Professional Documents
Culture Documents
Endocarditis
Uploaded by
lhenOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Endocarditis
Uploaded by
lhenCopyright:
Available Formats
NCLEX Review Endocarditis
Definition: Inflammation of the endocardium layer of the heart.
What is the endocardium layer? The endocardium is a membrane that lines the inside of the
heart chambers and the heart valves.
How many heart valves do you have? Four….Atrioventricular (tricuspid and mitral valve) and
Semilunar (pulmonic and aortic valves)
Endocarditis mainly affects the heart valves but it can affect the:
• interventricular septum: this separates the right and left ventricles (perforation)
• chordae tendineae: fibrous cords of tendons that connect papillary muscle to the tricuspid
and bicuspid valves (rupture)
Endocarditis is hard to treat because there is no blood flow to the valves so the body does NOT
respond properly to the pathogen present (hence, WBCs can NOT get to the valves to fight the
infection) and it is hard for antibiotics to get to it (so the patient will need weeks of IV antibiotics).
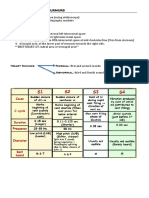
Types of Endocarditis:
• Infective (concentrated on in this lecture): bacteria, virus, or fungi gets into the bloodstream
and grows on the valve. The heart valves are more susceptible (especially defected heart
valves) to this because they don’t have a blood supply to help fight off infection (hence, white
blood cells). Therefore, the body doesn’t fight it properly.
• Patients who have weak heart valves due to defects on them are most at risk for this
(healthy valves are more resistant to the bacteria but can develop it as well).
• Examples of weak heart valves:
• Valve replacement (due to the increase risk of a thrombus forming on the valve is
the patient is not anticoagulated properly)
• Mitral valve prolapse
• Rheumatic heart disease
• History of IV drug use
• Invasive procedures: implanted device pacemaker, dental work surgery, central
line placement
• Congenital heart defects
Patients who have defective heart valves can experience complications of heart failure (valves are
leaking or have stenosis, embolic events (strokes), erosion of valve leaflets, and abscesses of the
heart tissue.
Non-effective: sterile platelets and fibrin (thrombus) form on the valve due to trauma or some
other issue (hypercoagulated blood) but it isn’t pathogenic. However, it is a site of origin for
possible infective endocarditis.
Patho of how a heart valve turns into Infective Endocarditis:
1. A defect on the valve allows platelets and fibrin (aka a thrombus…clotting ingredient) to stick
to the endothelial cells.
2. A pathogen enters into the blood (from invasive procedure….dental work, central line
placement, implantable device) and the pathogen sticks to the platelets and fibrin
(thrombus).
3. The pathogen is able to grow.
4. As it grows, parts of the pathogen, platelets, and fibrin can break off. This can cause a
stroke.
Type of Infective Endocarditis:
• Acute IE: affects patient who have healthy heart valves (high death rate). The onset is fast
and symptoms are very severe.
• Subacute IE: affects people who have a pre-existing condition like rheumatic heart disease,
valve problem. The symptoms are subtle and onset slower (several weeks to months to
develop).
*IV drug uses are susceptible to both
Signs and Symptoms of Infective Endocarditis:
Remember the mnemonic: Pathogens
Petechiae (tiny purplish red spots on the skin….from emboli)
Anorexia (loss of appetite and enlarged spleen pushing on the stomach)
Tired and weak
High Fever & Heart Failure
Osler’s Nodes: tender, red lesions on the hands and feet
finGernail changes: splinter hemorrhages that are small, dark lines under the nails…like petechiae
but found under the nails
Embolic events, Erythematous, non-tender nodular lesions on the palms or soles of feet (Janeway
Lesions)…small, septic emboli that form abscesses
Night sweats, New cardiac heart murmur or worsening of one
Splenomegaly (helps fight infection so it becomes enlarged), Roth Spots (burst of blood vessels in
the retinas with white centers)
Diagnosed:
TEE (transesophageal echocardiogram): an ultrasound probe is placed down through the
patient throat and it looks at the back side of the heart which helps assess the heart valves.
