Professional Documents
Culture Documents
Fono 2
Uploaded by
Xiomara RodriguezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fono 2
Uploaded by
Xiomara RodriguezCopyright:
Available Formats
Military Rehabilitation
Special Issue
Clinical Reasoning and Advanced
Practice Privileges Enable Physical
Therapist Point-of-Care Decisions in
the Military Health Care System:
3 Clinical Cases
Daniel I. Rhön, Gail D. Deyle, Norman W. Gill
D.I. Rhön, PT, DPT, DSc, OCS,
FAAOMPT, Department of Physi-
cal Medicine & Rehabilitation,
Background and Purpose. Physical therapists frequently make itnportatit
Madigan Army Medical Center, poitit-of-care decisions for musculoskeletal injuries and conditions. In the Military
Fort Lewis, Washington. Mailing Health System (MHS), these decisions may occur while therapists are deployed in
address: Department of Physical support of combat troops, as well as in a more traditional hospital setting. Proficiency
Medicine & Rehabilitation, Madi-
gan Army Medical Center, Build-
with the musculoskeletal examination, including aftindamentalunderstanding of the
ing 9040, Jackson Ave, Tacoma, diagnostic role of musculoskeletal imaging, is an important competency for physical
WA 98431 (USA). Address all cor- therapists. The purpose of this article is to present 3 cases managed by physical
respondence to Dr Rhön at: therapists in unique MHS settings, highlighting relevant challenges and clinical
daniel.rhon@us.army.mil. decision making.
CD. Deyle, PT, DPT, DSc, OCS,
FAAOMPT, US Army-Baylor Uni- Case Description. Three cases are presented involving conditions where the
versity Doctoral Fellowship in physical therapist was significantly involved in the diagnosis and clinical management
Orthopaedic Manual Physical plan. The physical therapist's clinical privileges, including the ability to order appro-
Therapy, San Antonio Military
Medical Center, Fort Sam Hous-
priate musculoskeletal imaging procedures, were helpful in making clinical decisions
ton, Texas. that facilitate timely management. The cases involve patients with an ankle sprain and
Maisonneuve fracture, a radial head fracture, and a pelvic neoplasm referred through
N.W. Gill, PT, DSc, OCS,
FAAOMPT, US Army-Baylor Uni-
medical channels as knee pain.
versity Doctor of Physical Therapy
Program, Fort Sam Houston, Outcomes. CUnical pathways from point of care are discussed, as well as the
Texas. reasoning that led to decisions affecting definitive care for each of these patients. In
[Rhön DI, Deyle GD, Gill NW. Clin- each case, emergent treatment and important combat evacuation decisions were
ical reasoning and advanced prac- based on a combination of examination and management decisions.
tice privileges enable physical
therapist point-of-care decisions Discussion. Physical therapists can provide important contributions to the pri-
in the military health care system:
3 clinical cases, i^hys Ther.
mary management of patients with musculoskeletal conditions in a variety of settings
201 3;93:1234-1243.] within the MHS. In the cases described, advanced clinical privileges contributed to
the success in this role.
© 2013 American Physical Therapy
Association
Published Ahead of Print:
February 7, 2013
Accepted: February 4, 2013
Submitted: March 30, 2012
Post a Rapid Response to
this article at:
ptjournal. opta, org
1234 m Physical Therapy Volume 93 Number 9 September 201 3
Physical Therapist Point-of-Care Decisions in the Military Health Care System
P
hysical therapists often are posi- disrupt joint surfaces or produce role in guiding the diagnostic pro-
tioned to make point-of-care instability, such as Lisfranc or ankle cess and ultimate management of
management decisions within syndesmosis injuries, have a better these patients.^
their area of specialty training, most prognosis w^ith timely recognition
often musculoskeletal conditions.'"^ and early appropriate manage- In the forward operating base, the
In the Military Health System (MHS), ment."^-i** Although very uncom- front-lines environment was austere,
these management decisions can mon, neoplasms also can masquer- with limited medical resources, and
occur -while the physical therapist is ade as musculoskeletal pathology, asthe only imaging medium available
deployed in a combat support the skeletal system is a common sitewas a small mobile radiography sys-
role,'''^'^ in addition to the more tra- of metastasis for various primary tem. A computed tomography scan-
ditional hospital settings.»•"' Physicalcancers.13-23 ner w^as available in the Combat Sup-
therapists in the MHS are often the port Hospital a short fiight away,
first credentialed providers to exam- The purpose of this article is to pres- where the closest surgeon was
ine and diagnose patients with mus- ent 3 cases where physical therapists located.^'* The medical personnel in
culoskeletal conditions.*' Formal clin- in the MHS played roles in the diag- the forward operating base included
ical privileges to order basic nosis and clinical management and 2 physicians (internal medicine and
laboratory and diagnostic imaging provide insight into their decision- family medicine specialties), a phys-
studies and refer patients to the making and clinical reasoning pro- ical therapist, 2 physician's assis-
appropriate specialty clinic may
cesses. Each case illustrates a focus tants, a dentist, a nurse, and a mental
facilitate timely and cost-effective
on clinical decisions, including health provider. Although there
management of musculoskeletal inju-
ordering diagnostic musculoskeletal were trauma, mass casualty, and
ries and conditions.^'"-12
images and implementing appropri- evacuation protocols that were prac-
ate subsequent care. ticed by the medical team, none
Strong patient interview and physi- existed for the standard management
cal examination skills also can facili- of musculoskeletal injuries and con-
tate timely and accurate decisions Therapist and Environment ditions. Additionally, leaving the con-
regarding necessary additional Characteristics fines of the forward operating base
screening. Physical therapists should The physical therapist providing for a convoy to the Combat Support
carefully formulate or select each care for the first 2 patients had a Hospital was a dangerous and poten-
interview question or diagnostic test master's degree in physical therapy, tially life-threatening course of
that may provide valuable informa- 4 years of outpatient orthopedic action and had to be weighed
tion to help rule in or nile out a experience in direct access settings, accordingly in the management deci-
clinical hypothesis. 1' Most clinical and formal credentials for advanced sions. Two of these cases were cho-
decision tools used for screening and clinical privileges, including order- sen from afileof cases brought back
diagnosis have not been studied in ing musculoskeletal imaging and from a combat deployment,^ based
combat settings. Keeping this per- basic laboratory studies. These cases on their musculoskeletal imaging
spective, a blend of current best evi- occurred during a 12-month combat application.
dence and clinical experience is deployment while serving in a for-
helpftil to identify and appropriately ward operating base in Iraq, where
channel patients w^ith injuries and the physical therapist served as the
conditions requiring treatment out- musculoskeletal asset attached to a Available With
side a physical therapist's scope of mechanized infantry brigade and This Article at
practice. Examples of pathology a saw 309 unique patients (1,362 total ptjournal.apta.org
physical therapist may encounter visits) during that time frame.^ The
include tumors, infections, aortic last case was seen in a large military Listen to a special Craikcast on
abdominal aneurysnis, fractures, dis- medical treatment facility by a phys- the Military Rehabilitation Special
locations, and a variety of other sys- ical therapist with a master's degree Issue with editors John Childs and
Alice Aiken.
temic diseases. Additionally, condi- in physical therapy, 20 years of gen-
tions such as cauda equina eral and orthopedic physical therapy Audio Podcast: "Advancing the
syndrome, stress fractures of the experience, and similar clinical priv- Evidence Base in Rehabilitation
femoral neck, or compartment syn- ileges. In each of these cases, the for Military Personnel and
Veterans" symposium recorded at
drome''' may require emergent sur- physical therapist played a helpful
APTA Conference 201 3, |une 28,
gical intervention. 14 15 Injuries that 2013, in Salt Lake City, Utah.
