Professional Documents
Culture Documents
Jurnal Cardio
Uploaded by
tiaanastaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal Cardio
Uploaded by
tiaanastaCopyright:
Available Formats
[Downloaded free from http://www.nigjcardiol.org on Friday, June 28, 2019, IP: 202.67.46.
42]
Original Article
Significant pleural effusion in congestive heart failure
necessitating pleural drainage
Eyo Effiong Ekpe, Ime O. Essien1, Umoh Idongesit1
Departments of Surgery, Cardiothoracic Surgery Unit, and 1Internal Medicine, Cardiology Unit, University of Uyo Teaching Hospital,
Uyo, Akwa Ibom, Nigeria
Address to correspondence: ABSTRACT
Dr. Eyo Effiong Ekpe,
Department of Surgery, Background: Pleural effusion is very common in congestive heart failure, and should resolve with treatment
Cardiothoracic Surgery Unit,
University of Uyo Teaching
of congestive heart failure, including diuretic. However, refractory, recurrent, massive, or significant pleural
Hospital, P.M.B. 1136, effusions contributing to symptoms in the patients with congestive heart failure warrant treatment by pleural
Uyo, Akwa Ibom, Nigeria. drainage. We sought to discover the clinic‑pathologic characteristic of such pleural effusion in our congestive
E‑mail: docekpe@yahoo. heart failure patients.
com
Materials and Methods: Retrospective analysis of medical records of congestive heart failure patients admitted
for inpatient treatment between January 2007 and June 2011.
Access this article online
Results: Out of the 342 patients that presented with congestive heart failure during the study period, ten (2.9%)
Website: www.nigjcardiol.org patients had significant pleural effusions in 12 pleural spaces that contributed to symptoms and refused to
DOI: 10.4103/0189-7969.152020
resolve on treatment of the congestive heart failure including diuretic. Male:Female was 1.2:1, modal age
range 40–50 years, 50% in the left, 30% in the right, and 20% bilateral. The estimate of the pleural effusion
Quick response code was <1000 ml–>2000 ml with 90% being transudate and 10% exudates. One patient had associated
pericardial effusion. Upon drainage, 70% of the patients improved immediately.
Conclusion: We recommend drainage of refractory, recurrent, massive, significant pleural effusion in congestive
heart failure contributing to symptoms and responding to diuretic therapy.
KEY WORDS: Congestive heart failure, drainage, pleural effusion
INTRODUCTION The pleural effusion in heart failure is usually small,
bilateral, and spontaneously resolves with the treatment
Pleural effusions, the result of the accumulation of fluid of the heart failure. [6] Rarely does pleural effusion
in the pleural space, are a common medical problem.[1] associated with heart failure requires drainage.[3,4,6] Our
They can be caused by several mechanisms including experience shows the occurrence of symptomatic pleural
increased permeability of the pleural membrane, effusion in our heart failure patients which would not
decreased negative intrapleural pressure, decreased resolve spontaneously with heart failure management,
oncotic pressure, obstructed lymphatic flow, and therefore, requiring drainage. This study therefore aims
increased pulmonary capillary pressure or increased to elucidate the clinico‑pathologic characteristics of
hydrostatic pressure.[1] Pleural effusions are classified into pleural effusion in cardiac failure patients requiring
exudative and transudative using the Light’s criteria.[2] A closed tube thoracostomy drainage (CTTD).
transudative pleural effusion occurs when the balance
of hydrostatic forces influencing the formation and MATERIALS AND METHODS
absorption of pleural fluid is altered to favor pleural fluid
accumulation, and is the type usually encountered in Retrospective analysis of the medical records of our heart
patients with heart failure including left ventricular failure failure patients who had associated significant pleural
and congestive heart failure.[1,2] Heart failure is reckoned effusion between January 2007 and June 2011 was
as a very common cause of pleural effusion in all parts done. Data on demography, socio‑economic parameters,
of the world, and also discovered to be the commonest clinical presentation, radiological findings, diagnosis,
cause of pleural effusion in some parts of the world.[1‑5] pleural aspirate analysis, treatment, and outcome were
106 Nigerian Journal of Cardiology | July - December 2015 | Vol 12 | Issue 2
[Downloaded free from http://www.nigjcardiol.org on Friday, June 28, 2019, IP: 202.67.46.42]
Ekpe, et al.: Significant pleural effusion in congestive heart failure
collated. The diagnosis of heart failure was made using the both the right and left posterior costophrenic angles, or
Framingham’s criteria of two major criteria or one major if there was minimal blunting of both the right and left
and two minor criteria.[7] The major criteria considered posterior and lateral costophrenic angles. Small pleural
included paroxysmal nocturnal dyspnea, neck vein effusions resulting in blunting of both the posterior and
distension, rales, cardiomegaly, acute pulmonary edema, lateral costophrenic angles on one side were said to be
S3 gallop, increased venous pressure (>16 cm of H20), larger than small pleural effusions that caused blunting
positive hepatojugular reflux; while the minor criteria of the posterior costophrenic angle only on the other side.
