Professional Documents
Culture Documents
Control and Management of Methicillin Resistant Staphylococcus Aureus (MRSA) / Michelle Bergin ... (Et Al.)
Uploaded by
alshanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Control and Management of Methicillin Resistant Staphylococcus Aureus (MRSA) / Michelle Bergin ... (Et Al.)
Uploaded by
alshanCopyright:
Available Formats
Control and management of Methicillin Resistant
Staphylococcus Aureus (MRSA) / Michelle Bergin ... [et al.]
Item Type Report
Authors Bergin, Michelle
Rights HSE Dublin Mid-Leinster
Download date 01/10/2019 17:48:34
Link to Item http://hdl.handle.net/10147/45945
Find this and similar works at - http://www.lenus.ie/hse
Feidhmeannacht na Seirbhíse Slàinte GL No: IPCR 12
Baile Átha Cliath & Lár Laighin Revision No: 4
HSE Dublin Mid-Leinster Page: 1
Department
No of Pages: 34
Infection Prevention and Control
Guideline Date: January 2008
Guideline Title: Control and Management of Methicillin Resistant
Staphylococcus Aureus (MRSA)
Written/Reviewed by: Title:
Michelle Bergin, Claire Dowling, CNM11’s Infection Control
Breda Corrigan, Pam O’Callaghan
Approved by: Marena Burd Title: ADON Infection Control
Table of Contents Page
1.0 Purpose 3
2.0 Scope 3
3.0 Definitions and abbreviations 3
4.0 Responsibility 3
5.0 Guideline 4
5.1 Patient management 4
5.2 Before leaving the affected patient's room or bedside 5
5.3 Management of the patient's environment 6
5.4 Patient screening 9
5.5 Admission to the acute hospital of a patient with M.R.S.A. 10
5.6 Screening during outbreaks 12
5.7 Treatment of patients with M.R.S.A. colonisation/infection 12
5.7.1 Neonates/Infants (birth to 3 months) 13
5.7.2 Neonates/Infants repeat screening and follow-up 14
5.7.3 Children and adults treatment/decolonisation 14
5.7.4 Children and adults - repeat screening and follow-up 15
5.7.5 Treatment - Skin lesion 16
5.7.6 Treatment - major wounds 16
5.7.7 Treatment - PEG and Tracheostomy sites 16
5.8 Surgery 17
5.8.1 Recovery room 17
5.9 Patient Discharge 18
5.10 Ambulance Transport 18
5.11 Out-patient Visits 19
5.12 Death 19
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 2
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
5.13 Healthcare Workers (HCW) 19
5.14 How can we prevent M.R.S.A. 20
5.15 Management of M.R.S.A. in Nursing Homes, Residential Homes,
District, Community hospitals and Special Hospitals. 21
5.16 M.R.S.A. screening 23
5.17 Treatment/Deconlonisation 23
5.18 Repeat screening and follow-up 24
6.0 Frequency of review 25
7.0 Method used to review operation of guideline 25
8.0 References 26
9.0 Appendices 26
9.1 Isolation Room door sign 27
9.2 Treatment Products 28
9.3 Discharge/Transfer Notification Form 29
9.4 Patient and Visitor Information 30
9.5 De-colonisation and re-screen record tool 33
9.6 How to use Octenisan Poster 34
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 3
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
1.0 Purpose
2.0 Scope
3.0 Definitions and Abbreviations
M.R.S.A. stands for Methicillin-Resistant Staphylococcus aureus.
M.S.S.A stands for Methicillin Sensitive Staphylococcus aureus which is a
bacterium that can reside on the skin or can be found in the nose of about one
third of healthy individuals. Generally it causes no harm but it may colonise or
infect pressure sores, varicose ulcers or surgical wounds occasionally it may
cause skin infections, such as boils or impetigo. M.S.S.A. can also cause more
serious illness, if it gains access to the blood stream, leading to bacteraemia,
or to the lungs, causing, for example, ventilator-associated pneumonia.
Early penicillin antibiotics such as Flucloxacillin were effective in the treatment
of M.S.S.A.infections but since the late 1960’s many strains have become
resistant to commonly used antibiotics. As Methicillin was amongst the first
antibiotics used to treat M.S.S.A. infections, these bacteria subsequently
developed resistance and became known as M.R.S.A.
M.R.S.A. colonisation: The term colonisation refers to the presence of
bacteria without a tissue reaction.
M.R.S.A. infection: The term infection refers to the deposition and
multiplication of bacteria e.g. MRSA in tissues or on surfaces of the body with
an associated tissue reaction.
Healthcare Worker (HCW)
Personal Protective Equipment (PPE)
4.0 Responsibility
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 4
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
5.0 Guideline
CONTROL OF M.R.S.A. IN ACUTE HOSPITAL WARDS, INCLUDING
SPECIALIST UNITS
5.1 Patient Management
• It is the responsibility of the patient’s consultant/team to inform the
patient/relative of their M.R.S.A. diagnosis.
• When a patient is identified with M.R.S.A. liaise with the Infection
Control Nurse.
• Advice regarding patient management and precautions required should
be given by the Nurse in charge to staff and visitors.
• Hand Hygiene is the most important and effective method of
preventing the spread of M.R.S.A.. Consultants and Nurse
Managers must insist on adherance to hand hygiene procedures
by all staff.
• Perform hand hygiene before and after each patient contact and after removal of PPE.
• An individual assessment of the medical and infectious condition of each
patient will dictate whether isolation is required
• Isolation is not essential to prevent the transmission of MRSA, however
contact precautions are achieved to a higher standard when patients are
accomodated in isolation.
• The door of the isolation must be kept closed at all times and
appropriate signage displayed Refer to appendix 9.1 Isolation Room
Door Sign
• Personal Protective Equipment (PPE)
• Wear a clean plastic apron and gloves if having direct contact with the
patient, their secretions/excretions, linen and their environment.
• Where major physical contact is required, it is advisable to wear a
disposable, impermeable gown, covering arms instead of an apron
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 5
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• Standard surgical masks are required for tracheal suctioning and/or for
chest physiotherapy with M.R.S.A. in sputum and also when performing
dressings on patients with extensive burns or lesions.
Movement/Transfer of Patient to other Departments
• Postpone elective surgical procedures until the patient is considered
non-infectious if not contra-indicated.
• Patient movement from the room should be minimised to essential
purposes only
N.B. Patients colonised/infected with MRSA should be allowed to
leave their room for rehabilitation.
• Inform the staff of other departments before movement/transfer of the
patient
• On movement to other departments the patient should be attended to
promptly and then returned directly to his/her room.
N.B. Visitors do not require protective clothing. Advice should be
given on hand hygiene before and after visiting the patient.