September 2013 Volume 93 Number 9 Physical Therapy m 1235
Physical Therapist Point-of-Care Decisions in the Military Health Care System
larities and verified neurovascular
integrity. A radiographie study of the
ankle (Fig. 1) was ordered in the
trauma triage room and read verba-
tim as a "possible avulsion of medial
malleolus but otherwise unremark-
able." It was unknown whether the
Ottawa Clinical Decision Rule^^ -^^g,
used before ordering the radiograph.
He was provided crutches, a com-
pression wrap, and instmctions to
ice and elevate the ankle. Two days
later, after the swelling had slightly
subsided, he came in to see the phys-
ical therapist for additional care.
Clinical impression 1. The other-
wise healthy patient was using
crutches, tolerating partial but not
full weight bearing. Moderate joint
effusion and ecchymosis over the lat-
eral ankle were still present. The
¡physical therapist's plan was to rule
out a fracture, and if a fracture
existed, to determine whether surgi-
cal stabilization was required (w^hich
would require an evacuation out of
the country). The physical thera-
m
l")ist's differential diagnosis included
medial collateral (deltoid) or lateral
collateral ligament ankle sprain, rear-
foot or midfoot sprain (Lisfranc or
Charcot), and high ankle (syndesmo-
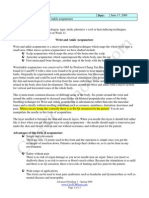
Figure 1. sis) sprain (Table). Unique consider-
Initial radiographs (lateral and anterior-posterior oblique/mortise views) taken of the ations for prognosis included the
ankle. Note the exposed area on the radiograph was below the proximal fibula. The need to ambulate on rocky terrain
hairline fracture can be seen on the medial malleolus in this image, but it is not easy to while wearing body armor (~8 kg).
detect.
The decision to consult with an
orthopedic surgeon would not be
trivial, as it required an escorted car-
Case Descriptions base for further evaluation by medi- avan of vehicles on a hostile route.
Case 1 (Maisonneuve Fracture) cal staff. He denied any low back, This patient case demonstrates some
Patient history and systems hip, or knee pain, and all of his vital unique considerations of managing a
review. A 38-year-old Hispanic signs were normal. He was not cur- patient with a musculoskeletal injury
male physician's assistant reported rently on other medications. He was in a combat environment, including
that he was on a combat foot patrol able to take 4 steps with some an assessment of resources and
in Iraq when he "stepped wrong" weight distributed on his right lower implications of clinical decisions on
and twisted his right ankle. He extremity, although he winced from ftirther care and prognosis.
reported immediate pain that pain. Upon removal of his boots,
increased with weight bearing, but there was obvious ankle effusion on Examination. The physical thera-
he was able to continue the patrol. the right compared with the left. Tlie pist used the Ottawa Ankle Rule-' to
After 30 minutes, due to increasing attending physician in the trauma screen the patient for a fracture,
pain, he was placed in a vehicle and room cleared the foot and ankle for even though a radiograph had
returned to the forward operating lacerations, "wounds, or other irregu- already been taken. The rules indi-
1236 • Physical Therapy Volume 93 Number 9 September 201 3
Physical Therapist Point-of-Care Decisions in the Military Health Care System
Table.
Clinical Reasoning Summary for All Cases
Case Differential Diagnosis Differentiation Point" Management Pian Outcome
Maisonneuve 1. Lateral collateral ligament Mechanism of injury. Sharp pain Discussion with orthopedic After 2 weeks of immobilization.
fracture ankle sprain on medial malleolus and surgeon in remote and based on minimal pain
2. Syndesmosis (high ankle) proximal fibula with location. Surgical and minimal widening with
sprain palpation. Inability to fully intervention usually proper stress views of the
3. Proximal fibula fracture bear weight in single-limb required for this ankle, the decision was made
stance due to pain. condition. Patient was to manage the fracture
evacuated out of theater nonsurgically. The patient
for surgical consideration. returned to the combat
theater 4 months later.
Radial head 1. Elbow contusion Mechanism of injury, joint Discussed with orthopedic Based on status and function of
fracture 2. Radial collateral ligament effusion, fracture-quality pain. surgeon the nature of patient on further evaluation.
sprain and inability to fully extend the fracture (articular decision was made to
3. Radial head dislocation the elbow. Fat pad sign seen surface). Based on age manage the fracture
4. Olecranon fracture on radiograph. and work demands. nonsurgically. Patient was
recommendation was able to return to theater
made to evacuate patient because the physical therapist
out of theater for surgical was able to manage him
fixation. there. By 14 weeks, patient
was able to do 10 push-ups
pain-free.
Hip neoplasm 1. Tumor: malignant or Gait indicating impaired hip Screening radiographs Same-day evaluation by
benign function with no mechanism ordered by physical orthopedic oncologist
2. Infection of injury. therapist at initial visit initiated plan for differential
3. Pelvic inflammatory Red flags: revealed aggressive diagnosis and definitive care.
disease 1. Night pain malignant process.
4. Fracture: hip or pelvis 2. Early satiation
3. Bowel changes
4. Bladder changes
5. Menstrual irregularity
Palpable fullness in the right
anterior pelvic region
" Differentiation point marks critical aspects from the examination leading to the decision to order diagnostic imaging. The results could have a significant
impact on determining the intervention plan.
