Professional Documents
Culture Documents
Antihistamines Used During Pregnancy 2012
Uploaded by
SRINIVASOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antihistamines Used During Pregnancy 2012
Uploaded by
SRINIVASCopyright:
Available Formats
[Downloaded free from http://www.jpharmacol.com on Tuesday, September 24, 2019, IP: 103.79.168.
143]
Mini Review
A review of antihistamines used during pregnancy
Sumit Kar, Ajay Krishnan, Preetha K., Atul Mohankar
Department of Dermatology, Venereology and Leprosy, Mahatma Gandhi Institute of Medical Sciences, Sewagram, Wardha, Maharashtra,
India
ABSTRACT
Antihistamines are one of the most common drugs that are used extensively in various dermatological and
nondermatological conditions. The use of H-1-antihistamines during pregnancy has been very controversial
due to possible teratogenic effects of these drugs. None of the antihistamines available today have been
categorized as safe during pregnancy. Control studies are available for certain first generation drugs regarding
their safety in pregnancy, but the newer agents require further studies to be declared safer in pregnancy. A
few drugs are comparatively safer to use in pregnancy than others. Every drug used in pregnancy carries a
risk for teratogenicity and careful risk/benefit assessment should be done before prescribing them.
Key words: Gestation, histamine antagonist, teratogenicity
INTRODUCTION teratogenic effect on the fetus. If a drug is consumed during
the first trimester, it can result in severe structural fetal
Pruritus is one of the most common dermatological symptoms in malformations and in the later part of pregnancy it can result
pregnancy.[1] Pruritus in pregnancy has always been challenging in various functional defects or growth disorders and can also
to the treating physician both in diagnosis and treatment. Pruritus lead to minor malformations. Drugs taken during the pregnancy
occurs due to various causes, and it can occur any time during can also lead to after effects in the neonatal and infancy period.
pregnancy. Causes for pruritus in pregnancy are numerous All pharmacological interventions are generally avoided
ranging from specific dermatoses of pregnancy to various during pregnancy due to the alarming information present in
dermatological conditions such as atopic dermatitis, urticarial, the patient information leaflet and also on the drug envelopes.
infections, and infestations or drug induced. In addition to these, The physician has to weigh the benefits of the treatment against
various systemic diseases can also manifest with pruritus. Other the potential teratogenic effects before using any drug during
than itching antihistamines are also used for various allergic pregnancy.
diseases and also used for emesis during pregnancy. Allergies
can occur in about 20–30% of women during pregnancy.[2] Among the drugs prescribed during pregnancy, antihistamines
are one of the commonest, either as an antipruritic agent or
Any drug taken during the pregnancy has a potential an antiemetic agent.[3] Many a times the patient procures these
agents as an over the counter preparation and uses it. Various
Access this article online
studies on the use of antihistamines (H1 blockers) during
Quick Response Code:
pregnancy, including a meta-analysis of more than 200,000
Website: women shows no increase in the teratogenic risk of these drugs
www.jpharmacol.com
in the humans. [3-6] Certain animal studies with hydroxyzine,
cyclizine, and promethazine have shown teratogenic effects,
DOI: but no human teratogenicity reports have so far been reported.
