Professional Documents
Culture Documents
0 Psychiatry Notes PDF
0 Psychiatry Notes PDF
Uploaded by
Coy Nuñez0 ratings0% found this document useful (0 votes)
21 views6 pagesOriginal Title
0 Psychiatry Notes.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
21 views6 pages0 Psychiatry Notes PDF
0 Psychiatry Notes PDF
Uploaded by
Coy NuñezCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 6
ea
LESSON 1: DOCTOR — PATIENT RELATIONSHIP
Listening : the key skill in Psychiatry
© Key Listening Skills
© Hearing ~Connotative meaning of words, Idiosyncratic uses of language, Figures of
Speech that tells a deeper story, voices, tones, modulation, stream of association
Seeing — Posture, Gestures, Facial Expression
Comparing ~ Noting what is omitted, Dissonances between modes of expression
Intuiting — Attending to one’s own internal reactions
Reflecting — Thinking it all through outside the immediate pressure to respond during,
the interview
+ Blocks to Effective Listening
© Patient-Psychiatrist Dissimilarities: Race, Sex, Culture, Religion, Regional dialect,
Individual differences, Socioeconomic class
© Superficial similarities : May lead to incorrect assumptions of shared meanings
© Countertransference: Psychiatrist fails to hear or reacts inappropriately to content
reminiscent of own unresolved conflicts
© External Forces : managed care settings, Emergency Department, Control oriented
inpatient unit
© Attitudes : Need for control, Psychiatrist having a bad day
‘+ Attitudes Important to Listening
(©The centrality of inner experience
‘There are no bad historians
‘The answer is always inside the patient
Control and power are shared in the interview
It is OK to feel confuse and uncertain
Objective truth is never simple as it seems
Listening to yourself too
Everything you hear is modified by the patient's filter
Everything you hear is modified by your own filters
‘There will always be another opportunity to hear more clearly
e000
000000000
Roles and Motivations
‘* The physician- patient relationship includes specific roles and motivations.
‘+ These form the core ingredients of the healing process
‘+ Ingeneric form the physician- patient relationship is defined as coming together of an expert
and a help seeker to identify and understand, solve the problems of the help seeker.
‘+The help seeker is motivated by the desire and hope for assistance and relief from pain
‘A physician is required to have a genuine interest in people and a desire to help
The relationship between the physician and the patient is essential to the healing of many
patients , itis critical to the therapeutic outcome
Formation of the Physician-Patient Relationship
Assessment and evaluation
Rapport
Therapeutic working alliance
Transference and countertransference
Defense Mechanism
Mental status of the Patient
ASSESSMENT AND EVALUATION
The physician and patient relationship develops during the assessment and evaluation of the
patient,
The patient observes the thoroughness and sensitivity with which the physician collects
information, performs the physical exams and explain the needed tests. At each step, the
physician's clarification of the treatment goals and interventions either builds up the patient’s
expectation of help and feelings of safety or creates increasing distress and disease for the
patient.
‘Alertness to the patient's fears and misunderstanding of the evaluation process can minimize
unnecessary disruptions of the relationship and provide information on the patent's previous
‘experiences with medical care and important authority figures.
RAPPORT
The psychiatri
offering help.
The way of relating between the physician and the patient, the physician-patient relationship
has begun.
‘The physician ability to empathize, to understand in feelings terms every patient's subjective
experience.
initiates the “contract” of the relationship by acknowledging the pain and
THERAPEUTIC OR WORKING ALLIANCE
For a patient to trust and work closely with a physician, itis essential that there be a reality
based relationship.
The experienced physician makes communication across the gap seem effortless, using a
different “language” for each patient.
The therapeutic alliance is extremely important in times of crisis such as suicidality,
hospitalization, and aggressive behaviour.
The therapeutic working alliance must endure in spite of what may, at times be intense,
irrational, delusional, characterologic, or transference based feelings of love and hate.
It must provide a stable base for the patient and physician when the patient's feelings or
behaviors may impair reflection and cooperation.
The alliance requires a basic trust by the patient that the physician is working in his or her best
interests.
‘The development of common goals fosters the physician and patient seeing themselves as
having a reciprocal responsibilities
TRANSFERENCE AND COUNTERTRANSFERENCE
Transference is the tendency we all have to see someone in the present as being like an
important figure from our past
This process occurs outside our conscious awareness
Transference influences the patients’ behaviour and can distort the physician-patient
relationship for good or ill
The transference can be the elaboration of an accurate observation into the “total” explanation
or the major evidence of some expected harm or loss
Often the physician may recognize the transference by the pressure she or he feels to respond
in a particular manner to the patient.
Transference is ubiquitous
Countertransference is the physician’s transference to the patient:
Two types of Countertransterence:
© Concordant Countertransference
= The physician experiences and empathizes with the patients’ emotional
experience and perception of reality.
© Complementary Countertransference
‘The physician experiences and empathizes with the emotional experience and
perception of reality of an important person from the patients’ life
DEFENSE MECHANISM
Defense mechanisms are specific cognitive process: ways of thinking that the mind employs to
avoid painful feelings
Defense mechanism may be more or less mature depending on the degree of distortion of
reality and interpersonal disruption they lead to.