5.2 Before leaving the affected patient’s room or bedside
• Remove gloves and apron and dispose into Healthcare non-risk waste
(BLACK) bag unless blood stained, then place into Healthcare Risk Waste
(YELLOW) bag, inside the room where possible.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 6
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• Place linen contaminated with blood of body fluids into a water-
soluble/alginate bag, which is then placed in RED/Contaminated laundry
bag/skip.
• Used, uncontaminated linen is placed into a WHITE laundry bag/skip.
• Before entering and on leaving the room or bedside perform hand hygiene.
5.3 MANAGEMENT OF THE PATIENT’S ENVIRONMENT
Daily Cleaning of Isolation room
• Vacuum cleaners may be used in isolation rooms, however they:
o Must be fitted with HEPA filters
o Must be serviced and HEPA filters replaced regularly
o Must have records kept of service and filter changing
• Clean all horizontal surfaces, with general purpose detergent and hot water
using colour coding system i.e. yellow basin and disposable yellow cloth.
• Wash floor with the floor cleaning product and yellow bucket and yellow
mop handle or change mop if using the flat mop system
• Clean patient equipment with general purpose detergent and hot water.
Keep all equipment in the patient’s room/area for his/her sole use where
possible, e.g. stethoscopes and blood pressure devices.
• A disposable blood pressure cuff or a designated blood pressure cuff for
isolation purposes, which is cleanable with a detergent wipe should be
used.
• A designated stethoscope which is cleaned after each use with 70% alcohol
wipes(Alco wipes).
• Electrical equipment, including TV remote control units, portable telephones
and patient call bells should be damp dusted with 70% alcohol wipes(Alco
wipes).
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 7
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• All charts should be kept outside the patient’s room/area where possible.
• No specific precautions are necessary for crockery and cutlery from a
patient with MRSA if a dishwasher is available.
• If no dishwasher is available, they should be washed with hot water and
detergent, dry with disposable paper towel and keep for use by that
patient.
Note: Disinfection with Precept is NOT required on a daily basis
Terminal Clean of Isolation room on Patient transfer or discharge
• On the patient’s transfer or discharge bed curtains/screens and bed
linen/duvets should be sent for laundering.
• Wash all surfaces, furniture, equipment, bed frame, mattress covers and
pillows with general purpose detergent.
• Followed by disinfection with Precept solution 1:1000 ppm ( 2 X 2.5 gram
tablets dissolved in 2.5 litres of water) freshly made up and discard after
use.
• Wash floor with designated floor cleaning detergent and then disinfect with
Precept solution 1:1000 ppm.
• It is not necessary to change window curtains routinely.
• Window blinds must be washed and disinfected where applicable.
• The room may be used immediately.
After cleaning, incubators should be disinfected with Precept
1:1000ppm, left for 30 minutes and then rinsed off with detergent and
water.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 8
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
Daily Cleaning of Patients bed-space when patient in open ward.
• Clean this patient’s bed-space last.
• Clean all horizontal surfaces, with general purpose detergent and hot
water.
• Wash floor with designated floor cleaning detergent.
• Clean patient equipment with general purpose detergent and hot water.
• Launder cleaning cloths and mops or dispose after single use
• Use BLUE bucket and mop handle, but water and mop head must be
changed after use in this bed space.
Terminal Cleaning of bed-space on Patient transfer or discharge
• On the patient’s transfer or discharge bed curtains/screens and bed
linen/duvets should be sent for laundering.
• Wash all surfaces, furniture, equipment, bed frame, mattress covers and
pillows with general purpose detergent.
• Followed by disinfection with Precept solution 1:1000 ppm ( 2 X 2.5 gram
tablets dissolved in 2.5 litres of water) freshly made up and discard after
use.
• Wash floor with designated floor cleaning detergent and then disinfect with
Precept solution 1:1000 ppm.
• It is not necessary to change window curtains routinely.
• Window blinds must be washed and disinfected where applicable.
• The bed-space may be used immediately
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 9
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
5.4 PATIENT SCREENING
An MRSA screen consists of samples from nose, groin and
any skin breaks, using 1 swab for both nostrils and 1 swab
for both groins.
Axillae are no longer screened
• For adults and children, take screening swabs from: (do not repeat site
already identified)
o Anterior Nares (both sides, using 1 swab only)
o Perineum or Groin (not both), if from groin, use 1 swab only.
o Any wound or skin condition e.g. eczema
o Sputum (if present)
o CSU if catheterised.
• For Infants/neonates in special care baby units, take screening swabs
from:
o Nose
o Umbilicus until healed
o Perineum
Patients who should be screened for MRSA include
• Patients known to be previously positive and who are being re-admitted to
hospital.
• Patients admitted from another hospital or health care facility.
• During an outbreak as determined by the infection control nurse.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 10
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• Patients with signs of infection in wounds and ulcers
N.B. Before taking wound swab remove exudate by cleaning
wound with normal saline
• Patients due to undergo elective high-risk surgery, e.g. Cardio-
thoracic/Orthopaedic implant surgery.
• Weekly screening in High Risk areas e.g. Intensive Care Unit (ICU)/Special
Care Baby Unit (SCBU).
• Mothers of positive infants and infants of positive mothers may require
screening in consultation with Infection Control Nurse/G.P.
• N.B. There is no rationale for screening prior to discharge home or
to long stay units or nursing homes.
MRSA IS NOT A REASON TO REFUSE ADMISSION FROM AN ACUTE
HOSPITAL, OTHER INSTITUTION OR FROM THE COMMUNITY
5.5 Admission to the acute hospital of a patient with M.R.S.A.
• The responsibility is on the referring doctor to inform the admitting hospital
of the patient’s MRSA status.
• Inform an Infection Control Nurse and/or Consultant Microbiologist.
• Admit to a single room, if available, or place patient away from other
patients at high risk until screening swabs are negative. Examples of high-
risk patients include ventilated, tracheotomy, all those with surgical
wounds, skin lesions, central venous catheter (CVC), drains, tubes and
urinary catheters.
• Send screening swabs as appropriate.
• Explain the reason for this procedure to the patient/relatives and/or
parents where relevant.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 11
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• Following the identification of patients with MRSA, single room isolation will
be required for patients in the following areas:
o Intensive Care,
o Special Care Baby Units,
o Surgical,
o Orthopaedics,
o Gynaecology,
o Maternity
o ENT.
o Patients who are very ill
o Sputum carriers
o Patients with exfoliate conditions
o Patients awaiting high-risk surgery e.g. Cardio-thoracic/Orthopaedic
surgery.
• If there are two or more MRSA positive patients, they may be co-horted in
a designated area.
• Inform relevant departments prior to any procedure, e.g. operating
theatres, x-ray, physiotherapy.
• Accompanying staff DO NOT require gloves and apron.
• The movement of patients with M.R.S.A. within the hospital should be kept
to a minimum.