were extremity edema, night cough, dyspnea on exertion, Moderate and large bilateral pleural effusions were said
hepatomegaly, pleural effusion, vital capacity reduced by to be of the same size if the position of the highest point
1/3 from normal, and tachycardia (>120 bpm). Weight of the meniscus of fluid along the right lateral chest
loss >4.5 kg over 5 days’ treatment was given equal wall was at the same level as the highest point of the
weighting as major or minor criterion.[7] meniscus of fluid along the left lateral chest wall, or if
the two were separated by a centimeter or less. Moderate
The following signs of pleural effusion were evaluated or large pleural effusions on one side were said to be
on each patient’s postero‑anterior (PA) and lateral chest larger than moderate or large pleural effusions on the
radiograph obtained at the time of presentation: Blunting contralateral side if the position of the highest point of
of the posterior and lateral costophrenic angles; the the meniscus of fluid along the lateral chest wall on one
meniscus sign; manifestations of subpulmonic collection side was higher than that on the contralateral side by
of pleural effusion including increased separation of more than one centimeter.[8] The patients’ medical records
aerated right lung and subdiaphragmatic fat on the were also reviewed to see if thoracentesis was performed
right compared with prior chest radiographs, increased in any of these cases.
separation of aerated left lung and the gastric air bubble
on the left compared with prior chest radiographs, The diagnosis of pleural effusion confirmed in all patients
and flattening or lateral shift of the “apparent” apex using plain chest radiograph which also helped in
of the right or left hemidiaphragm (pseudodiaphragm) estimation of the amount of the pleural effusion was
compared with prior chest radiographs; and obscuration further confirmed during closed tube thoracostomy
of pulmonary vessels below the level of the upper margin drainage as the initial amount of pleural fluid drained
of the pleural effusion or right or left pseudodiaphragm.[8] into the drainage bottle following placement of the
The presence or absence of pleural effusion in the right drainage tube.
and left hemithorax was recorded for each case. The size
of pleural effusion was roughly quantified as follows. Samples of the fluid were subjected to biochemical
If minimal detectable blunting of the posterior and/or analysis bases on the parameters of Light’s criteria for
lateral costophrenic angle was evident on the PA and characterisation of the pleural effusion as transudate or
lateral chest radiograph, the quantity of pleural effusion exudate. It was the only single case of exudate that was
was classified as small. This is reported to correlate with subjected to further tests of cytology, microscopy, culture
pleural effusions in the range of 25 to 525 mL.[8] Effusions and sensitivity, and Ziehl‑Nellsen stain. Analysis was by
were classified as moderate in size if the effusion occupied simple proportions and percentages.
the lower part of the hemithorax but did not extend
above the fourth rib anteriorly on the PA view. This RESULTS
correlates with pleural effusions larger than 525 mL.[9‑11]
Large effusions extended above the level of the fourth Out of the 342 adult patients diagnosed, admitted, and
anterior rib on the PA view.[9‑11] The distribution of pleural treated for heart failure during the study period, only
effusion was recorded in each case as falling into one of ten (2.9%) had associated significant pleural effusion in
the following five categories: Right‑sided only; bilateral 12 pleural spaces that required pleural drainage. There
but larger on the right side than the left; bilateral and of were six males and four females and all ten patients
roughly equal size on each side; bilateral but larger on the were adults with the modal age‑group being 40–60 years
left side than the right; and left‑sided only. When there where 60% of the patients belonged [Table 1]. The
were bilateral pleural effusions, the following criteria were remaining 40% were evenly distributed in the below
used to determine whether or not the effusions were of 40 years and above 60 years age‑groups. Analysis of
the same size. Since the posterior costophrenic angle the occupational status of the ten patients shows that
is lower in position in the hemithorax than the lateral 50% of them were unemployed as at the time of onset
costophrenic angle, small pleural effusions typically of their illness, while the remaining were either public
cause blunting of the posterior costophrenic angle on the servants (30%) or self‑employed (20%). Table 1 further
lateral chest radiograph before they cause blunting of the shows that half of the patients were either uneducated
lateral costophrenic angle on the PA chest radiograph.[8] or attended only primary education, while the remaining
Small bilateral pleural effusions were classified as being 50% had secondary education (40%) or tertiary level of
of the same size if there was either minimal blunting of education (10%).
