newborn Facilities (NSF) in the Philippines
- Discordant twins
- Plethora or hyperviscosity What disorders are tested in newborn screening?
- Hypovolemia/hypotension 1. Congenital Hypothyroidism (CH)
- Fetal or neonatal blood loss 2. Congenital Adrenal Hyperplasia (CAH)
- LGA/SGA 3. Phenylketonuria (PKU)
- Maternal diabetes 4. Galactosemia (GAL)
- Pathologic jaundice 5. Glucose 6 Phosphate Dehydrogenase Deficiency (G6PD Def.)
- Maternal bleeding 6. Maple Syrup Urine Disease (Branched Chain Ketoaciduria)
- Suspected sepsis
o Newborn Screening Why are these disorders included in the NBS panel?
- PKU 1. Local prevalence
2. Reversible if treated on time Spastic hypertonic cerebral palsy in 30%
3. Treatment is available Seizures in 20%
EEG abnormalities in 80%
Light colored hair
Eczematoid rash/intractable itching
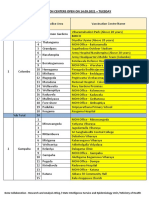
Disorders Confirmed Prevalence Laboratory diagnosis
CH 378 1:3,548 Bacterial inhibition assay using Bacillus subtilils – no bacterial
CAH 171 1:7,842 growth means lack of phenylalanine so the baby is positive for
GAL 15 1:89,401 PKU
PKU 10 1:134,102 Treatment
G6PD DEF. 23,557 1:54 dietary restriction of phenylalanine
frequent measurement of phenylalanine plasma levels
Total number of screened as of December 2008 special formula for PKU patients
4 tests 1,341,017 Prognosis
G6PD 1,264,122 Mental deficiency is prevented if treatment is started before 2
months of life.
Benefits of Newborn Screening
Detection of silent metabolic conditions as early as the first CONGENITAL HYPOTHYROIDISM
week of life Causes
Prevention of neonatal or infant death (i.e. CAH) Thyroid dysgenesis (most common)
Facilitates accurate diagnosis when symptoms are nonspecific Thyroid dyshormogenesis
or non-existent Hypothalamic/pituitary dysfunction
Makes effective management of metabolic disorders feasible Maternal antithyroid drug ingestion
Sample collection is simple, safe, inexpensive and reliable Maternal autoimmune disorders
Gives affected infants a chance at a normal life Immaturity
Clinical Manifestations
GALACTOSEMIA < 5% are symptomatic in the newborn period
Deficiency of galactose-1-phosphate uridyl transferase Most will manifest by 4th month of life
This enzyme catalyzes the formation of uridin diphosphate Clinical Manifestations in Newborn Period
(UDP)-galactose to glucose-1-phosphate Prolonged jaundice
Results in increased galactose-1-phosphate and galactitiol in Constipation
the liver, brain, kidney and eyes Lethargy
Autosomal recessive Poor feeding
Clinical Manifestations Hypothermia
Failure to thrive – baby is hungry all the time that’s why he Described as “good babies”
stops from growing Usually quiet
Hepatomegaly – no detoxification Seldom cries when wet
Jaundice Loses one IQ point everyday
Cataracts – glucose is found in lenses of the eyes Long term undetected congenital hypothyroidism leads to CRETINISM:
Mental retardation Developmental delay
Renal failure (Fanconi syndrome) Hollow empty eyes which appear far apart
Laboratory Diagnosis Swollen eyelids
Enzyme assay in RBC, cord blood, fibroblasts Narrow palpebral fissures
Treatment Narrow/depressed nasal bridge
Exclusion of galactose from the diet Laboratory Diagnosis
Use casein hydrolysates and soy milk substitutes (vegetable- Determination of TSH by immunofluorescence
based milk) Anemia
Prognosis Increase indirect bilirubin
Good with strict dietary control Delayed bone age
Cataracts are reversible if treatment is started within 5 Decreased T4, increase TSH
months of life Thyroid scan
Hepatic and renal manifestations are reversible Radioactive Iodine Uptake
Treatment
PHENYLKETONURIA L-thyroxine
Deficiency of phenylalanine hydroxylase which catalyzes the Early detection and treatment are crucial!