• Patients colonised/infected MRSA should be allowed to leave their room for
rehabilitation
• Ensure that the patient/relatives understand MRSA and it’s implications,
and that reassurance is offered and they are provided with the leaflet,
MRSA: information for the Patients and Visitors 2006.
• Tag all charts as soon as MRSA is identified.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 12
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
5.6 SCREENING DURING OUTBREAKS (Patients and staff)
Following the advice of Infection Control Nurse/Microbiologist
Screening
Initially nasal swabs only, if positive screen as above.
• For a newly identified case of MRSA in ICU, SCBU, screen all patients in
that area.
• If there is another positive case, screen medical, nursing and the Allied
Medical Professionals. Other staff may also require screening at the
discretion of the Infection Control/Nurse/Team.
• Increase cleaning measures in the area.
• If two or more patients are newly identified with M.R.S.A. within a two
week period in medium risk areas, (e.g. Surgical/Obstetric Deptartments)
screen surgical/obstetric team, other health care staff and patients at
discretion of the infection control Nurse
• If two or more patients are newly identified with MRSA in a low risk area
e.g. Medical or Care of the Elderly wards, liase with Infection Control
Nurse.
• Discharge patients as soon as possible.
5.7 TREATMENT OF PATIENTS WITH MRSA COLONISATION/INFECTION
• Some antiseptics suitable for skin and body disinfection and treatment of
carriage sites are listed in Appendix 9.1. This table must be consulted for
additional comments.
• Decolonisation treatment should not commence until the results of
screening swabs are available as this predisposes to the emergence
of resistance.
• N.B. Only treat positive sites as per Microbiology Laboratory
results
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 13
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
5.7.1 Neonates/Infants (birth to 3 months)
Neonates after consultation with a Consultant Paediatrician
N.B. Only treat positive sites as per Microbiology Laboratory results
Treatment/Decolonisation
• Nose MRSA positive
Mupirocin (Bactroban) Nasal Ointment three times per day for 5 days
• Groin MRSA positive
Octenisan antimicrobial body wash lotion instead of soap/bath solution
for full body washing daily for 5 days. (See Appendix 9.5).
• Skin folds- e.g. axilla, groin, elbow joints and behind knees,
Apply CX Powder sparingly once daily after shower for 5 days.
Procedure for using Octenisan:
• Wet the skin
• Apply Octenisan to disposable cloth
• Wash body with Octenisan and observe a contact time of 3 minutes.
• Rinse off all of the Octenisan.
• Dry body with a clean towel (Change towel daily).
• Ensure that hair is washed with Octenisan on Day 2 and 4
Additional procedures:
• Change wash cloths, towel, cot/incubator linen and clothing daily for the
duration of treatment
• Send to laundry as per normal laundry guidelines
Umbilicus MRSA positive
• Clean umbilicus with 70% alcohol (Surgical spirit) and allow to dry.
• Sparingly apply Chlorhexidine acetate 1% (CX powder) daily for five days
or up to three times daily at nappy change
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 14
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
If more than one site is positive Octenisan, Bactroban and CX powder
should commence on the same day and must all be prescribed in the
patient’s Medication Record.
5.7.2 Neonates/Infants Repeat screening (nose, umbilicus and
perineum) and follow-up
Step 1 Re-screen on the third day following completion of treatment.
Step 2 If any sites remain positive treat positive sites only.
Step 3 Re-screen on the third day following 2nd treatment. If any sites
remain positive contact the Infection Control Nurse.
Step 4 If in step 2 the screen results are negative, re-screen for 3rd time.
5.7.3 Children & Adults Treatment/Decolonisation
Nose MRSA positive
Mupirocin (Bactroban) Nasal Ointment three times per day for 5 days
Groin MRSA positive
Octenisan antimicrobial body wash lotion instead of soap/bath/shower gel
for full body washing daily for 5 days. (See Appendix 9.5).
Skin folds- e.g. axilla, groin, under breasts, elbow joints and behind knees,
Apply CX Powder sparingly once daily after shower for 5 days.
Procedure for using Octenisan
• Wet the skin
• Apply Octenisan to disposable cloth
• Wash body with Octenisan and observe a contact time of 3 minutes.
• Rinse off all of the Octenisan.
• Dry body with a clean towel (Change towel daily).
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 15
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• Ensure that hair is washed with Octenisan on Day 2 and 4
If more than one site is positive Octenisan, Bactroban and CX powder
should commence on the same day and must all be prescribed in the
patient’s Medication Record.
Additional procedures:
• Change wash cloths, towels, bed linen, nightwear and clothing daily, after
body washing, during treatment
• Send to laundry as per normal laundry guidelines.
5.7.4 Children & Adults - REPEAT SCREENING AND FOLLOW UP:
Step 1 Re-screen on the third day following completion of treatment.
Step 2 If any sites remain positive treat positive sites only.
Step 3 Re-screen all sites on the third day following 2nd treatment. If any
sites remain positive contact the Infection Control Nurse.
Step 4 If in step 2 the screen results are negative, re-screen for 3rd time.
• Repeat screening specimens two days following the end of treatment (no
sooner) and on two additional occasions, leaving at least a 4 day interval
between screens.
• Continue isolation and/or contact precautions until three consecutive sets of
screening swabs are negative or in consultation with the Infection Control
Nurse.
• If screening specimens remain positive after first treatment, repeat treatment
and re-screen. In the event that screening specimens remain positive after
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 16
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
second treatment, do not re-treat. Consult the Infection Control Nurse or
Consultant Microbiologist
• In acute hospitals if the patient receives antibiotics subsequently repeat full
screening procedure two days after antibiotics are discontinued, as additional
antibiotic therapy may cause re-emergence of MRSA.
• Repeat full screening procedures on re-admission.
5.7.5 Skin lesion e.g. minor wounds, minor ulcers etc.
Apply Mupirocin 2% (Bactroban) ointment, daily for 5 days, after
consultation with the patient’s clinician and after appropriate wound toilet.
Note: Risk of renal toxicity with Mupirocin, must be prescribed by
doctor and is contra-indicated during pregnancy and lactation.
5.7.6 Major wounds, Critically colonised/infected e.g. leg ulcers
Consult with a doctor or nurse specialist in wound care for advice on
choice of dressing products e.g. Acticoat, Betadine/Inadine tulle.
5.7.7 PEG and tracheostomy sites
Clean with 0.05% Chlorhexidine (Unisept)
Mupirocin (Bactroban) 2% is contraindicated as is can damage the
plastic tubing.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 17
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
5.8 Surgery
• Postpone elective surgical procedures until the patient is considered non-
infectious if not contra-indicated.
• In conditions where staphylococcal prophylaxis is indicated, consult
the Microbiologist or Antibiotic Pharmacist, consider using a prophylactic
glycopeptide (e.g. I.V. Vancomycin).
• Cover all lesions with an impermeable dressing.
• Place the patient last on theatre list (if possible).