10.4103/0976-500X.95503 Drugs such as dexchlorpheniramine and alimemazine
(trimeprazine) were not found to have any teratogenic effect
Address for correspondence:
Sumit Kar, Department of Dermatology, Venereology and Leprosy, Mahatma Gandhi Institute of Medical Sciences, Sewagram,
Wardha 442 102, Maharashtra, India. E-mail: karmgims@gmail.com
Journal of Pharmacology and Pharmacotherapeutics | April-June 2012 | Vol 3 | Issue 2 105
[Downloaded free from http://www.jpharmacol.com on Tuesday, September 24, 2019, IP: 103.79.168.143]
Kar, et al.: Antihistamines in pregnancy
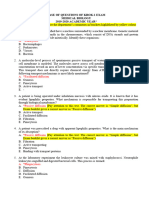
even in animal studies. None of the antihistamines has been so Table 1: FDA pregnancy category classification
far declared safe during the pregnancy by FDA on the basis for the first-generation antihistamines
of controlled animal or human studies.[7] Isolated reports Drug name Pregnancy category
of antihistamines causing congenital malformations have Chlorpheniramine B
been reported, but they warrant further investigations and Cyproheptadine B
interpretation.[6,8,9] Dexchlorpheniramine B
Hydroxyzine C
Classification of antihistamines Promethazine C
Tripelennamine B
h1-antihistamines are classified into the first generation
sedating antihistamines and the second generation nonsedating
antihistamines. Table 2: FDA pregnancy category classification
for second-generation antihistamines[10]
The first generation antihistamines include drugs such Drug name Pregnancy category
Cetirizine B
as diphenhydramine, cyproheptadine, promethazine,
Fexofenadine C
chlorpheniramine, and hydroxyzine. They have a very potent
Loratidine B
effect with high lipophilicity but are short acting. They are Levocetrizine B
metabolized in the liver by the microsomal cytochrome Desloratidine C
P-450 system. The common side effects of this category of
antihistamines include sedation and anticholinergic effects— Loratadine had previously been proposed as a possible factor
dryness of the mouth, blurring of vision, constipation and for the increased incidence of hypospadiasis in infants born
urinary retention. FDA has categorized the first generation to mothers who had taken loratadine during pregnancy.[12]
antihistamines according to the pregnancy complications However, recent studies have ruled out this possibility and
[Table 1]. [10] Promethazine and hydroxyzine have been suggest that this agent does not represent a major teratogenic
categorized as pregnancy category C due to lack of well- risk.[13,14] However, loratadine is still considered as a category
controlled studies in human being. Michigan Medicaid Birth B drug by FDA.
Defects study has linked hydroxyzine to cleft palate in new
borns.[11] Safety of antihistamines during pregnancy
Although pruritus is not a life-threatening medical condition,
Pregnancy category B means the drug has failed to demonstrate it can be extremely troublesome for pregnant women. Because
a risk to the fetus in animal reproduction studies and there of potential effects on the fetus, the treatment of pruritus in
is a lack of well-controlled studies in pregnant women or pregnancy requires prudent consideration. At one point, the
animal studies have shown an adverse effect, but adequate physician will have to use the antihistamines and weigh the
and well-controlled studies in pregnant women have failed benefits against the teratogenic effects of the antihistamines.
to demonstrate a risk to the fetus in any trimester. Pregnancy Physicians must decide whether to select an older, better-
category C means that animal reproduction studies have studied antihistamine, thought to be relatively safe during
shown an adverse effect on the fetus and there are no adequate pregnancy, or a newer agent that has less adverse effect on
and well-controlled studies in humans, but potential benefits quality of life but has a potential teratogenic effect.[9]
may warrant the use of the drug in pregnant women despite
potential risks. Various recommendations and studies favor the use of first
generation antihistamines for use during pregnancy.[15] They
The second generation antihistamines include drugs such point out that these antihistamines were in use for a longer period
as loratadine, fexofenadine, cetirizine, and azelastine. They of time and were more widely used during pregnancy. More data
have a high therapeutic index, with highly selective actions are available about the various effects of the first generation
and are nonsedating. They are long acting, but are poorly antihistamines in pregnancy.[16,17] Moreover a few of the second
lipophilic and hence have no entry to the central nervous generation agents have been reported to be associated with an
system. Side effects of the second generation antihistamines increased incidence of certain congenital malformations.[13]
include photosensitivity, tachycardia, and prolongation of the
Q–T interval. FDA has categorized the second generation In 1993, the National Asthma Education and Prevention
antihistamines as shown in [Table 2]. Fexofendine and Program (NAEPP) Working Group on Asthma and Pregnancy
desloratidine have been classified as pregnancy category C. recommended the first-generation agents chlorpheniramine
Reduction in pup weight and survival were observed with and tripelennamine as the antihistamines of choice during
fexofenadine. There are no human data on fexofenadine and pregnancy, based on duration of availability as well as
loratadine for them to be categorized as safe during pregnancy. reassuring animal and human data.[18]
106 Journal of Pharmacology and Pharmacotherapeutics | April-June 2012 | Vol 3 | Issue 2
[Downloaded free from http://www.jpharmacol.com on Tuesday, September 24, 2019, IP: 103.79.168.143]
Kar, et al.: Antihistamines in pregnancy
The Allergic Rhinitis and Its Impact on Asthma (ARIA) should be the first choice of agents. The patient should also be
guidelines, published in 2001, concluded that the older advised to drink plenty of water when taking antihistamines
antihistamines have an overall unfavorable risk/benefit ratio, during pregnancy to overcome the anticholinergic side effects.