Nigerian Journal of Cardiology | July - December 2015 | Vol 12 | Issue 2 107
[Downloaded free from http://www.nigjcardiol.org on Friday, June 28, 2019, IP: 202.67.46.42]
Ekpe, et al.: Significant pleural effusion in congestive heart failure
[Table 2] shows that the cardinal symptoms of cardiac while one (50%) did not. Outstandingly, all the
failure were experienced by all the ten patients who had five (100%) patients whose pleural effusion was more
significant pleural effusion. These symptoms include than 2000 ml had significant symptomatic relief upon
cough, dyspnea, easy fatigability, and dependent edema, drainage of the pleural effusion.
while [Table 3] shows the causes of heart failure to include
systemic hypertension in 50% of the patients, rheumatic DISCUSSION
heart disease in 30%, and dilated cardiomyopathy in the
remaining 20% of the patients. Pleural effusion in heart failure results from increased
interstitial fluid in the lung due to elevated pulmonary
By Light’s criteria, the pleural effusion was transudates
capillary pressure.[1‑5] It used to be believed before now
in 90% of the cases, while exudates was discovered in
that pleural effusion in heart failure should be bilateral,
only 10% of the cases. Analysis of the distribution of the
or if unilateral should be on the right.[6,12] Isolated
pleural effusion shows that 50% occurred in the left side,
left‑sided pleural or bilateral pleural effusion worse
30% in the right side and the remaining 20% occurred
on the left in patient with heart failure was thought to
bilaterally [Tables 4 and 5] contains information on the
be caused by additional pathology.[12] Such cases were
severity of the pleural effusion and the response of the
subjected to additional diagnostic investigations and
patients to the drainage of the pleural effusion. Of the
pleural drainage.[11] Pleural effusion in heart failure was
three patients whose pleural fluid accumulation was
also believed to be transudative only occurring as a result
less than 1000 ml, only one (33%) had symptomatic
improvement upon drainage of the pleural effusion, of systemic factors.[1‑5,11] Discovery of exudative pleural
while two (66%) did not have significant symptomatic effusion in heart failure patient was attributed to pathology
relief immediately following pleural fluid drainage. of the pleural membrane and therefore warranted further
Again of the two patients whose pleural effusion was diagnostic investigations and treatment.[11,13]
between 1000 to 2000 ml, one (50%) had symptomatic
improvement upon drainage of the pleural effusion, However, more recently, it has been discovered that
pleural effusion of uncomplicated heart failure can in
up to 25% of cases be exudate, and it can be distributed
Table 1: Demography and socio‑economic characteristics
bilaterally worse on any side, right‑sided, or left‑sided.[11]
of patients with significant pleural effusion in congestive
This present study corroborated this with significant
heart failure
left sided pleural effusion being present in up to 50% of
Parameter Female Male Total
patients with congestive heart failure who needed pleural
Age‑groups drainage with 10% being exudates [Table 4].
18-39 1 1 2
40-60 2 3 6
Table 3: Causes of heart failure in patients with massive
>60 1 1 2 pleural effusion in congestive heart failure
Total 4 6 10
Cause of heart failure Female Male Total
Employment status
Systemic hypertension 2 3 5
Civil servant 1 2 3
Valvular heart disease 1 2 3
Self‑employed 1 1 2
Dilated cardiomyopathy 1 1 2
Unemployed 2 3 5
Total 4 6 10
Total 4 6 10
Educational status
Non‑formal 1 2 3 Table 4: Characteristics of pleural effusion in patients with
Primary 1 1 2 significant pleural effusion in congestive heart failure
Secondary 2 2 4 Type Left side Right side Bilateral Total
Tertiary ‑ 1 1 Transudate 4 3 2 9
Total 4 6 10 Exudate 1 ‑ ‑ 1
Total 5 3 2 10
Table 2: Cardinal presenting symptoms in patients with
massive pleural effusion in congestive heart failure Table 5: Response to drainage of pleural fluid in patients
Symptoms Female Male Total with significant pleural effusion in congestive heart failure
Cough 4 6 10 Initial drainage Improved Not improved Total
Dyspnea 4 6 10 <1000 ml 1 2 3
Easy fatigability 4 6 10 1000-2000 ml 1 1 2
Dependent edema 4 6 10 >2000 ml 5 ‑ 5
Total 4 6 10 Total 7 3 10
108 Nigerian Journal of Cardiology | July - December 2015 | Vol 12 | Issue 2
[Downloaded free from http://www.nigjcardiol.org on Friday, June 28, 2019, IP: 202.67.46.42]
Ekpe, et al.: Significant pleural effusion in congestive heart failure
This study documents 2.9% cases of significant pleural
effusion in heart failure necessitating pleural drainage.