• All excess equipment should be removed from the operating theatre
prior to surgery.
• Theatre Staff – Scrubs and attire must be changed after handling infected
or colonised cases.
• On the patient’s transfer, cleaning must be followed by disinfection with
Precept 1: 1000 ppm (see dilutions poster).
• Linen should be sent to the laundry as per linen guidelines.
• The theatre may then be used immediately.
5.8.1 RECOVERY ROOM
• Patient may be nursed in the recovery room, but must have a dedicated
nurse.
• If the patient is colonised at a wound site only, ensure this site is covered
with an impermeable dressing.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 18
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
5.9 Patient Discharge
• When discharging a patient with a history of MRSA to any hospital or
Community Care unit, the hospital/Community Care unit should be notified in
advance of discharge.
• The Medical and Nursing discharge letters should include the MRSA status of
the patient, and treatment received or required.
• MRSA Discharge / Transfer Notification Form must be completed. (see
appendix 9.2, page 27)
• MRSA carriage is not a reason to delay discharge to nursing homes, special
hospitals or to the patient’s family home.
• MRSA should not be a reason for refusing to accept a patient back to the
referring hospital.
5.10 Ambulance transport:
• There is no evidence that ambulance staff are at risk when transporting
patients with MRSA.
• Ambulance staff should be informed that the risk of MRSA spread is not to
themselves but to other susceptible patients using the ambulance.
• Patients colonised with MRSA may be transported with other patients as
normal. Ensure wounds are covered with impermeable dressing and adhere to
good hand hygiene practice.
• Ambulance staff should observe the same ambulance cleaning precautions as
for all patients.
• Ambulance staff should perform hand hygiene after contact with a patient who
has MRSA.
• Glove usage must be adhered to as per standard precautions, i.e. when
handling blood, body fluids, broken skin and mucous membranes.
• Blankets and linen in contact with the patient should be laundered, in the
normal way following single patient use.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 19
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
5.11 Out-patient visits
• Inform Department manager of patient’s MRSA status
• Accompanying staff DO NOT require gloves and apron.
• Patient should be attended to promptly
• Ensure that all HCWs perform hand hygiene before and after contact with
the patient and on removal of PPE .
• Cleaning followed by disinfection is required especially after clinics where
patients have wounds exposed e.g. leg ulcer clinics.
5.12 Death:
No special precautions are required when a patient dies. The precautions taken
when laying-out patient remains should be the same as those taken for other
deceased patients (e.g. lesions should be covered with an impermeable
dressing).
5.13 Healthcare Workers (HCW)
These guidelines will help to prevent carriage among HCWs and should be
implemented in liaison with the Infection Control Nurse and Microbiologist.
• Hand hygiene is the most effective method of preventing the spread of
MRSA
• HCWs with exfoliative or pustular skin conditions should not, if possible,
nurse patients with MRSA.
• In health care setting, any exfoliative/pustular skin lesion should be
reported to the supervisor who will advise if any further management is
necessary.
• Routine screening of HCWs is not necessary, and of doubtful value as staff
are often transient carriers only.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 20
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• HCWs dealing with patients with MRSA during an outbreak, may need to be
screened on completion of this duty.
• All HCWs need to be informed of their positive M.R.S.A. colonisation.
• HCWs identified as MRSA positive on nasal screen should have groin swabs
collected.
• HCWs with nasal carriage only can continue to work in low risk areas. If
staffing allows, they should not work in ICU or other high-risk areas until
24 hours after commencing topical treatment (they may work in low risk
areas).
• HCWs carrying MRSA in any site are treated the same as for patient
management. After treatment (at least 48 hours) swabs should be sent to
the laboratory
• Chronic or repeat carriers will be managed on an individual basis.
• HCWs who deal with many patients in different units of the hospitals, e.g.
physiotherapists and phlebotomists, should be informed of patients
identified as MRSA positive and their role in taking measures to prevent
transmission.
• HCWs who themselves are in contact with MRSA carriers outside work,
should seek advice from the Infection Control Nurse or Microbiologist.
5.14 HOW CAN WE PREVENT MRSA?
• Strict control of antibiotics is essential in hospitals and the community, as
widespread use of both systemic and topical antibiotics predisposes to the
emergence of MRSA.
• Hand hygiene between attending to patients is the most effective method
of preventing the spread of MRSA.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 21
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• Early identification of cases and carriers, with appropriate treatment of
carriage sites and isolation of cases in the acute hospital setting will prevent
spread.
• Adhering to high standards of environmental hygiene.
• Early discharge of patients from hospital reduces the risk of acquiring MRSA.
5.15 MANAGEMENT OF MRSA IN NURSING / RESIDENTIAL HOMES
DISTRICT / COMMUNITY HOSPITALS AND SPECIAL HOSPITALS
MRSA IS NOT A REASON TO REFUSE ADMISSION FROM AN ACUTE
HOSPITAL, OTHER INSTITUTION OR FROM THE COMMUNITY.
GENERAL GUIDELINES:
N.B. Routine screening is not indicated and MUST NOT be undertaken
prior to acute hospital discharge or on admission to extended care
centres from another hospital or the community.
(These swabs will not be processed by the laboratory).
• The nurse-in-charge will be responsible for ensuring that the following
guidelines for the control of MRSA are implemented.
• The hospital discharge or admission letter should include the MRSA status
of the patient, and treatment received or required.
• MRSA Discharge/Transfer Notification Form must be completed(see
appendix 9.2)
• HAND HYGIENE IS THE MOST IMPORTANT AND EFFECTIVE MEHTOD
OF PREVENTING THE SPREAD OF MRSA.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 22
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• HAND HYGIENE MUST BE PERFORMED APPROPRIATELY BY ALL
HCWs.
• Wash hands with soap and water or use alcohol gel on visibly clean hands
before and after direct patient contact and on removal of PPE.
• Use disposable gloves when performing invasive procedures or handling
blood or body fluids. Dispose of gloves in Health care non-risk waste bag
(black).
• HCWs changing dressings should comply with aseptic technique, using
disposable gloves and a plastic apron.
• Change dressings in the resident’s own room / area.
• Cover wounds with appropriate dressings.
• Isolation nursing is rarely necessary as this may adversely affect patient
rehabilitation or well being. If in doubt, contact an Infection Control Nurse.
• Patients who are MRSA positive should be placed away from the more
vulnerable patients e.g. patients with PEG tubes, urinary catheters.
• If the patient is to travel by ambulance, inform ambulance personnel of the
patient’s MRSA status in advance.
• If the patient is to be admitted to an Acute Hospital or attend for Out-
Patient treatment or Accident & Emergency, the Department Manager of
should be informed.
• All skin lesions of an infective or exfoliative nature should be covered.
• Management and staff need to be aware of the importance of MRSA. HCWs
with extensive skin lesions (e.g. pustular or exfoliative) should be screened
for MRSA and managed appropriately.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 23
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
5.16 MRSA Screening
• This must only occur following a positive specimen result for
culture and sensitivity.