even in the nonpregnant population, because of their poor They should also be advised to take immediate gynecological
selectivity and their sedative and anticholinergic effects.[19] consultation if they find any change in the frequency of baby’s
ARIA recommends that where possible, first-generation movement or increased contractions after taking the drugs.
antihistamines should no longer be prescribed. In general,
second-generation antihistamines are more potent, have a If a second generation agent has to be used then loratadine
longer duration of action, and produce minimal sedation. or cetirizine should be preferred as they have been widely
studied for possible teratogenic effects and have been found
The American College of Obstetricians and Gynecologists to be nonteratogenic till date. Both these agents are pregnancy
(ACOG) and The American College of Allergy, Asthma and category B agents. Second generation agents are preferably used
Immunology (ACAAI) have recommended chlorpheniramine after the first trimester if it has to be and preferably avoided in
and tripelennamine as the antihistamines of choice for pregnant the early pregnancy when organogenesis takes place.
women.[20] They also recommend cetirizine and loratadine
after the first trimester in patients who cannot tolerate or To conclude first generation antihistamines such as
do not respond to maximal doses of chlorpheniramine or chlorpheniramine, hydroxyzine, and dexchlorpheniramine
tripelennamine. are the safest among antihistamines to be used in pregnancy.
Other studies suggest that there is insufficient evidence to
REFERENCES
support the first-line use of cetirizine and loratadine during
pregnancy and recommend first considering chlorpheniramine, 1. Black MM, McKay M, Braude PR. Color atlas and text of obstetric and
tripelennamine, or hydroxyzine if an antihistamine is needed gynecologic dermatology. 2nd ed. London: Times Mirror International
Publishers Limited; 2001.
during pregnancy.[21] 2. Keleş N. Treatment of allergic rhinitis during pregnancy. Am J Rhinol
2004;18:23-8.
3. Stephansson O, Granath F, Svensson T, Haglund B, Ekbom A, Kieler H.
CONCLUSION AND RECOMMENDATIONS Drug use during pregnancy in Sweden - assessed by the Prescribed Drug
Register and the Medical Birth Register. Clin Epidemiol 2011;3:43-50.
In every pregnant case with pruritus the basic cause of pruritus 4. Seto A, Einarson T, Koren G. Pregnancy outcome following first trimester
exposure to antihistamines: meta-analysis. Am J Perinatol 1997;14:119-24.
should first be sought out before starting the antihistamines. 5. Weber-Schoendorfer C, Schaefer C. The safety of cetirizine during pregnancy.
Appropriate investigations should also be done. Before any A prospective observational cohort study. Reprod Toxicol 2008;26:19-23.
medication is taken during pregnancy, the doctor and patient 6. Gilboa SM, Strickland MJ, Olshan AF, Werler MM, Correa A. Use of
antihistamine medications during early pregnancy and isolated major
should have a risk/benefit discussion. The patient should malformations. Birth Defects Res A Clin Mol Teratol 2009;85:137-50.
be explained the fact that though no definite teratogenic 7. Lis-Swiety AD, Brzezinska-Wcislo LA. [The safety of the antihistamines in
effects have been reported to be associated with the intake dermatoses of pregnancy]. Wiad Lek 2006;59:89-91.
8. Kallen B. Use of antihistamine drugs in early pregnancy and delivery
of antihistamines in pregnancy, they are not licensed by the outcome. J Matern Fetal Neonatal Med 2002;11:146-52.