conversion of phenylalanine to tyrosine (for skin color and
neurotransmitters) GLUCOSE 6 PHOSPHATE DEHYDROGENASE DEFICIENCY
Increased phenylalanine and degradation products in tissues Deficiency of Glucose-6-phosphate dehydrogenase
Autosomal recessive Most common among Filipinos
Mild signs and symptoms
Clinical Manifestations X-linked – only males are affected
Mental retardation: 99% of untreated Pathophysiology
Failure to thrive Glucose is responsible for the production of glutathione which
Light skin fights free radicals
Musty smelling Severe hemolysis after exposure to:
Antimalarials (quinine/primaquine) MAPLE SYRUP URINE DISEASE (Branched Chain Ketoaciduria)
Infections Inability to breakdown branched chain amino acids (leucine,
Acidosis isoleucine, valine)
Sulfonamines Deficiency of a multienzyme complex called branched chain
Nitrofurans ketoacid carboxylase
Antipyretic/analgesics ASA Results in accumulation of branched chain amino acid in
Sulfones plasma, urine, and CSF
Others (vit K, PAS, naphthalene balls, phenylhydrasine, Leucine and 2-oxoisocaproic acid are the most toxic to the
chloramphenicol) brain
Clinical Manifestations Autosomal recessive
Jaundice Several molecular phenotypes
Anemia
Hemolysis can happen in all age groups Classic MUSD
Treatment 0-2% activity
PRBC transfusion Overwhelming illness in the first few days of life
Avoidance of triggering factors Lethargy - coma – seizures
Sweet odor resembling burnt sugar detected in urine,
CONGENITAL ADRENAL HYPERPLASIA sweat, hair, and cerumen
Family autosomal recessive disorders of cortisol biosynthesis Hypoglycemia
Cortisol deficiency increases ACTH producing adrenocortical Intermittent
hyperplasia and overproduction of intermediate metabolites Milder manifestations
Signs and symptoms depend on the enzymatic step that is Patients become very sick when stressed
deficient Intermediate
Milder manifestations
Signs and Symptoms 15-25% activity of enzymes
No weight gain Thiamine Responsive
Irritability Similar manifestations as intermediate type
Vomiting Biochemical abnormality corrected with intake of high dose of
Acute shock thiamine
Ambiguous genitalia in females E-3 Variant
Masculinization in males Lactic acidosis
Hypoglycemia Similar symptomatology to classic MSUD
Decreased Na, increased K More rapid CNS depression
Treatment Diagnosis
Cortisone Plasma amino acid analysis (increased branched chain amino
Salt replacement acid)
Types of Congenital Adrenal Hyperplasia (CAH) Urine organic analysis; increased ketoacids
1. 21 Hydroxylase Deficiency Branched chain ketoacid decarboxylase enzyme activity
Most common (>90% of cases) determination in fibroblasts, leukocytes or amniotic fluid cells
75% are salt losing form (definitive diagnosis)
Decreased aldosterone Presumptive diagnosis: urine + 2,4 dinitrophenylhydrazine
Decreased cortisol (DNPH) – yellow precipitate
Increased androgens (virilization)
Develops at 2 weeks of age
Death occurs in days or weeks if without treatment
Vomiting – metabolic acidosis
Acute shock
Manifests sepsis-like symptoms
Large genitals in males and ambiguous genitalia in
females due to high production of testosterone
Treatment
Glucocorticoid replacement
Mineralocorticoid for salt wasting form
Surgical management of ambiguous genitalia
2. 11 β Hydroxylase Deficiency
5-8% of cases
Normal aldosterone
Increased corticotropin
Increased androgens (virilization)
Hypernatremia
Treatment
+/- mineralocorticoids
Glucocorticoid for hypertension
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Adult History Taking and Physical ExaminationDocument6 pagesAdult History Taking and Physical ExaminationDoc Prince Caballero100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Nursing Practice Skills: Adult Intensive Care Unit PatientsDocument10 pagesNursing Practice Skills: Adult Intensive Care Unit PatientsMona Doria67% (3)