Screening Sites are:
• Anterior Nares (both sides, using 1 swab only)
• Perineum or Groin (not both) if from groin 1 swab only
• Any wound or abnormal skin lesion
• Sputum if present
• CSU if catheterised
• PEG site
Do not repeat site already identified.
5.17 Treatment/Decolonisation
Nose MRSA positive
Mupirocin (Bactroban) Nasal Ointment three times per day for 5 days
Groin MRSA positive
Octenisan antimicrobial body wash lotion instead of soap/bath/shower gel
for full body washing daily for 5 days. (See Appendix 9.5).
Skin folds- e.g. axilla, groin, under breasts, elbow joints and behind knees,
Apply CX Powder sparingly once daily after shower for 5 days.
Procedure for using Octenisan
• Wet the skin
• Apply Octenisan to disposable cloth
• Wash body with Octenisan and observe a contact time of 3 minutes.
• Rinse off all of the Octenisan.
• Dry body with a clean towel (Change towel daily).
• Ensure that hair is washed with Octenisan on Day 2 and 4
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 24
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
If more than one site is positive Octenisan, Bactroban and CX powder
should commence on the same day and must all be prescribed in the
patient’s Medication Record.
• N.B. Only treat positive sites as per Microbiology Laboratory
results and discussion with Infection Control Nurse
• Skin lesion e.g. minor wounds, minor ulcers etc.
• Apply Mupirocin (Bactroban) ointment, daily after consultation with the
patient’s clinician and after appropriate wound toilet. (see table 1 for contra
indications).
Note: Risk of renal toxicity, must be prescribed by doctor.
• Major wounds, Critically colonised/infected e.g. leg ulcers
Consult with a medical or nurse specialist in wound care.
Additional procedures:
• Change all bed linen, wash cloths and towels daily.
• Send to laundry as per normal laundry guidelines
• Change all night-clothes after body washing daily.
• In ambulatory patients, washable garments and undergarments should be
changed as often as possible, and preferably daily. Non-washable garments
should be dry cleaned during treatment if possible and must be dry cleaned at
the end of treatment.
5.18 REPEAT SCREENING AND FOLLOW UP:
• Repeat screening specimens two days following the end of treatment (no
sooner).
• If screening specimens remain positive after first treatment, repeat
treatment and re-screen.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 25
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
• In the event that screening specimens remain positive after second
treatment, do not re-treat or re-swab unless clinical infection suspected.
• Clearance swabs are not required as when patients recommence antibiotics
they will most likely re-emerge with MRSA colonisation.
• Patients with a history in these settings can be presumed to be chronic
carriers of MRSA.
• Standard precautions should be taken as with all patients.
N.B. If patients are on any of the beta-lactam (e.g. Augmentin)
antibiotics, they need to be discontinued and the patient put
on appropriate treatment. Continued use of these antibiotics
continues selection of MRSA.
If a nursing home/Community Care facility is in doubt about the management of
a patient or staff member with MRSA, they should contact the local Infection
Control Nurse or Consultant Microbiologist and follow the advice given.
6.0 Frequency of Review
2 yearly
7.0 Method used to review operation of Guideline
Data collection
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 26
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
8.0 References
8.1 The Control and Prevention of MRSA in Hospitals and in the
Community SARI September 2005
8.2 Children's University Hospital Temple Street, Dublin 2006
8.3 Bugs & Drugs Newsletter of the Mullingar, Portlaoise and Tullamore
Microbiology Laboratories, Infection Control and Antibiotic Pharmacist
Vol 1 No1 Page 1
9.0 Appendices
9.1 Isolation Room door sign
9.2 Treatment Products
9.3 Discharge/Transfer Notification Form
9.4 Patient Information Leaflet
9.5 De-colonisation and re-screening record tool
9.6 How to use Octenisan Poster
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 27
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
9.1 Isolation Room door sign
Attention
Please contact Nursing Staff
before entering this room.
Please wash hands or use the
alcohol hand rub/gel
before entering and when
leaving this room.
Thank you for your co-operation
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 28
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
9.2 Treatment Products.
Proprietary Constituents Comments
Preparations and
Indications
*Octensian Octenidine Use as liquid
soap/shower gel
“Bactroban nasal” Mupirocin 2% in paraffin For mucous membranes
base only. (agent of first
choice) Do not use in
pregnancy.
“Bactroban ointment” Mupirocin 2% in Skin carriage sites and
polyethulene glycol base small wounds
Avoid eyes, mucous
membranes, large
wounds and large raw
areas: do not use in
pregnancy or
lactation
CX antiseptic dusting Skin carriage sites.
powder
In the case of hypersensitivity, contra indications seek special advice
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 29
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
9.3 Discharge / Transfer Notification Form
NOTIFICATION OF M.R.S.A.
This form is to notify the relevant health professionals that a patient is or was
colonised/infected with M.R.S.A. This is not a discharge letter.
To: _______________________ _______________________
Name of Hospital
Re: _______________________
Dear____________________
The above patient was found to be colonised / infected with methicillin resistant
Staphylococcus aureus (M.R.S.A.). Sites found to be positive were as follows (
include dates of swabs):
_____________________________________________________________
_________________________________________________________________
_________________________________________________________
the following topical treatment was administered (treatment and dates)
_________________________________________________________________
_________________________________________________________________
_____________________________________________________
The most recent swabs were obtained on _____________________ (date)
All sites were negative / the following sites were positive (delete as applicable)
_____________________________________________________________
The present decolonisation treatment is as follows:
_____________________________________________________________
The treatment should continue for ___________________ days
In the event that the patient has to be admitted to another hospital, please
advise the receiving hospital / nursing home that the patient was M.R.S.A.
positive
Yours sincerely,
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 30
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
__________________
9.4 Information for Patients and Visitors 2006
What is MRSA?
MRSA stands for meticillin, resistant Staphylococcus aureus. Staphylococcus
aureus (pronounced staf-ill-o-kok-us or-ee-us), or "Staph aureus" for short, is a
common germ that lives completely harmlessly on the skin or in the nose of
about one in three people. MRSA is a type of Staph aureus that has become
resistant to a number of different antibiotics.
Most people who carry MRSA on their bodies or in their noses don't suffer any ill
effects. Carrying the germ harmlessly like this is called "colonisation". However
MRSA sometimes causes infections if it enters the body. This is more likely to
happen to people who are already unwell, particularly those who are in hospital
with a serious illness. Most MRSA infections are called "local" infections, such as
boils, abscesses or infected wounds. These are easily treated in a small number
of people, however, MRSA can cause serious infections such as septicaemia (also
known as "bloodstream infection" or "blood poisoning").
How can you tell if someone has MRSA?
Most people with MRSA carry the germ harmlessly and have no ill effects.