FDA as category A or the safe group. Also it is important 9. Schatz M. H1-antihistamines in pregnancy and lactation. Clin Allergy
to mention that in India no definitive guidelines have been Immunol 2002;17:421-36.
10. Meadows M. Pregnancy and the drug dilemma. FDA Consumer Magazine,
given or followed by the government to prevent the use of
Washington, D.C., U.S. Food and Drug Administration, May-June, 2001.
H1-antihistamines as over the counter medicines. Even for 11. Tang Y, Ma CX, Cui W, Chang V, Ariet M, Morse SB, et al. The risk of
prescription purposes, no definitive guidelines have been birth defects in multiple births: a population-based study. Matern Child
given by the government and practitioners generally follow Health J 2006;10:75-81.
12. Pedersen L, Norgaard M, Skriver MV, Olsen J, Sorensen HT. Prenatal
the FDA criteria. exposure to loratadine in children with hypospadias: a nested case-control
study within the Danish National Birth Cohort. Am J Ther 2006;13:320-4.
If possible the pruritus and other allergic manifestations in 13. Diav-Citrin O, Shechtman S, Aharonovich A, Moerman L, Arnon J,
Wajnberg R, et al. Pregnancy outcome after gestational exposure to loratadine
the first trimester of pregnancy should be managed using or antihistamines: a prospective controlled study. J Allergy Clin Immunol
topical medications like bland emollients and systemic 2003;111:1239-43.
antihistamines should be avoided as none of the antihistamines 14. Centers for Disease Control and Prevention (CDC). Evaluation of
an association between loratadine and hypospadias United States, 1997-
are categorized as safe by the FDA and in India no specific
2001. MMWR Morb Mortal Wkly Rep. 2004;53:219-21.
guidelines exist regarding their use in pregnancy.[10] Preferably 15. So M, Bozzo P, Inoue M, Einarson A. Safety of antihistamines during
all drug usage including antihistamines should be deferred in pregnancy and lactation. Can Fam Physician 2010;56:427-9.
the first trimester. If antihistamines have to be prescribed then 16. Buhimschi CS, Weiner CP. Medications in pregnancy and lactation: Part
2. Drugs with minimal or unknown human teratogenic effect. Obstet
first generation agents should be preferred and among them Gynecol 2009;113:417-32.
chlorpheniramine, dexchlorpheniramine and hydroxyzine 17. Gilbert C, Mazzotta P, Loebstein R, Koren G. Fetal safety of drugs used in
Journal of Pharmacology and Pharmacotherapeutics | April-June 2012 | Vol 3 | Issue 2 107
[Downloaded free from http://www.jpharmacol.com on Tuesday, September 24, 2019, IP: 103.79.168.143]
Kar, et al.: Antihistamines in pregnancy
the treatment of allergic rhinitis: a critical review. Drug Saf 2005;28:707-19. American College of Obstetricians and Gynecologists (ACOG) and The
18. Asthma and Pregnancy Report. NAEPP Report of the Working Group on American College of Allergy, Asthma and Immunology (ACAAI). Ann
Asthma and Pregnancy: Management of Asthma During Pregnancy. NIH Allergy Asthma Immunol 2000;84:475-80.
Publication No. 93-3279. Bethesda, MD: U.S. Department of Health and 21. Gilbert C, Mazzotta P, Loebstein R, Koren G. Fetal safety of drugs used in
Human Services; National Institutes of Health; National Heart, Lung, the treatment of allergic rhinitis: a critical review. Drug Saf 2005;28:707-19.
and Blood Institute, 1993. Available from URL: http://www.nhlbi.nih.gov/
health/prof/lung/ asthma/astpreg.txt. Accessed May 11, 2011. How to cite this article: Kar S, Krishnan A, Preetha K, Mohankar A. A
19. Bousquet J, Van Cauwenberge P, Khaltaev N; Aria Workshop Group; World review of antihistamines used during pregnancy. J Pharmacol Pharmacother
Health Organization. Allergic rhinitis and its impact on asthma. J Allergy
2012;3:105-8.