Of the patients whose pleural effusion was less than 1000
ml, only about 33% reported improvement in symptoms
immediately following pleural fluid drainage. The
improvement was based on respiratory effort and exercise
tolerance. This may imply that in heart failure patients
whose pleural effusion is less than 1000 ml, pleural
drainage may not be absolutely necessary. However, when
the pleural effusion is estimated to be above 2000 ml,
pleural drainage becomes absolutely beneficial as 100% of
the patients in this category had symptomatic improvement
following pleural drainage. For patients whose pleural fluid
is between 1000–2000 ml, the possibility of benefit stands
at 50% as exhibited by this same study.
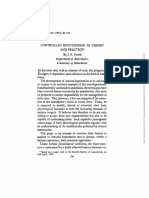
Figure 1: Intra-operative mini left thoracotomy and window The other findings of this study have corroborated findings
pericardiostomy of the single patient that presented with pericardial of previous related studies. Both transudate (90%) and
effusion and left sided pleural effusion in congestive heart failure exudate (10%) and pleural effusion distributed as
bilateral, right‑sided, and left‑sided have previously
Because the pleural effusion of heart failure is generally been documented.[11] Also occurrence in both males and
transudate and most of the times small or moderate, it is females as was found in the presence study has previously
usually not given any specific treatment. Rather when the been noted, although the study by Woodring was only
heart failure is treated with diuretic, the pleural effusion on male patients.[11] One of our patients had associated
is expected to resolve.[3‑6] This position is partly so because pericardial effusion which has also been reported in
the symptoms of heart failure and pleural effusion are other studies.[19‑22] This patient’s treatment consisted of
to a large extent similar and it may be difficult to know mini‑thoracotomy and window pericardiostomy [Figure 1].
what proportion of the symptoms are attributable to the Finally in one of the two patients that presented with
pleural effusion as an entity. When the pleural effusion massive bilateral pleural effusion in congestive heart
in congestive heart failure is refractory, recurrent, failure, the fluids were not similar as one side was
significant, massive, or large enough to cause symptoms, transudate and the other side exudates. This pattern has
drainage of the plural fluid should be undertaken.[2,14‑16] previously been reported by Kalomenidis et al.[23]
The socio‑demographic characteristics of heart failure CONCLUSION
patients with significant pleural effusion were not different
from those without significant pleural effusion. Most of Pleural effusion of heart failure can occur bilaterally or
them (60%) belonged to middle age of 40–50 years with unilaterally in either pleural space, can be transudate
slight male preponderance with female: Male ratio of 1:1.2. or exudates, and should be drained when significantly
About 50% of the patients were unemployed which may massive to contribute to symptoms.
mean that early symptoms of heart failure may have been
neglected because of poverty. Same has been discovered
REFERENCES
in the region in a paper that advocated the expansion of
national health insurance scheme to benefit unemployed 1. Fridlender ZG, Gotsman I. Pleural effusion. N Engl J Med
citizens.[17] Low level of education has also been discovered 2002;347:1286‑7.
to correlate with late presentation of diseases to healthcare 2. Light RW, Broaddus VC. Pleural Effusion. In: Murray JF, Nadel JA,
facilities because of prior presentations to medical Mason RJ, Boushey HA, editors. Textbook of respiratory medicine.
3rd ed. Philadelphia: WB Saunders; 2000. p. 2013‑41.
charlatans which make situation worse.[18] 3. Johnson JL. Pleural effusions in cardiovascular disease: Pearls
for correlating the evidence with the cause. Postgrad Med
The etiology of heart failure in the patients with 2000;107:95‑101.
significant pleural effusion was not different from those 4. Porcel JM. Pleural effusions from congestive heart failure. Semin
Respir Crit Care Med 2010;31:689‑97.
without significant pleural effusion. In half of the patients
5. Chakko S. Pleural effusion in congestive heart failure. Chest
the cause was long term systemic hypertension, valvular 1990;98:521‑2.
heart disease in 30%, and dilated cardiomyopathy in 6. Raasch BN. Carsky EW, Lane EJ, O’Callaghan JP, Heitzman ER.
the remaining 20% [Tables 3 and 4] shows that all the Pleural effusion: Explanation of some typical appearances. AJR Am
patients with significant pleural effusion in heart failure J Roentgenol 1982;139:899‑904.