Patients who have an infection caused by MRSA do not look or feel any different
to patients who have infections caused by other germs. The only way to tell if
someone is carrying MRSA, or has an infection caused by MRSA, is to do a
laboratory test on a sample from a wound, blood, urine, nose, or other part of
the body. If MRSA is found in a sample it means that the person has MRSA on
their body.
How do people get MRSA?
The people most at risk of getting MRSA are those who have been in hospital for
a long time, or have a lot of contact with hospitals, or have a long-term illness,
or have had a lot of antibiotics. In the hospital, MRSA may be passed from one
person to another on the hands, of staff or visitors, by patient care equipment, or
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 31
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
by contamination of the hospital environment. MRSA is most likely to spread
where there is overcrowding and where a lot of antibiotics are used.
How does having MRSA affect a person's care in hospital?
Even though most people with MRSA carry the germ harmlessly, hospitals take
steps to stop the spread of MRSA to other people so that the risk of serious MRSA
infections is reduced. Patients in hospital who are carrying MRSA may be cared
for in a single room on their own, or may be cared for with other people with
MRSA in a particular ward area. Some patients who are carrying MRSA may also
be given antiseptic body and hair shampoo and an antiseptic cream for their nose
to try and get rid of the germ. Extra swabs may be taken from the nose and
other parts of the body after this treatment, to see if MRSA is still present.
If a person has an infection caused by MRSA they are treated with antibiotics,
usually given intravenously, i.e. by a 'drip'.
Can family and friends visit a person in hospital with MRSA?
MRSA does not harm healthy people, including pregnant women, children and
babies. MRSA rarely if ever presents a danger to the general public so friends
and family can visit normally. Visitors will be asked to clean their hands after
visiting a person with MRSA, so that they do not spread MRSA to other people.
If the family help to physically care for a person in hospital with MRSA, nursing
staff will tell them of any extra precautions that may need to be taken.
Can patients go home with MRSA?
Yes. Patients with MRSA will be allowed home when medically fit. Most people
lose MRSA when they leave hospital and when antibiotics are stopped. Relatives
including children and friends at home are not at risk form a patient with MRSA
who has been discharged from hospital.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 32
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
What happens if a person with MRSA needs to be re-admitted to
hospital?
A person who has had MRSA in the past will have swabs taken to see if they are
still carrying MRSA. They may be nursed in a single room, until the results of
these swabs are known.
Where can I get more information?
Patents in hospital and their relatives should not hesitate to ask medical or
nursing staff for more information on MRSA. Further advice may also be sought
from the hospital's infection prevention and control team.
Further information on MRSA is also available form, the following websites:
www.hpsc.ie
The Health Protection Surveillance Centre (HPSC) has a "Frequently Asked
Questions" page on Staph aureus and MRSA in the "Topics A-Z" section of their
website. Information ton the current levels of MRSA, and other infections, in
Ireland can also be found in the EARSS section of the HPSC website.
www.hpa.org.uk
The UK Health Protection Agency has background information on MRSA in the
"Topics A-Z" section of its website.
www.cdc.gov
The US Centres for Disease Control (CDC) website has information on MRSA
under its "A-Z Index"
www.amm.co.uk
The UK Association of Medical Microbiologists has a fact sheet on MRSA available
in the publications section of their website.
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 33
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
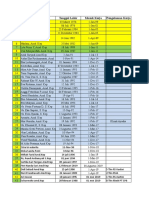
9.5 MRSA Decolonisation and Screening Chart
Patients Name:________________ D.O.B:________ Chart No.:_________________ Treatment No. _______________(Two treatments only allowed).
Treatment Day 1 Day 2 Day 3 Day 4 Day 5 Reswab
Nasal - Nasal Bactroban (Mupirocin 2%) T.D.S. x 5 day
Date: Date: Date: Date: Date: Date:
Skin/Groin
Octenisan antimicrobial body wash daily for 5 days. Wash hair with
Octenisan on Day 2 and Day 4
Date: Date: Date: Date: Date: Date:
Tracheostomy Site
Clean site with Chlorhexidine 0.05% (unisept)
Date Date Date Date Date Date
PEG Site
Clean site with Chlorhexidine 0.05% (unisept)
Date: Date: Date: Date: Date: Date:
Dialysis Exit Site
Clean site with Chlorhexidine 0.05% (unisept)
Nasal bactroban (Mupirocin 2%) x 5 treatments
Date: Date: Date: Date: Date: Date:
MRSA Screening Sites: Initial positive site:_________________________________
1. Nose ______________________________________ 5. C.S.U. (if catheterised) ________________
2. Groin OR Perineum _______________________ ()
3. Wounds________________________________
Device sites e.g. PEG, Trachy,CVP line ___________________________________________ 6. Sputum (if productive) _____________
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
FSS - Baile Átha Cliath & Lár Laighin GL No: IPCR 12
HSE - Dublin/Mid-Leinster Revision No: 4
Department
Infection Prevention and Control Page: 34
Guideline
Guideline Title: Control and Management of Methicillin Resistant Staphylococcus
Aureus (MRSA)
9.6 How to use Octenisan Poster
QA Template 002 Rev 3 March 2006
This is a controlled document and may be subject to change at any time.
QA Template 002 Rev 24 August 2006
This is a controlled document and may be subject to change at any time.