Clin Immunol 2001;108 (5 Suppl):S147-334.
20. The use of newer asthma and allergy medications during pregnancy. The Source of Support: Nil, Conflict of Interest: None declared.
Author Help: Online submission of the manuscripts
Articles can be submitted online from http://www.journalonweb.com. For online submission, the articles should be prepared in two files (first
page file and article file). Images should be submitted separately.
1) First Page File:
Prepare the title page, covering letter, acknowledgement etc. using a word processor program. All information related to your identity should
be included here. Use text/rtf/doc/pdf files. Do not zip the files.
2) Article File:
The main text of the article, beginning with the Abstract to References (including tables) should be in this file. Do not include any information
(such as acknowledgement, your names in page headers etc.) in this file. Use text/rtf/doc/pdf files. Do not zip the files. Limit the file size
to 1024 kb. Do not incorporate images in the file. If file size is large, graphs can be submitted separately as images, without their being
incorporated in the article file. This will reduce the size of the file.
3) Images:
Submit good quality color images. Each image should be less than 4096 kb (4 MB) in size. The size of the image can be reduced by decreasing
the actual height and width of the images (keep up to about 6 inches and up to about 1800 x 1200 pixels). JPEG is the most suitable file
format. The image quality should be good enough to judge the scientific value of the image. For the purpose of printing, always retain a good
quality, high resolution image. This high resolution image should be sent to the editorial office at the time of sending a revised article.
4) Legends:
Legends for the figures/images should be included at the end of the article file.
108 Journal of Pharmacology and Pharmacotherapeutics | April-June 2012 | Vol 3 | Issue 2
You might also like
- Paces Guide 2012 From Online NotesDocument228 pagesPaces Guide 2012 From Online NotesThistell ThistleNo ratings yet
- IJPHRD February - 2020 PDFDocument2,663 pagesIJPHRD February - 2020 PDFzaenab anissaNo ratings yet
- Case Study On GlaucomaDocument6 pagesCase Study On GlaucomaKing GamerNo ratings yet
- Mksap PulmonaryDocument77 pagesMksap PulmonaryAna Roman100% (4)
- A Review of Antihistamines Used During Pregnancy 2012 PDFDocument4 pagesA Review of Antihistamines Used During Pregnancy 2012 PDFRicardo Robles AlfaroNo ratings yet
- Unit: 6 Pharmacology For Midwives: Prepared By: Anita Khadka M.SC Nursing 4 BatchDocument244 pagesUnit: 6 Pharmacology For Midwives: Prepared By: Anita Khadka M.SC Nursing 4 BatchAnita KhadkaNo ratings yet
- Drug in PregnancyDocument5 pagesDrug in PregnancyNesru Ahmed AkkichuNo ratings yet
- 6811-Article Text-24511-1-10-20110110Document3 pages6811-Article Text-24511-1-10-20110110Mohammed shamiul ShahidNo ratings yet
- Drugs in PregnancyDocument2 pagesDrugs in PregnancyDeepankar SrigyanNo ratings yet
- Over-the-Counter Medications in PregnancyDocument8 pagesOver-the-Counter Medications in PregnancyAlloiBialbaNo ratings yet
- Teratogen Information Service For Pharmacists: A Pilot StudyDocument13 pagesTeratogen Information Service For Pharmacists: A Pilot StudyfooleiNo ratings yet