Nursing Interventions for Infective Endocarditis:
Monitor:
• Embolic episodes of the spleen, renal, brain, pulmonary status:
• Spleen embolic: radiating abdominal pain that goes to the left shoulder
• Renal: flank pain in the groin with possible pus or blood in the urine
• Brain (stroke): changes in neuro status…confusion, speech difficulty
• Pulmonary: chest pain, shortness of breath, dyspnea, decreased oxygen saturation
• Signs and symptoms of heart failure
• Monitor vital signs especially temperature, heart rate, blood pressure, oxygen saturation
Interventions:
• Collecting blood cultures to find out what type of microorganism is infecting the
patient…antibiotic treatment is based on this
• Administered IV antibiotics…type of antibiotics depends on the pathogen causing the
problem
• Example: Vancomycin or Rocephin (strong…usually need a central line because
patient will be on long term and go home on them…up to 4 weeks)
Educate the patient about:
• inform other healthcare practitioners about history of endocarditis because they are at risk
for it again and will need prophylactic antibiotics prior to invasive procedures
• how to take or administer antibiotics (complete all doses)
• monitor central line site and how to care for it
• good oral care
You might also like
- 7th Heart Sounds and MurmursDocument6 pages7th Heart Sounds and MurmursbabibubeboNo ratings yet
- Heart BlocksDocument3 pagesHeart BlockslhenNo ratings yet
- 1st Year Anatomy Final Exam ImpDocument19 pages1st Year Anatomy Final Exam ImpSai Pardhu100% (1)
- L3,4-Cardiac Cycle Mcqs Fre, XBN.DDocument7 pagesL3,4-Cardiac Cycle Mcqs Fre, XBN.DsajidNo ratings yet
- Anatomy Quiz 2Document45 pagesAnatomy Quiz 2Upscaled100% (1)
- 25) Aetiology and Pathogenesis of Valvular Heart DiseaseDocument34 pages25) Aetiology and Pathogenesis of Valvular Heart DiseaseGurrajvin Singh0% (1)
- Aortic Valve DiseaseDocument63 pagesAortic Valve DiseaseFaridOrahaNo ratings yet
- MedicineDocument9 pagesMedicinernvisNo ratings yet
- Congenital Heart Disease (CHD) : Kussia Ayano (MD)Document54 pagesCongenital Heart Disease (CHD) : Kussia Ayano (MD)Yemata HailuNo ratings yet
- De Anisya Tri Ab - CBD - 30101507419 - FixDocument198 pagesDe Anisya Tri Ab - CBD - 30101507419 - FixFarah UlyaNo ratings yet
- Valvular Heart DiseasesDocument29 pagesValvular Heart Diseasesbpt2No ratings yet
- Infective EndocarditiDocument31 pagesInfective EndocarditiMansi DabolaNo ratings yet
- Nursing Professional ResponsibilitiesDocument9 pagesNursing Professional ResponsibilitieslhenNo ratings yet
- Chapter 2 Blood Circulation & TransportDocument37 pagesChapter 2 Blood Circulation & TransportYanhyNo ratings yet
- Anak 3.1 Infective Endocarditis DRTLTDocument21 pagesAnak 3.1 Infective Endocarditis DRTLTAnastasia PinkyNo ratings yet
- Endocarditis, Pericarditic, Myocarditis: TopicDocument104 pagesEndocarditis, Pericarditic, Myocarditis: TopicOM VERMANo ratings yet
- Mksap 17 MCQ FullDocument282 pagesMksap 17 MCQ Fullfermann100% (1)
- Endokarditis, Miokarditis Perikarditis: Blok KardiovaskularDocument31 pagesEndokarditis, Miokarditis Perikarditis: Blok KardiovaskularTiara RamliNo ratings yet
- Renr Practice Test 7 FinalDocument13 pagesRenr Practice Test 7 FinalTk100% (1)
- Infective Endocarditis: Hariprasad KDocument28 pagesInfective Endocarditis: Hariprasad KHari Prasad K100% (1)
- True PDFDocument459 pagesTrue PDFAmna MmfNo ratings yet
- EndocarditisDocument13 pagesEndocarditisSumathi GopinathNo ratings yet
- 9) Infective Endocarditis (IE)Document3 pages9) Infective Endocarditis (IE)Aris PaparisNo ratings yet
- Endocarditis, MyocarditisDocument37 pagesEndocarditis, MyocarditisJuma AwarNo ratings yet
- Infective EndocarditisDocument10 pagesInfective EndocarditisShrests SinhaNo ratings yet
- Rheumatic Heart Disease: Dr. Gehan Mohammed Dr. Abdelaty ShawkyDocument46 pagesRheumatic Heart Disease: Dr. Gehan Mohammed Dr. Abdelaty ShawkyimanNo ratings yet