cate that radiographs are necessary the lateral malleolus. Gentle ligamen- the forefoot and mid-foot joints did
only if there is any pain in the mal- tous stress tests (talar tilt and ante-not reproduce any pain. The Achilles
leolar zone along with the presence rior drawer) were inconclusive due tendon was intact, and resisted
of at least 1 of these 3 factors: (1) to pain. Additionally, their value as straight plantar flexion was not pain-
bone tenderness along the distal 6 conclusive diagnostic tests for liga- ftil. A mild forced external rotation
cm of the posterior edge of the tibia ment disruption is questionable due force'^ to the leg and foot repro-
or tip of the medial malleolus, (2) to poor duced pain in the medial and lateral
bone tenderness along the distal 6 ankle, in addition to the proximal
cm of the posterior edge of the fibula In order to provide a thorough eval- lateral leg. The medial malleolous
or lateral malleolus, or (3) inability to uation, the entirefibulawas carefully also was tender. The physical thera-
bear weight both immediately after palpated for a possible fracture and pist evaluated the radiographs taken
the injury and for at least 4 steps in compressed against the tibia as a pro- 2 days prior, but the proximal fibula
the emergency department. The sen- vocative assessment of the syndes- was not visualized in that particular
sitivity for ruling out a fracture with- mosis, suggestive of a positive test image (Fig. 1). The differential at this
out the need of a radiograph if these for syndesmotic injury (kappa= point included a syndesmosis sprain
factors are not present is 100%2'5; 0.50),-» although it should not be versus a proximal fibula fracture,
however, these rtiles have not been relied on alone for the diagnosis.^** with the potential for a concurrent
validated in a combat setting. The This intervention reproduced the medial ankle sprain or fracture. He
patient was putting partial body- patient's pain.'" Palpation to the placed the patient non-weight bear-
weight on his foot, but it caused sig- proximal fibula produced sharp ing on crutches with an immobilizer
nificant pain and discomfort. Tender- pain, even without a provocative boot and ordered repeat radiographs
ness was elicited with palpation of squeeze. Joint mobility assessment of
September 2013 Volume 93 Number 9 Physical Therapy • 1237
Physical Therapist Point of-Care Decisions in the Military Health Care System
ankle injuries should include assess-
ment of adjacent joints,^^ in this
case, careful palpation of the fib-
ula*'-^* and the bones of the foot,^*
in addition to the malleoli. The areas
above and below the area of primary
symptoms should be assessed for
less obvious injury and potentially
related or referred pain. Maison-
neuve fractures occur as a result of
an external rotation injury to the
ankle (often causing medial malleo-
lus pathology) whose force is trans-
mitted up through the interosseous
membrane, ultimately resulting in a
fracture of the proximal fibula. The
proximal fibular fracture, in isola-
tion, can in many cases be managed
nonsurgically.^"^ However, some
medial malleolar fractures and del-
toid ligament sprains may result in
Figure 2. significant ankle instability, requiring
The combination of a proximal fibular fracture (often indicating injury to the syndes- surgical fixation.^^••*'' Because of
mosis) and medial malleolus fracture can predispose the talocrural joint to significant these possible complications and the
instability and often requires surgical fixation. (A) The fracture of the medial malleolus austere medical setting, the physical
was more evident on anterior-posterior view than In the oblique (mortise) view in Figure
1. (B) Exposure of the entire leg revealed a fracture of the proximal diaphysis of the
therapist decided to have the patient
fibula. medically evacuated. Once back in
the United States, the orthopedic
surgeon decided that due to optimal
initial management and good joint
to include the proximal leg and knee of this nature without proper treat- stability, the best option was to con-
region. ment could result in greater disabil- tinue treating the fracture conserva-
ity. The diagnosis may have been tively with immobilization. Had the
Clinical impression 2. The physi- missed without the additional radio- fracture been missed originally, the
cal therapist evaluated the new graphic images of the knee and prox- patient may have displaced his frac-
images and visualized a spiral frac- imal fibula. After several weeks of ture, creating greater instability and
ture of the proximal fibula in addi- rest and proper immobilization dur- a need for surgery, leading to a lon-
tion to a fracture of the medial mal- ing the transition back to the United ger period of disability. In this case,
leolus (Fig. 2). These findings were States, the injury showed early callus optimal early management by the
consistent with the clinical examina- formation and minimal widening of physical therapist may have contrib-
tion and the diagnosis of a Maison- the mortise with proper stress imag- uted to the surgeon's decision to
neuve fracture.'* ing (radiographs and fluoroscopy). forgo surgery and return the soldier
The surgeon decided to treat the to the combat theater later that year.
Outcome. The injury had been well-positioned fracture conserva-
assessed as thoroughly as permitted tively with a short leg cast in a non- Case 2 (Radial Head Fracture)
in that clinical setting. The decision weight-bearing status for 6 additional Patient history and systems
was made to medically evacuate the weeks. review. A 21-year-old Caucasian
patient to the United States for fur- male soldier was seen by the physi-
ther evaluation by an orthopedic sur- Discussion. Maisonneuve frac- cal therapist with a complaint of
geon at a large Army hospital. The tures are easy to misdiagnose."*"•*' A right elbow pain after a fall sustained
decision, based on the rocky terrain comprehensive clinical examination while playing basketball several
and instability of the ankle from the that assesses areas above and below hours earlier. The pain was primarily
Maisonneuve fracture, was in the the area of symptoms can make mis- in the posterior-lateral elbow, and
best interest of the patient. An injury diagnosis less likely. Examination of the patient was unable to ftilly
1238 • Physical Therapy Volume 93 Number 9 September 2013
Physical Therapist Point-of-Care Decisions in the Military Health Care System
extend his elbow because of the
pain. The patient denied any symp-
toms in the neck, shoulder, or hand,
other medical issues, or prior history
of elbow injury. The soldier was 3
months into his 1-year deployment
in Iraq, hoping to remain in theater
with his unit. After initial triage in
the trauma room to rule out other
injuries, the patient was sent to the
physical therapist for a thorough
evaluation of the elbow.
Clinical impression 1. The soldier
presented with his arm in a sUng, and
he wasftiUyalert and oriented to the Figure 3.
situation. He denied hitting Ws head Mason grade II fracture: (A) anterior-posterior view with forearm in supination, (B)
or any symptoms in the wrist, shoul- anterior-posterior view with forearm in pronation, (C) lateral view. Note the value in this
der, or neck but reported his lateral case of obtaining pronation and supination views of the forearm. The views in images
elbow pain as 9/10 on the numeric B and C appear unremarkable at first glance, and the fracture is difficult to visualize. The
view in supination (A) reveals the extent of the fracture coursing across articular surface
pain rating scale. Despite the swell- of the radial head.
ing, he w^as willing to take liis arm
out of the sling, but guarded his
elbow against full elbow extension.
diminish before casting or splinting apist placed the patient in a plaster-
Examination. Gentle palpation the elbow. fabricated long-arm cast in elbow
produced intense pain on the poste- flexion and full forearm supitiation.
rior lateral aspect of the elbow. Clinical impression 2. In the
There was visible elbow effusion, absence of a radiologist or orthope- Outcome. Due to the nature of
and pain limited full elbow exten- dist, the physical therapist initially the fracture involving the articular
sion. There was neurovascular integ- evaluated the radiographs. A radial surface, the physical therapist pre-
rity of the distal forearm and hand. head fracture, later categorized as a sented the case to an orthopedic sur-
Shoulder range of motion was full Mason grade II, was identified span- geon at a larger Combat Support
and pain-free. The physical therapist ning through the articular surface Hospital using e-mail to send him the
decided to order a set of anterior- and coursing the length of the radial radiograpliic images. In this particu-
posterior and lateral view radio- head (Fig. 3).^** *' The Mason classi- lar case, the surgeon felt that surgical
graphs of the elbow in order to rule fication system for radial head frac- evaluation was appropriate; there-
out a fracture. The inability to ftilly tures is: (1) type I—nondisplaced fore, the patient was evacuated to a
extend the elbow (elbow extension fracture of the radial head; (2) type hospital outside the combat theater.
test) has been associated with a 50% II—marginal radial head fracture Ultimately, because the fracture was
likelihood of fracture.^^ Alternately, with minimal displacement, depres- minimally displaced and the patient
ftiU extension of the elbow can rule sion, or angulation; and (3) type Ill- was already showing promising signs
out a fracture with a sensitivity of comminuted radial head fracture.''" of recovery, the fracture was man-
98.4% (negative likelihood ratio of Although the reliability of the classi- aged nonsurgically in a long-arm
0.03).^^ The patient was instmcted fication system has been called into cast. The patient requested to return
to continue wearing the sling, mon- question,^y it has been shown to be to the combat theater, despite med-
itor his neurovascular status, use ice, one of the more reproducible classi- ical evacuation orders stating,
elevate the upper extremity, and fication systems (intrarater "Patient will need conservative treat-
report back the next day. The phys- kappa=0.58, interrater kappa= ment unavailable in theater due to
ical therapist reasoned that even if a 0.43-0.56).^' The patient returned his job." Subsequently, the soldier's
fracture were present (Table), it after 72 hours, reporting decreased case manager contacted the physical
would be better to wait at least 24 to pain of 0/10 at rest and 3/10 when therapist on the base in Iraq to deter-
48 hours to allow the effusion to moving the elbow. The effusion had mine whether the patient could
decreased substantially, and the ther- receive conservative care there. The
September 2013 Volume 93 Number 9 Physical Therapy • 1239
Physical Therapist Point-of-Care Decisions in the Military Health Care System
athletic activity, a specific mecha-
PI: Constant,slightly nism of injury, or a change in her
variable, fatiguing, work-related duties. She had been
deep ache to sharp
8-10/10 seen in the medical center adoles-
cent clinic on 3 occasions during the
previous month for right hip and
knee pain. The prescribed naproxen
did not provide appreciable symp-
tom relief. A contrast bowel study
performed due to her recent history
of difficult bowel movements was
unremarkable. No imaging of the pel-
P2: Intermittent intense vis, hip, or thigh had been obtained.