7. Maestre A, Gil V, Gallego J, Aznar J, Mora A, Martín‑Hidalgo A.
presented with the four cardinal symptoms of heart
Diagnostic accuracy of clinical criteria for identifying systolic and
failure which include productive cough, dyspnea, easy diastolic heart failure: Cross‑sectional study. J Eval Clin Pract
fatigability, and pitting pedal/leg edema.[7] 2009;15:55‑61.
Nigerian Journal of Cardiology | July - December 2015 | Vol 12 | Issue 2 109
[Downloaded free from http://www.nigjcardiol.org on Friday, June 28, 2019, IP: 202.67.46.42]
Ekpe, et al.: Significant pleural effusion in congestive heart failure
8. Vix VA. Roentgenographic recognition of pleural effusion. JAMA 18. Ekpe EE. Akpan MU. Poorly treated broncho‑pneumonia with
1974;229:695‑8. progression to empyema thoracis in Nigerian children. TAF Prev Med
9. Onadeko BO. The radiological patterns of pleural effusions in Bull 2010;9:181‑6.
Nigerians. Niger Med J 1979;9:687‑91. 19. Kataoka H. Pericardial and pleural effusions in decompensated chronic
10. Colins JD, Burwell D, Furmanski S, Lorber P, Steckel RJ. Minimal heart failure. Am Heart J 2000;139:918‑23.
detectable pleural effusions. A roentgen pathology model. Radiology 20. Natanzon A, Kronzon I. Pericardial and pleural effusions in congestive
1972;105:51‑3. heart failure‑anatomical, pathophysiologic, and clinical considerations.
11. Woodring JH. Distribution of pleural effusion in congestive heart failure: Am J Med Sci 2009;338:211‑6.
What is atypical? South Med J 2005;98:518‑23. 21. Peterman TA, Brothers SK. Pleural effusions in congestive heart failure
12. Weiss JM, Spodick DH. Laterality of pleural effusions in chronic and in pericardial disease. N Engl J Med 1983;309:313.
congestive heart failure. Am J Cardiol 1984;53:951. 22. Brixey AG, Light RW. Pleural effusions occurring with right heart failure.
13. Muller NL, Fraser RS, Colman NC, et al. Radiologic Diagnosis of Curr Opin Pulm Med 2011;17:226‑31.
Diseases of the Chest. Philadelphia: WB Saunders Co; 2001. p. 653‑4. 23. Kalomenidis I, Rodriguez M, Barnette R, Gupta R, Hawthorne M,
14. Kinasewitz GT. Transudative effusions. Eur Respir J 1997;10:714‑8. Parkes KB, et al. Patient with bilateral pleural effusion: Are the findings
15. Herlihy JP, Loyalka P, Gnananandh J, Gregoric ID, Dahlberg CG, the same in each fluid. Chest 2003;124:167‑76.
Kar B, et al. PleurX catheter for the management of refractory
pleural effusions in congestive heart failure. Tex Heart Inst J
2009;36:38‑43.
16. Chetty KG. Transudative pleural effusions. Clin Chest Med How to cite this article: Ekpe EE, Essien IO, Idongesit U. Significant pleural
1985;6:49‑54. effusion in congestive heart failure necessitating pleural drainage. Nig J
17. Ekpe EE, Umanah IN, Ikpe MC. Neglected soft tissue chest wall Cardiol 2015;12:106-10.
tumours in Nigeria; A call for expansion of national health insurance Source of Support: Nil, Conflict of Interest: None declared.