You might also like
- Trust Guideline For The Management of Stoma Output in Neonates and Infants v1Document23 pagesTrust Guideline For The Management of Stoma Output in Neonates and Infants v1Vian100% (1)
- NHS Application - TTMDocument12 pagesNHS Application - TTMelvis uduNo ratings yet
- Neonatal SepsisDocument21 pagesNeonatal SepsisDyah Ayu Puspita AnggarsariNo ratings yet
- Draft CPG Dengue in Children For ReviewerDocument59 pagesDraft CPG Dengue in Children For ReviewerhacepNo ratings yet
- HTTPSWWW - Moh.gov - mymohresourcesPenerbitanCPGInfectious20DiseaseCPG Management of Dengue in Children 06072021 PDFDocument72 pagesHTTPSWWW - Moh.gov - mymohresourcesPenerbitanCPGInfectious20DiseaseCPG Management of Dengue in Children 06072021 PDFesthersumiNo ratings yet
- ANBL09P1DOCDocument160 pagesANBL09P1DOCrheaNo ratings yet
- MRSA Procedure 2021Document28 pagesMRSA Procedure 2021توفيق باعبادNo ratings yet
- Patients With Clostridium Difficile Associated With Diarrhoea Management of - CA1001 v8.1 - C12Document25 pagesPatients With Clostridium Difficile Associated With Diarrhoea Management of - CA1001 v8.1 - C12andreeaNo ratings yet
- WHO On Tuberculosis: Operational HandbookDocument110 pagesWHO On Tuberculosis: Operational HandbookRafael SanchezNo ratings yet
- AALL0331DOC Standard RiskDocument208 pagesAALL0331DOC Standard RiskKim66No ratings yet
- Guidelines For Phase I Clinical Trials 2018 Edition 20180626Document72 pagesGuidelines For Phase I Clinical Trials 2018 Edition 20180626Juan Vasquez100% (1)
- ICUDocument84 pagesICUSarahNo ratings yet
- 3 National Guidelines On DRTB 2019 PDFDocument186 pages3 National Guidelines On DRTB 2019 PDFOnline Test NepalNo ratings yet
- Staphylococcus Aureus (MRSA) Clinical GuidelineDocument31 pagesStaphylococcus Aureus (MRSA) Clinical GuidelinedanielaNo ratings yet
- Clinical+Guideline MRSA April2014 PDFDocument31 pagesClinical+Guideline MRSA April2014 PDFLoudry Amsal EGNo ratings yet
- VaricellaDocument9 pagesVaricellaWajih FarhanNo ratings yet
- COVID 19 Policy KP V1Document60 pagesCOVID 19 Policy KP V1Tufail Khan100% (3)
- GuidelinesDocument64 pagesGuidelinesdayanandasagar pNo ratings yet
- Policies & Procedures On Infection Prevention and ControlDocument308 pagesPolicies & Procedures On Infection Prevention and ControlHawthorn ANo ratings yet
- Manual Vacuum Aspiration MVA Response 7876Document17 pagesManual Vacuum Aspiration MVA Response 7876OmolosoNo ratings yet
- CPG Haemophilia 2018Document101 pagesCPG Haemophilia 2018m14zarNo ratings yet
- CPG Management of Haemophilia 20191024 PDFDocument21 pagesCPG Management of Haemophilia 20191024 PDFwinnie yewNo ratings yet
- Nationl 2520 Guideline 2520 TB2520 and 25202015Document60 pagesNationl 2520 Guideline 2520 TB2520 and 25202015Patricia SmitNo ratings yet
- COVID-19: Guidance For The Remobilisation of Services Within Health and Care SettingsDocument43 pagesCOVID-19: Guidance For The Remobilisation of Services Within Health and Care SettingsAndreea MorgovanNo ratings yet
- Antifungal Clinical Guideline CA4006 v3.2Document18 pagesAntifungal Clinical Guideline CA4006 v3.2Adrian Pardo VillegasNo ratings yet
- 2) CPG Management of Rheumatoid ArthritisDocument58 pages2) CPG Management of Rheumatoid ArthritisEdward LaurentNo ratings yet
- HIV Consensus Guideline 2022Document124 pagesHIV Consensus Guideline 2022rihuiNo ratings yet
- Draft CPG Management of Tuberculosis (Fourth Edition) For ReviewersDocument97 pagesDraft CPG Management of Tuberculosis (Fourth Edition) For ReviewersBrian BeeNo ratings yet
- Guidelines Molds FinalDocument36 pagesGuidelines Molds Finalmhafez1979No ratings yet
- Tracheostomy Guidelines 2018Document97 pagesTracheostomy Guidelines 2018KateCuadraNo ratings yet
- General Surgical Services Operational PolicyDocument97 pagesGeneral Surgical Services Operational PolicyHEHENo ratings yet
- WHO MDR 2020 Handbook Treatment PDFDocument88 pagesWHO MDR 2020 Handbook Treatment PDFYuanita GunawanNo ratings yet
- CPG Management of Glaucoma (Second Edition) PDFDocument87 pagesCPG Management of Glaucoma (Second Edition) PDFShashidharan MenonNo ratings yet
- Treatment Tuberculosis Guidelines Fourth EditionDocument160 pagesTreatment Tuberculosis Guidelines Fourth Editionhasan andrianNo ratings yet
- COVID-19 Workplace Protection: and Improvement GuideDocument36 pagesCOVID-19 Workplace Protection: and Improvement GuideKoushik Mukhopadhyay50% (2)
- The Control and Prevention of MRSA in Hospitals and in The CommunityDocument41 pagesThe Control and Prevention of MRSA in Hospitals and in The CommunityDimas RfNo ratings yet
- VarmamGuideline PDFDocument50 pagesVarmamGuideline PDFsaivasmaNo ratings yet
- 06.15.20 Management of Vaginal Birth After Caesarean Section (Vbac) Attachment 1Document16 pages06.15.20 Management of Vaginal Birth After Caesarean Section (Vbac) Attachment 1Muhammad HaziqNo ratings yet
- Who HCV 2018Document108 pagesWho HCV 2018hendrawanNo ratings yet
- SL Microbiology - Manual-2005Document201 pagesSL Microbiology - Manual-2005Ishara VithanaNo ratings yet
- Codigos Sagrados Orden AlfabeticoDocument51 pagesCodigos Sagrados Orden AlfabeticomedellincolombiaNo ratings yet
- Listeria Monocytogenes and Other Listeria Species PDFDocument27 pagesListeria Monocytogenes and Other Listeria Species PDFkurniawan0031No ratings yet
- Niv BK 9051941 EnusDocument84 pagesNiv BK 9051941 EnusmatijahNo ratings yet
- Ccu PDFDocument82 pagesCcu PDFSarahNo ratings yet
- CCUDocument82 pagesCCUSarah100% (1)
- Management of Patients With Venous Leg Ulcers FINAL 2016Document67 pagesManagement of Patients With Venous Leg Ulcers FINAL 2016dwirkyNo ratings yet
- Niv Fibel BK 9051941 en PDFDocument84 pagesNiv Fibel BK 9051941 en PDFmatijahNo ratings yet
- UTI in Children NICE GuidelinesDocument178 pagesUTI in Children NICE GuidelinesDanielle ConcepcionNo ratings yet
- Recommendations For The Control of Carbapenemase-Producing Enterobacterales Final Accessible PDF Version November 2021Document66 pagesRecommendations For The Control of Carbapenemase-Producing Enterobacterales Final Accessible PDF Version November 2021obakhit91No ratings yet