- Natural History of DiseaseDocument9 pagesNatural History of DiseaseAan Sucitra Hollan Fm'sNo ratings yet
- Children and Death: Dr. Chua 07/25/2013 Group 6 - Witwew!Document6 pagesChildren and Death: Dr. Chua 07/25/2013 Group 6 - Witwew!Doc Prince CaballeroNo ratings yet
- Is Schizophrenia Really Demonic PossessionDocument5 pagesIs Schizophrenia Really Demonic PossessionUproottNo ratings yet
- Grief, Mourning and BereavementDocument5 pagesGrief, Mourning and BereavementDoc Prince Caballero100% (1)
- San Antonio Elem. School: Contingency Plan ON Covid - 19Document12 pagesSan Antonio Elem. School: Contingency Plan ON Covid - 19Loraine Anna100% (2)
- Antepartum Fetal MonitoringDocument9 pagesAntepartum Fetal MonitoringDoc Prince CaballeroNo ratings yet
- Talk It Out Before You Say I DoDocument6 pagesTalk It Out Before You Say I DoDoc Prince CaballeroNo ratings yet
- Panunumpa NG Propesyonal PDFDocument2 pagesPanunumpa NG Propesyonal PDFAngelo Bonje100% (1)
- CPR With AedDocument37 pagesCPR With AedDoc Prince CaballeroNo ratings yet
- New Guidelines in Attendance Tracker SubmissionDocument1 pageNew Guidelines in Attendance Tracker SubmissionDoc Prince CaballeroNo ratings yet
- Bone Growth and Growth Pattern in ChildhoodDocument6 pagesBone Growth and Growth Pattern in ChildhoodDoc Prince CaballeroNo ratings yet
- The Midlife: Henrietta V. Cabado-Española, MD, FPPADocument7 pagesThe Midlife: Henrietta V. Cabado-Española, MD, FPPADoc Prince CaballeroNo ratings yet
- GI Disorders During Newborn PeriodDocument5 pagesGI Disorders During Newborn PeriodDoc Prince CaballeroNo ratings yet
- Medical Problems in AdolescentsDocument3 pagesMedical Problems in AdolescentsDoc Prince CaballeroNo ratings yet
- Principles of ImmunizationDocument4 pagesPrinciples of ImmunizationDoc Prince CaballeroNo ratings yet
- The Midlife: Henrietta V. Cabado-Española, MD, FPPADocument7 pagesThe Midlife: Henrietta V. Cabado-Española, MD, FPPADoc Prince CaballeroNo ratings yet
- GI Disorders During Newborn PeriodDocument5 pagesGI Disorders During Newborn PeriodDoc Prince CaballeroNo ratings yet
- NEONATAL RESUSCITATION GUIDELINESDocument5 pagesNEONATAL RESUSCITATION GUIDELINESDoc Prince CaballeroNo ratings yet
- Ballard Scoring: Component Description How To IllicitDocument4 pagesBallard Scoring: Component Description How To IllicitDoc Prince CaballeroNo ratings yet
- Current Status of The Filipino YouthDocument10 pagesCurrent Status of The Filipino YouthDoc Prince CaballeroNo ratings yet
- Early and Middle AdulthoodDocument6 pagesEarly and Middle AdulthoodDoc Prince CaballeroNo ratings yet
- Current Status of The Filipino YouthDocument10 pagesCurrent Status of The Filipino YouthDoc Prince CaballeroNo ratings yet
- Initial Care of Newborn & Newborn Screening Group 5 (Joy Marie Pillado's Conflicted Copy 2013-06-25)Document4 pagesInitial Care of Newborn & Newborn Screening Group 5 (Joy Marie Pillado's Conflicted Copy 2013-06-25)Doc Prince CaballeroNo ratings yet
- Surgical Problems in NewbornsDocument7 pagesSurgical Problems in NewbornsDoc Prince CaballeroNo ratings yet
- Breastfeeding BenefitsDocument4 pagesBreastfeeding BenefitsDoc Prince CaballeroNo ratings yet
- Aural Toilet Guideline1Document2 pagesAural Toilet Guideline1Ariska Peradilla100% (1)
- Systemic Response To InjuryDocument4 pagesSystemic Response To InjuryDoc Prince CaballeroNo ratings yet
- MenopauseDocument9 pagesMenopauseDoc Prince CaballeroNo ratings yet
- OB Tickler 1 PDFDocument22 pagesOB Tickler 1 PDFAnonymous de6SlW1No ratings yet
- Neonatal JaundiceDocument6 pagesNeonatal JaundiceDoc Prince CaballeroNo ratings yet