tingling
The referral diagnosis from the phy-
sician in the adolescent clinic was
patellar tendinitis. Her primary com-
plaint was a constant, slightly vari-
able ache to sharp pain (10/10 at
Figure 4. worst) with intermittent intense tin-
Body chart or map of patient-reported symptoms. PI represents the worst or most
gling that extended from the anterior
severe area of symptom reported by the patient. Cleared areas were determined by pelvic region distally to the anterior
touching the area and asking the patient whether she was experiencing any symptoms knee (Fig. 4). The symptoms were
in this location. Check marks indicate symptom-free areas. severe enough to keep her from get-
ting more than 1 hour of sleep per
night. Her pain was most intense
physical therapist confirmed that the range-of-motion exercises in the when squatting, lifting her leg to get
soldier's fracture could be managed physical therapy clinic. By 14 weeks, out of the car or show^er, moving her
there, and the soldier was able to there was adequate union, and the leg for braking while driving, and
return to Iraq. patient was able to complete 10 while standing to operate the cash
push-ups without pain. Ultimately, register at work. During health
Discussion. The articular surface the soldier was able to finish his screening, she indicated that she was
involvement of the radial head frac- entire deployment in Iraq. experiencing a decreased capacity
ture required evaluation by an ortho- for food, urgency and frequency of
pedic surgeon. Management of this Case 3 (Tumor Case) urination, difficulty initiating bowel
type of fracture can be conserva- Patient history and systems movements, and menstrtial irregular-
tive'*2 or surgical, depending on age review. A 21-year-old African ity. She also indicated general health
or functional demands of the American female college student changes of fatigue and malaise.
patient.''* The outcome often can be with right knee, thigh, and hip
favorable without surgery.^'' Evi- region symptoms was referred to a Clinical impression 1. The
dence for surgical versus nonsurgical physical therapist at a large MHS aca- patient/client history indicated that
care for a Mason type II radial head demic medical center. Although the injury or overuse influencing the
fracture remains inconclusive. A patient had received prior medical musculoskeletal system was not
recent systematic review showed attention for a variety of signs and likely. The onset, progression,
there was insufficient evidence from symptoms associated with her con- behavior, and severity of symptoms
which to draw firm conclusions.'" dition, the physical therapist's diag- were atypical for a musculoskeletal
After the surgeon decided on non- nostic hypothesis shifted the focus condition. Additionally, the "red
surgical treatment, the physical ther- to examining structures of the hip flags" of early satiation,^'^ consistent
apist was able to help manage the and pelvic region, inckiding radio- difficulty with bowel movements,
patient in the combat theater. At 6 graphic studies, which revealed an urinary urgency,"^ changes in men-
weeks, radiographs revealed incom- aggressive malignant neoplasm. strual regularity,**'' and general health
plete healing, so the physical thera- changes suggested the possibility of
pist transitioned to partial immobili- The patient attended college and pathology outside the musculoskele-
zation by fabricating a splint that worked nights in a convenience tal system and possibly within the
could be removed for active-assisted store. She denied regular physical or genitourinary or lower gastrointesti-
1240 • Physical Therapy Volume 93 Number 9 September 2013
Physical Therapist Point-of-Care Decisions in the Military Health Care System
nal system (Table). The physical
therapist planned a careftil examina-
tion of the pelvic region, hip, thigh,
and knee.
Examination. Her pain at rest in a
standing position was 8/10. The
patient's gait was antalgic, and she
walked on her forefoot on the pain-
ftil side with a fiexed hip and knee.
Active attempts to straighten the hip
and knee in a standing position
increased the pain to 10/10. During
supine examination, the knee could Figure 5.
Imaging of the pelvic neoplasm. (A) An anterior-posterior view radiograph of the pelvis
reach full passive extension when reveals an aggressive destructive lesion involving the right superior pubic ramus (blue
the hip was slightly flexed without arrow) and acetabulum. A Codman's reactive triangle of bone is present along the
increasing her knee pain. Knee flex- medial surface of the right ilium (yellow arrow). Residual contrast material from previous
ion was equal to the contralateral bowel study is apparent (green arrow). (B) Coronal magnetic resonance image of the
side and did not increase her pain if pelvis revealing large soft tissue tumor (black arrows), displaced bladder (orange arrow),
and femoral head (red arrow).
the hip was held stable. No ligamen-
tous instability was noted at the
knee. There were no typical signs of
infrapatellar tendinitis such as swell- ical therapist ordered an anterior- tum likely accounted for the bowel
ing or crepitus, but there was vague posterior and lateral view radio- and bladder changes and early satia-
palpation tenderness over the ante- graphic study of the pelvis, which tion the patient had experienced.
rior aspect of the infrapatellar ten- also would reveal hip structures. Ultimately, upon receiving definitive
don. By disrobing the patient to her cancer treatment, the diagnosis was
undergarments and carefully palpat- Outcome. A highly aggressive, a malignant peripheral nerve sheath
ing the pelvic region,'*^'*'^ fullness in
destructive lesion was identified on tumor,5^ a class of sarcoma.
the right anterior lateral pelvic the radiographie images involving
region was appreciated, with pain the right superior pubic ramus and Discussion. This patient presenta-
over the superior pubic ramus and right acetabulum (Fig. 5A). The mus- tion was identified as atypical by a
anterior ipsilateral hip. Hip passive culoskeletal radiologist's report physical therapist who routinely
range of motion was limited by pain stated that a Codman's triangle (a examines patients with musculoskel-
in all directions. Resisted strength triangular periosteal bone forma- etal problems. Accurately complet-
tests of the foot and ankle were 5/5, tion)" was present along the medial ing the body chart or symptom map
but those of the hip and thigh were surface of the right ilium with aggres- helped focus the examination to the
weak and painftil. sive periosteal reaction. This finding hip and pelvic region (Fig. 4). The
has been reported in other tumors of patient interview helped identify red
Clinical impression 2. Due to the the pelvis.^- The radiologist's initial fiags and changes associated with 2
atypical history, including several differential diagnosis included tel- major body systems. Tenderness at
redflags,and the abnormal examina- angietatic osteosarcoma'* and infec- the knee was most likely referred
tion findings in the pelvic and hip tion. The radiologist contacted the pain from the involved somatic struc-
region, the physical therapist physical therapist recommending a tures in the pelvic region, a well-
decided additional screening was magnetic resonance imaging (MRI) documented phenomenon.''"''"'' The
indicated. She selected an initial scan and a bone scan. The physical intense tingling may have been
screening strategy of plainfilmradio- therapist immediately notified the caused by the peripheral nerve
graphs to be followed as necessary orthopedic oncologist on call, who sheath pathology. The physical ther-
by the appropriate screening labora- contacted the patient. The subse- apist facilitated the diagnosis with a
tory studies such as an erythrocyte quent MRI study revealed a lytic thorough examination ofthe patient,
sedimentation rate<'^ and complete bone lesion that had completely including an appropriate imaging
blood cell count'" and advanced destroyed the right superior pubic screening strategy. The physical
imaging. The thigh and knee seemed ramus (Fig. 5B). A large necrotic soft therapist's credentials to order the
to be minimally involved. The phys- mass displacing the bladder and rec- appropriate musculoskeletal imaging
September 2013 Volume 93 Number 9 Physical Therapy • 1241
Physical Therapist Point-of-Care Decisions in the Military Health Care System
helped facilitate a more timely privileges, and they add to the body 11 Rhön DI. Gill NW, Teyhen D, et al. Clini-
cian perception of the impact of deployed
diagnosis. of literature describing progressive physical therapists as physician extenders
clinical practice patterns of physical in a combat environment. Mil Med. 2010;
175:305-312.
