Professional Documents
Culture Documents
Sdo Wim QF Sgod SHN 000 Health Profile of Teaching Non Teaching Personnel
Uploaded by
Sally Angelcor0 ratings0% found this document useful (0 votes)
12 views2 pagesMEMO
Original Title
Sdo Wim Qf Sgod Shn 000 Health Profile of Teaching Non Teaching Personnel
Copyright
© © All Rights Reserved
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentMEMO
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views2 pagesSdo Wim QF Sgod SHN 000 Health Profile of Teaching Non Teaching Personnel
Uploaded by
Sally AngelcorMEMO
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 2
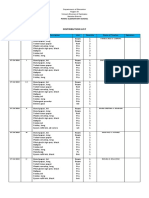
HEALTH PROFILE OF TEACHING & NON-TEACHING PERSONNEL
Date: April 12, 2019
Name: AMOR F. CABATAN Date of Birth: 09/05/1990 Age:29 Gender: M
School/District/Division: Porac Integrated School Civil Status: S
Position/Designation: _________________________________________ Years in Service: _________
Family History: (pls. check) Y N Specify Relationship
Hypertension [ ] [ ] ____________________________________________
Cardiovascular Disease [ ] [ ] ____________________________________________
Diabetes Mellitus [ ] [ ] ____________________________________________
Kidney Disease [ ] [ ] ____________________________________________
Cancer [ ] [ ] ____________________________________________
Asthma [ ] [ ] ____________________________________________
Allergy [ ] [ ] ____________________________________________
Other Remarks: _____________________________________________________________________________________
Past Medication History: (check) Y N Y N
Hypertension [ ] [ ] Tuberculosis [ ] [ ]
Asthma [ ] [ ] Surgical Operation (pls. specify) [ ] [ ]
Diabetes Mellitus [ ] [ ] Yellowish Discoloration of Skin/Sclera [ ] [ ]
Cardiovascular Disease [ ] [ ] Last Hospitalization (reason) [ ] [
]
Allergy (pls. specify) [ ] [ ] Others (pls. specify) [ ]
[ ]
Last Taken Date Result Date Result
CXR/Sputum Result _______ _______ Drug Testing _______ _________ Others: Specify ______
ECG _______ _______ Neuropsychiatric exam _______ _________
Urinalysis _______ _______ Blood Typing _______ _________
Social History:
Smoking Y ______ N _____ Age Started: _______ Stick/packs per day: _____ Pack per Year: _______
Alcohol Y ______ N _____ How Often: _______ Food Preference: ____________________
OB Gyn History (pls. encircle) (Female Teachers)
Menarche: ____________ Cycle: ____________ Duration: _____________
Parity F P A L
Papsmear done Y N if Yes, when: _____________
Self Breast Examination done Y N
Mass Noted: Y N Specify where: ______________
For Male personnel: Digital Rectal examination done: Y N Date Examined: _________________________
Result: ________________________________
Present Health Status (pls. check) Y N Y N
Cough 2 weeks 1 month longer Lumps [ ] [ ]
Dizziness [ ] [ ] Painful Urination [ ] [ ]
Dyspnea [ ] [ ] Poor/Loss of Hearing [ ] [ ]
Chest/Back pain [ ] [ ] Syncope/Fainting [ ] [ ]
Easy Fatigability [ ] [ ] Convulsions [ ] [ ]
Joint/Extremity pains [ ] [ ] Malaria [ ]
[ ]
Blurring of Vision [ ] [ ] Goiter [ ] [ ]
Wearing Eyeglasses [ ] [ ] Anemia [ ] [ ]
Vaginal Discharge/Bleeding [ ] [ ] Others (pls. specify) __________________________
Interviewed by: ______________________________
Date: ________________________________________
CONSULTATION AND TREATMENT RECORD
Treatment /
Date Chief Compliant Findings
Recommendation
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- Acr For MpreDocument1 pageAcr For MpreSally AngelcorNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Activity Completion ReportDocument1 pageActivity Completion ReportSally AngelcorNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Science Quiz QuestionsDocument3 pagesScience Quiz QuestionsSally AngelcorNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Form 138 Kto12 and RBEC 1 1Document13 pagesForm 138 Kto12 and RBEC 1 1Sally AngelcorNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Use Short (8.5 X 11 Board Paper)Document12 pagesUse Short (8.5 X 11 Board Paper)Sally AngelcorNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Daily Lesson Log School Grade Level Teacher Learning Area Teaching Dates and Time QuarterDocument2 pagesDaily Lesson Log School Grade Level Teacher Learning Area Teaching Dates and Time QuarterSally AngelcorNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Porac Elementary School Daily Accomplishment Report: Completed Started But Not Yet Completed Not DoneDocument1 pagePorac Elementary School Daily Accomplishment Report: Completed Started But Not Yet Completed Not DoneSally AngelcorNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Acr PrimalsDocument4 pagesAcr PrimalsSally Angelcor100% (4)