scheme. Int J Trop Surg 2012;6:55‑9
110 Nigerian Journal of Cardiology | July - December 2015 | Vol 12 | Issue 2
You might also like
- 714 Full PDFDocument5 pages714 Full PDFMuhammad Aulia RahmanNo ratings yet
- Pleur Odes IsDocument29 pagesPleur Odes IsjamalNo ratings yet
- Reviews: Congestion in Heart Failure: A Contemporary Look at Physiology, Diagnosis and TreatmentDocument15 pagesReviews: Congestion in Heart Failure: A Contemporary Look at Physiology, Diagnosis and TreatmentntnquynhproNo ratings yet
- 1153-Article Text-4888-1-10-20200206 PDFDocument6 pages1153-Article Text-4888-1-10-20200206 PDFAdrian CaballesNo ratings yet
- SaludDocument16 pagesSaluddianamera84No ratings yet
- Hemodynamic Parameters To Guide Fluid Therapy: Review Open AccessDocument9 pagesHemodynamic Parameters To Guide Fluid Therapy: Review Open AccessClaudioValdiviaNo ratings yet
- Recurrent Unilateral Pleural Effusion From Constrictive Pericarditis of Unknown Etiology Requiring PericardiectomyDocument3 pagesRecurrent Unilateral Pleural Effusion From Constrictive Pericarditis of Unknown Etiology Requiring PericardiectomyJaya Semara PutraNo ratings yet
- Pericardial EffusionDocument26 pagesPericardial EffusionjsenocNo ratings yet
- Pleuraleffusion 160424141916Document20 pagesPleuraleffusion 160424141916Jessa Adenig100% (1)
- Research ArticleDocument8 pagesResearch ArticleMiguelNo ratings yet
- Oncologicmechanical Emergencies: Umar A. Khan,, Carl B. Shanholtz,, Michael T. MccurdyDocument14 pagesOncologicmechanical Emergencies: Umar A. Khan,, Carl B. Shanholtz,, Michael T. MccurdySandra PargaNo ratings yet
- Sepsis Parte 2Document12 pagesSepsis Parte 2Maria AlejandraNo ratings yet
- Apasi Yg Ga Buat NisaDocument20 pagesApasi Yg Ga Buat Nisamuhammad iqbal mahfuzhNo ratings yet
- Pleural Effusion in Adults-Etiology, Diagnosis, and Treatment (24.05.2019)Document10 pagesPleural Effusion in Adults-Etiology, Diagnosis, and Treatment (24.05.2019)lordiroh1No ratings yet
- Clinical CardiologyDocument5 pagesClinical CardiologyMarco BiscosiNo ratings yet
- Jennifer T Thibodeau Characterization of A NovelDocument8 pagesJennifer T Thibodeau Characterization of A NovelHayley NicNo ratings yet
- Pulmonary Edema - StatPearls - NCBI BookshelfDocument7 pagesPulmonary Edema - StatPearls - NCBI BookshelfriyanasirNo ratings yet
- The Diagnosis and Treatment of Pulmonary Valve SteDocument6 pagesThe Diagnosis and Treatment of Pulmonary Valve SteNiarti Ulan SariNo ratings yet
- Fluid Managemnet-HfDocument16 pagesFluid Managemnet-HfAri Dwi PrasetyoNo ratings yet
- Cor Pulmonale - StatPearls - NCBI BookshelfDocument4 pagesCor Pulmonale - StatPearls - NCBI BookshelfAldi RafaelNo ratings yet
- Transesophageal Echocardiography: The Hemodynamic Monitoring UtilizingDocument14 pagesTransesophageal Echocardiography: The Hemodynamic Monitoring UtilizingvegasbabyNo ratings yet
- Management of Pericardial Effusion: Clinical UpdateDocument13 pagesManagement of Pericardial Effusion: Clinical UpdateRizky Agus MNo ratings yet
- PulmonaryDocument3 pagesPulmonaryBaha'aeddin HammadNo ratings yet
- 45 1057Document5 pages45 1057Gabriela PinticanNo ratings yet
- Echocardiographic Evaluation of Pericardial Effusion and Cardiac TamponadeDocument10 pagesEchocardiographic Evaluation of Pericardial Effusion and Cardiac TamponadeGustiTiballaNo ratings yet
- Aortic StenosisDocument11 pagesAortic StenosisIra Anuddin100% (1)
- Pulmonary Hypertension Is Prevalent in Catheter and Arterio-Venous Access HemodialysisDocument6 pagesPulmonary Hypertension Is Prevalent in Catheter and Arterio-Venous Access HemodialysisMichelle FernandoNo ratings yet
- A Rational Approach To Fluid Therapy in Sepsis: Journal Reading Dalam Bahasa InggrisDocument11 pagesA Rational Approach To Fluid Therapy in Sepsis: Journal Reading Dalam Bahasa InggrisCorey WoodsNo ratings yet
- PCP Pediatria Revision 2023Document35 pagesPCP Pediatria Revision 2023Jorge CamarilloNo ratings yet