Outcomes therapists.
12 Deyle GD. Musculoskeletal imaging in
The 3 cases in this report describe physical therapist practice. / Orthop
select patient management pro- Sports Phys Ther 2005:35:708-721.
All authors provided concept/idea/project
cesses in these various clinical set- design and writing. Dr Rhön and Dr Deyle 13 Groves M, O'Rourke P, Alexander H. Clin-
tings within the MHS. Point-of-care provided the patient cases. Dr Deyle and Dr ical reasoning: the relative contribution of
identification, interpretation and hypothe-
clinical decision pathways and rele- Gill provided consultation (including review sis errors to misdiagnosis. Med Teach.
vant clinical reasoning affected of manuscript before submission). 2003:25:621-625.
definitive care for each of these The views expressed are those of the authors 14 Zaraea F, Ponzoni A, Stringari C, et al.
Lower extremit)' traumatic vascular injury
patients (Table). Urgent intervention and do not reflect the official policy of the at a level II trauma center: an analysis of
and important medical evacuation Department of the Army, the Department of limb loss risk factors and outcomes. Min-
erva Chir 2011;66:397-407.
decisions in these cases were possi- Defense, or the US Government. 15 Crowell MS, GUI NW. Medical screening
ble, in part, because of the physical DOI: 10.2522/ptj.20120148 and evacuation: cauda equina syndrome in
therapists'ftillscope of relevant clin- a combat zone./ Orthop Sports Phys Tloer.
2009:39:541-549.
ical privileges. The value of an appro- References 16 Watson TS, Shumas PS, Denker J. Treat-
priately tailored examination, com- 1 Baxter RE, Garbcr MB. Physical therapists ment of Lisfranc joint injury: current con-
bined with the skills and credentials in combat health support: reeommenda- c e p t s . / ^ O T Acad Orthop Surg. 2010:18:
tions for employment. US Army Med Dep 718-728.
to perform simple screening tests J. July-September 2004:13-19. 17 Zalavras C, Thordarson D. Ankle syndes-
such as musculoskeletal imaging 2 Childs JD, Wliitman JM, Sizer PS, et al. A motie injury. / Am Acad Orthop Surg.
when indicated, was illustrated. description of physical therapists' knowl- 2OO7;15:33O-339.
edge in managing museuloskeletal condi- 18 Sagi HC, Shah AR, Sanders RW. The func-
tions. BMC Musculoskelet Disord. 2005:6: tional consequence of syndesmotic joint
Discussion 32. malreduction at a minimum 2-year follow-
up, y Orthop Trauma. 2012:26:430-443.
Physical therapists in the MHS often 3 Garber MB. Diagnostic imaging and differ-
ential diagnosis in 2 case reports. / Orthop 19 Lakmichi MA, Jarir R, KabourJ, etal. Sci-
serve the role of musculoskeletal Sports Phys Tl:>er 2005:35:745-754. atica leading to the discovery of a renal
specialists, many times being the first 4 Garber MB, Baxter RE. Physical therapists cell carcinoma. Pan AfrMedJ. 2011:9:18.
credentialed provider to evaluate in combat health support: history and 20 Gasbarrini A, Beisse R, Fisher C, Rhines L.
rationale for army transformation (part I). Spine metastasis. Int J Surg Oncol. 2011;
and diagnose these patients.^ These US Army Med Dep J. 2004:8-12. 2011:375097.
cases illustrate examples of decision- 5 Greathouse DG, Schreck RC, Benson CJ. 21 Gonzalez MN, DiFurio MJ, Sundborg MJ,
making and clinical reasoning pro- The United States Army physical therapy Leath CA III. Undifferentiated uterine sar-
experience: evaluation and treatment of coma presenting as a pathologic liumems
cesses by physical therapists in the patients with neuromusculoskeletal disor- fracture. Mil Med. 2010:175:691-692.
MHS and augment similar reported ders. / Orthop Sports Phys Ther 1994:19:
22 Singh J, James SL. Kroon HM, et al.
261-266.
cases in this setting.•^'^•^'"-''^ The Tumour and tumour-like lesions of the
6 Moore JH, Goss DL, Baxter RE, et al. Clin- patella: a multicentre experience. Eur
year that the physical therapist ical diagnostic accuracy and magnetic res- Radiol. 2009:19:701-712.
served in Iraq was the first year that onance imaging of patients referred by
23 Damron TA, Morris C, Rougraff B, Tamu-
physical therapists, orthopaedic surgeons,
physical therapists were organically and nonorthopaedic providers. J Orthop rian R. Diagnosis and treatment of joint-
related tumors that mimic sports-related
and routinely placed within Brigade Sports Phys Ther. 2005;35:67-71.
injuries. Instr Course Lect. 2009;58:833-
Combat Teams to provide advanced 7 Rhön DI. A physical therapist experience, 847.
observation, and practice with an infantry
musculoskeletal care closer to the brigade combat team in support of Oper- 24 Bagg MR, Covey DC, Powell ET IV. Levels
point of injury (cases 1 and 2). There ation Iraqi Freedom. Mil Med. 2010;175: of medical care in the global war on ter-
442-447. rorism. / Am Acad Orthop Surg. 2006;
was little precedence for physical 14(10 Spec No.):S7-S9.
8 Davis S, Machen MS, Chang L. The bene-
therapists working at this level in the ficial relationship of the colocation of 25 Stiell IG, Greenberg GH. McKnight RD,
combat theater; however, prelimi- orthopedics and physical therapy in a et al. A study to develop clinical decision
deployed setting: Operation Iraqi Free- rules for the use of radiography in acute
nary data suggest that other mem- dom. MiVMerf. 2006:171:220-223. ankle injuries. Ann Emerg Med. 1992:21:
bers of the medical team highly value 384-390.
9 Deyle GD. Direct access physical therapy
the their musculoskeletal exper- and diagnostic responsibility: the risk-to- 26 Simon RR, Hoffman JR, Smith M. Radio-
benefit ratio. J Orthop Sports Phys Ther. graphic comparison of plain films in
tise." Future research should evalu- 2006:36:632- 634. second- and third-degree ankle sprains.
ate outcomes for military units with Am J Emerg Med. 1986:4:387-389.
10 Moore JH, McMillian DJ, Rosenthal MD,
and without physical therapists as Weishaar MD. Risk determination for 27 Wilkin EJ, Hunt A, Nightingale EJ. et al.
patients with direct access to physical Manual testing for ankle instability. Man
part of their teams. These cases therapy in military health care facilities. Ther. 2O12;17:593-596.
exemplify the potential advantages / Orthop Sports Phys Ther. 2OO5;35:674- 28 Nussbaum ED, Hosea TM, Sieler SD, et al.