- The Relation Between Antihistamine Medication During Early Pregnancy & Birth DefectsDocument4 pagesThe Relation Between Antihistamine Medication During Early Pregnancy & Birth DefectsRandilufti SantosoNo ratings yet
- Drug Therapy in PregnancyDocument14 pagesDrug Therapy in PregnancySNo ratings yet
- Drugs in PregnancyDocument2 pagesDrugs in Pregnancysnehalmane260No ratings yet
- Drugs in PregnancyDocument33 pagesDrugs in PregnancyserbalexNo ratings yet
- PHARMA - Module 1Document3 pagesPHARMA - Module 1Ashley AmihanNo ratings yet
- Drug Use in Pregnancy & Lactation: Department of Pharmaceutical CareDocument39 pagesDrug Use in Pregnancy & Lactation: Department of Pharmaceutical CareretnodwiNo ratings yet
- Rhinitis and PregnancyDocument14 pagesRhinitis and PregnancyIwan SumantriNo ratings yet
- Pharma NotesDocument17 pagesPharma Notesseanne kskwkwkaNo ratings yet
- Kategori Obat KehamilanDocument38 pagesKategori Obat Kehamilantheresa shintauliNo ratings yet
- 4-Drugs in Obs & GyneDocument52 pages4-Drugs in Obs & Gyneapi-37033520% (2)
- OtcdrugDocument2 pagesOtcdrugDaffodil PearlNo ratings yet
- Some Issues To Consider While Prescribing Medications For : Pregnant and Lactating PatientsDocument25 pagesSome Issues To Consider While Prescribing Medications For : Pregnant and Lactating PatientsKishor Bajgain100% (1)
- Drug Toxicity in Pregnancy and LactationDocument3 pagesDrug Toxicity in Pregnancy and LactationPardeep SonyNo ratings yet
- Antibiotic GuidelinesDocument38 pagesAntibiotic GuidelinesKomang Adhi AmertajayaNo ratings yet
- Pharma ReviewerDocument16 pagesPharma ReviewerChris AnnNo ratings yet
- Teratogenic Effect of Different Drugs at Different Stages in PregnancyDocument4 pagesTeratogenic Effect of Different Drugs at Different Stages in PregnancyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- New Drugs: Self-Test QuestionsDocument3 pagesNew Drugs: Self-Test QuestionscNo ratings yet
- Antimicrobial Stewardship in Primary CareDocument6 pagesAntimicrobial Stewardship in Primary CareMohammed HaiderNo ratings yet
- The Nursing Process in Drug Therapy: College of Health SciencesDocument76 pagesThe Nursing Process in Drug Therapy: College of Health SciencesNat Lynne Distor TrondilloNo ratings yet
- NUR 304 Study Guide For Unit 1 TestDocument23 pagesNUR 304 Study Guide For Unit 1 Testccapps25No ratings yet
- (OBa TeratogensDocument15 pages(OBa TeratogensClyde Yuchengco Cu-unjiengNo ratings yet
- BJSTR MS Id 002667Document9 pagesBJSTR MS Id 002667misulica2010No ratings yet
- ObstetricsA - Teratology, Teratogens, and Fetotoxic Agents - Dr. Marinas (Lea Pacis) PDFDocument15 pagesObstetricsA - Teratology, Teratogens, and Fetotoxic Agents - Dr. Marinas (Lea Pacis) PDFPamela CastilloNo ratings yet
- Gamma-Hydroxybutyric Acid: Controlled Drug SubstancesDocument5 pagesGamma-Hydroxybutyric Acid: Controlled Drug SubstancesAngelica Charisse BuliganNo ratings yet
- 02 Pharmacotherapy in Pregnancy and LactationDocument10 pages02 Pharmacotherapy in Pregnancy and LactationAlejandra RequesensNo ratings yet
- Sato 2012Document6 pagesSato 2012triNo ratings yet
- Drugs in Pregnancy and LactationDocument6 pagesDrugs in Pregnancy and LactationRidwan FajiriNo ratings yet
- Clinical Pharmacy Roger Walker Clinical Pharmacy and Therapeutics 5th EdDocument14 pagesClinical Pharmacy Roger Walker Clinical Pharmacy and Therapeutics 5th Edstella.gillesania.chenNo ratings yet