- Clinical Trial Protocol: Funding SourceDocument34 pagesClinical Trial Protocol: Funding Source4 - Alya RamadhaniNo ratings yet
- Clinical Procedures For Safer Patient Care 1634318703. PrintDocument792 pagesClinical Procedures For Safer Patient Care 1634318703. PrintAnn DassNo ratings yet
- Niv Fibel Inlay BK 9051941 enDocument84 pagesNiv Fibel Inlay BK 9051941 enPopescu Cristina ElenaNo ratings yet
- National Guidelines and Operational Manual For Tuberculosis Control PDFDocument90 pagesNational Guidelines and Operational Manual For Tuberculosis Control PDFFaisol KabirNo ratings yet
- Safety and Preliminary of Immunogenicity Following Recombinant Hepatitis B (Bio Farma) Vaccine in Adults & Children Phase I Study ProtocolDocument58 pagesSafety and Preliminary of Immunogenicity Following Recombinant Hepatitis B (Bio Farma) Vaccine in Adults & Children Phase I Study ProtocolSariAngrainiNo ratings yet
- 7 UlannDocument2 pages7 UlannLidwina ApyakaNo ratings yet
- Vale of Leven Hospital ReportDocument456 pagesVale of Leven Hospital Reportpurses18No ratings yet
- Ukall Xii V4.1Document62 pagesUkall Xii V4.1Doc Javaria ChaudryNo ratings yet
- Acute Care For Nurses Student Survival Skills Jan 17 2023 - 1119882451 - Wiley Blackwell 1St Edition Boyd Full ChapterDocument68 pagesAcute Care For Nurses Student Survival Skills Jan 17 2023 - 1119882451 - Wiley Blackwell 1St Edition Boyd Full Chapterjoyce.wilson922100% (5)
- Handbook of Evidence-Based Veterinary MedicineFrom EverandHandbook of Evidence-Based Veterinary MedicineRating: 2.5 out of 5 stars2.5/5 (1)
- Discussion On Difficulties and Countermeasures in The Construction of Financial Shared Service Center Under The Background of DigitizationDocument6 pagesDiscussion On Difficulties and Countermeasures in The Construction of Financial Shared Service Center Under The Background of DigitizationEditor IJTSRDNo ratings yet
- 5-Mini-Implant-Miniscrews in Orthodontics-Cbct Tads - Oussama Sandid - Mohamad Aboualnaser-Awatef Shaar-Miniscrews Mini-Implant en Orthodontie Orthodontists Dentists Lebanon Beirut France UsaDocument15 pages5-Mini-Implant-Miniscrews in Orthodontics-Cbct Tads - Oussama Sandid - Mohamad Aboualnaser-Awatef Shaar-Miniscrews Mini-Implant en Orthodontie Orthodontists Dentists Lebanon Beirut France UsaAnonymous oD9H6T8pNo ratings yet
- Artificial Method (Hormonal Method)Document45 pagesArtificial Method (Hormonal Method)Ninfa Lansang100% (1)
- Dr. Neeraj Suri For ENT Surgeon, Best Hearing Aid, Cochlear Implant in Ahmedabad, Gandhinagar, Rajkot, Baroda, Surat, GujaratDocument9 pagesDr. Neeraj Suri For ENT Surgeon, Best Hearing Aid, Cochlear Implant in Ahmedabad, Gandhinagar, Rajkot, Baroda, Surat, GujaratDesai Tourism - ThailandNo ratings yet
- P2 NCP 1Document4 pagesP2 NCP 1Kyle Albert EstoestaNo ratings yet
- Electrotherapy KovacsDocument706 pagesElectrotherapy KovacsDibyendunarayan BidNo ratings yet
- Mapping Perawat N BidanDocument9 pagesMapping Perawat N BidanHevrimaHtmNo ratings yet
- CDI Background: Respiratory Failure: Definitions For Acute Respiratory Failure and ARDS Endorsed by Sutter SystemDocument5 pagesCDI Background: Respiratory Failure: Definitions For Acute Respiratory Failure and ARDS Endorsed by Sutter SystemNafisah Putri WyangsariNo ratings yet
- Ati RN Proctored Maternal Newborn Form C 2016Document2 pagesAti RN Proctored Maternal Newborn Form C 2016Stevania96% (24)
- Ge Resuscitation Using T PieceDocument4 pagesGe Resuscitation Using T Pieceyagnaashi9092No ratings yet
- Application For Assessment of Training: Required Form For Entry To The MRCOG Part 3 Membership Exam Personal InformationDocument4 pagesApplication For Assessment of Training: Required Form For Entry To The MRCOG Part 3 Membership Exam Personal InformationMd ZhidNo ratings yet
- Severity Anemia Pregnancy Adverse Maternal Fetal Outcomes Tertiary CareDocument8 pagesSeverity Anemia Pregnancy Adverse Maternal Fetal Outcomes Tertiary CareSSR-IIJLS JournalNo ratings yet
- Neonatal FracturesDocument25 pagesNeonatal FracturesORTOPEDIKUS - ANGOLANo ratings yet
- Obeid Specialized Hospital - Riyadh: Inpatient DeptsDocument4 pagesObeid Specialized Hospital - Riyadh: Inpatient DeptsLovelydePerioNo ratings yet
- Evidence Based Practice: College of Allied Health Department of NursingDocument8 pagesEvidence Based Practice: College of Allied Health Department of NursingIzelle FigueroaNo ratings yet
- N30965F Freedom Surgical+toolsDocument2 pagesN30965F Freedom Surgical+toolsBlack Tear MiseryNo ratings yet
- Cho Session DesignDocument8 pagesCho Session DesignConsolacion Binarao DoloresNo ratings yet
- Vaginismus Day 2Document9 pagesVaginismus Day 2Joanne BlancoNo ratings yet
- Hopkins Medicine Review NephrologyDocument35 pagesHopkins Medicine Review NephrologyMuhammad Bilal50% (2)
- Audit, Registry and QIP: Supporting The IBD StandardsDocument23 pagesAudit, Registry and QIP: Supporting The IBD Standardscfmunro65No ratings yet
- Tibio-Tarsal Luxation and Its Management in A Dog: Ayyappan, S., M. Shiju Simon, B. C. Das and R. Suresh KumarDocument4 pagesTibio-Tarsal Luxation and Its Management in A Dog: Ayyappan, S., M. Shiju Simon, B. C. Das and R. Suresh KumarEnnur NufianNo ratings yet
- Cesarean Section Under Spinal Anesthesia in A Patient With Ankylosing SpondylitisDocument4 pagesCesarean Section Under Spinal Anesthesia in A Patient With Ankylosing SpondylitisFendy PrasetyoNo ratings yet
- Massive Transfusion. CHEST. 2009.Document14 pagesMassive Transfusion. CHEST. 2009.Jose Fernando Díez ConchaNo ratings yet
- 1 Institutional Nursing - Field in NursingDocument18 pages1 Institutional Nursing - Field in NursingsannsannNo ratings yet
- Of These Parts of The Body. Example: What Structure Is Above The Eye?)Document4 pagesOf These Parts of The Body. Example: What Structure Is Above The Eye?)Anonymous QexowtfNo ratings yet
- Menstrual CycleDocument8 pagesMenstrual CycleAlloiBialba100% (1)
- China Successfully Launching Billings Ovulation MethodDocument8 pagesChina Successfully Launching Billings Ovulation MethodDr. Liza ManaloNo ratings yet
- Goso - Ob WardDocument1 pageGoso - Ob WardKristine Nacua100% (1)
- P7 TR Apg 2020Document26 pagesP7 TR Apg 2020Lia NurNo ratings yet