678. Prospective evaluation of syndesmotic
of early involvement by physical ankle sprains without diastasis. Am J
therapists with appropriate clinical Sports Med. 2OOl;29:31-35.
1242 • Physical Therapy Volume 93 Number 9 September 2013
Physical Therapist Point-of-Care Decisions in the Military Health Care System
29 Sman AD, HUler CE, Refshauge KM. Diag- 41 Matsunaga FT, Tamaoki MJ, Cordeiro EF, 52 Peersman B, Vanhoenacker FM, Heyman S,
nostic accuracy of clinical tests for diagno- et al. Are classifications of proximal radius et al. Ewing's sarcoma: imaging features.
sis of ankle syndesmosis injury: a system- fractures reproducible? BMC Musculo- JBR-BTR. 2007:90:368-376.
atic revievif. Br J Sports Med. 2013;47: skelet Disord. 2OO9;1O:12O.
620-628. 53 Yarmish G, Klein MJ, Landa J, et al. Imag-
42 Akesson T, Herbertsson P, Josefsson PO, ing characteristics of primary osteosarco-
30 Savoie FH, Wilkinson MM, Bryan A, et al. et al. Primary nonoperative treatment of ma: nonconventional subtypes. Radio-
Maisonneuve fracture dislocation of the moderately displaced two-part fractures of graphics. 2010:30:1653-1672.
ankle, y ^fW Train. 1992;27:268-269. the radial head. / Bone Joint Surg Am.
2006:88:1909-1914. 54 Sideras PA, Castoreña F, Singh J. Simulta-
31 Lock TR, Schaffer JJ, Manoli A Jr. Maison- neous presentation in the neck and abdo-
neuve fracture: case report of' a missed 43 Kaas L, Stmijs PA, Ring D, et al. Treatment men of malignant peripheral nerve sheath
diagnosis. Ann Emerg Med. 1987;l6:805- of Mason type II radial head fractures with- tumors involving two different nerve
807. out associated fractures or elbow disloca- tracts./ Clin Neurosci. 2013:20:602-604.
.32 Slimmon D, Brukner P. Sports ankle inju- tion: a systematic review. / Hand Surg
Am. 2O12;37:1416-I421. 55 Houghton KM. Review for the generalist:
ries: assessment and management. Aust evaluation of pédiatrie hip pain. Pediatr
Fam Physician. 2010;39:18-22. 44 Herbertsson P, Josefsson PO, Hasserius R, Rheumatol Online J. 2009:7:10.
33 Taweel NR, Raikin SM, Karanjia HN, et al. Uncomplicated Mason type-II and III
fractures of the radial head and neck in 56 Lesher JM, Dreyfuss P, Hager N, et al. Hip
Alimad J. The proximal fibula should be joint pain referral patterns: a descriptive
examined in all patients with ankle injury: adults: a long-term follow-up study./Bone
Joint Surg Am. 2004;86:569-574. study. Pain Med. 2008:9:22-25.
a case series of missed maisonneuve frac-
tures. / Emerg Med. 2O13;44:e251-e255. 45 Andersen MR. Goff BA, Lowe KA, et al. 57 Zhai G, Buzzard L, Srikanth V, et al. Corre-
Use of a symptom index, CA125, and HE4 lates of knee pain in older adults: Tasma-
34 Judd DB, Kim DH. Foot fractures fre- nian older adult cohort study. Arthritis
quently misdiagnosed as ankle sprains. Am to predict ovarian cancer. Gynecol Oncol.
Rheum. 2006:35:264-271.
Fam Physician. 2002;66:785-794. 2010; 116:378-383.
46 Humphrey L, Arbuckle R, Moldwin R, 58 Hetsroni 1, Weigl D. Referred knee pain in
35 Stufkens SA, van den Bekerom MP, Doorn- posterior dislocation ofthe hip. Clin Pedi-
berg JN, et al. Fvidence-based treatment of et al. The bladder pain/interstitial cystitis
symptom score: development, validation, atr (Phila). 2006:45:93-95.
Maisonneuve iricvares.J Foot Ankle Surg.
2011;50:62-67. and identification of a cut score. Eur Urol. 59 Klian AM, McLoughlin E, Giannakas K,
2012;6l:271-279. et al. Hip osteoarthritis: where is the pain?
36 Babis GC, Papagelopoulos PJ. Tsarouchas Ann R Coll Surg Engl 2004:86:119-121.
J, et al. Operative treatment for Maison- 47 Brakner P, Bennell K. Stress fractures in
neuve fracture of the proximal fibula. female athletes: diagnosis, management 60 Croweü MS, Tragord BS, Taylor AL, Deyle
Orthopedics 2000;23:687- 690. and rehabilitation. Sports Med. 1997;24: GD. Integration of critically appraised top-
419-429. ics into evidence-based physical therapist
37 Appelboam A, Reuben AD. Benger JR. practice. J Orthop Sports Phys Ther. 2012:
et al. Elbow extension test to rule out 48 Noakes TD, Smith JA, Lindenberg G, Wüls
CE. Pelvic stress fractures in long distance 42:870-879.
elbow fracture: multicentre, prospective
validation and observational study of diag- ranners. Am J Sports Med. 1985;13:120- 61 Hair LC, Deyle GD. Eosinophilic granu-
nostic accuracy in adults and children. 123. loma in a patient with hip pain. / Orthop
BMJ. 2008;337:a2428. 49 Watson J, Round A, Hamilton W. Raised Sports Phys Ther. 2011:41:119.
38 Doornberg J, Eisner A, Kloen P, et al. inflammatory markers. BMJ. 2012:344: 62 Jordan CL, Rlion DL Differential diagnosis
Apparently isolated partial articular frac- e454. and management of ankylosing spondylitis
tures of the radial head: prevalence and 50 Tefferi A, Hanson CA, Inwards DJ. How to masked as adhesive capsulitis: a resident's
reliability of radiographically diagnosed interpret and pursue an abnormal com- case problem. / Orthop Sports Phys Ther.
displacement. / Shoulder Elbow Surg. plete blood cell count in adults. Mayo 2012:42:842-852.
2007:16:603-608. Clin. 2005:80:923-936. 63 Ryder M, Deyle GD. Differential diagnosis
39 lannuzzi NP, Leopold SS. In brief: the 51 Kim-Gavino C, Lomasney LM, Demos TC, of fibular pain in a patient with a history of
Mason classification of radial head frac- Ryan D. Wliat's your diagnosis: aggressive breast cancer. / Orthop Sports Phys Ther.
tures. Clin Orthop Relat Res. 2012;470: periosteal reaction and Codman's triangle 2009:39:230.
1799-1802. marginal to an osteosarcoma of distal 64 Miller JM, Svoboda SJ, Gerber JP. Diagnosis
40 Mason ML. Some observations on fractures femur. Orthopedics. 2006;29:382, 459- of an isolated posterior malleolar fracture
of the head of the radius with a review of 463. in a young female military cadet: a resident
one hundred cases. Br J Surg. 1954;42: case report. Int J Sports Phys Ther. 2012:
123-132. 7:167-172.
September 201 3 Volume 93 Number 9 Physical Therapy • 1243
Copyright of Physical Therapy is the property of American Physical Therapy Association and
its content may not be copied or emailed to multiple sites or posted to a listserv without the
copyright holder's express written permission. However, users may print, download, or email
articles for individual use.