- Infectious EndocarditisDocument4 pagesInfectious EndocarditisKhalid Mahmud Arifin100% (1)
- Ch. 36 - Infectious Diseases of The Heart, Infective Endocarditis, Myocarditis, and PericarditisDocument34 pagesCh. 36 - Infectious Diseases of The Heart, Infective Endocarditis, Myocarditis, and Pericarditisمحمد الحواجرةNo ratings yet
- Infeksi JantungDocument36 pagesInfeksi JantungIntania FadillaNo ratings yet
- Rheumatic Fever & Infective EndocarditisDocument46 pagesRheumatic Fever & Infective EndocarditisMosab MasoudNo ratings yet
- Case Presentation of Infective Endocarditis-1Document23 pagesCase Presentation of Infective Endocarditis-1pritidinda3070No ratings yet
- Inflammatory and Valvular DisordersDocument43 pagesInflammatory and Valvular DisordersRifqi Hary ZulfikarNo ratings yet
- HHD VHD Systemic PathoDocument22 pagesHHD VHD Systemic PathoJireh MejinoNo ratings yet
- Infective EndocarditisDocument37 pagesInfective EndocarditisBiruk WorkuNo ratings yet
- Infective Endocarditis FinalDocument32 pagesInfective Endocarditis FinalAbdallahNo ratings yet
- Cardiac Pathology 2 Alzahrawi PDFDocument43 pagesCardiac Pathology 2 Alzahrawi PDFMΘΘNNo ratings yet
- CASE STUDY - Infective EndocarditisDocument6 pagesCASE STUDY - Infective EndocarditisDudil GoatNo ratings yet
- PathologyDocument28 pagesPathologyakkashamrishNo ratings yet
- Infections of The Cardiovascular System 2024Document46 pagesInfections of The Cardiovascular System 2024aguilarjanicaNo ratings yet
- Infective EndocarditisDocument66 pagesInfective Endocarditissanjivdas100% (4)
- Subjective Data Objective DataDocument4 pagesSubjective Data Objective DataElena Cariño De GuzmanNo ratings yet
- Cardiac Infections: (Outside To Inside)Document7 pagesCardiac Infections: (Outside To Inside)Ashley MalsonNo ratings yet
- Infective Endocarditis: Akriti DahalDocument79 pagesInfective Endocarditis: Akriti DahalAkriti100% (1)
- Infective Endocarditis.... MshembaDocument39 pagesInfective Endocarditis.... MshembaTimothy Casmiry MshembaNo ratings yet
- Infective EndocarditiDocument31 pagesInfective EndocarditiMansi DabolaNo ratings yet
- ValvularHeartDisease Notes S5w4Document6 pagesValvularHeartDisease Notes S5w4razzletothedazzleNo ratings yet
- Infective Endocarditis (IE)Document76 pagesInfective Endocarditis (IE)Mahesh RathnayakeNo ratings yet
- VALVULAR HEART DISEASE Copy AutosavedDocument33 pagesVALVULAR HEART DISEASE Copy AutosavedShienna Rose Ann ManaloNo ratings yet
- 1 - Rheumatic Fever and Valvular Diseases (Summary and MCQS)Document12 pages1 - Rheumatic Fever and Valvular Diseases (Summary and MCQS)فرقان سلام عيسى عبدNo ratings yet
- Infective Endocarditis 4TH (Compatibility Mode)Document14 pagesInfective Endocarditis 4TH (Compatibility Mode)Mohammed Al-KebsiNo ratings yet
- 8 EndocarditisDocument19 pages8 EndocarditisdaisyNo ratings yet
- Infective EndocarditisDocument50 pagesInfective EndocarditisIsaac ayobamiNo ratings yet
- Cardiovascular Disorders in Children - StudentDocument53 pagesCardiovascular Disorders in Children - StudentKeanu Win CatipayNo ratings yet
- Inflammatory Disorders PDFDocument41 pagesInflammatory Disorders PDFMoon KillerNo ratings yet
- Disturbances in The Blood Flow1Document41 pagesDisturbances in The Blood Flow1ammar amerNo ratings yet
- Cardiac+Conditions 1Document14 pagesCardiac+Conditions 1simonedarling100% (2)
- Cardio InfectionDocument6 pagesCardio InfectionCindy Mae de la TorreNo ratings yet
- Report Pathopysiology (Endocarditis) 12Document7 pagesReport Pathopysiology (Endocarditis) 12Ade Yulina Mursyidah Sa'adNo ratings yet
- 6.infective EndocarditisDocument62 pages6.infective Endocarditisbereket gashuNo ratings yet
- Ventricular Septal DefectDocument43 pagesVentricular Septal DefectmalekNo ratings yet
- PAEDs - CVS-1Document44 pagesPAEDs - CVS-1Priscah bhokeNo ratings yet