- Dr. Vikas S. Sharma MD PharmacologyDocument67 pagesDr. Vikas S. Sharma MD Pharmacologyrevathidadam55555No ratings yet
- Dr. Vikas S. Sharma MD PharmacologyDocument67 pagesDr. Vikas S. Sharma MD Pharmacologyrevathidadam55555No ratings yet
- Clinical Pharmacy and Therapeutics by Cate Whittlesea and Karen HodsonDocument15 pagesClinical Pharmacy and Therapeutics by Cate Whittlesea and Karen Hodsonstella.gillesania.chenNo ratings yet
- New Changes in Pregnancy and Lactation Labelling RDocument11 pagesNew Changes in Pregnancy and Lactation Labelling RraidasilvabrNo ratings yet
- Journal Pone 0180108Document18 pagesJournal Pone 0180108phoenixNo ratings yet
- Risco Potencial Do Uso de Medicamentos Durante A Gravidez e A LactaçãoDocument6 pagesRisco Potencial Do Uso de Medicamentos Durante A Gravidez e A LactaçãoAnna Elisa Borges BarcelosNo ratings yet
- Antifungal Drugs During Pregnancy: An Updated ReviewDocument9 pagesAntifungal Drugs During Pregnancy: An Updated ReviewLenin CarrilloNo ratings yet
- Pharma NotesDocument18 pagesPharma Notesseanne kskwkwkaNo ratings yet
- Pregnancy and Surgery-Do They Mix?Document79 pagesPregnancy and Surgery-Do They Mix?PutriRahayuMoidadyNo ratings yet
- PIIS0016508506008651Document29 pagesPIIS0016508506008651Ongoongoseven b. e. bNo ratings yet
- 1 Introduction To Pharmacology: 1.1 BackgroundDocument10 pages1 Introduction To Pharmacology: 1.1 BackgroundDental LecturesMMQNo ratings yet
- Notes FormatDocument4 pagesNotes FormatSamuel IdoNo ratings yet
- Dick PharmaDocument10 pagesDick PharmaMaverick LimNo ratings yet
- Use of Antihistamines in PediatricsDocument13 pagesUse of Antihistamines in PediatricsBIOLA OSIFESONo ratings yet
- Medications in Pregnancy 2Document16 pagesMedications in Pregnancy 2Franklin GarzaNo ratings yet
- Antifungal Drugs During Pregnancy An Updated ReviewDocument9 pagesAntifungal Drugs During Pregnancy An Updated ReviewRochnald PigaiNo ratings yet
- Pharma Reviewer-1Document9 pagesPharma Reviewer-1pinpindalgoNo ratings yet
- Csdmard in Rheumatoid Arthritis During Pregnancy and Lactation: A ReviewDocument10 pagesCsdmard in Rheumatoid Arthritis During Pregnancy and Lactation: A Reviewyuliana160793No ratings yet
- Pharma LectureDocument68 pagesPharma LectureMax LocoNo ratings yet
- Prescribing in PregnancyDocument2 pagesPrescribing in Pregnancymedical studentNo ratings yet
- Amer Peds Recomm Re Psy Drugs and PregnancyDocument10 pagesAmer Peds Recomm Re Psy Drugs and Pregnancyscribd4kmhNo ratings yet
- Jurnal KehamilanDocument13 pagesJurnal KehamilanNuraini Putri UtamiNo ratings yet
- The New Pregnancy and Lactation Labeling RuleDocument3 pagesThe New Pregnancy and Lactation Labeling RuleVijendra RNo ratings yet
- Anti Microbial DrugsDocument35 pagesAnti Microbial DrugsUmashankar SharmaNo ratings yet
- Taking Medicines in Pregnancy: What’s Safe and What’s Not - What The Experts SayFrom EverandTaking Medicines in Pregnancy: What’s Safe and What’s Not - What The Experts SayNo ratings yet
- Vol 27.5 - Neurocritical Care.2021Document363 pagesVol 27.5 - Neurocritical Care.2021RafaelNo ratings yet
- AntitrombolitikDocument7 pagesAntitrombolitikadityaNo ratings yet