You might also like
- E3 - Tennis Elbow OPDocument3 pagesE3 - Tennis Elbow OPAnonymous qX3Ktq6No ratings yet
- Clinical Desision in Therapeutik ExerciseDocument335 pagesClinical Desision in Therapeutik ExerciseBrina BeBe Ifakristina100% (3)
- Astm D4910-02Document4 pagesAstm D4910-02Saqib GhafoorNo ratings yet
- (IPD A) Prelims and Midterms Compilation (KMT)Document8 pages(IPD A) Prelims and Midterms Compilation (KMT)Joshua MandaweNo ratings yet
- Soccer Exercise Library PDFDocument89 pagesSoccer Exercise Library PDFBruno Oliveira Do Nascimento100% (1)
- Ortho Survival GuideDocument28 pagesOrtho Survival GuideAmir AliNo ratings yet
- Theraband Exercise ManualDocument22 pagesTheraband Exercise Manualnoonoons100% (10)
- Upload 5Document9 pagesUpload 5umair muqriNo ratings yet
- Upload 1Document10 pagesUpload 1umair muqriNo ratings yet
- 1 s2.0 S0031940610001100 MainDocument11 pages1 s2.0 S0031940610001100 MainkkkjaegiNo ratings yet
- Article 2Document12 pagesArticle 2umair muqriNo ratings yet
- Optimizing Health Before Elective Thoracic Surgery: Systematic Review of Modifiable Risk Factors and Opportunities For Health Services ResearchDocument18 pagesOptimizing Health Before Elective Thoracic Surgery: Systematic Review of Modifiable Risk Factors and Opportunities For Health Services ResearchEva GarciaNo ratings yet
- Childs 2004 - Proposal of A Classi Cation System For Patients With Neck PainDocument15 pagesChilds 2004 - Proposal of A Classi Cation System For Patients With Neck PainRogéria RibeiroNo ratings yet
- Articles 1Document9 pagesArticles 1mk78_inNo ratings yet
- Changing Our Diagnostic Paradigm Part II Movement System Diagnostic ClassificationDocument11 pagesChanging Our Diagnostic Paradigm Part II Movement System Diagnostic ClassificationSandro PerilloNo ratings yet
- 9 FullDocument15 pages9 FulllipemagalhaesNo ratings yet
- ARTG - 2011 - PT Practice in Acute Care SettingDocument14 pagesARTG - 2011 - PT Practice in Acute Care SettingSM199021No ratings yet
- Articulo FisioterapiaDocument10 pagesArticulo FisioterapiaMonica LopezNo ratings yet
- Sports Participation by Athletes With CVDDocument4 pagesSports Participation by Athletes With CVDhearthurNo ratings yet
- Shoulder Pain of Spinal Source in The Military - A Case SeriesDocument7 pagesShoulder Pain of Spinal Source in The Military - A Case SeriesLee SmithNo ratings yet
- The Effectiveness of Manual Physical Therapy and Exercise For Mechanical Neck Pain - A Randomized Clinical TrialDocument8 pagesThe Effectiveness of Manual Physical Therapy and Exercise For Mechanical Neck Pain - A Randomized Clinical TrialHarshoi KrishannaNo ratings yet
- Original Research: Intensive Care Unit Structure Variation and Implications For Early Mobilization PracticesDocument12 pagesOriginal Research: Intensive Care Unit Structure Variation and Implications For Early Mobilization Practicesandi kurniawanNo ratings yet
- Primer: History and Examination in The Assessment of Musculoskeletal ProblemsDocument8 pagesPrimer: History and Examination in The Assessment of Musculoskeletal ProblemsNikkaFlorenceTanNo ratings yet
- Arthroscopic Surgery or Physical Therapy For Patients With Femoroacetabular Impingement SyndromeDocument9 pagesArthroscopic Surgery or Physical Therapy For Patients With Femoroacetabular Impingement SyndromeEricNo ratings yet
- Cancer Rehabilitation AssessmentDocument21 pagesCancer Rehabilitation AssessmentLiliana Carolina Guzman RiosNo ratings yet
- The Implementation of Therapeutic Alliance in The RehabilitationDocument13 pagesThe Implementation of Therapeutic Alliance in The RehabilitationniekoNo ratings yet
- Caldwell CAVan Dillen LRetal JOSPT2007Document14 pagesCaldwell CAVan Dillen LRetal JOSPT2007camila hernandezNo ratings yet
- Work-Related Musculoskeletal Disorders Among Physical TherapistsDocument9 pagesWork-Related Musculoskeletal Disorders Among Physical TherapistsDr. SheikhNo ratings yet
- Medical and Cardiac Risk Stratification and Exercise Prescription in Persons With CancerDocument7 pagesMedical and Cardiac Risk Stratification and Exercise Prescription in Persons With CancermarciarigaudNo ratings yet
- Fusion of The Lumbar Spine. A Consideration of The IndicationsDocument12 pagesFusion of The Lumbar Spine. A Consideration of The IndicationsCristina Galvez PerezNo ratings yet
- Postsurgical Physical Therapy Management of.16OledzkaSuhr2017Document8 pagesPostsurgical Physical Therapy Management of.16OledzkaSuhr2017naeemullahNo ratings yet
- Eccentric Overload Training in Patients With Chronic Achilles Tendinopathy A Systematic ReviewDocument6 pagesEccentric Overload Training in Patients With Chronic Achilles Tendinopathy A Systematic ReviewOscar NgNo ratings yet
- 166-Article Text-300-1-10-20190603Document4 pages166-Article Text-300-1-10-20190603Achmad JunaidiNo ratings yet
- 2021 Indicação para o Dry NeedlingDocument8 pages2021 Indicação para o Dry NeedlingRafel FisioNo ratings yet
- Clinical Policy For The Initial Approach To Patients Presenting With A Chief Complaint of Seizure Who Are Not in Status EpilepticusDocument19 pagesClinical Policy For The Initial Approach To Patients Presenting With A Chief Complaint of Seizure Who Are Not in Status EpilepticusVivin KarlinaNo ratings yet
- Musculosketal Imaging in Physical TherapyDocument14 pagesMusculosketal Imaging in Physical TherapyWasemBhatNo ratings yet
- Systematic ReviewDocument7 pagesSystematic ReviewErwin WibowoNo ratings yet
- Final Article 310Document8 pagesFinal Article 310NoahPintoNo ratings yet
- American Medical Society For Sports MedicineDocument13 pagesAmerican Medical Society For Sports MedicineAlvaroNo ratings yet
- Review Article: Best Practice Management of Neck Pain in The Emergency Department (Part 6 of The Musculoskeletal Injuries Rapid Review Series)Document19 pagesReview Article: Best Practice Management of Neck Pain in The Emergency Department (Part 6 of The Musculoskeletal Injuries Rapid Review Series)Eduardo BarreraNo ratings yet
- 2016 - Optimal Perioperative Management of The Geriatric PatientDocument18 pages2016 - Optimal Perioperative Management of The Geriatric PatientruthchristinawibowoNo ratings yet
- Closed-Reduction Techniques For Glenohumeral-, Patellofemoral-, and Interphalangeal-Joint DislocationsDocument11 pagesClosed-Reduction Techniques For Glenohumeral-, Patellofemoral-, and Interphalangeal-Joint DislocationsNovita AngelyNo ratings yet