The patient’s characteristic defense mechanisms, the cognitive process or coping skills used to
lower anxiety and unpleasant feelings, can greatly affect the physician-patient relationship.
Defense mechanism operates all the time in times of high anxiety or during a life crisis.
Healthier Defense Mechanism
© Sublim
© Humor
© Repression
© Displacement
© Intellectualization
© Reaction formation
°
°
°
o
Reversal
Identification with the aggressor
Asceticism
Altruism
© Isolation of affect
More primitive Defense Mechanism
© Splitting
© Projection
Projective identification
Omnipotence
Devaluing
Primitive idealization
Denial
Conversion
Avoidance
ec 00cc00
MENTAL STATUS OF THE PATIENT
‘+The patient's mental status is a major determinant of the formation and nature of the
relationship with the physician.
‘* The ability to work with an empathic listener while confronting limitations and feelings of shame
and embarrassment is a special opportunity of a well formed patient-doctor relationship.
PHASES OF TREATMENT
‘©The treatment phase:
© Early : involves developing rapport, forming shared initial goals, and initiating working,
alliance.
* Education of the patient is important to the success of the doctor patient
relationship, so that patient can learn what he or she can expect
© Middle: the physician and patient continuously refine their shared goals, and various
interventions are tried
Transference and countertransference are likely to emerge
"How these are recognized and managed is critical to whether the relationship
continues and is therapeutic
(© Late : the assessment of the outcome and plans for the future are the primary focus
The physician and the patient discuss the end of their relationship in a process
known as termination.
= Success and disappointments associated with the treatment are reviewed.
+ The therapeutic alliance is strengthened in this stage when the physician
accepts expressions of the patient's disappointments, encourages such
expressions when they are not forthcoming, and prepares the patient for the
future.
© Factors affecting the Physician-Patient relationship:
© Phases of treatment: Early, Middle, Late
© Treatment setting
© Transition between inpatient and outpatient treatment
© Managed care
© Health and illness of the physician
LESSON 2: PROFESSIONAL ETHICS AND BOUNDARIES
+ Medical professionalism : is demonstrated by what physicians do with patients and within their
communities.
© These physician behaviors include responding to and advocating for the needs of
patients of patients, promoting the welfare of public health and honourably
representing the profession
© The values that have been associated with the profession of medicine include: service,
altruism, duty, advocacy, respect, honesty, integrity, excellence and accountability.
© Questions to guide clinical decision making:
© BENEFICENCE : what is goad for the patient
© NONMALEFICENCE: would this cause harm to this patient
© AUTONOMY: what does this patient want
© JUSTICE: Is this fair
‘SUMMARY OF THE WPA GUIDELINES REGARDING THE ROLE OF THE PSYCHIATRIST ON SPECIFIC ETHICAL
Issues:
‘* EUTAHNASIA : use caution regarding actions that could lead to the death of those with mental
illness
© TORTURE: should not take part in any mental or physical torture
* DEATH PENALTY: should not participate in executions or assess competency of those to be
executed
‘+ SELECTION OF SEX: should not participate in decisions to abort for the purpose of sex selection
‘+ ORGAN TRANSPLANTATION: helps patients exercise self determination in organ transplantation,
and avoid use of psychotherapeutic skills to influence the decision
‘+ ADDRESSING MEDIA: advocate for those with mental disorders, represent psychiatry with
dignity, do not discuss presumed diagnoses of individuals, and be aware of the effect of
discussions about mental illness on the public
* DISCRIMINATION: never be involved on ethnic cleansing
* GENETIC RESEARCH AND COUNSELLING: understand the impact of genetic information on
patients, obtain informed consent, ensure confidentiality and protect data against misuse
+ ETHICS OF PSYCHOTHERAPY IN MEDICINE: be trained in techniques, use therapy as part of
clinical treatment, be aware of need for informed consent, confidentiality and boundaries
‘© CONFLICT OF INTEREST WITH INDUSTRY: guard against gifts that influence clinical work and
research trials
‘© CONFLICTS WITH THIRD PARTY PLAYERS: advocate for patients and oppose discriminatory
practices towards mentally il
* VIOLATING BOUNDARIES AND TRUST: no sexual relationship with patients
‘+ PROTECTION OF RIGHTS OF PSYCHIATRISTS: protect, treat and advocate for the mentally ill
without undue pressure from systems and without undue pressure from systems and without
discrimination toward the practice of psychiatry
‘DISCLOSING THE DIAGNOSIS OF DEMENTIA: be sensitive to the patient's rights to know and the
role of family in the disease process
DUAL RESPONSIBILITIES: must disclose to patient the absence of a therapeutic doctor-patient
relationship at initial assessment
WORKING WITH PATIENTS AND CAREGIVERS: awareness of the value of collaborating with
patients and caregivers in legislation, policy and clinical practice.