- Medical Israeli Syllabus For Internal Medicine For Exam LicenseDocument4 pagesMedical Israeli Syllabus For Internal Medicine For Exam Licensemohammadeid0% (2)
- Cpe Common Diagnoses 6-4-2021Document9 pagesCpe Common Diagnoses 6-4-2021Shubham HarishNo ratings yet
- A Practical Guide To Integrated Type 2 Diabetes Care: Irish College of General PractitionersDocument77 pagesA Practical Guide To Integrated Type 2 Diabetes Care: Irish College of General PractitionersH. Putri M.No ratings yet
- Gagal Ginjal Akut Dan Kronik: Divisi Ginjal & Hipertensi SMF/Lab - Ilmu Penyakit Dalam FK - UNS / RSUD DR - MoewardiDocument29 pagesGagal Ginjal Akut Dan Kronik: Divisi Ginjal & Hipertensi SMF/Lab - Ilmu Penyakit Dalam FK - UNS / RSUD DR - MoewardiHabiby Habibaty QolbiNo ratings yet
- O.M Final ExamDocument4 pagesO.M Final ExamAwilNo ratings yet
- Nej M CPC 2004992Document11 pagesNej M CPC 2004992Deina IdlcNo ratings yet
- Adult Referral For PC Assessment FormDocument1 pageAdult Referral For PC Assessment Formwhy u reading thisNo ratings yet
- Juhairina: Medical Nutrition Therapy For Disorders of The Lower Gastrointestinal TractDocument82 pagesJuhairina: Medical Nutrition Therapy For Disorders of The Lower Gastrointestinal Tractdesy100% (1)
- (IM A) (Com Dse) Typhoid Fever (Strawberry)Document4 pages(IM A) (Com Dse) Typhoid Fever (Strawberry)NoreenNo ratings yet
- Moving Exam NCM 109 Lecture For PrintDocument6 pagesMoving Exam NCM 109 Lecture For PrintMoneto CasaganNo ratings yet
- Febrile Convulsion & EpilepsyDocument17 pagesFebrile Convulsion & EpilepsyprajwalNo ratings yet
- Headache When To WorryDocument9 pagesHeadache When To Worryezra_putriNo ratings yet
- Review Article On BarbituratesDocument32 pagesReview Article On BarbituratesChelsea Ritz MendozaNo ratings yet
- Pedia Uworld DrillsDocument9 pagesPedia Uworld DrillsMhing's Printing ServicesNo ratings yet
- DK IPD 3 - Ogie AsitesDocument174 pagesDK IPD 3 - Ogie AsiteshariogieNo ratings yet
- Icd 10Document170 pagesIcd 10Silverius Seantoni SabellaNo ratings yet
- The Amyloid Beta Peptide A Chemist S Perspective. Role in Alzheimer's and FibrillizationDocument46 pagesThe Amyloid Beta Peptide A Chemist S Perspective. Role in Alzheimer's and FibrillizationAdrianENo ratings yet
- 2020 - Long-Term Non-Invasive Ventilation in Children - Current Use, Indications, and ContraindicationsDocument9 pages2020 - Long-Term Non-Invasive Ventilation in Children - Current Use, Indications, and ContraindicationsHack clashNo ratings yet
- MEDBIO KROK-1 English 2019-2020Document65 pagesMEDBIO KROK-1 English 2019-2020Катерина КабишNo ratings yet
- Lymph Nodes Normal Anatomy Major ZonesDocument5 pagesLymph Nodes Normal Anatomy Major ZoneschristianNo ratings yet
- Skin Rashes: An Emerging Symptom of COVID-19: What Clinicians Need To Know About Cutaneous Manifestations of COVID-19Document3 pagesSkin Rashes: An Emerging Symptom of COVID-19: What Clinicians Need To Know About Cutaneous Manifestations of COVID-19littlemisseeeNo ratings yet
- Meddra Important Medical Event Terms List Version 241 enDocument691 pagesMeddra Important Medical Event Terms List Version 241 enLuis Antonio Camacho CamachoNo ratings yet
- Bomb and Blast Injuries PDFDocument64 pagesBomb and Blast Injuries PDFMilosevic Goran100% (1)
- 2.D17 419 Kastriot Meqa Agim BegzatiDocument6 pages2.D17 419 Kastriot Meqa Agim BegzatiAndi Ndaru WNo ratings yet