- Early Onset SchizophreniaDocument3 pagesEarly Onset SchizophreniaDoc Prince CaballeroNo ratings yet
- Pharmacology '' Routes of Administration #Local RouteDocument13 pagesPharmacology '' Routes of Administration #Local RouteNitin NawaleNo ratings yet
- Ethical Issues in NeonateDocument11 pagesEthical Issues in Neonatethilaga880% (1)
- The Key Role of The Dental Practitioner in Early Diagnosis of Periodontal Ehlers Danlos Syndromes A Rare Case Report of SiblingsDocument9 pagesThe Key Role of The Dental Practitioner in Early Diagnosis of Periodontal Ehlers Danlos Syndromes A Rare Case Report of SiblingsnadhiracindyNo ratings yet
- JT 4412/11 AUG/SIN-DPS Flight PlanDocument62 pagesJT 4412/11 AUG/SIN-DPS Flight PlanWahdhan HadiNo ratings yet
- Serious Fungal Infections in The Philippines: Original ArticleDocument5 pagesSerious Fungal Infections in The Philippines: Original ArticleAilen LagulaNo ratings yet
- Lumpy Skin DiseaseDocument99 pagesLumpy Skin DiseaseDaoud IssaNo ratings yet
- Cap 2019 04 01 PDFDocument58 pagesCap 2019 04 01 PDFRajeev PareekNo ratings yet
- DFM, Colombo, ProspectusDocument16 pagesDFM, Colombo, ProspectusMatin Ahmad Khan100% (1)
- Chest Tube InsertionDocument3 pagesChest Tube InsertionprofarmahNo ratings yet
- Hyperacusis: Major Research Questions: Background Epidemiology and Natural HistoryDocument6 pagesHyperacusis: Major Research Questions: Background Epidemiology and Natural HistoryFuninganaNo ratings yet
- Mount Carmel Medication Management Pocket GuideDocument2 pagesMount Carmel Medication Management Pocket GuideWOSU100% (1)
- NCM 112 - Rle Nursing Care Plan: To Have Baseline Data. Normal Values Indicate Adequate Tissue PerfusionDocument7 pagesNCM 112 - Rle Nursing Care Plan: To Have Baseline Data. Normal Values Indicate Adequate Tissue Perfusiontherese BNo ratings yet
- Involution and LochiaDocument2 pagesInvolution and Lochiaapi-316491996100% (1)
- Copptech: Successful Tests Against Sars-Cov-2Document2 pagesCopptech: Successful Tests Against Sars-Cov-2enologiacomNo ratings yet
- Cadi PDFDocument66 pagesCadi PDFpradeepsj ReddyNo ratings yet
- Sir ModelDocument5 pagesSir ModelJaehun JeongNo ratings yet
- Getting To The Roots of Failure: The Left May Be Down, But It Is Certainly Not Out. How May It Renew Itself?Document2 pagesGetting To The Roots of Failure: The Left May Be Down, But It Is Certainly Not Out. How May It Renew Itself?Priyank BhatiaNo ratings yet
- Terapi ToxoplasmosisDocument9 pagesTerapi Toxoplasmosissarah disaNo ratings yet
- Vaccination Centers On 14.09.2021Document8 pagesVaccination Centers On 14.09.2021Chanu On CTNo ratings yet
- Treatment Outcome and Factors Affecting Time To Recovery in Children With Severe Acute Malnutrition Treated at Outpatient Therapeutic Care ProgramDocument11 pagesTreatment Outcome and Factors Affecting Time To Recovery in Children With Severe Acute Malnutrition Treated at Outpatient Therapeutic Care ProgramMelkamuMeridNo ratings yet
- CFR - Code of Federal Regulations Title 21Document2 pagesCFR - Code of Federal Regulations Title 21Faradina Astari MunandarNo ratings yet
- Covid Vaccine Status Class MasandiganDocument4 pagesCovid Vaccine Status Class MasandiganServus DeiNo ratings yet
- Ceftriaxone Compared With Sodium Penicillin G For Treatment of Severe LeptospirosisDocument9 pagesCeftriaxone Compared With Sodium Penicillin G For Treatment of Severe LeptospirosisFifi SumarwatiNo ratings yet
- NURS FPX 6414 Assessment 3 Tool Kit for BioinformaticsDocument5 pagesNURS FPX 6414 Assessment 3 Tool Kit for BioinformaticsCarolyn HarkerNo ratings yet
- Evidence Based PostpartumDocument75 pagesEvidence Based PostpartumAnnisatus SholehahNo ratings yet
- C1 Editable Quiz 3 - 0Document3 pagesC1 Editable Quiz 3 - 0Hiền Vũ Thị MaiNo ratings yet