- Background: EmbryologyDocument25 pagesBackground: EmbryologydonisaputraNo ratings yet
- Anesthesia For Non Cardiac Surgery in Children With Congenital Heart DiseaseDocument3 pagesAnesthesia For Non Cardiac Surgery in Children With Congenital Heart Diseasevenkatesh chowdaryNo ratings yet
- Review Article: Bedside Ultrasound in Resuscitation and The Rapid Ultrasound in Shock ProtocolDocument14 pagesReview Article: Bedside Ultrasound in Resuscitation and The Rapid Ultrasound in Shock ProtocolClaudioValdiviaNo ratings yet
- Eco DopplerDocument8 pagesEco DopplerClaudia IsabelNo ratings yet
- Effect of Right Ventricular Function and Pulmonary Pressures On Heart Failure PrognosisDocument7 pagesEffect of Right Ventricular Function and Pulmonary Pressures On Heart Failure PrognosisMatthew MckenzieNo ratings yet
- Cheng 2017Document6 pagesCheng 2017Lepaca KliffothNo ratings yet
- 67-Article Text-115-1-10-20171026Document5 pages67-Article Text-115-1-10-20171026Maria MiripNo ratings yet
- Cardiac ResuscitationDocument24 pagesCardiac ResuscitationPaulinaNo ratings yet
- CEN Case ReportsDocument13 pagesCEN Case Reportsvedora angeliaNo ratings yet
- Aruna Ramesh-Emergency...Document6 pagesAruna Ramesh-Emergency...Aishu BNo ratings yet
- 510732Document13 pages510732PaulHerreraNo ratings yet
- CSS 6 - Right Ventricular Failure - Dr. Pudji SP - PD-KKV - Rizky Regia Triseynesya 1815136Document16 pagesCSS 6 - Right Ventricular Failure - Dr. Pudji SP - PD-KKV - Rizky Regia Triseynesya 1815136Rizky Regia TriseynesyaNo ratings yet
- Pleural Effusions From Congestive Heart Failure: Jose M. Porcel, M.D., F.C.C.P., F.A.C.PDocument9 pagesPleural Effusions From Congestive Heart Failure: Jose M. Porcel, M.D., F.C.C.P., F.A.C.PDaniil KorzačNo ratings yet
- Kjim 2017 355Document12 pagesKjim 2017 355Carolina Aguilar OtáloraNo ratings yet
- Ehs 372Document13 pagesEhs 372Binod KumarNo ratings yet
- The Heart Rate Response Pattern To Dialysis Hypotension in Haemodialysis PatientsDocument5 pagesThe Heart Rate Response Pattern To Dialysis Hypotension in Haemodialysis PatientsAnton SampNo ratings yet
- PericarditisDocument11 pagesPericarditisjosefamdNo ratings yet
- NPT El FinalDocument40 pagesNPT El FinalSelma Alonso BuenabadNo ratings yet
- Tuberculous Pericardial EffusionDocument6 pagesTuberculous Pericardial EffusionLink BuiNo ratings yet
- Special Situations: Intradialytic Hypertension/chronic Hypertension and Intradialytic HypotensionDocument8 pagesSpecial Situations: Intradialytic Hypertension/chronic Hypertension and Intradialytic HypotensionDavid SantosoNo ratings yet
- Controlled HypotensionDocument21 pagesControlled HypotensionChristian YonathanNo ratings yet
- Idiopathic Pre-Capillary Pulmonary Hypertension in Patients With End-Stage Kidney Disease - Effect of Endothelin Receptor AntagonistsDocument9 pagesIdiopathic Pre-Capillary Pulmonary Hypertension in Patients With End-Stage Kidney Disease - Effect of Endothelin Receptor AntagonistsyuliaNo ratings yet
- Truncus ArteriosusDocument20 pagesTruncus ArteriosusjustinahorroNo ratings yet
- Ecocardiografia Monitoreo Hemodinamico en Critico..Document12 pagesEcocardiografia Monitoreo Hemodinamico en Critico..cositaamorNo ratings yet
- Case Report Cteph EditDocument13 pagesCase Report Cteph EditapekzzzzNo ratings yet
- Hemodynamic Parameters To Guide Fluid Therapy: Review Open AccessDocument9 pagesHemodynamic Parameters To Guide Fluid Therapy: Review Open AccessIrma DamayantiNo ratings yet
- Right Heart Failure A Narrative Review For Emergency CliniciansDocument8 pagesRight Heart Failure A Narrative Review For Emergency ClinicianssunhaolanNo ratings yet
- Abhay KumarDocument3 pagesAbhay KumarDr. Jatin GargNo ratings yet
- Neonatal Pericardial Effusion: Case Report and Review of The LiteratureDocument9 pagesNeonatal Pericardial Effusion: Case Report and Review of The LiteratureMarsya Yulinesia LoppiesNo ratings yet