- Input Data Sheet For E-Class Record: Region Division School Name School IdDocument48 pagesInput Data Sheet For E-Class Record: Region Division School Name School IdSally AngelcorNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- Distribution List: Porac Elementary SchoolDocument8 pagesDistribution List: Porac Elementary SchoolSally AngelcorNo ratings yet
- Daily Lesson LOG: Addition of Integers Subtraction of Integers Multiplication of Integers Division of IntegersDocument5 pagesDaily Lesson LOG: Addition of Integers Subtraction of Integers Multiplication of Integers Division of IntegersSally Angelcor100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- First Quarter Examination 2018-2019Document1 pageFirst Quarter Examination 2018-2019Sally AngelcorNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Teacher II: Juan Dela CruzDocument2 pagesTeacher II: Juan Dela CruzSally AngelcorNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Consolidated Report of Quarter Exam in A.PDocument6 pagesConsolidated Report of Quarter Exam in A.PSally AngelcorNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Blood Urea Nitrogen (Bun)Document4 pagesBlood Urea Nitrogen (Bun)Vanessa VillanuevaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Bone Tumor - Dr. Andri R. Winoto, SpOT (K)Document19 pagesBone Tumor - Dr. Andri R. Winoto, SpOT (K)Aramanda DianNo ratings yet
- Microscopic Colitis Is Characterized by Intestinal DysbiosisDocument3 pagesMicroscopic Colitis Is Characterized by Intestinal Dysbiosisalexandra robuNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Chicken Infectious AnemiaDocument6 pagesChicken Infectious AnemiaChristian VillarrealNo ratings yet
- Introduction To Exercise PrescriptionDocument46 pagesIntroduction To Exercise PrescriptionabhijeetNo ratings yet
- Blood TransfusionDocument28 pagesBlood TransfusionPORTRAIT OF A NURSENo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Brosur Dan Etikel RL Dan Salep MataDocument1 pageBrosur Dan Etikel RL Dan Salep MataSuwandi NhgNo ratings yet
- What Are Anxiety Disorder/depression?Document4 pagesWhat Are Anxiety Disorder/depression?Joanna Mæ Nuñez SaysønNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Saline SprayDocument3 pagesSaline Sprayagus subagiartaNo ratings yet
- LG 3.1 Pedigree AnalysisDocument27 pagesLG 3.1 Pedigree AnalysisAeon BeluanNo ratings yet
- 01 Colon Cancer Staging DR MasiaDocument66 pages01 Colon Cancer Staging DR MasiaAtyna CarelessNo ratings yet
- GYNE Endometrial Hyperplasia Dr. Ahyong Reyes Sleepy CrammersDocument3 pagesGYNE Endometrial Hyperplasia Dr. Ahyong Reyes Sleepy CrammersMiguel Luis NavarreteNo ratings yet
- Abbreviation For ChartingDocument12 pagesAbbreviation For ChartingJomar De BelenNo ratings yet
- Pediatric Nursing Reviewer 40 BulletsDocument4 pagesPediatric Nursing Reviewer 40 Bulletsjege80No ratings yet
- CABANADocument14 pagesCABANAIsmael Rivera DiazNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- JAGADocument2 pagesJAGAneurosurgery kimsNo ratings yet
- MYCO VIRO 1-MergedDocument29 pagesMYCO VIRO 1-MergedGennelyn Ross Delos ReyesNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hypertension: Unit-5 - Non-Communicable Disease Community Health Nursing - IDocument19 pagesHypertension: Unit-5 - Non-Communicable Disease Community Health Nursing - IPrabhakaran AranganathanNo ratings yet
- Health Status and Travel Declaration FormDocument1 pageHealth Status and Travel Declaration FormArmand HapinatNo ratings yet
- Pain Managment in Labor 2020Document5 pagesPain Managment in Labor 2020António BragaNo ratings yet
- Breastfeeding HivDocument20 pagesBreastfeeding HivPersonal Stories To KeepNo ratings yet
- Positive ResultDocument3 pagesPositive Resultநந்தினி வீரப்பெருமாள்No ratings yet
- Kunjungan Rawat Inap 11 November 2018Document22 pagesKunjungan Rawat Inap 11 November 2018asep sumarwanNo ratings yet
- Wellen EcgDocument9 pagesWellen EcgElokNo ratings yet
- Crop 311 Crop Protection - Lecture 5Document18 pagesCrop 311 Crop Protection - Lecture 5CindyNo ratings yet
- Collected Male Dr. Svasti Report Status: Final: Name Lab No. P 159709569 Mr. Dushyant HoodaDocument2 pagesCollected Male Dr. Svasti Report Status: Final: Name Lab No. P 159709569 Mr. Dushyant Hoodadushyant33% (3)
- 2nd QRT Drug Abuse Mapeh 9Document22 pages2nd QRT Drug Abuse Mapeh 9Alyssa GraceNo ratings yet
- Toxicology Uddd3303/Udee3313 Tutorial: Prepared by NGWJDocument1 pageToxicology Uddd3303/Udee3313 Tutorial: Prepared by NGWJMohana MaradamuthuNo ratings yet
- Surgery SyllabusDocument23 pagesSurgery SyllabusNajmul Hassan MubarakNo ratings yet
- 14.PhotoDermDiagnosis Keratotic Papules Over Chest and BackDocument3 pages14.PhotoDermDiagnosis Keratotic Papules Over Chest and BackDwi Tantri SPNo ratings yet