GUIDELINES FOR PROFESSIONAL BEHAVIORS IN CLINICAL PRACTICE
Be alert to warning signs in the doctor-patient relationship that trigger self reflection. Ifa
behaviour doesn’t feel right, it’s probably not, when in doubt, don’t
Be aware of the nned for self monitoring and on going consultation during one’s professional
career. This can occur one-on-one with a trusted colleague or in a group setting with several
psychiatrists discussing their countertransference experiences and seeking input and direction
for troubling cases
Be sensitive to inner feelings and any behaviors that appear outside the norm when interacting
with certain patients, the so called “red flags”
Transfer care of patient's where there is a high potential for a boundary violation to another
physician, preferably not in the same practice
Consider use of an index of suspicion to identify risky behvaiors in professional conduct.
Never make the patient’s problems your own
Report unethical behaviors of colleagues to appropriate entities
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Berne and Levy Physiology Test BankDocument1 pageBerne and Levy Physiology Test BankCoy Nuñez0% (3)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 3 Renal Vascular Disease 3Document46 pages3 Renal Vascular Disease 3Coy NuñezNo ratings yet
- 2 Gram Negative Bacterial InfectionDocument89 pages2 Gram Negative Bacterial InfectionCoy NuñezNo ratings yet
- Group 16: University of The Visayas Gullas College of Medicine Banilad, Mandaue City, CebuDocument6 pagesGroup 16: University of The Visayas Gullas College of Medicine Banilad, Mandaue City, CebuCoy NuñezNo ratings yet
- 2 Renal Tubular, Interstitial Disease 2Document94 pages2 Renal Tubular, Interstitial Disease 2Coy NuñezNo ratings yet
- Benito K. Lim Hong III, M.DDocument55 pagesBenito K. Lim Hong III, M.DCoy NuñezNo ratings yet
- 1 Glomerular DiseasesDocument127 pages1 Glomerular DiseasesCoy NuñezNo ratings yet
- 1 Gram Positive Bacterial InfectionDocument87 pages1 Gram Positive Bacterial InfectionCoy NuñezNo ratings yet
- 4 Obstructive UropathyDocument37 pages4 Obstructive UropathyCoy NuñezNo ratings yet
- Patho Immune System PathologyDocument7 pagesPatho Immune System PathologyCoy Nuñez100% (1)
- 1 Introduction To General PathologyDocument91 pages1 Introduction To General PathologyCoy NuñezNo ratings yet
- Exercise 7 g6pd MedsDocument8 pagesExercise 7 g6pd MedsCoy NuñezNo ratings yet
- Sample Case: EndocrinologyDocument42 pagesSample Case: EndocrinologyCoy NuñezNo ratings yet
- What Will Do If You Find Money On The Sidewalk?Document10 pagesWhat Will Do If You Find Money On The Sidewalk?Coy NuñezNo ratings yet
- General Pathology - Group 9 I. Clinical Impression - ACNE II. PathophysiologyDocument1 pageGeneral Pathology - Group 9 I. Clinical Impression - ACNE II. PathophysiologyCoy NuñezNo ratings yet
- Inflammation: Benito K. Lim Hong III, M.DDocument70 pagesInflammation: Benito K. Lim Hong III, M.DCoy NuñezNo ratings yet
- Systemic Response To Injury & Metabolic Support: Josef S. Lim, MD, FPSGS, FPCS, PalesDocument132 pagesSystemic Response To Injury & Metabolic Support: Josef S. Lim, MD, FPSGS, FPCS, PalesCoy NuñezNo ratings yet
- Rate Limiting Step PDFDocument1 pageRate Limiting Step PDFCoy NuñezNo ratings yet
- Biochem Notes 1Document10 pagesBiochem Notes 1Coy NuñezNo ratings yet
- Page 55 (Growth, Survival, and Death of Microorganisms)Document4 pagesPage 55 (Growth, Survival, and Death of Microorganisms)Coy NuñezNo ratings yet
- Commensal AmoebaDocument2 pagesCommensal AmoebaCoy NuñezNo ratings yet
- Cooh Coo Coo NH NH NH: Function of Proteins: 2. Ionic Properties of AADocument6 pagesCooh Coo Coo NH NH NH: Function of Proteins: 2. Ionic Properties of AACoy NuñezNo ratings yet
- Pathogenesis and PathologyDocument3 pagesPathogenesis and PathologyCoy NuñezNo ratings yet
- Immunity of Parasitic InfectionsDocument4 pagesImmunity of Parasitic InfectionsCoy NuñezNo ratings yet
- Page 55 (Arrabis, Baylosis, Gudapati)Document4 pagesPage 55 (Arrabis, Baylosis, Gudapati)Coy NuñezNo ratings yet
- Cestodes NotesDocument20 pagesCestodes NotesCoy NuñezNo ratings yet
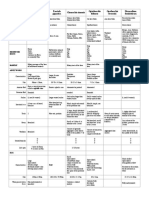
- Trematodes TableDocument3 pagesTrematodes TableCoy NuñezNo ratings yet
- 0.07 - 0.12 MM in Thickness But May Reach UpDocument8 pages0.07 - 0.12 MM in Thickness But May Reach UpCoy NuñezNo ratings yet