- Delitto 1995Document16 pagesDelitto 1995Raúl BrizuelaNo ratings yet
- Adult Physiatric History and ExaminationDocument11 pagesAdult Physiatric History and Examinationsylschebe22gmailNo ratings yet
- Mohr PDFDocument8 pagesMohr PDFyulione vickyNo ratings yet
- Moore 2019Document5 pagesMoore 2019Tania salais obregonNo ratings yet
- AC Joint InjuryDocument13 pagesAC Joint InjuryFarhan JustisiaNo ratings yet
- The Influence of Timing of Surgical Decompression For Acute Spinal Cord Injury - A Pooled Analysis of Individual Patient DataDocument10 pagesThe Influence of Timing of Surgical Decompression For Acute Spinal Cord Injury - A Pooled Analysis of Individual Patient DataballroomchinaNo ratings yet
- Pincus 2006Document9 pagesPincus 2006Claudio Andrés Olmos de AguileraNo ratings yet
- Gebremariam 2013Document9 pagesGebremariam 2013Jailson CamposNo ratings yet
- Pain - Assessment JE DWDocument8 pagesPain - Assessment JE DWAshesh DahalNo ratings yet
- Rehab After Shoulder SurgeryDocument11 pagesRehab After Shoulder Surgerymarcelogascon.oNo ratings yet
- 2014 Article 3495Document7 pages2014 Article 3495cogajoNo ratings yet
- Pi Is 1556370715000784Document7 pagesPi Is 1556370715000784Guillermo HuertaNo ratings yet
- Ijspt 14 564Document18 pagesIjspt 14 564WaterfloNo ratings yet
- FritzDocument12 pagesFritzvalentinaro73No ratings yet
- Early Intensive Care Unit Mobility Therapy in The Treatment of Acute Respiratory FailureDocument6 pagesEarly Intensive Care Unit Mobility Therapy in The Treatment of Acute Respiratory FailureTakashi NakamuraNo ratings yet
- A Blinded, Randomized, Controlled Trial Assessing Conservative Management Strategie - 20170730120051Document8 pagesA Blinded, Randomized, Controlled Trial Assessing Conservative Management Strategie - 20170730120051sebafigueroa94No ratings yet
- BMC Musculoskeletal Disorders: Diagnosis and Treatment of Musculoskeletal Chest Pain: Design of A Multi-Purpose TrialDocument10 pagesBMC Musculoskeletal Disorders: Diagnosis and Treatment of Musculoskeletal Chest Pain: Design of A Multi-Purpose TrialMuhammad Afiq JNo ratings yet
- Physical Restraint Use in Adult Patients Presenting To A General Emergency DepartmentDocument10 pagesPhysical Restraint Use in Adult Patients Presenting To A General Emergency DepartmentBeatrizNo ratings yet
- Evaluation of Outcomes in Patients Following Surgical Treatment of Chronic Exertional Compartment Syndrome in The LegDocument9 pagesEvaluation of Outcomes in Patients Following Surgical Treatment of Chronic Exertional Compartment Syndrome in The LegAnonymous kdBDppigENo ratings yet
- Research ReportDocument12 pagesResearch ReportarlindoeliasNo ratings yet
- Spinal Cord InjuryDocument6 pagesSpinal Cord InjuryAngela ValeroNo ratings yet
- Terzic, A., Moore, R. L. y Waldman, S. A. (2007) - Cardioprotección Adquirida e Innata.Document2 pagesTerzic, A., Moore, R. L. y Waldman, S. A. (2007) - Cardioprotección Adquirida e Innata.Luis ReyNo ratings yet
- 2010 CHEST - CURVES Mnemonic Medical Decision Making CapacityDocument7 pages2010 CHEST - CURVES Mnemonic Medical Decision Making CapacityMarcelo Viana PsiquiatraNo ratings yet
- Damage Control Resuscitation: Identification and Treatment of Life-Threatening HemorrhageFrom EverandDamage Control Resuscitation: Identification and Treatment of Life-Threatening HemorrhagePhilip C. SpinellaNo ratings yet
- NURS02-Assessment of The Musculoskeletal SystemDocument129 pagesNURS02-Assessment of The Musculoskeletal SystemAlec AnonNo ratings yet
- Fracture Classification and Eponym Fractures: Supervisor: DR SyarifahDocument56 pagesFracture Classification and Eponym Fractures: Supervisor: DR SyarifahNurul AshikinNo ratings yet
- Smart Phones ErgonomicsDocument12 pagesSmart Phones ErgonomicsAnonymous F1eDbwN0t100% (1)
- Spinal Cord Injury - Physical Therapy ManagementDocument86 pagesSpinal Cord Injury - Physical Therapy Managementphysiovipin96% (70)
- Rajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaDocument9 pagesRajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaNavin ChandarNo ratings yet
- John BrzenkDocument22 pagesJohn BrzenkTom HillNo ratings yet
- Archery Form HandbookDocument13 pagesArchery Form Handbooklovakfaszat100% (1)
- Anatomy Shelf NotesDocument34 pagesAnatomy Shelf Notessmian08No ratings yet
- Effect of Physiotherapy Rehabilitation On Volkmann Ischemic Contracture-A Case StudyDocument2 pagesEffect of Physiotherapy Rehabilitation On Volkmann Ischemic Contracture-A Case StudyIntan HaddadNo ratings yet
- BANDAGING Powerpoint 1Document30 pagesBANDAGING Powerpoint 1Maria Eloisa Junelle O. Nacawili0% (1)
- Shoulder Exam ChecklistDocument2 pagesShoulder Exam ChecklistJaymin BhattNo ratings yet
- EMRA SportsMedicine Splint GuideDocument4 pagesEMRA SportsMedicine Splint Guidehppyduck32No ratings yet
- Translated Russian To English (Topography Anatomy)Document110 pagesTranslated Russian To English (Topography Anatomy)Harjun SinghNo ratings yet
- c2 Training v2Document253 pagesc2 Training v2cscswimmer227No ratings yet
- Conventional Radiology in Rheumatoid ArthritisDocument26 pagesConventional Radiology in Rheumatoid ArthritisDanNo ratings yet
- Chest and Shoulder ExerciseDocument17 pagesChest and Shoulder ExerciseLeilaThereseNo ratings yet
- 20 Essential Exercises For Bigger BicepsDocument102 pages20 Essential Exercises For Bigger BicepszainNo ratings yet
- RA1Document19 pagesRA1Ioana Omnia OkamNo ratings yet
- Figure Sculpting Tutorial ZbrushDocument10 pagesFigure Sculpting Tutorial ZbrushAfin Tulus N100% (5)
- BreastDocument2 pagesBreastJaily O. MarianoNo ratings yet
- Class 9 and 10 - Wrist and Ankle AcupunctureDocument13 pagesClass 9 and 10 - Wrist and Ankle Acupunctureg23164100% (4)
- RestraintsDocument47 pagesRestraintsDr. Jayesh PatidarNo ratings yet
- PE10 - q4 - CLAS3 - Cheerdancing and Contemporary Dance (Engages in Moderate To Vigorous Physical Activities) (For QA) - XANDRA MAY ENCIERTODocument11 pagesPE10 - q4 - CLAS3 - Cheerdancing and Contemporary Dance (Engages in Moderate To Vigorous Physical Activities) (For QA) - XANDRA MAY ENCIERTOPrincess Irish Daryll DiegoNo ratings yet
- HandDocument95 pagesHandAsad noor mirzaNo ratings yet