- Coronary Arteri DiseaseDocument3 pagesCoronary Arteri DiseasetriNo ratings yet
- Atrial Septal Defect (ASD) Dan Ventricular Septal Defect (VSD)Document10 pagesAtrial Septal Defect (ASD) Dan Ventricular Septal Defect (VSD)Anis Syafa'atul HusnaNo ratings yet
- U1 The Human Body 5Document12 pagesU1 The Human Body 5Francisco RosNo ratings yet
- Cellular Respiration - ReviewerDocument3 pagesCellular Respiration - ReviewerJoyce Cañal100% (1)
- Putting Injectable Facial Fillers To Their Best Use PDFDocument4 pagesPutting Injectable Facial Fillers To Their Best Use PDFvini_tbNo ratings yet
- Fever in The Neurointensive Care UnitDocument9 pagesFever in The Neurointensive Care UnitDiayanti TentiNo ratings yet
- Summative Science 3rd QTRDocument4 pagesSummative Science 3rd QTRRosalie Tilos OritoNo ratings yet
- E Learning SensoriDocument15 pagesE Learning SensoriadnajaniNo ratings yet
- Patent Ductus ArteriosusDocument4 pagesPatent Ductus ArteriosusseigelysticNo ratings yet
- The Cell Cycle & Cell Division: BOT 1P: Lecture 5Document48 pagesThe Cell Cycle & Cell Division: BOT 1P: Lecture 5Cham RosarioNo ratings yet
- Sports, Exercise and Health Science Standard Level Paper 2: 16 Pages © International Baccalaureate Organization 2011Document16 pagesSports, Exercise and Health Science Standard Level Paper 2: 16 Pages © International Baccalaureate Organization 2011ALFREDO CASTRONo ratings yet
- Evolution of Nonsteroidal Anti-Inflammatory Drugs (Nsaids) : Cyclooxygenase (Cox) Inhibition and BeyondDocument30 pagesEvolution of Nonsteroidal Anti-Inflammatory Drugs (Nsaids) : Cyclooxygenase (Cox) Inhibition and BeyondnesakusumaNo ratings yet
- Medical Terminology and Anatomy For ICD-10 CodingDocument1 pageMedical Terminology and Anatomy For ICD-10 CodingsrdjanNo ratings yet
- LI Peak Expiratory FlowDocument3 pagesLI Peak Expiratory FlowukmppdNo ratings yet
- Hygiene and Health in Quran and ScienceDocument13 pagesHygiene and Health in Quran and Sciencehda_solo7195No ratings yet
- Informative Speech Outline LatestDocument4 pagesInformative Speech Outline LatestAzlan KinGshah II100% (2)
- Osmolarity VsDocument4 pagesOsmolarity VsSuhail Ahmed SahitoNo ratings yet
- Blood Gas ElectrodesDocument63 pagesBlood Gas Electrodeswellawalalasith0% (1)
- The Creators College of Science & Commerce: 1 TermDocument2 pagesThe Creators College of Science & Commerce: 1 TermJhangir Awan33% (3)
- Introduction To The Clinical ChemistryDocument18 pagesIntroduction To The Clinical ChemistrySasa AbassNo ratings yet
- Structure and Function of The Gas Exchange System - Respiration and Gas Exchange - KS3 Biology - BBC Bitesize - BBC BitesizeDocument1 pageStructure and Function of The Gas Exchange System - Respiration and Gas Exchange - KS3 Biology - BBC Bitesize - BBC BitesizewatchmakerparikshitNo ratings yet
- Standardized Postnatal Management of Infants With Congenital Diaphragmatic Hernia in Europe: The CDH EURO Consortium Consensus - 2015 UpdateDocument9 pagesStandardized Postnatal Management of Infants With Congenital Diaphragmatic Hernia in Europe: The CDH EURO Consortium Consensus - 2015 UpdatericardolsanchezNo ratings yet
- Hoon - Medical First Aid HandoutDocument100 pagesHoon - Medical First Aid HandoutSaptarshi BasuNo ratings yet
- C20431 07434997Document4 pagesC20431 07434997Prodigal SonNo ratings yet
- The Toxicology of MercuryDocument10 pagesThe Toxicology of MercuryworldsawayNo ratings yet
- Anatomy TermsDocument1 pageAnatomy TermsStephanie MolinaNo ratings yet
- 1000 Ico Basic MCQDocument231 pages1000 Ico Basic MCQNidia M. Quispe Rodríguez100% (3)
- Pyloric Stenosis Case StudyDocument37 pagesPyloric Stenosis Case StudyFaith Torralba100% (3)
- ECG Interpretation BookDocument57 pagesECG Interpretation BookLouis Plan100% (2)
- SOP For Anti Syphilis TP ICTDocument3 pagesSOP For Anti Syphilis TP ICTyasirNo ratings yet
- Sleep DissertationDocument5 pagesSleep DissertationHelpMeWriteMyPaperPortSaintLucie100% (1)