- Risk Factors Include Having: Congenital Heart DefectsDocument3 pagesRisk Factors Include Having: Congenital Heart Defectspragna novaNo ratings yet
- Infective Endocarditis Case ReportDocument40 pagesInfective Endocarditis Case Reportliu_owen17100% (1)
- Case Study Worksheet EndocarditisDocument6 pagesCase Study Worksheet EndocarditisSharlee StoneNo ratings yet
- Infective EndocarditisSDocument26 pagesInfective EndocarditisSDeepika LingamNo ratings yet
- Endocarditis Internal Medicine 15 March2020Document33 pagesEndocarditis Internal Medicine 15 March2020Ledia EssamNo ratings yet
- S Infective EndocarditisDocument24 pagesS Infective EndocarditisMpanso Ahmad AlhijjNo ratings yet
- Infective EndocarditisDocument49 pagesInfective EndocarditismajdNo ratings yet
- Infective Endocarditis Year 2 Semester1 - 010117-1Document13 pagesInfective Endocarditis Year 2 Semester1 - 010117-1chebetnaomi945No ratings yet
- 2 - RH Fev, Inf EndoDocument37 pages2 - RH Fev, Inf EndoLobna ElkilanyNo ratings yet
- cvs6 IEDocument21 pagescvs6 IEsavyasachinNo ratings yet
- Beating with Precision: The Science of Cardiology: Understand the Intricacies of the Human HeartFrom EverandBeating with Precision: The Science of Cardiology: Understand the Intricacies of the Human HeartNo ratings yet
- Pericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerDocument2 pagesPericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerlhenNo ratings yet
- CHF Low Salt Diet TeachingDocument2 pagesCHF Low Salt Diet TeachinglhenNo ratings yet
- Myocardial Infarction NCLEX ReviewDocument4 pagesMyocardial Infarction NCLEX ReviewlhenNo ratings yet
- How To Count Atrial and Ventricular Rate Using The 6 Second RuleDocument2 pagesHow To Count Atrial and Ventricular Rate Using The 6 Second RulelhenNo ratings yet
- Atrial Fib Vs Atrial FlutterDocument3 pagesAtrial Fib Vs Atrial FlutterlhenNo ratings yet
- 1 Cardiovascular System by DR - Sana TauqeerDocument38 pages1 Cardiovascular System by DR - Sana TauqeerSyed Ali Faizan NaqviNo ratings yet
- Anaphy - Lesson 4 - Topic 4 and 5Document21 pagesAnaphy - Lesson 4 - Topic 4 and 5Rica Abigail DagosNo ratings yet
- Using The Surface Electrocardiogram To Localization of Idiopathic Ventricular TachycardiaDocument12 pagesUsing The Surface Electrocardiogram To Localization of Idiopathic Ventricular TachycardiaNavojit ChowdhuryNo ratings yet
- Ebook Echocardiography With SimulationsDocument91 pagesEbook Echocardiography With SimulationsAbdul WaheedNo ratings yet
- Chapter 7. CirculationDocument54 pagesChapter 7. CirculationankurbiologyNo ratings yet
- Human Body Revision NotesDocument83 pagesHuman Body Revision NotesdoaaNo ratings yet
- Necropsy Techniques: General Pathology (VPM 152) Jan 2008Document5 pagesNecropsy Techniques: General Pathology (VPM 152) Jan 2008Naresh RaviNo ratings yet
- Specification Z8Document17 pagesSpecification Z8Radiologi JagakarsaNo ratings yet
- Pcap D, CHF 2 CHDDocument78 pagesPcap D, CHF 2 CHDtrew_wertNo ratings yet
- Perevod Natalya VasilevnaDocument186 pagesPerevod Natalya Vasilevnamohammad farooque razaa71% (7)
- CardioDocument48 pagesCardiomalisalukmanNo ratings yet
- Liverpool SDL IABPDocument26 pagesLiverpool SDL IABPSathya Swaroop PatnaikNo ratings yet
- Calcification AorticDocument28 pagesCalcification AorticGaal PinNo ratings yet
- Ebstein AnomalyDocument14 pagesEbstein AnomalyNataliaMaedyNo ratings yet
- AnaPhy Lab Exercise 24-41Document6 pagesAnaPhy Lab Exercise 24-41Angelyka Cabalo50% (2)
- Contemporary Reviews in Cardiovascular Medicine: Epidemiology and Pathophysiology of Mitral Valve ProlapseDocument14 pagesContemporary Reviews in Cardiovascular Medicine: Epidemiology and Pathophysiology of Mitral Valve ProlapseyunielsyaNo ratings yet
- APMC Questionaire For ANATOMYDocument17 pagesAPMC Questionaire For ANATOMYChristian Mark Gerard TuveraNo ratings yet
- Physio 2 - NotesDocument157 pagesPhysio 2 - NotesSivaranjini BhalaNo ratings yet